179
Traumatic airway disruption in a child:
a diagnostic challenge
Andréa Maria Cordeiro Ventura,1 Patrícia Freitas Góes,1 José Pinhata Otoch,2 José Carlos Fernandes3
0021-7557/05/81-02/179
Jornal de Pediatria
Copyright © 2005 by Sociedade Brasileira de Pediatria
C
ASER
EPORTAbstract
Objective: To report a case of airway disruption in a child victim of blunt thoracic trauma due to falling off a sink.
Description: Descriptive case report. A 34-month old boy victim of thoracic trauma was seen at the pediatric intensive care unit of a university hospital. Plain chest radiograph, thoracic computed tomography, bronchoscopy, thoracotomy, antibiotics, hemodynamic and respiratory support were performed. Plain chest radiograph, thoracic computed tomography and bronchoscopy were performed in order to arrive at a precise diagnosis of traumatic airway disruption associated with pulmonary contusion, pneumothorax, mediastinal and subcutaneous emphysema. The patient underwent thoracotomy for surgical repair of an almost complete disruption of the left main bronchus. Antibiotics and ventilatory support contributed to a favorable outcome without medium-term sequelae.
Comments: Children presenting with thoracic trauma must be investigated for uncommon, but potentially lethal injuries, such as tracheobronchial disruption, particularly in cases where there is strong clinical evidence. Diagnostic workup should be optimized with plain chest radiograph and thoracic computed tomography, while bronchoscopy will confirm the definitive diagnosis.
J Pediatr (Rio J). 2005;81(2):179-82: Thoracic trauma, tracheobronchial disruption, pneumothorax, mediastinal emphysema, subcutaneous emphysema, children.
1. MSc. Assistant physician, Pediatric Intensive Care Unit, Hospital Universitário, Universidade de São Paulo (USP), São Paulo, SP, Brazil. 2. PhD. Physician responsible for the Surgery Service of Hospital
Universitário, USP, São Paulo, SP, Brazil.
3. Physician responsible for the Pediatrics Intensive Care Unit of Hospital Universitário, USP, São Paulo, SP, Brazil.
Manuscript received Jun 02 2004, accepted for publication Sep 08 2004.
Suggested citation: Ventura AM, Góes PF, Otoch JP, Fernandes JC. Traumatic airway disruption in a child: a diagnostic challenge. J Pediatr (Rio J). 2005;81:179-82.
Introduction
Nowadays, traumatic lesions of whatever type are a significant cause of morbidity and mortality in children from 1 to 14 years of age. Of all the different types of possible injury, thoracic traumas are a cause for extreme concern because of the elevated mortality they cause. Blunt thoracic trauma was recorded in just 5-12% of admissions for traumas in the pediatric age group in the United States.1,2 The lethality associated with these admissions, however, was significantly elevated. In isolation, thoracic trauma was associated with a 5% mortality rate in children1 and was the
direct cause of death in 14% of a cohort of 25,301 pediatric trauma victims in the United States.2 If other organs were also traumatized, mortality was significantly increased, reaching 20% for abdominal and thoracic traumas in association and 35% for head and thoracic trauma and 39% for abdominal, thoracic and head trauma.1
Blunt thoracic trauma was the principal type of injury, caused by automobile accident, being run down, abuse or falls. Blunt thoracic trauma occurred in 81% of 79 children in a study undertaken in the United States,3 in 60% of 225 children in a study conducted in Turkey4 and 96% of 87 children in a study conducted in Saudi Arabia.5
180 Jornal de Pediatria - Vol. 81, No.2, 2005 Traumatic airway disruption in child Ventura AMC et alii
0.5-2.8% of thoracic traumas and presented elevated mortality (15-30%).7-10
We present the case of a child who suffered thoracic trauma in falling off a sink and who exhibited commonly encountered injuries such as pulmonary contusion and pneumothorax, but in association with a rare injury, which was a ruptured airway.
Case description
A 34-month-old, male child suffered a fall from on top of a sink while playing. Immediately after the accident the family found him, still conscious. He complained of chest pain and difficulties talking and breathing. At this point a swelling had already been noted in the region of the throat. One hour after the accident, while being seen in the emergency room, he exhibited intense respiratory difficulty (cyanosis breathing room air, inspiratory stridor, intense tachydyspnea and moaning). He appeared sleepy, presented scratches to the lower third of the sternum and subcutaneous emphysema affecting the thorax, the cervical region, extending up to his face. Tracheal intubation was decided upon because of respiratory insufficiency. After this procedure, chest x-ray showed right-side pulmonary contusion and bilateral pneumomediastinum. The child then underwent thoracic drainage, and fluids replacement was started with saline due to poor peripheral perfusion, weak peripheral pulse and tachycardia (HR = 170 bpm). After these initial treatments he was transferred to the Pediatric ICU at the of the Universidade de São Paulo Teaching Hospital.
On admission to the ICU the patient presented intense respiratory distress, cutaneous-mucosal pallor and extensive subcutaneous emphysema all the way from the scalp to the start of both thighs. Vital signs were BP = 130 x 82 (M = 104); HR = 144 bpm; RR = 25 brpm; T = 37.4 °C; SO2 = 70% at FiO2 = 1%. The segmental examination showed thoracic drainage with bilateral drainage tubes that did not bubble or oscillate, reduced respiratory noises with
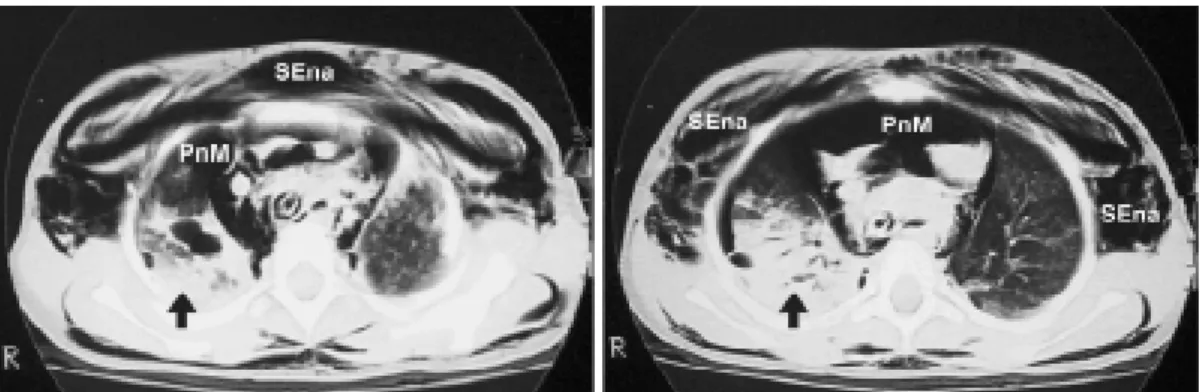
crepitant rales on the right. Hemodynamics were as follows: sounds were rhythmic and subdued, capillary filling was slow and peripheral pulses weak. The initial procedure was to connect the patient to a mechanical ventilator, establish central venous access, initiate volemic replacement, sedation, anesthesia and H2 blocker for prophylaxis of gastric mucosa injuries. The patient then underwent ultrasound and simple abdominal x-ray, echocardiogram and cranial tomography, which were normal. Tomography of the thorax revealed a posterior displacement of the trachea and bronchi sources. The primary left bronchus was compressed close to the carina, there was voluminous pneumomediastinum at the anterior mediastinum and the pulmonary parenchyma presented areas of segmental consolidation and air bronchograms, primarily on the right, the thoracic drains were visible in an apparently virtual pleural cavity and significant subcutaneous emphysema could also be observed (Figure 1). Endoscopic airway examination was requested and blood was found in the airways.
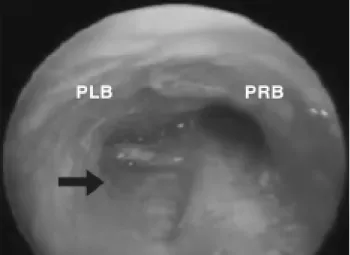
After initial stabilization, further respiratory endoscopy revealed a partial rupture of the primary left bronchus close to the carina together with moderate tracheobronchitis (Figure 2). Thoracotomy was performed on the fourth day in hospital because of concerns that infectious processes could interfere with the sutures healing and encourage stenosis of the anastomosis. The patient had been febrile since the day he was admitted and C-reactive protein values were 96 on the first day and 131 on the fourth, despite antibiotic therapy (clindamycin and ceftriaxone). Surgical findings agreed with the endoscopy and the near-total rupture of the left primary bronchus was repaired.
The patient was maintained on mechanical ventilation, with progressively lower ventilation requirements; the thoracic drains showed no evidence of fistula, and both the pneumomediastinum and subcutaneous emphysema receded. The patient was extubated 2 days after the surgical operation. The thoracic drains were removed 24 hours after extubation. Endoscopic reevaluation, on the 14th day after
Figure 1 - Endoscopy imaging showing the airway rupture (arrow)
181 Jornal de Pediatria - Vol. 81, No.2, 2005
surgery showed a reduction in the lumen of the left main bronchus, although with no clinical repercussions. The patient was discharged from the ICU 24 days after admission and is currently been followed-up in outpatients.
Discussion
We have described the case of a child who had suffered a thoracic trauma and who presented clinical signs suggestive of airway rupture, which was confirmed after a second endoscopic examination. The case has several different important features for discussion, but we would like to concentrate on the diagnosis of the rare condition.
One fact that may have contributed to the difficulty in confirming the diagnosis is that a ruptured airway is not a common finding with pediatric thoracic traumas. In a literature review covering 1,653 thoracic trauma patients, 225 of whom were children (13.6%), not one case exhibited a ruptured airway.4 Similarly, Peclet et al. reported that 2,086 children were admitted for trauma. Thoracic trauma occurred in 104 cases (4.4%), and tracheobronchial rupture was not observed in any of the patients.1 Tracheobronchial ruptures are ten times less frequent in children than in adults.11 Thoracic traumas in children have a singular feature which is that they have a more complacent thoracic wall, which permits external forces to be transmitted directly to mediastinal structures with no external signs of trauma.12,13 Thus, the fractured ribs that are present in 90% of adults with ruptured trachea or bronchi are present in less than 24% of children suffering the same type of trauma.13 This characteristic may contribute to delayed diagnosis and consequent elevated morbidity and mortality. Diagnosis is thus dependent on strong suspicion which is based on the mechanism of the trauma, and clinical radiological and bronchoscopic findings.
There are several mechanisms involved in airway injuries secondary to thoracic trauma: compression of the thorax with lateral displacement of the lungs, producing traction on the trachea which is fixed to the carina;14 sudden increase in intraluminal pressure, creating a pressure gradient between the airway lumen and the mediastinum with a rupture close to the carina;14,15 rapid deceleration producing a pressure difference between fixed and unfixed tissue which lead to torsion of the hilus and rupture of the bronchus close to the carina14,15 and crushing of the thorax with compression of the airway between the sternum and spine. Knowledge of these pathophysiologic mechanisms is of interest in the sense that it alerts physicians to those injuries that can occur as a result of a thoracic trauma.
The occult nature of traumatic airway rupture is also due to the fact that clinical signs may be absent in up to 10% of cases16 and when present have low specificity and, in the presence of other associated injuries may not be properly valued. The majority of patients present air mediastinum, although more distal airway ruptures may lead to air leaking into the pleural cavity, consequently, to hypertensive pneumothorax.17 Dyspnea with stridor, cyanosis, chest pain, hemoptysis, pneumomediastinum and pneumothorax that are refractory to thoracic drainage and subcutaneous emphysema are generally present. In cases of complete rupture of the main bronchus, the lung will collapse.17 In contrast, when the rupture is minimal, the injured area may become covered by mediastinal t i s s u e , s o t h a t s u b c u t a n e o u s e m p h y s e m a a n d p n e u mo me d i a s t i n u m o n l y b e c o me e v i d e n t a f t e r mechanical ventilation. In a series of nine cases of tracheobronchial rupture, Nishiumi et al. observed that hemoptysis was present in all patients.15 Chu & Chen reported that up to 60% of patients with airway trauma presented dyspnea, 69% subcutaneous emphysema, 43% pneumomediastinum and 69% had pneumothorax.16 Notwithstanding, other associated injuries may contribute to clinical findings. The presence of cyanosis, for example, may also depend of the quantity of intrabronchial blood and on the severity and extension of pulmonary contusion.15 In the case described here, attention was attracted by dyspnea, stridor and subcutaneous emphysema with rapid onset and progression. The respiratory distress with very early onset might have been due to an accumulation of secretions and/or blood in the airway, injured mucosa or cartilage with interrupted continuity or, even, compression of the airway by mediastinal or subcutaneous emphysema.16
Imaging examinations were used in this case to help with the diagnosis of injuries associated with the thoracic trauma. Simple chest x-ray can diagnose the presence of fractured ribs,18 find early evidence of abnormalities compatible with pulmonary contusion19 and even pleural cavity and mediastinum involvement. Computerized tomography can be useful for the evaluation and management of pulmonary contusion. It has been demonstrated that mechanical ventilation is necessary when more than 28% of the pulmonary parenchyma, and is not necessary when pulmonary involvement is less than 18%.20
Figure 2 - Endoscopy imaging showing the airway rupture (arrow) PLB = primary left bronchus; PRB = primary right bronchus
182 Jornal de Pediatria - Vol. 81, No.2, 2005
References
1. Peclet MH, Newman KD, Eichelberger MR, Gotschall CS, Garcia VF, Bowman LM Thoracic trauma in children: an indicator of increased mortality. J Pediatr Surg. 1990;25:961-5.
2. Cooper A, Barlow B, Di Scala C, String D. Mortality and truncal injury: the pediatric perspective. J Pediatr Surg. 1994;29:33-8. 3. Peterson RJ, Tepas JJ 3rd, Edwards FH, Kissoon N, Pieper P, Ceithaml EL. Pediatric and adult thoracic trauma: age-related impact on presentation and outcome. Ann Thorac Surg. 1994;58:14-8.
4. Ceran S, Sunam GS, Aribas OK, Gormus N, Solak H. Chest trauma in children. Eur J Cardiothorac Surg. 2002;21:57-9. 5. Crankson SJ, Fischer JD, Al-Rabeeah AA, Al-Jaddan SA. Pediatric
thoracic trauma. Saudi Med J. 2001;22:117-20.
6. Holmes JF, Sokolove PE, Brant WE, Kuppermann N. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med. 2002;39:492-9. 7. Bertelsen S, Howitz P. Injuries of the trachea and bronchi.
Thorax. 1972;27:188-94.
8. Calhoon JH, Grover FL, Trinkle JK. Chest trauma. Approach and management. Clin Chest Med. 1992;13:55-67.
9. Meislin HW, Iserson KV, Kaback KR, Kobernick M, Sanders AB, Seifert S. Airway trauma. Emerg Med Clin N Am. 1983;1:295-312. 10. Devitt JH, Boulanger BR. Lower airway injuries and anaesthesia.
Can J Anaesth. 1996;43:148-59.
11. Kaptanoglu M, Dogan K, Nadir A, Gonlugur U, Akkurt I, Seyfikli Z, et al. Tracheobronchial rupture: a considerable risk for young teenagers. Int J Pediatr Otorhinolaryngol. 2002;62:123-8. 12. Balci AE, Eren N, Eren S, Ulku R. Surgical treatment of
post-traumatic tracheobronchial injuries: 14-year experience. Eur J Cardiothorac Surg. 2002;22:984-9.
13. Grant WJ, Meyers RL, Jaffe RL, Johnson DG. Tracheobronchial injuries after blunt chest trauma in childrenhidden pathology. J Pediatr Surg. 1998;33:1707-11.
14. Slimane MA, Becmeur F, Aubert D, Bachy B, Varlet F, Chavrier Y, et al. Tracheobronchial ruptures from blunt thoracic trauma in children. J Pediatr Surg. 1999;34:1847-50.
15. Nishiumi N, Maitani F, Yamada S, Kaga K, Iwasaki M, Inokuchi S, et al. Chest radiography assessment of tracheobronchial disruption associated with blunt chest trauma. J Trauma. 2002;53:372-7.
16. Chu CP, Chen PP. Tracheobronchial injury secondary to blunt chest trauma: diagnosis and management. Anaesth Intensive Care. 2002;30:145-52.
17. Harvey-Smith W, Bush W, Northrop C. Traumatic bronchial rupture. Am J Roentgenol. 1980;134:1189-93.
18. Bliss D, Silen M. Pediatric thoracic trauma. Crit Care Med. 2002;30 Suppl:S409-15.
19. Bonadio WA, Hellmich T. Post-traumatic pulmonary contusion in children. Ann Emerg Med. 1989;18:1050-2.
20. Wagner RB, Crawford WO Jr, Schimpf PP, Jamieson PM, Rao KC. Quantitation and pattern of parenchymal lung injury in blunt chest trauma. Diagnostic and therapeutic implications. J Comput Tomogr. 1988;12:270-81.
21. Wan YL, Tsai KT, Yeow KM, Tan CF, Wong HF. CT findings of bronchial transection. Am J Emerg Med. 1997;15:176-7. 22. Iwasaki M, Kaga K, Ogawa J, Inoue H, Shohtsu A. Bronchoscopy
findings and early treatment of patients with blunt tracheo-bronchial trauma. J Cardiovasc Surg. 1994;35:269-71. 23. Kiser AC, OBrien SM, Detterbeck FC. Blunt tracheobronchial
injuries: treatment and outcomes. Ann Thorac Surg. 2001;71:2059-65.
Correspondence:
Rua Jacques Felix, 96/94, Vila Nova Conceição CEP 04509-000 São Paulo, SP
Brazil
Tel.: +55 (11) 3039.9248 / 3039.9458 / 3044.7179 E-mail: amgcordeiro@uol.com.br
The most common radiographic findings when the airway has been injured, according to Devitt & Boulanger,10 include pneumothorax, mediastinal emphysema and subcutaneous emphysema, which were diagnosed in this case. In a series of nine cases Nishiumi et al. observed that pneumothorax was present in all seven patients with complete or incomplete rupture of the central airway and subcutaneous emphysema in all six cases of incomplete central airway rupture. In contrast, injuries to the distal airway may not be accompanied by air leakage, as two cases demonstrated.15 Atelectasis of segments or lobes and pulmonary collapse are other findings that can be associated with airway trauma. Chest tomography can be of help in defining the location of damage. According to Wan et al., the presence of a shadow indicative of peribronchial hematoma associated with mediastinal emphysema is an important finding in airway rupture.21
Bronchoscopic examination establishes the definitive diagnosis of airway rupture in addition to locating the position and extension of injury. However, it is important to consider that, because of the urgency of clinical presentation, there may not be enough time available for endoscopic analysis and that surgical intervention may be indicated based on clinical presentation and x-ray findings.15 In certain cases, the injury may be concealed by blood and mucus making it difficult to confirm diagnosis.22
In this case, it was not possible to confirm diagnosis with the initial endoscopic evaluation, probably because of blood in the airway. Despite the first examination having been inconclusive it was decided that a second was necessary because of the clinical progression and persistent pneumomediastinum, despite thoracic drainage and pulmonary collapse. Kiser et al. after a retrospective analysis of 265 patients report that diagnosis was established in an average of 9 days post-trauma and that surgical intervention took place after an average of 25 days.23 Of the 122 patients with injuries to the right main bronchus, the average number of days to diagnosis was just 1 day (variation = 1-21), while for those patients with injuries to the main left bronchus, the average time to diagnosis was 30 days (variation = 1-23 days).
We conclude that in the event of thoracic trauma in children, the diagnostic search for uncommon, but potentially lethal injuries such as airway rupture, must be incessant, particularly in those patients with strong clinical evidence. Diagnostic aids should include simple chest x-ray, chest tomography and endoscopic examination, which establishes the definitive diagnosis.