Hos patienter med grad II AV-blok af Wenchebach-typen er der ingen indikation for invasiv elektrofysiologisk undersøgelse for at bestemme HV-intervallet. Indikation for de-novo implantation af et CRT-system hos patienter med konventionel pacemakerindikation og hjertesvigt.
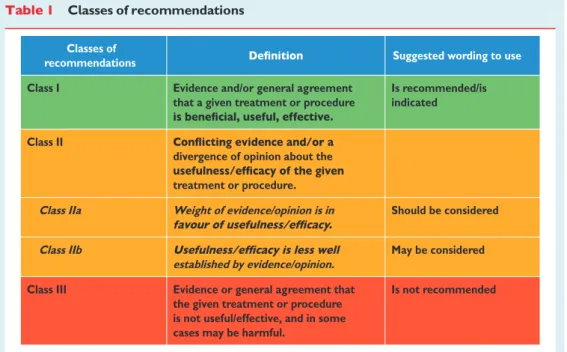
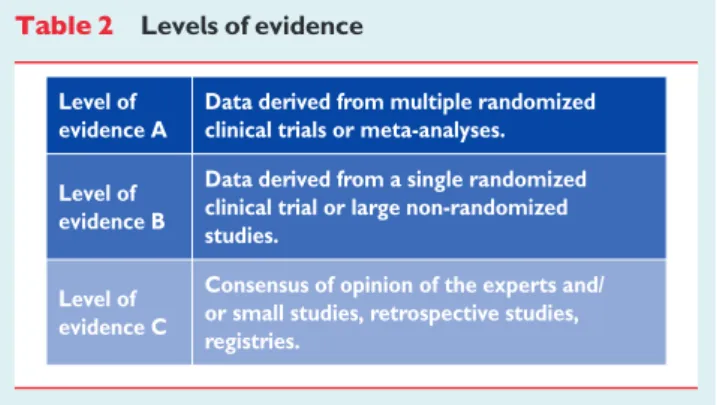
Preamble
They are only available on the ESC website at http://www.escardio.org/guidelines-surveys/. The national associations of the ESC are encouraged to endorse, translate and implement the ESC guidelines.
Indications for pacing
Epidemiology, natural history, pathophysiology,
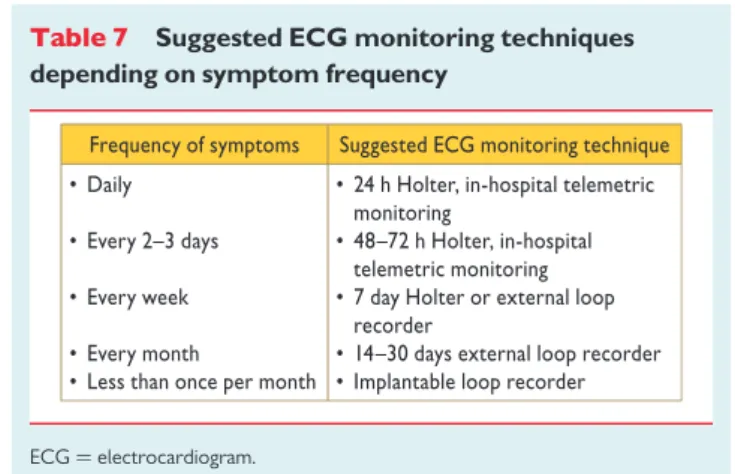
While the permanent forms of bradyarrhythmia are caused by an intrinsic disease of the sinus node or AV conduction system, the etiology of intermittent bradyarrhythmia can be difficult to determine. Laboratory testing. The assumption is that provoked abnormalities will have the same mechanism as a spontaneous episode.
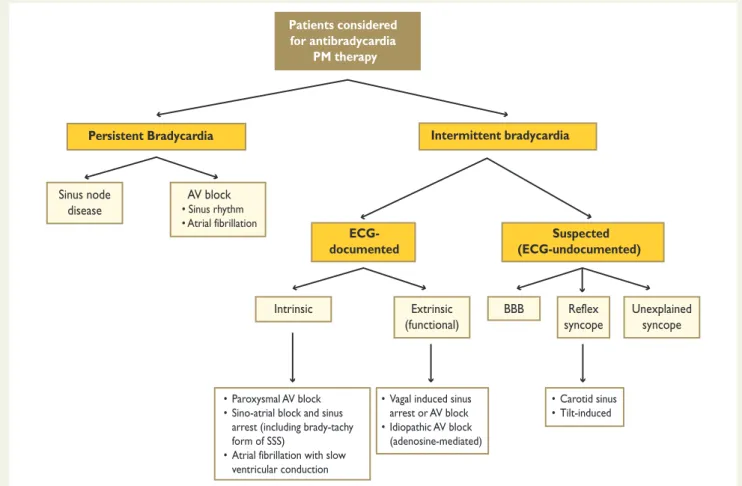
Persistent bradycardia
- Indications for pacing
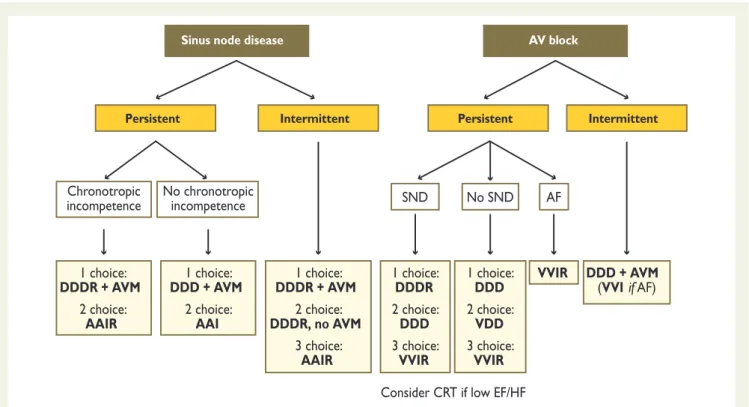
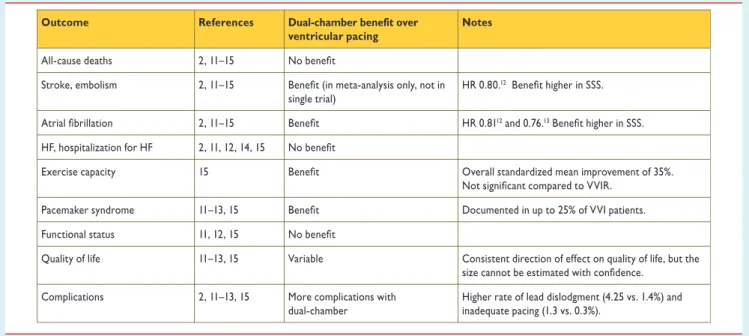
- Choice of pacing mode
Pacing is not indicated in patients with AV block due to reversible causes. In patients with persistent SB, dual chamber pacing is the pacing mode of choice (Figure 3).
Intermittent (documented) bradycardia
- Indications for pacing
- Choice of pacing mode
Pacing is indicated in patients with intermittent/paroxysmal intrinsic third- or second-degree AV block. Pacing should be considered in patients with a history of syncope and documentation of asymptomatic pauses >6 s due to sinus arrest, sinus-atrial block, or AV block.
Suspected (undocumented) bradycardia
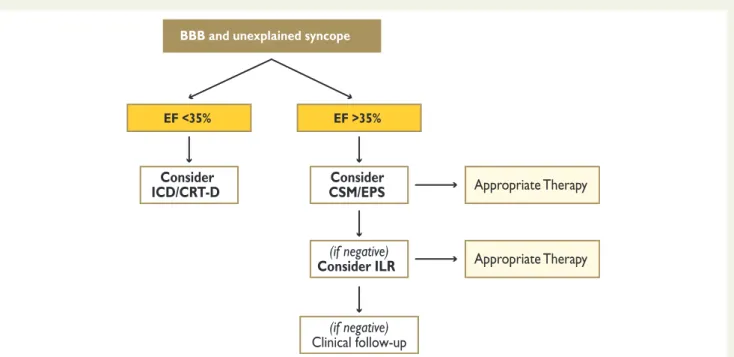
- Bundle branch block
- Reflex syncope
- Unexplained syncope (and fall)
- Indications for cardiac resynchronization therapy
- Epidemiology, prognosis, and pathophysiology of heart
There is sufficient evidence and a strong consensus that stimulation is not indicated in patients with asymptomatic BBB. Pacing is indicated in patients with dominant carotid sinus cardioinhibitory syndrome and recurrent unpredictable syncope. In patients with carotid sinus syndrome, the most suitable method of stimulation is in two chambers.
In patients with cardioinhibitory vasovagal syncope, dual-chamber pacing is the preferred mode of pacing. The loss of ventricular preload then leads to a reduction in LV Indication for cardiac pacing in patients with unexplained. Patients are not indicated in patients with unexplained syncope without evidence of bradycardia or conduction disturbance.

Patients in sinus rhythm
Indications for cardiac resynchronization therapy
- Patients in New York Heart Association
- Patients in New York Heart Association
- Patient selection: role of imaging techniques to
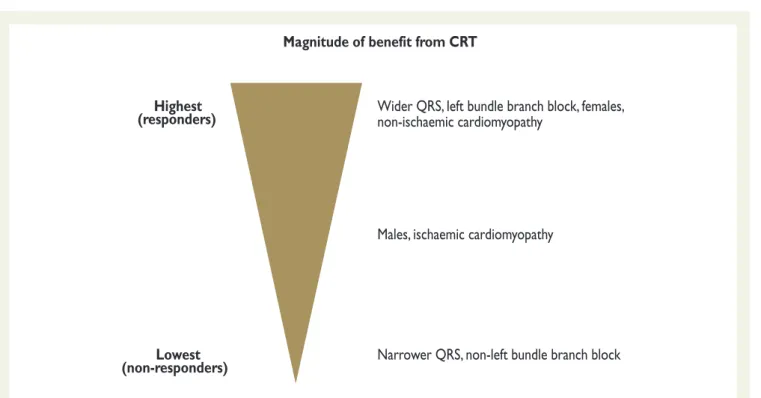
In the Cardiac Resynchronization Therapy in Patients with Heart Failure and Narrow QRS (RethinQ) trial, 65CRT did not improve peak oxygen consumption (primary endpoint) or quality of life in the subgroup of patients with QRS ≥120 ms and evidence of echocardiographic dyssynchrony . The recent randomized, double-blind Evaluation of Resynchronization Therapy for Heart Failure in Patients with QRS Duration of Less than 120 ms (MORE ALL) trial66, which compared active trials vs. definitive, due to the low number of patients enrolled in the RCT.
The evidence for recommending CRT in patients with NYHA class IV is inconclusive, due to the low number of patients enrolled in RCTs. Sub-analyses of randomized clinical trials and meta-analyses showed that the beneficial effects of CRT were observed in patients with typical LBBB. The evidence of benefit in patients with non-LBBB configuration is weak, especially in patients with QRS ,150 ms and NYHA classes I and II.

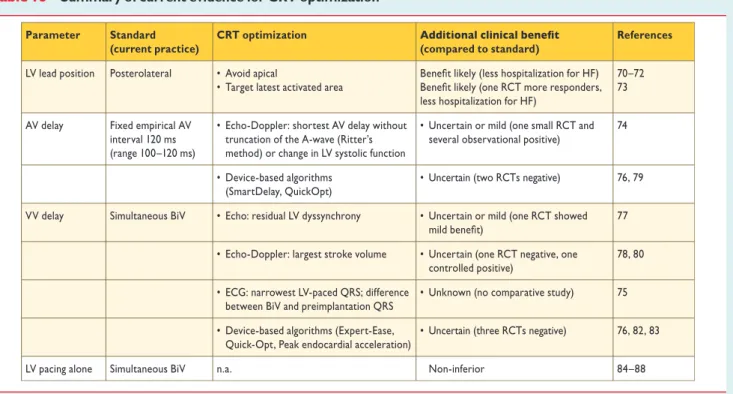
Choice of pacing mode (and cardiac resynchronization
Furthermore, in a cross-sectional analysis that included 80,768 patients,69 a percentage of biventricular pacing was achieved.98% in only 59% of patients. This evidence suggests that biventricular pacing should be kept as close to 100% as possible. Cardiac resynchronization therapy device optimization Observational studies have identified suboptimal programming of the AV and/or VV delays as determinant factors of poor response to CRT.w133 Small randomized trials and some observational series have shown significant improvements in HF symptoms and HF hospitalizations after optimization of the AV and VV delays,74,75,w134 – w143 especially in ischemic HF patients.w144 These findings were not supported by the results of larger multicenter trials,76–83 which suggested that routine AV and VV delay optimization had limited effect on clinical or echocardiographic effects have outcomes in CRT recipients, compared with a fixed 100-120 ms AV delay and simultaneous biventricular pacing (RV and LV) (Web Table 12).
LEVO Univentricular Pacing with ICD Back-up in Patients with Heart Failure (B-LEVO) A heart failure trial that randomized 176 CRT-D recipients to biventricular or LV pacing. similar improvements in 6-minute walk, quality of life, NYHA functional class, and peak oxygen consumption compared with biventricular pacing. Regarding echocardiographic endpoints, biventricular pacing tended to produce greater improvements in LVEF and reductions in LV volumes compared with no LV pacing.86 Results of a multicenter, double-blind, crossover evaluation of resynchronization therapy for heart failure in patients with a QRS duration GREATER than 120 ms (GREATER- EARTH) trial showed that LV pacing is similar to biventricular. LV pacing alone in pacemaker-independent patients appears to be non-inferior to biventricular pacing for improving soft endpoints (quality of life, exercise capacity and LV reverse remodeling) and could be considered to reduce cost and complexity procedure and extending the life of the device.
Patients in atrial fibrillation
Patients with heart failure, wide QRS, and reduced
Conversely, other studies, 97,103–105 which showed similar improvement in SR and AF, support a conservative initial strategy in patients with AF by optimizing the medical treatment and programming the CRT device to achieve a higher percentage of ventricular pacing , and reserve AV node ablation only for patients with poor heart rate control. In conclusion, the routine use of AV junction ablation ensures adequate biventricular pacing in patients with AF (Figure 10). Despite the weak evidence - due to a lack of large randomized trials - the prevailing opinion of experts is in favor of the usefulness of CRT in AF patients with the same indications as for patients in SR, provided that AV junction ablation is added in those patients with incomplete (.99%) biventricular capture.
Some experts were concerned about the lack of evidence from randomized trials on the benefits of CRT in patients with AF and felt that too much emphasis had been placed on the theory that the dominant mechanism of CRT was bi-ventricular pacing. Much of the benefit of CRT may be due to atrioventricular rather than biventricular stimulation; in this case, CRT may be less effective or ineffective in patients with AF, as atrioventricular pacing cannot be provided in AF. Demonstration that CRT is effective or not effective in patients with AF should provide further insight into the mechanisms of CRT effect.
Patients with uncontrolled heart rate who are
In a recent systematic review, 99CRT and AV junction ablation were associated with significant reductions in all-cause mortality (hazard ratio 0.42) and cardiovascular mortality (hazard ratio 0.44) and improvements in NYHA functional class (hazard ratio 0.52 ) compared with CRT without AV junction ablation. AV junction ablation can be performed at the time of CRT implantation or several weeks later, after which lead and device function is guaranteed. The PAVE,94Optimal Pacing SITE (OPSITE)106and AV Node Ablation with CLS and CRT Pacing Therapies for Treatment of AF (AVAIL CLS/CRT)105 trials showed that CRT has a modest but significant effect on quality of life, NYHA class and LVEF. compared to RV pacing, in patients with AF and AV nodal ablation and different levels of LV function.
There is evidence, from small randomized trials, of an additional benefit of performing CRT pacing in patients with reduced EF, who are candidates for AV junction ablation for rate control, to reduce hospitalization and improve quality of life. improve. There is weak evidence that CRT is superior to RV pacing in patients with preserved systolic function. In perspective, there is a need for large RCTs to assess the efficacy of CRT in patients with permanent or long-term persistent AF in terms of morbidity and mortality.
Patients with heart failure and conventional pacemaker
- Patients with an indication for upgrading from
Novocardial resynchronization therapy pacing in patients with a conventional indication for bradycardia pacing (Recommendation 2). Small randomized trials suggested that patients with moderate to severe LV dysfunction might benefit from CRT instead of conventional RV apical stimulation (Table). In general, the primary endpoints of these trials were surrogate hemodynamic endpoints. The same findings were observed in 2 years of follow-up.124 The PREventing VENTricular Dysfunction in Pacemaker Patients Without Advanced Heart Failure (PREVENT-HF) study, 129 randomly assigned 108 patients with high levels of AV block to CRT or RV pacing with or without an ICD, showed no benefit for CRT in terms of LV remodeling at 12 months.
In the biventricular versus right ventricular rhythm test in patients with AV block (BLOCK HF) with. There is emerging evidence that implantation of novoCRT can reduce HF hospitalization, improve quality of life, and reduce HF symptoms in patients with a history of HF, depressed cardiac function, and a bradycardia pacing indication. Late enhancement after the development of HF appears to offer benefits similar to denovimplantation in patients with initially preserved cardiac function.

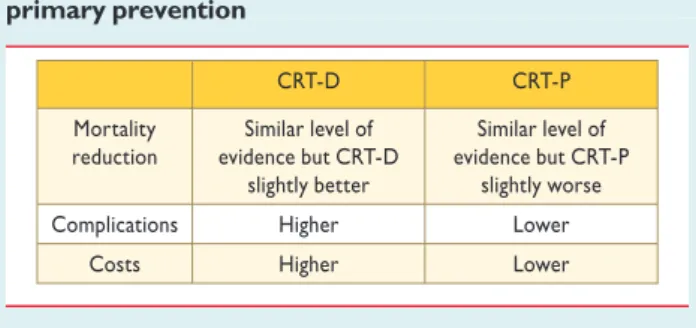
Back-up implantable cardioverter defibrillator in
- Benefit of adding cardiac resynchronization therapy in
- Benefit of adding implantable cardioverter defibrillator
- Indications for pacing in specific conditions
- Pacing in acute myocardial infarction
- Pacing after cardiac surgery, transcatheter aortic valve
- Pacing and cardiac resynchronization therapy in children
- Pacing in hypertrophic cardiomyopathy
- Pacing in rare diseases
- Pacing in pregnancy
- Pacing for first-degree atrioventricular block
- Algorithms for prevention and termination of atrial
- Complications of pacing and CRT implantation
- Management considerations
- Pacing from alternative right ventricular sites
- Re-implantation of pacemaker/cardiac resynchronization
- Magnetic resonance imaging in patients with implanted
- Emergency (transvenous) temporary pacing
- Remote management of arrhythmias and device
Effects of multi-site biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med. Meta-analysis of randomized controlled trials comparing isolated left ventricular and biventricular pacing in patients with chronic heart failure.Am J Cardiol. Left ventricular versus simultaneous biventricular pacing in patients with heart failure and a QRS complex./¼120 milliseconds.Circulation2011;.
Comparison of benefit and mortality in cardiac resynchronization therapy in patients with atrial fibrillation versus patients in sinus rhythm (Results of the Spanish Atrial Fibrillation and Resynchronization Study [SPARE]). Am J Cardiol. Comparison of response to cardiac resynchronization therapy in patients with sinus rhythm versus chronic atrial fibrillation.Am J Cardiol. Comparison of the benefit of cardiac resynchronization therapy in patients with atrial fibrillation and heart failure versus patients with sinus rhythm and heart failure.Am J Cardiol.
Upgrading to biventricular pacing in patients with conventional pacemakers and heart failure: a double-blind, randomized crossover study. Europace. Long-term effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure. Europace.