Brazilian
Journal
of
OTORHINOLARYNGOLOGY
www.bjorl.org
ORIGINAL
ARTICLE
Autotransplant
tissue
selection
criteria
with
or
without
stereomicroscopy
in
parathyroidectomy
for
treatment
of
renal
hyperparathyroidism
夽
Monique
Nakayama
Ohe
a,∗,
Rodrigo
Oliveira
Santos
b,
Murilo
Catafesta
das
Neves
b,
Aluizio
Barbosa
Carvalho
c,
Ilda
Sizue
Kunii
a,
Márcio
Abrahão
b,
Onivaldo
Cervantes
b,
Marise
Lazaretti-Castro
a,
José
Gilberto
Henriques
Vieira
aaDepartmentofEndocrinologyandMetabology,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(EPM-UNIFESP), SãoPaulo,SP,Brazil
bDepartmentofOtorhinolaryngology,HeadandNeck,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo (EPM-UNIFESP),SãoPaulo,SP,Brazil
cDepartmentofNephrology,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(EPM-UNIFESP),SãoPaulo,SP,Brazil
Received2July2013;accepted24January2014 Availableonline11June2014
KEYWORDS
Parathyroidhormone; Hyperparathyroidism, secondary;
Parathyroidectomy
Abstract
Introduction:Severalmethodshavebeenproposedtoimproveoperativesuccessinrenal hyper-parathyroidism.
Objective:Toevaluatestereomicroscopyinparathyroidtissueselectionfortotal parathyroidec-tomywithautotransplantationinsecondary(SHPT)/tertiary(THPT)hyperparathyroidism.
Methods:118renalpatientsunderwentsurgeryfromAprilof2000toOctober2009.Theywere dividedintotwogroups:G1,66patientsoperatedfromAprilof2000toMayof2005,withtissue selectionbasedonmacroscopicobservation;G2,52patientsoperatedfromMarchof2008to October2009withstereomicroscopyfortissueselectionsearchingforthepresenceofadipose cells.Allsurgeries were performedby thesame surgeon.Patientspresented SHPT(dialysis treatment)orTHPT(renal-grafted).Follow-upwas12---36months.Intra-operativeparathyroid hormone(PTH)wasmeasuredin100/118(84.7%)patients.
Results:Dataarepresentedasmeans.G1included66patients(38SHPT,24females/14males; 40.0yearsofage;28THPT,14females/14males;44yearsofage).G2included52patients(29 SHPT,11females/18males;50.7yearsofage;23 THPT,13females/10males,44.4yearsof age).SHPTpatientsfromG2presentedpreoperativeserumcalciumhigherthanthoseofSHPT patientsinG1(p<0.05),suggestingamoreseveredisease.Definitivehypoparathyroidismwas foundinsevenof118patients(5.9%).Graft-dependentrecurrenceoccurredinfourpatients, twoineachgroup.Alloccurredindialysispatients.
夽 Pleasecitethisarticleas:OheMN,SantosRO,NevesMCd,CarvalhoAB,KuniiIS, AbrahãoM,etal.Autotransplant tissueselection criteriawithorwithout stereomicroscopyin parathyroidectomyfor treatmentofrenal hyperparathyroidism. Braz JOtorhinolaryngol. 2014;80:318---24.
∗Correspondingauthor.
E-mail:moniqueohe@uol.com.br(M.N.Ohe). http://dx.doi.org/10.1016/j.bjorl.2014.05.012
Conclusion: StereomicroscopyinSHPT/THPTsurgicaltreatmentmaybeausefultoolto stan-dardizeparathyroidtissueselection.
© 2014Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE Hormônio
paratireóideo; Hiperparatireoidismo secundário;
Paratireoidectomia
Influênciadocritériodeselec¸ãodetecidoparatiroideanocomousem
estereomicroscopiaparaautoimplantenoresultadodotratamentocirúrgicodo
hiperparatiroidismoassociadoadoenc¸arenalcrônica
Resumo
Introduc¸ão: Diversosmétodostêmsidopropostoscomintuitodemelhoraríndicesdesucesso cirúrgiconotratamentodohiperparatiroidismoassociadoàdoenc¸arenalcrônica(DRC).
Objetivos: Avaliar uso do estereomicroscópio na selec¸ão de tecido paratiroideano na paratiroidectomiatotalcomautoimplanteempacientescomDRC.
Métodos: 118 pacientes DRC operados entre 04/2000-10/2009 foram divididos em: G1-66 pacientesoperados entre04/2000-05/2005cujaselec¸ãodetecidofoi realizadapormétodo convencional(macroscopia);G2-52pacientesoperadosentre03/2008-10/2009,cujaselec¸ão detecidofoirealizadacomusodaestereomicroscopia:Leica-Stereomicroscope(amplificac¸ão: 10×-80×).Pacientesforamaindacategorizadosemhiperparatiroidismosecundário (HPS)ou
terciário (HPT) (HPS-diálise/HPT-transplantados renais). Seguimento pós-operatório: 12-36 meses.PTHintraoperatóriomedido100/118pacientes(84.7%).Todospacientesforamoperados pelomesmocirurgião.
Resultados: Dadosemmédia.G1,66pacientes(38HPS,24f/14m;40anos;28HPT,14f/14m; 44anos).G2,52pacientes(29HPS,11f/18m;50,7anos;23HPT,13f/10m;44,4anos).Pacientes dialíticosdoG2apresentaramcálciopré-operatóriomaiorqueG1(p<0,05),sugerindodoenc¸a maissevera. Hipoparatiroidismodefinitivo: 7/118(5,9%)pacientes:G1,4/66(6%);G2,3/52 (5,7%).Recorrência dohiperparatiroidismonoautoimplante:4pacientes,2em cadagrupo. Todasforamempacientesemdiálise.
Conclusão:EstereomicroscopianotratamentodohiperparatiroidismoassociadoàDRCéútilna padronizac¸ãodatécnicadeselec¸ãodetecidoparaoautoimplante.
©2014Associac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicado por ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Thelongersurvivalofchronicrenalpatientshasincreased theincidenceofsymptomatichyperparathyroidism, increas-ing the need of surgical procedure.1 The best surgical
approachforrenalhyperparathyroidismisstilldebatedand controversy remains.Relevant questionshave been raised regardingtreatmentelection,sincepost-surgicalrecurrence and the risk of definitive hypoparathyroidism should be avoided. Total parathyroidectomy with parathyroid tissue autotransplantation is a well-accepted technique for the management of these patients.2---7 Since recurrence rates
of 8%8 to 20%9 and up to 76%10 have been reported in
the literature,the greatmajority graft-dependent, tissue selection for autotransplantation has been presented as a considerable challenge. Analysis of parathyroid hyper-plastic tumors, using X-chromosome inactivation, have demonstratedthatmonoclonaltransformationisafrequent occurrencein uremicpatients.11 In fact,thegreat
major-ity(64%)ofparathyroidglandswithgeneralizedhyperplasia (non-nodular component) wereunequivocally monoclonal, asdemonstratedby Arnold etal.11 This findingimposes a
difficultcondition inparathyroidtissueselectionfor auto-transplantation.
Intraoperativetissueselectionofparathyroidfragments usingastereomagnifierwasfirstdescribed byNeyeretal. in2002.12Thetechniquecandifferentiateparathyroid
nor-motropic areas by the presence of stromal fat cells from thosethataredisfunctionalandhyperplastictissuewithout fatcells.12 Cellsfromtheselipid-containingareas present
an optimal in vitro suppression of parathyroid hormone (PTH)secretionbyhighcalciumlevels,13indicatinganormal
calcium set-point and suggesting the eligibility for auto-transplantation.
Theaimofthisstudywastocomparestereomicroscopy toconventionalmacroscopicobservationinparathyroid tis-sueselectionusingahistoricalcontrol,inordertoprovide a standardized procedure for renal hyperparathyroidism surgery.
Patients
and
methods
Patients
118renalpatientsunderwenttotalparathyroidectomywith intramuscular presternal autotransplantation7 from April
at the Renal Osteodystrophy Unit in this institution and werereferred tosurgical treatment for persistent hyper-calcemia not responsive to medical interventions and/or persistent hyperphosphatemia despite the continued use of dietary phosphorus restriction and phosphate-binding agents, withsigns andsymptoms such asintractable pru-ritus,severebone pain,fracturesor highrisk offracture, skeletaldeformities,extraskeletalcalcifications, develop-mentofcalciphylaxis,andradiographicevidencesofrenal osteodystrophy.
Patients were divided into two groups: group 1 (G1) consistedof66patientswhounderwentsurgeryfromApril of 2000 to May of 2005, and parathyroid tissue selection for autotransplantation wasperformed usingconventional techniquebasedonmacroscopicparathyroidtissue observa-tionbyasingleexperiencedsurgeon;group2(G2)consisted of52patientswhounderwentsurgeryfromMarchof2008 to October of 2009, and parathyroid tissue selection for autotransplantationwasperformedbythesamesurgeonas G1, based on stereomicroscopy observation using a Leica Stereo Zoom S8 APO Stereomicroscope (Leica Microsys-tems GmbH --- Wetzlar, Germany), with magnification of 10---80×.
Patientswereclassifiedassecondaryor tertiary hyper-parathyroidism:secondaryhyperparathyroidism(SHPT)was characterized as an acquired disorder observed in end-stage renal disease, in which the uremic state presents a continuous stimulus to the parathyroid glands. The SHPT group included patients under dialysis treatment who presented severe hyperparathyroidism with normal or high serum calcium levels. The tertiary hyper-parathyroidism (THPT) group comprised renal patients with functioning kidney transplant and nonsuppressible parathyroid hyperplasia, with persistent increased PTH levels and hypercalcemia. Hypercalcemia after kidney transplantation is usually due to hyperparathyroidism that persists from the preceding chronic kidney disease period.14
Surgical cure was definedas restoration of serum cal-cium and PTH levels14 throughout the first six months
after surgery. Recurrence was defined when high lev-els of PTH were observed throughout latepost-operative follow-up (one year after surgical procedure) that failed to respond to medical/pharmacological management. Definitive hypoparathyroidism was defined when PTH measurements under 10pg/mL endured one year after parathyroidectomy,withnormalorlowserumcalciumlevels undervitaminDandoralcalciumsupplementation.
Serum ionized calcium (iCa), phosphorus (P), alka-line phosphatase (AP), and intact parathyroid hormone (iPTH) were measured before parathyroidectomy and every six months after surgery in all patients from both groups.
Regardingthefollow-up,patientsfrombothgroupswere followed-up after surgery ona regular basis in the Renal OsteodystrophyUnit,andpatientdatafrommedicalreports wereavailablefor thisstudy.PatientsfromG1 underwent surgeryfrom2000 to2005, whilepatients fromG2 under-wentsurgeryfrom2008to2009.Thus,forsurgicaloutcome analysis,thefirst36 monthswerethe periodselectedfor studyinbothgroups,sinceitwasthelongestperiod avail-ableforG2patients.
Methods
Studydesign
This was a comparative study using a historical control, evaluatingstereomicroscopyincomparisontoconventional macroscopictechniqueinparathyroidtissueselectionin sur-gicaltreatmentofrenalhyperparathyroidism.
This investigation was approved by the institutional ethicscommittee(approvalNo.CEP0234/06)andpatients signed an informedconsentprior totheir inclusionin the study.
Surgicalstrategy
Bilateral cervical exploration with at least four-gland excision confirmed by frozen section examination and/or intra-operativePTH(IO-PTH)measurementwasperformed inall118patients(IO-PTHavailablein100patients).
Removed parathyroid glands were carefully examined in ordertoselect aparathyroidarea(non-nodular region) for implant and cryopreservation. The selected parathy-roidfragmentwasgentlydicedintosmallpiecesmeasuring approximately2.0mm3.Approximately30parathyroid frag-ments were implanted in presternal musculature over a singleareaof1.5cminlength.7Another30fragmentswere
selectedforcryopreservation.Thereasonsforchangingthe grafted area from the forearm to the presternal muscu-lature are relatedto some potential advantages. First, it preservestheforearmforarterio-venousus-fistuladialysisif needed.Second,thepresternalregionisclosetothe cervi-cotomy,exposingthesamesurgicalarea.Third,itallowsfor an easier graft-removal in case of graft-dependent recur-rence;the sternalbone presentsaposterior boundaryfor the grafted tissue, enabling a graft removal under local anestesia.7 Allsurgerieswereperformedby thesame
sur-geoninbothgroupsG1andG2.
Protocolforintraoperativetissueselection
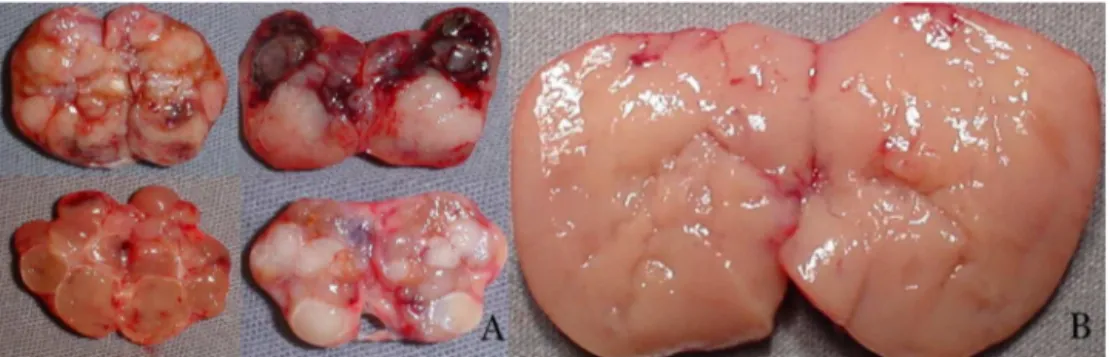
Group 1 --- Conventional technique: tissue selection for autotransplantation based on macroscopic parathyroid observationwasperformedin66patients.Nodular parathy-roid regions were avoided, while hyperplasic non-nodular parathyroid areas were considered eligible for autotrans-plantation(Fig.1).
Group2---Stereomicroscopy:parathyroidtissueselection using Leica Stereo Zoom S8APO Stereomicroscope (Leica Microsystems GmbH --- Wetzlar, Germany) with apochro-matic 8:1zoom, 10---80×magnification, wasperformed in
52patients.Resectedparathyroidglandswerefirstobserved macroscopically, and stereomicroscopic analysis was per-formedthereafter,searchingforthepresenceofstromalfat cellsintheparathyroidglands(Fig.2,arrows).
Biochemistry
Figure1 Macroscopicparathyroid tissue observation:A, nodular parathyroid regionsnoteligible for autotransplantation; B, hyperplasicnon-nodularparathyroidareaeligibleforautotransplantation.
Table1 Pre-operativedataandlaboratoryfindings.
G1(n=66) G2(n=52) SHPT THPT SHPT THPT
n 38 28 29 23
Age 40.0(14---58) 44.0(24---62) 50.7(26---74) 44.4(28---63) Female/male 24/14 14/14 11/18 13/10 Yearsondialysis 7.7(0.6---16) 6.5(2---20) 7.9(3---25) 6.4(0.8---13) Yearsofrenalgraft --- 2.8(0.5---7) --- 3.3(0.4---10) Pre-opiCa 1.36a(1.19---1.83) 1.59(1.42---1.77) 1.41a(1.21---1.59) 1.58(1.41---1.90)
Pre-opiPTH 1618.7(298---2500) 442.2(109---1758) 1810.2(561---3500) 465.8(181---2237)
Referencevalues:iCa=1.20---1.40mmol/L;iPTH=10---65pg/mL. Dataexpressedasmeanandrange.
SHPT,secondaryhyperparathyroidism;THPT,tertiaryhyperparathyroidism;iCa,serumionizedcalcium;iPTH,intactparathyroid hor-mone.
at-test:p<0.05.
Table2 Post-operativemeaniCaandiPTHincuredpatientsinG1-group(conventional).
SHPT THPT
iCa iPTH iCa iPTH 12months (n=34) 1.17 79.8 (n=25) 1.25 58.4 24months (n=29) 1.22 86.0 (n=19) 1.22 64.7 36months (n=21) 1.19 83.0 (n=16) 1.22 78.5
Referencevalues:iCa=1.20---1.40mmol/L;iPTH=10---65pg/mL. Dataexpressedasmeans.
SHPT,secondaryhyperparathyroidism;THPT,tertiaryhyperparathyroidism;iCa,serumionizedcalcium;iPTH,intactparathyroid hor-mone.
measuredusingtheElecsysPTHImmunoassay(Elecsys1010 System; Roche --- Mannheim, Germany) and was available for100patients(84.7%).Thetimerequiredtoperformthe assayisnineminutesandreferencevaluesare10---70pg/mL. Peripheral venous blood sample (4.0mL) was obtained immediatelyafterinductionofanesthesiaand20minafter removalofallparathyroidglands.15---17
Total serum calcium, phosphorus, total alkaline phos-phatase, and creatinine were measured by means of standard automatic assays (Hitachi 912 --- Roche). Serum ionized calcium was measured by using an ion-specific electrode (AVL 9180 Electrolyte Analyzer --- Roswell, Georgia, United States). Parathyroid hormone in ambu-latory conditions was measured by immunometric assay
(Immulite; Siemens --- São Paulo, Brazil: reference values 10---65pg/mL).
All removed parathyroid tissue underwent complete histopathologyanalysis.
Results
Pre-operativedataandlaboratory findingsaredepictedin
Table1.
Meanpost-operativeiPTHandiCaserummeasurements during thefollow-up of cured patientsin both groups are showninTables2and3.
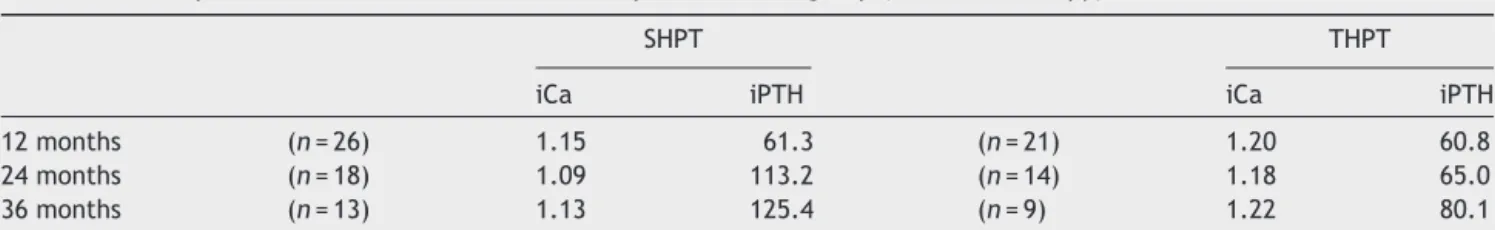
Table3 Post-operativemeaniCaandiPTHincuredpatientsinG2-group(stereomicroscopy).
SHPT THPT
iCa iPTH iCa iPTH 12months (n=26) 1.15 61.3 (n=21) 1.20 60.8 24months (n=18) 1.09 113.2 (n=14) 1.18 65.0 36months (n=13) 1.13 125.4 (n=9) 1.22 80.1
Referencevalues:iCa=1.20---1.40mmol/L;iPTH=10---65pg/mL. Dataexpressedasmean.
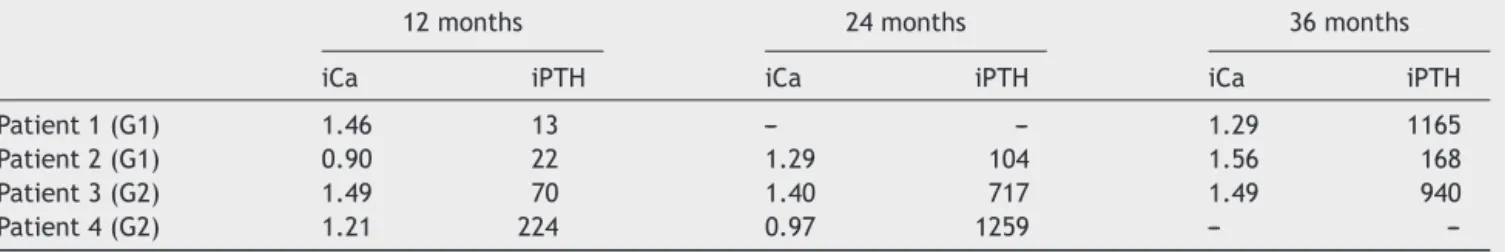
Table 4 Graft-dependent recurrence in patients from G1 (2/66) --- conventional technique, and from G2 (2/52) ---stereomicroscopy.
12months 24months 36months iCa iPTH iCa iPTH iCa iPTH Patient1(G1) 1.46 13 --- --- 1.29 1165 Patient2(G1) 0.90 22 1.29 104 1.56 168 Patient3(G2) 1.49 70 1.40 717 1.49 940 Patient4(G2) 1.21 224 0.97 1259 ---
---Referencevalues:iCa=1.20---1.40mmoL/L;iPTH=10---65pg/mL. iCa,serumionizedcalcium;iPTH,intactparathyroidhormone.
Persistent hyperparathyroidism due to supernumerary parathyroidglandsnotrecognizedduringsurgicalprocedure wasobservedintwopatients,onefromeachgroup;those patientswereexcludedfromthestudy.
Definitive hypoparathyroidism was observed in 7/118 (5.9%)patients,4/66(6%)inG1,and3/52(5.7%)inG2.
Graft-dependent recurrence was observed in 4/118 (3.3%) patients, two in each group (G1, 2/66; 3.0% and G2,2/52;3.8%)(Table4).Allgraft-dependentrecurrences wereobservedindialysispatients.Noneoccurredin kidney-graftedpatients.
Discussion
SurgeryforrenalhyperparathyroidismisperformedinBrazil inrelativelyfewmedicalcenters,sometimesleadingtolong waiting times and, consequently,to worse clinical condi-tions at the time of surgery. Throughout the years, the authors have observed a worsening in medical conditions among renal patients at the time of surgery, when com-paringpatientsfromG1(surgeriesperformedfrom04/2000 to 05/2005) to G2 (surgeries performed from03/2008 to 10/2009).AsobservedinSHPTpatientsfromG2,serum cal-ciumlevels werehigherthan thoseseen inSHPTpatients fromG1(t-test;p<0.05).Thisfindingisinagreementwith patientswithamore severediseaseand,moreover, these are indicators that patients in G2 underwent surgery in a worse condition. Thus, the apparently similar surgical resultsingraft-dependentrecurrenceobservedbetweenG1 andG2(tworecurrencesineachgroup)couldbeassessedas apositiveoutcomeforstereomicroscopy.The moresevere disease observed in G2 may be the explanation for the finding of a similar recurrence in both groups. Since the macroscopicexaminationprotocolusedinG1wasperformed by the same surgeon that also supervised the stereomi-croscopyinG2,afaircomparisoncanbeperformed.
From the 118 overall patients, graft-dependent recur-rence was observed only in four (3.3%). This can be considered a low graft-dependent recurrence rate com-pared to literature data.18---20 Considering the gravity of
the illness observed in these patients, the experienceof the surgeon probably contributed to such a positive out-come.
The clearly abnormal macroscopic findings observed in removed parathyroid indicate the severity of the ill-nessandimpose an especiallydifficult challengein tissue
selection. The effort for finding eligible areas for auto-transplantationamongabnormalparathyroidglandsmakes stereomicroscopyaninterestingtoolforitsstandardization. Thesearchforstromalfatcells aspreviouslydescribedby Neyer et al.12 may provide a reproducible technique for
tissueselectionin attempts toreachlowgraft-dependent recurrencesrates,evenforsurgeonsnotsoexperiencedin parathyroidsurgeries.
Another important observation is that all graft-dependent recurrences were in dialysis patients. None occurred in kidney-grafted patients. It is probable that thecontinuous exposureof thegrafted parathyroidtissue touremicenvironmentmay bethe main driverfor tumor recurrenceinpatientsunderlong-termdialysistreatment, independentofthesurgicaltechniqueemployed.
Post-operativePTH measurementsduringthefollow-up ofcuredpatientsweresimilarinG1andG2,aswere defini-tivehypoparathyroidismrates.
Asmentionedabove,persistenthyperparathyroidismdue tosupernumerary parathyroid glands not recognized dur-ingsurgical procedure wasobserved in twopatients, one in each group and those patients were excluded from the study. Occurrence of supernumerary and/or ectopic parathyroid glands is more frequent among chronic kid-neyfailurepatients,21 andthispresentsan importantand
additionalchallengein surgical treatment of renal hyper-parathyroidism.
Limitationsarerelatedtotheheterogeneous character-istics of renal patients enrolled in this study, with their particularclinicalandlaboratory findings,andconsidering themasagrouppresentsarealchallenge,especiallywhen ahistoricalcontrolisused.Anotherlimitationisrelatedto theseverityofthesepatients:themarkedillnessand long-lastingrenalconditionmakesthemaspecialgroup,whose outcomewould notbeexpectedin ordinarypatients with chronicrenaldisease.Inaddition,levelsof25-OHvitaminD werenotavailableinthisstudy.
Conclusion
Funding
ThisstudywassupportedbyFAPESP:N◦ 07/51056-5.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Monchik JM, Bendinelli C, Passero Jr MA, Roggin KK. Sub-cutaneous forearmtransplantation ofautologousparathyroid tissue in patients with renal hyperparathyroidism. Surgery. 1999;126:1152---8.
2.WellsJrSA,GunnellsJC,ShelburneJD,SchneiderAB,Sherwood LM.Transplantationoftheparathyroidglandsinman:clinical indicationsandresults.Surgery.1975;78:34---44.
3.Wells Jr SA, Ross 3rdAJ, Dale JK, GrayRS. Transplantation oftheparathyroidglands:currentstatus.SurgClinNorthAm. 1979;59:167---77.
4.PackmanKS, DemeureMJ.Indicationsfor parathyroidectomy and extent of treatmentfor patients withsecondary hyper-parathyroidism.SurgClinNorthAm.1995;75:465---82.
5.SokollLJ,DrewH,UdelsmanR.Intraoperativeparathyroid hor-mone analysis:astudyof200consecutivecases.ClinChem. 2000;46:1662---8.
6.Weber KJ, Misra S, Lee KJ, Wilhelm SW, DeCresce R, Prinz RA.IntraoperativePTHmonitoringinparathyroidhyperplasia requiresstrictercriteriaforsuccess.Surgery.2004;136:1154---9. 7.SantosRO,OheM,CarvalhoABC,NevesMC,KuniiI,Lazaretti CastroM,etal.Totalparathyroidectomywithpresternal intra-muscularautotransplantationinrenalpatients:aprospective studyof66patients.JOsteoporos.2012;2012[serialonline], ArticleID631243,6pp.
8.TominagaY,UchidaK,HabaT,KatayamaA,SatoT,HibiY,etal. Morethan 1,000cases oftotalparathyroidectomywith fore-armautograftforrenalhyperparathyroidism.AmJKidneyDis. 2001;384Suppl.1:S168---71.
9.TominagaY,MatsuokaS,SatoT.Surgicalindicationsand pro-ceduresofparathyroidectomyinpatientswithchronickidney disease.TherApherDial.2005;9:44---7.
10.Hampl H, Steinmuller T, Stabell U, Klingenberg HJ, Schnoy N, Neuhaus P. Recurrent hyperparathyroidism after total parathyroidectomy and autotransplantation in patients with
long-term hemodialysis. Miner Electrolyte Metab. 1991;17: 256---60.
11.Arnold A, Brown MF, Ure˜na P, Gaz RD,Sarfati E, Drüek TB. Monoclonality of parathyroid tumors in chronic renal fail-ure and in primary parathyroid hyperplasia. J Clin Invest. 1995;95:2047---53.
12.Neyer U, Hoerandner H, Haid A, Zimmermann G, Niederle B. Total parathyroidectomy with autotransplantation in renal hyperparathyroidism:low recurrence rates after intra-operativetissue selection.Nephrol DialTransplant.2002;17: 625---9.
13.NiederleB,HorandnerH,RokaR,WoloszczukW.Morphologic andfunctionalstudiestopreventgraft-dependentrecurrence inrenalosteodystrophy.Surgery.1989;106:1043---8.
14.KidneyDisease:ImprovingGlobalOutcomes(KDIGO)CKD-MBD WorkGroup:KDIGOclinicalpracticeguidelineforthe diagno-sis, evaluation, preventionand treatment ofchronic kidney disease-mineralandbonedisorder(CKD-MBD).KidneyIntSuppl. 2009;(113):S1---130.
15.OheMN,SantosRO,KuniiIS,CarvalhoAB,AbrahãoM,Cervantes O,etal.Usefulnessofarapidimmunometricassayfor intraop-erativeparathyroidhormone measurements.Braz JMedBiol Res.2003;36:715---21.
16.OheMN,SantosRO,KuniiIS,CarvalhoAB,AbrahãoM,Cervantes O,etal.UsefulnessofintraoperativePTHmeasurementin pri-maryand secondary hyperparathyroidism:experience in 109 patients.ArqBrasEndocrinolMetabol.2006;50:869---75. 17.OheMN,SantosRO,KuniiIS,CarvalhoAB,AbrahãoM,NevesMC,
etal.IntraoperativePTHcutoffdefinitiontopredictsuccessful parathyroidectomy in secondary and tertiary hyperparathy-roidism.BrazJOtorhinolaryngol.2013;79:494---9.
18.GagnéER,Ure˜naP,Leite-SilvaS,ZingraffJ,ChevalierA,Sarfati E,etal.Short-andlong-termefficacyoftotal parathyroidec-tomy with immediate autografting compared with subtotal parathyroidectomyinhemodialysispatients.JAmSocNephrol. 1992;3:1008---17.
19.HigginsRM,RichardsonAJ,RatcliffePJ,WoodsCG,OliverDO, MorrisPJ.Totalparathyroidectomyaloneorwithautograftyfor renalhyperparathyroidism?QJMed.1991;79(288):323---32. 20.TominagaY,NuomanoM,TanakaY,UchidaK,TakagiH.
Surgi-caltreatmentofrenalhyperparathyroidism.SeminSurgOncol. 1997;13:87---96.