REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Post
analysis
simulated
correlation
of
the
El-Ganzouri
airway
difficulty
score
with
difficult
airway
Ruggero
M.
Corso
a,∗,
Davide
Cattano
b,
Matteo
Buccioli
a,
Elisa
Carretta
c,
Stefano
Maitan
aaDepartmentofEmergency,AnaesthesiaandIntensiveCareSection,‘‘G.B.Morgagni-Pierantoni’’Hospital,Forlì,Italy bDepartmentofAnesthesiology,TheUniversityofTexasMedicalSchoolatHouston,Houston,USA
cBiostatisticsandClinicalTrialsUnit,InstituteScientificoRomagnoloperloStudioelaCuradeiTumori(IRST),Meldola,Italy
Received24August2014;accepted3September2014 Availableonline27November2014
KEYWORDS
Difficultairway;
Predictivescore;
Sleepapnea
Abstract
Background: Difficult airway (DA) occurs frequently (5---15%) in clinical practice. The El-Ganzouri Risk Index (EGRI) has a high sensitivity for predicting a difficult intubation (DI). Howeverdifficultmaskventilation(DMV)wasneverincludedintheEGRI.SinceDMVwasnot includedintheEGRIassessment,andobstructivesleepapnea(OSA)isalsocorrelatedwithDMV, astudycorrelatingthepredictionofDAandOSA(identifiedbySTOP-Bangquestionnaire,SB) seemedimportant.
Methods:Weaccessedadatabasepreviouslycollectedforapostanalysissimulationofthe air-waydifficultypredictivityoftheEGRI,associatedwithnormalanddifficultairway,particularly DMV.Assecondaryaim, wemeasuredthecorrelationbetweentheSBpredictionsystemand DA,comparedtotheEGRI.
Results:Atotalof2747patientswereincludedinthestudy.TheproportionofpatientswithDI was14.7%(95%CI13.4---16)andtheproportionofpatientswithDMVwas3.42%(95%CI2.7---4.1). TheincidenceofDMVcombinedwithDIwas(2.3%).TheoptimalcutoffvalueofEGRIwas3. EGRIregisteredalsoanhigherabilitytopredictDMV(AUC=0.76(95%CI0.71---0.81)).Addingthe SBvariablesinthelogisticmodel,theAUCincreaseswiththeinclusionof‘‘observedapnea’’ variable(0.83vs.0.81,p=0.03).TheareaundertheROCcurveforthepatientswithDIand DMVwas0.77(95%CI0.72---0.83).
Conclusions:ThisstudyconfirmsthattheincidenceofDAisnotnegligibleandsuggeststheuse oftheEGRIassimplebedsidepredictivescoretoimprovepatientsafety.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:rmcorso@gmail.com(R.M.Corso).
http://dx.doi.org/10.1016/j.bjane.2014.09.003
PALAVRAS-CHAVE
Viaaéreadifícil;
Escorepreditivo;
Apneiadosono
Correlac¸ãosimuladaapósanálisedosescoresdeEl-Ganzouriparaviaaéreadifícil
Resumo
Justificativa: Aviaaéreadifícil(VAD)ocorrecomfrequência(5-15%)napráticaclínica.OÍndice deRiscodeEl-Ganzouri(EGRI)temumaaltasensibilidadeparapreverintubac¸ãodifícil(ID). Noentanto,aventilac¸ãodifícilviamáscara(VDM)nuncafoiincluídanoEGRI.ComoaVDMnão foiincluídanaavaliac¸ãoEGRIeaapneiaobstrutivadosono(AOS)tambémestácorrelacionada comaVDM,umestudocorrelacionandoaprevisãodaVADeAOS(identificadapeloquestionário STOP-Bang,SB)pareceuimportante.
Métodos: Nósacessamosumbancodedadospreviamentecoletadosparasimularumaanálise posteriordaprevisibilidadedoEGRIparaviaaéreadifícil,associadoàviaaéreanormaledifícil, particularmente VDM.Comoobjetivosecundário,avaliamosacorrelac¸ãoentreosistemade previsãodoSBedaVAD,emcomparac¸ãocomoEGRI.
Resultados: Nototal,2.747pacientesforamincluídosnoestudo.Aproporc¸ãodepacientescom IDfoide14,7%(ICde95%;13,4-16)eaproporc¸ãodepacientescomVDMfoide3,42%(ICde 95%2,7-4,1).AincidênciadaVDMcombinadacomadeIDfoide2,3%.Ovalordecorteideal dedoEGRIfoi3.EGRItambémregistrouumacapacidademaiordepreverVDM(ASC=0,76(IC de95%;0,71-0,81)).Ao somarasvariáveisdoSBnomodelologístico,aASCaumentacoma inclusãodavariável‘‘apneiaobservada’’(0,83vs.0,81,p=0,03).AáreasobacurvaROCpara ospacientescomIDeVDMfoide0,77(ICde95%;0,72-0,83).
Conclusões: EsteestudoconfirmaqueaincidênciadeVADnãoédesprezívelesugereousodo EGRIcomoumescoredecabeceirapreditivosimplesparamelhoraraseguranc¸adopaciente. ©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Difficultairway(DA),ingeneralasdifficultytosecurean
air-wayandventilateforoptimalpatient’soxygenation,occurs
frequently(5---15%)inclinicalpractice,howevera
challeng-ingdifficult that couldresultsin morbidityor mortalityis
notsofrequentyetitisfatal.1,2Theabilitytoforeseea
seri-ousdifficultyinanefficientmanner wouldbeideal3---6:but unfortunatelymostofthetestsutilizedforpredictionfails toreachhighsensitivityandhighpositivepredictedvalue: thepoortestsperformancepromptedtoquestionthevalue ofavailablebedsidescreeningtestsaspointlessexercise.7 Indeedtherehasbeenachangeinpractice,8and, serendipi-tousornot,theNAP4studyrecentlyshowedpoorassessment isamajorfactorcontributingtoairwaydisasters.1The mul-tivariateriskindexdevelopedbyEl-Ganzouriandcoworkers (EGRI)9 involves the analysisof six parameterscommonly performedduringthepreoperativeevaluationandincludes a history of DA. Each variable is assigned a score (from 0 to 1), a score ≥4 has a high sensitivity for predicting a difficultintubation (DI).Howeverdifficult mask ventila-tion was never included in the EGRI scoring. Since DMV wasnotincluded in theEGRI assessment,and obstructive sleepapnea(OSA),10,11isalsocorrelatedwithDMV,astudy correlatingthepredictionofDAandOSA,lookingatthe out-comesofDMVaswellDIseemedimportant.TheSTOP-Bang (SB)questionnaireisacommonscreeningtestusedforthis aim,patientsidentifiedashighriskforOSAatthe question-nairebeingalsoathighriskforDA.Basedonthehypothesis that El-Ganzouritest is valuable regardless of the airway technique, but based onthe definitionof difficult airway
utilized,weaccessedadatabasepreviouslycollected10 for apostanalysissimulationoftheairwaydifficulty predictiv-ityoftheEGRI,associatedwithnormalanddifficultairway, particularlyDMV.Assecondary aim,wealsomeasuredthe correlationbetweentheSBpredictionsystemanddifficult airway,comparedtotheEGRI.
Methods
headpositionandexternallaryngealmanipulationresulting in: (a) difficult laryngoscopy, defined as being character-izedby the impossibilityof obtaining a viewof the vocal cords even after the best external laryngeal manipula-tion;(b) necessity of repeatedattempts; (c) necessity of non standard devices and/or procedures; (d) withdrawal andprocedure re-planning.Accordingly,a singlerepeated attemptorswitchtoadifferentbladequalifiesasdifficult intubation.Standard equipmentis specified asthe Macin-toshlaryngoscopeandsimpleendotrachealtube; allother devices,suchasvideolaryngoscopesorprocedures,suchas theuseofsupraglotticairwaydevicesasaconduitfor tra-chealintubation, aredefined asnonstandard.DMV occurs whenevertherequiredtidalvolumecannotbeadministered tothe patientunless anyairway device or external help, standardprocedurewithdrawalorintubation.Nogradingof DMVwasrecorded.We adopted thecut-offof ≥5to clas-sifypatientsasathighorlowriskofhavingOSAasrecently suggested.13
Statistical
analysis
Dataarepresentedusingdescriptivestatistics(mean±SD, median(range)andpercentage).Continuousvariableswere compared using the Wilcoxon---Mann---Whitney test. Chi-squared or Fisher’sexact tests were used for categorical variables.Toassess thediscriminationabilityoftheEGRI, receiver operating characteristic (ROC) curves were con-structed,andtheareas underthe ROCcurves(AUC)were calculated.Foreach threshold,thesensitivity, specificity, positive predictive value (PPV),negative predictive value (NPV),positiveandnegativelikelihoodratios(LR+,LR−)and positiveandnegativepost-testprobabilities(PTP+,PTP−) werecalculated.TheoptimalcutoffvalueofEGRItopredict difficultairwaywasidentifyusingtheYoudenindexmethod, which definesthe cutoff in terms of the maximal sum of sensitivityandspecificity.
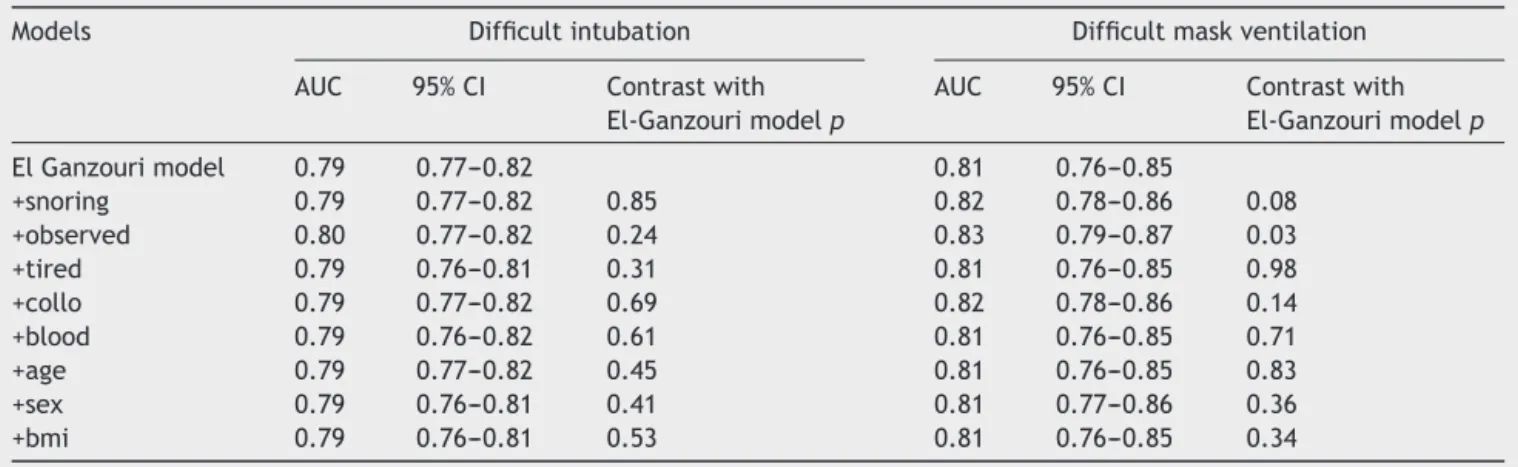
Nine multivariate logistic regression models were per-formedincludingallthe EGRIvariablesandadding oneat timethevariablesoftheSBquestionnaire.Wealsoexplored theinclusionofbodymassindex(BMI)variableinsteadofthe patient’sweightinthelogisticmodelthatconsideredallthe EGRIvariables.PatientswithBMI<30kg/m2wereassigneda
valueof0andpatientswithBMI≥30kg/m2wereassigneda
valueof1.TheHosmer---Lemeshovtestandtheareaunder theROC,wereusedtocompare thegoodnessoffitofthe
models.Differenceswerestatedasstatisticallysignificant whenp<0.05.AlltheanalysiswasperformedusingSAS9.3 (SAS209Institute,Cary,NC,USA).
Results
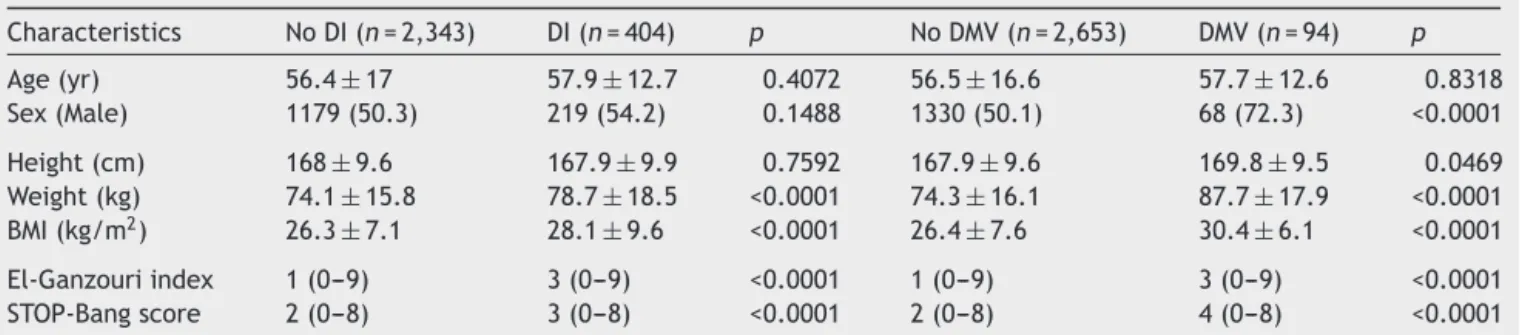
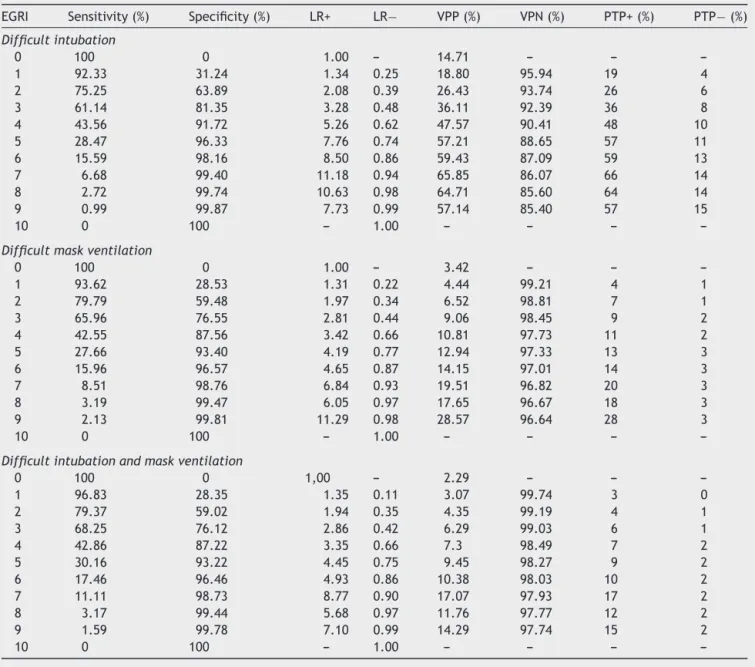
A total of 2747 patients were included in the study.The proportionofpatients withDIwas14.7%(95% CI13.4---16) andtheproportionofpatientswithDMVwas3.42%(95%CI 2.7---4.1). Patientswho concurrently reported DIand DMV were63(2.3%).ThemedianEGRIandSBscorewere1(range 0---9)and2(range0---8).Thedemographicandclinical char-acteristicsofstudyparticipantswerepresentedinTable1. PatientswithandwithoutDIorDMVdifferedonBMIwhereas malepatients weremorelikelytohave DMV.Higher level of EGRI andSB scorewere predictive of DIand DMV.The entire ability of EGRI to predict DI and DMV was evalu-atedusingtheROCcurves(Fig.1).TheareaundertheROC curveforDIwas0.77(95%CI0.74---0.80).Theoptimal cut-off value of EGRI was3, withsensitivity, specificity, PPV, andNPVvaluesof64.1%,81.4%,36.1%,and92.4%, respec-tively(Table2).Thepre-testprobabilityofDIinthestudy samplewas14.7%.Afteranegativetest,thepost-test prob-abilityofDIwasreducedto8%incorrespondenceto3cutoff valueofEGRI.Thecutoffvalueof4suggestedbyEl-Ganzouri wasassociated witha sensitivity of 43.6% a specificity of 91.7%andpost-testprobabilitywithanegativetestof10% (Table2).Inthemultivariatelogisticanalysisincludingthe EGRIvariables,theHosmerandLemeshowtestindicateda goodmodelfit(Chi-Square=11.03,p=0.14).Replacingthe patientsweightwiththeBMIvariable(<30vs.≥30kg/m2),
theareaundertheROC curvefor DIdidnotchange (0.78 vs.0.79,p=0.23)andthemodelfitremainreasonable (Chi-Square=8.76,p=0.19). Addingthe SB variables(one at a time)to theEGRI variablesin the logistic model,did not improvethe AUCof themodels(Table3).EGRI registered also a higher ability to predict DMV (AUC=0.76 (95% CI 0.71---0.81)). An EGRI ≥3 was the optimal cutoff for pre-dictaDMVwithasensitivityof66%andaspecificityof77% (Table2).Afteranegativetest,theprobabilityofDMVwas reducedfrom3%toapost-testprobabilityof2%bothfora cutoffvalueof3and4.Thecutoffvalueof4showedalower sensibilityandahigherspecificity(43%and88%respectively) comparedtothecutoffof3(Table2).Themultivariate logis-ticmodelincludingtheEGRIvariableshadanotsignificant HosmerandLemeshowtest(Chi-Square=4.64,p=0.59)and
Table1 Characteristicsofthesamplebydifficultairwayanddifficultmaskventilation.
Characteristics NoDI(n=2,343) DI(n=404) p NoDMV(n=2,653) DMV(n=94) p
Age(yr) 56.4±17 57.9±12.7 0.4072 56.5±16.6 57.7±12.6 0.8318
Sex(Male) 1179(50.3) 219(54.2) 0.1488 1330(50.1) 68(72.3) <0.0001
Height(cm) 168±9.6 167.9±9.9 0.7592 167.9±9.6 169.8±9.5 0.0469
Weight(kg) 74.1±15.8 78.7±18.5 <0.0001 74.3±16.1 87.7±17.9 <0.0001 BMI(kg/m2) 26.3±7.1 28.1±9.6 <0.0001 26.4±7.6 30.4±6.1 <0.0001
El-Ganzouriindex 1(0---9) 3(0---9) <0.0001 1(0---9) 3(0---9) <0.0001 STOP-Bangscore 2(0---8) 3(0---8) <0.0001 2(0---8) 4(0---8) <0.0001
1.00
0.75
0.50
0.25
0.00
0.00 0.25 0.50 0.75 1.00
1- Specificity
0.00 0.25 0.50 0.75 1.00
1- Specificity 1.00
0.75
0.50
0.25
0.00
Difficult tracheal intubation Difficult mask ventilation
Sensitivity
Sensitivity
9 8 7 6
5 4
3 2
1
0
Figure1 ROCcurvesfortheEGRItopredictDIandDMV.
Table2 DiagnosticindicatoroftheEl-Ganzouriindexinpredictingadifficultintubationanddifficultmaskventilation.
EGRI Sensitivity(%) Specificity(%) LR+ LR− VPP(%) VPN(%) PTP+(%) PTP−(%)
Difficultintubation
0 100 0 1.00 --- 14.71 --- ---
---1 92.33 31.24 1.34 0.25 18.80 95.94 19 4
2 75.25 63.89 2.08 0.39 26.43 93.74 26 6
3 61.14 81.35 3.28 0.48 36.11 92.39 36 8
4 43.56 91.72 5.26 0.62 47.57 90.41 48 10
5 28.47 96.33 7.76 0.74 57.21 88.65 57 11
6 15.59 98.16 8.50 0.86 59.43 87.09 59 13
7 6.68 99.40 11.18 0.94 65.85 86.07 66 14
8 2.72 99.74 10.63 0.98 64.71 85.60 64 14
9 0.99 99.87 7.73 0.99 57.14 85.40 57 15
10 0 100 --- 1.00 --- --- ---
---Difficultmaskventilation
0 100 0 1.00 --- 3.42 --- ---
---1 93.62 28.53 1.31 0.22 4.44 99.21 4 1
2 79.79 59.48 1.97 0.34 6.52 98.81 7 1
3 65.96 76.55 2.81 0.44 9.06 98.45 9 2
4 42.55 87.56 3.42 0.66 10.81 97.73 11 2
5 27.66 93.40 4.19 0.77 12.94 97.33 13 3
6 15.96 96.57 4.65 0.87 14.15 97.01 14 3
7 8.51 98.76 6.84 0.93 19.51 96.82 20 3
8 3.19 99.47 6.05 0.97 17.65 96.67 18 3
9 2.13 99.81 11.29 0.98 28.57 96.64 28 3
10 0 100 --- 1.00 --- --- ---
---Difficultintubationandmaskventilation
0 100 0 1,00 --- 2.29 --- ---
---1 96.83 28.35 1.35 0.11 3.07 99.74 3 0
2 79.37 59.02 1.94 0.35 4.35 99.19 4 1
3 68.25 76.12 2.86 0.42 6.29 99.03 6 1
4 42.86 87.22 3.35 0.66 7.3 98.49 7 2
5 30.16 93.22 4.45 0.75 9.45 98.27 9 2
6 17.46 96.46 4.93 0.86 10.38 98.03 10 2
7 11.11 98.73 8.77 0.90 17.07 97.93 17 2
8 3.17 99.44 5.68 0.97 11.76 97.77 12 2
9 1.59 99.78 7.10 0.99 14.29 97.74 15 2
---Table3 ROCcontrastestimationbetweenEl-GanzourimodelandEl-Ganzouri+SBmodels.
Models Difficultintubation Difficultmaskventilation
AUC 95%CI Contrastwith El-Ganzourimodelp
AUC 95%CI Contrastwith El-Ganzourimodelp
ElGanzourimodel 0.79 0.77---0.82 0.81 0.76---0.85
+snoring 0.79 0.77---0.82 0.85 0.82 0.78---0.86 0.08
+observed 0.80 0.77---0.82 0.24 0.83 0.79---0.87 0.03
+tired 0.79 0.76---0.81 0.31 0.81 0.76---0.85 0.98
+collo 0.79 0.77---0.82 0.69 0.82 0.78---0.86 0.14
+blood 0.79 0.76---0.82 0.61 0.81 0.76---0.85 0.71
+age 0.79 0.77---0.82 0.45 0.81 0.76---0.85 0.83
+sex 0.79 0.76---0.81 0.41 0.81 0.77---0.86 0.36
+bmi 0.79 0.76---0.81 0.53 0.81 0.76---0.85 0.34
aAUCof 0.81(95%CI0.76---0.85).AddingtheSBvariables
(oneatatime)inthelogisticmodel,theAUCincreaseswith
theinclusionofobserved variable(0.83vs.0.81,p=0.03)
(Table3).The areaundertheROCcurvefor thesubsetof patientswithDIandDMVwas0.77(95%CI0.72---0.83).The diagnosticindexconfirmed theoptimal cutoffof 3witha sensitivityof68%andaspecificity of76%.The probability ofthecombineddifficultairwaywasreducedfrom2%to1% (negativepost-testprobability).
Discussion
In the current study the incidence of DMVwas 3.42%, DI 14.7%,andtheDI-DMVcombination2.3%.EGRIhasproved auseful bedside screening test topredict DA, performing wellforbothDIasintheoriginaldescription,butalsofor DMV.ThecombinationofEGRIandSBdoesnotimprovethe predictivevalueforDA,exceptforobservedapneaitemin theSBquestionnaire.The DMVhasbecomethesubjectin recentyearsofamoreextensiveinvestigationawareofthe factthattheabilitytoventilateandoxygenatethepatient isthekeytoagoodoutcomeinfrontofaDA.Theincidence ofDMVvaries from1.4% to16%,depending onthe defini-tionanddifferencesinthestudypopulation, thereported incidence in our study is in line with the literature and non-negligible.14---16Severalriskfactorshavebeenidentified andpredictivescores proposed butnot widespreadinthe dailyclinicalpractice.3---6ThisstudyfoundanincidenceofDI higherthanusuallyreported,howeverastandarddefinition ofthedifficultairwaycannotbeidentifiedintheavailable literatureasalsomentionedintheupdateofDifficult Air-wayGuidelinesrecentlypublishedbyASA.17Wedecidedto use the definitions of Difficult Airwayof the Italian Soci-ety of Anaesthesia,12 as formally adopted by the centers involvedin the studyand referencestandardsof the Ital-ianMinistryofHealth.Itisrecognizedintheliteraturethat theincidenceofdifficultairwaychangeswiththedefinition used,14accordinglythepublishedestimatesoftheincidence ofdifficultintubationrangefrom0.1to13%.Recently,Corso andcoworkers10usingthesamedefinitionfoundsimilarrate ofDI.The incidenceofDI combinedwithDMV,despite its importance,hasonlyrecentlybeenhighlighted.Kheterpal andcolleagues6inarecentmulticenterobservationalstudy
anindirect evidenceofOSA. Thisis notsurprisingsinceit isknownintheliteraturetheassociationbetweenOSAand DMV.6Ourstudy alsohaslimitations: firstthe sample size is underpowered to identifythe situation of DI combined toDMV,second wedidnotgradetheDMVpotentially pro-ducinganoverestimationofrateofDMV,finallythenature retrospective of our analysiscould ledto aselection and treatmentbias.Inconclusiontheresultsofthisstudy con-firmthatinarealworldclinicalsetting,theincidenceofDA isnotnegligibleandsuggesttheuseoftheEGRIassimple bedsidepredictivescoretoimprovepatientsafety.Further prospectivestudytovalidatethisscorewouldbeuseful.
Authorship
RuggeroM.Corsoconceivedof thestudy,andparticipated in its design and coordination and helped to draft the manuscript,DavideCattanohelpedtodraftthemanuscript, MatteoBucciolihaspreparedthedatabaseandassistedin thepresentationofdata,ElisaCarrettaparticipatedinthe designofthestudyandperformed thestatisticalanalysis, OrianaNanni hasrevised thestatistical analysis,Salvatore Zampone helped to draft the manuscript, StefanoMaitan helpedtocollectdataanddraftthemanuscript.Allauthors readandapprovedthefinalmanuscript.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.CookTM,Woodall N,FrerkC,FourthNationalAuditProject. MajorcomplicationsofairwaymanagementintheUK:resultsof theFourthNationalAuditProjectoftheRoyalCollegeof Anaes-thetistsandtheDifficultAirwaySociety.Part1:anaesthesia.Br JAnaesth.2011;106:617---31.
2.CheneyFW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology.2006;105:1081---6.
3.ArnéJ,DescoinsP,FusciardiJ,etal.Preoperativeassessment for difficult intubation in general and ENT surgery: predic-tivevalueofaclinicalmultivariateriskindex. BrJAnaesth. 1998;80:140---6.
4.WilsonME,SpiegelhalterD,RobertsonJA,etal.Predicting dif-ficultintubation.BrJAnaesth.1988;61:211---6.
5.L’Hermite J, Nouvellon E, Cuvillon P, et al. The simpli-fied predictive intubation difficulty score: a new weighted score for difficult airway assessment. Eur J Anaesthesiol. 2009;26:1003---9.
6.KheterpalS,HealyD,AzizMF,etal.,MulticenterPerioperative OutcomesGroup(MPOG)PerioperativeClinicalResearch Com-mittee.Incidence,predictors,and outcome ofdifficultmask ventilationcombinedwithdifficultlaryngoscopy:areportfrom themulticenterperioperativeoutcomesgroup.Anesthesiology. 2013;119:1360---9.
7.YentisSM.Predictingdifficultintubation---worthwhileexercise orpointlessritual?Anaesthesia.2002;57:105---9.
8.McPhersonD,VaughanRS,WilkesAR,etal.Asurveyof anaes-thetic practice in predicting difficult intubation in UK and Europe.EurJAnaesthesiol.2012;29:218---22.
9.El-GanzouriAR,McCarthyRJ,TumanKJ,etal.Preoperative air-wayassessment:predictivevalueofamultivariateriskindex. AnesthAnalg.1996;82:1197---204.
10.CorsoR,PetriniF,BuccioliM,etal.Clinicalutilityof preopera-tivescreeningwithSTOP-Bangquestionnaireinelectivesurgery. MinervaAnestesiol.2013[Epubaheadofprint].
11.Killoran PV, Madduku V, Altamira AV, et al. Use of a com-prehensive airway assessmentform to predictdifficult mask ventilation.Anesthesiology.2011:A442.
12.Gruppo di Studio SIAARTI ‘‘Vie Aeree Difficili’’, IRC e SARNePI; Task Force. Recommendations for airway control anddifficultairwaymanagement.MinervaAnestesiol.2005;71: 617---57.
13.ChungF,SubramanyamR,LiaoP,etal.HighSTOP-Bangscore indicatesahighprobabilityofobstructivesleepapnoea.BrJ Anaesth.2012;108:768---75.
14.RoseDK,CohenMM.Theincidenceofairwayproblemsdepends onthedefinitionused.CanJAnaesth.1996;43:30---4.
15.KheterpalS,MartinL,ShanksAM,etal.Predictionandoutcomes ofimpossiblemaskventilation:areviewof50,000anesthetics. Anesthesiology.2009;110:891---7.
16.CattanoD,PanicucciE,PaolicchiA,etal.Riskfactors assess-mentofthedifficultairway:anItaliansurveyof1956patients. AnesthAnalg.2004;99:1774---9.
17.ApfelbaumJL,HagbergCA,CaplanRA,etal.Practice guide-linesformanagementofthedifficultairway:anupdatedreport by the American Society of Anesthesiologists Task Force on ManagementoftheDifficultAirway.Anesthesiology.2013;118: 251---70.
18.ConnorCW,SegalS.Theimportanceofsubjectivefacial appear-ance on the ability of anesthesiologists to predict difficult intubation.AnesthAnalg.2014;118:419---27.