www.jped.com.br
ORIGINAL
ARTICLE
Urinary
tract
infection
caused
by
community-acquired
extended-spectrum

-lactamase-producing
bacteria
in
infants
夽
Yun
Hee
Kim
a,
Eun
Mi
Yang
a,∗,
Chan
Jong
Kim
a,baChonnamNationalUniversityHospital,Gwangju,RepublicofKorea
bChonnamNationalUniversityMedicalSchool,Gwangju,RepublicofKorea
Received12February2016;accepted22June2016 Availableonline11November2016
KEYWORDS Urinarytract infection; Antimicrobial resistance;
-Lactamase; Riskfactors; Infant
Abstract
Objective: Urinarytractinfection(UTI)causedbyresistantstrainsofbacteriaisincreasingly prevalentinchildren.Theaimofthisstudywastoinvestigatetheclinicalcharacteristicsand riskfactorsforUTIcausedbycommunity-acquiredextended-spectrum-lactamase (CA-ESBL)-producingbacteriaininfants.
Methods: Thiswas aretrospectivestudy performed over5years inasingleKorean center. HospitalizedinfantswithfebrileUTIwereenrolledanddividedintotwogroups(CA-ESBLvs. CAnon-ESBLUTI).Theyearlyprevalencewascalculated.Baselinecharacteristicsandclinical coursesuchasfeverduration,laboratoryandradiologicalfindingswerecomparedbetweenthe twogroups.RiskfactorsassociatedwiththeCA-ESBLUTIwereinvestigated.
Results: Amongtheenrolledinfants(n=185),31(17%)hadCA-ESBLUTI.Theyearlyprevalence ofESBLofCA-ESBLUTIincreasedduringthestudy (0%in2010,22.2% in2015).Infantswith CA-ESBLUTIhadalongerdurationoffeverafterinitiatingantibiotics(2.0±1.1vs.1.5±0.6 days,p=0.020).Corticaldefectsonrenalscanandearlytreatmentfailureweremorefrequent inCA-ESBL(64.5vs.42.2%,p=0.023;22.6vs.4.5%,p=0.001).Alogisticregressionanalysis revealedthaturinarytractabnormalitiesandpreviousUTIwereindependent riskfactorsfor CA-EBSLUTI(oddsratio,2.7;p=0.025;10.3;p=0.022).
Conclusion: TheincidenceofUTIcausedbyESBL-producingbacteriahasincreasedinKorean infants.RecognitionoftheclinicalcourseandriskfactorsforESLB-producingUTImayhelpto determineappropriateguidelinesforitsmanagement.
©2016PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradePediatria.Thisis anopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/
by-nc-nd/4.0/).
夽
Pleasecitethisarticle as:KimYH,YangEM,KimCJ. Urinarytract infectioncausedbycommunity-acquired extended-spectrum -lactamase-producingbacteriaininfants.JPediatr(RioJ).2017;93:260---6.
∗Correspondingauthor.
E-mail:emyang@chonnam.ac.kr(E.M.Yang).
http://dx.doi.org/10.1016/j.jped.2016.06.009
0021-7557/©2016PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradePediatria.Thisisanopenaccessarticleunder
PALAVRAS-CHAVE Infecc¸ãodotrato urinário;
Resistência antimicrobiana;
-Lactamase; Fatoresderisco; Neonato
Infecc¸ãodotratourináriocausadaporbactériasprodutorasde-lactamases deespectroampliadoadquiridasnacomunidadeemneonatos
Resumo
Objetivo: A infecc¸ãodotratourinário(ITU) causadaporcepasdebactériasresistentesestá cadavezmaisprevalenteemcrianc¸as.Oobjetivodesteestudofoiinvestigarascaracterísticas clínicas e os fatores de riscode ITU causada por bactérias produtoras de-lactamases de espectroampliadoadquiridasnacomunidade(ESBLCA)emneonatos.
Métodos: Estefoiumestudoretrospectivorealizadopormaisde5anosemumúnicocentro coreano.NeonatosinternadoscomITUfebrilforaminscritosedivididosemdoisgrupos (ITU porESBLCAemcomparac¸ãoanãoESBLCA).Aprevalênciaanualfoicalculada.As caracterís-ticasbásicaseocursoclínico,comodurac¸ãodafebreeachadoslaboratoriaiseradiológicos, foramcomparadosentreosdoisgrupos.OsfatoresderiscoassociadosàITUporESBLCAforam investigados.
Resultados: Entreosneonatosinscritos(n=185),31(17%) apresentaramITUporESBLCA.A prevalênciaanualdeESBLemITUporESBLCAaumentouduranteoestudo(0%em2010,22,2% em2015).OsneonatoscomITUporESBLCAapresentarammaiordurac¸ãodefebreapósoinício dos antibióticos(2,0±1,1em comparac¸ão a1,5±0,6dias, p=0,020).Osdefeitos corticais no examerenal e afalhaprecoce notratamentoforammais frequentesemESBL CA(64,5 em comparac¸ãoa42,2%,p=0,023; 22,6em comparac¸ãoa4,5%, p=0,001).Umaanálisede regressãologísticarevelouqueasanomaliasdotratourinárioeaITUanterioreramfatoresde riscoindependentesdeITUporESBLCA(razãodechance:2,7;p=0,025;10,3;p=0,022).
Conclusão: A incidência de ITU causada por bactérias produtoras de ESBL aumentou em neonatoscoreanos.OreconhecimentodocursoclínicoedosfatoresderiscodeITUporESBL poderáajudaradeterminarasdiretrizesadequadasdemanejo.
©2016PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradePediatria.Este ´
eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/
by-nc-nd/4.0/).
Introduction
Urinary tract infection (UTI) is a common cause of
bacterial infections among infants and young children
with fever without a source. In general, initial antibi-otic therapy for UTI is empirically supported until the culture and sensitivity results are available. However, due to the frequent use of antibiotics, resistant strains
are emerging. The resistance of Gram-negative
bacte-ria is usually due to plasmid-mediated enzymes called
extended-spectrum -lactamases (ESBLs).1 These are
fre-quentlyproducedbyEscherichiacoliandKlebsiellaspecies, which are the most common UTI-causing pathogens.2
ESBL-producing bacteria werefirst reportedin the 1983,3
and are now widespread worldwide.4 ESBLs confer not
only resistance to -lactam antibiotics but, oftentimes, cross-resistance to other antibiotics such as aminogly-cosides, trimethoprim-sulfamethoxazole (TMP-SMX), and quinolones.5
Infectionscausedbythesebacteriaarethoughttooccur mainlyinhospitalsandnursinghomes.6Morerecently,
ESBL-producingbacteria havestartedtodisseminatewithinthe widercommunity;indeed,inmanycountries,theincidence of community-onset infections has increased.7---10 Whereas
several studies have analyzed risk factors for UTI caused by ESBL-producing bacteria in adults7,10 and children,8,9
onlylimiteddataareavailableoncommunity-acquired(CA) UTIscausedbyESBL-producingbacteriaininfants.Theaim of this study, therefore, was to investigate the clinical
characteristicsandriskfactorsforCAUTIcausedby ESBL-producingbacteriaininfants.
Methods
Studydesignandpatientselection
Thisretrospectivestudywasconductedatsinglecenterin Korea betweenJanuary 2010 and June 2015. The criteria for enrollment wereas follows:(1) febrile UTI caused by
E. coli and Klebsiella spp.; (2) hospitalized patients; (3) ageunder12months. Patientswhohad beenhospitalized withinthepastweekandthosewithurineculturesobtained
more than 48h after admission were excluded. UTI was
definedasabnormalurinalysisresults andapositiveurine culture(≥5×104colonyformingunits/mL)accordingtothe
AmericanAcademy of Pediatrics guidelines.11 Early
CA-ESBLandCAnon-ESBLgroupswerecomparedregarding the possible risk factors. The study was approved by the InstitutionalReviewBoardofthishospitalandwasin agree-mentwiththeDeclarationofHelsinki.
Imagingstudies
Renal abnormalities, including vesicoureteral-reflux,
hydronephrosis,and dysplastic kidney, were investigated.
Renal ultrasound (US) and technetium-99m
dimercapto-succinic acid (DMSA) scan were performed to determine
any anatomical abnormalities and the presence of acute pyelonephritis,respectively.TheUSresultswereconsidered pathological in case of abnormal kidney morphology and parenchymal echogenicity, any grade of dilatation of the collectingsystem(renalpelvis,calyces,or distalureters), or bladder mucosal thickening. An abnormal DMSA result wasdefined by the presence of focal or diffuse areas of reducedradionuclide uptake without evidence of cortical
loss or by the presence of diffusely decreased uptake
in an enlarged kidney.12 DMSA was repeated after six
monthstodetect any renal corticalscarring. Voiding cys-tourethrographywasperformedforpatientswithabnormal imagingresults.Thevesicoureteralreflux(VUR)wasgraded according to the International Reflux Study Committee classification.13
IdentificationofESBLs
Antimicrobial susceptibility testing was performed by the
disk diffusion method as recommended by the Clinical
andLaboratory StandardsInstitute guidelines.14 ESBL
pro-duction was determined by the double-disk synergy test, also according to the Clinical and Laboratory Standards Institute guidelines.14 A minimum 5-mm increase in the
zone tested in combination with clavulanic acid vs. the zone tested alone was accepted as an indication of ESBL production.15
Statisticalanalysis
Descriptivestatisticswerereportedasmeanwithstandard deviation or percentages where appropriate. Continuous variableswereanalyzedusingt-testsforindependent sam-ples,andcategoricalvariableswereanalyzedusingFisher’s exactor thechi-squared test. Linear regressionwas used toassess the trends of the yearly prevalence of CA-ESBL UTI.Logisticregressionwasusedtodeterminetherisk fac-torsforESBL-producingbacteria.Theresultswereevaluated with 95% confidence intervals. A p-value<0.05 was con-sideredsignificant.Allstatisticalanalyseswereperformed usingSPSSversion21.0(SPSSInc.,IL,UnitedStates).
Results
A total of 185 infants were enrolled and divided into
two groups (CA-ESBL vs. CA non-ESBL UTI). Thirty-one
(16.7%)ofthepatientshadUTIscausedbyESBL-producing bacteria,while the remaining154 patients had non-ESBL-producingbacteriaintheirurinecultures.Theproportionsof
50%
40%
30%
20%
10%
0%
2010
0%(0/27) 6.9%(2/29)
13.2%(5/38) 14.7%(5/34)
43.3%(13/30)
22.2%(6/27)
2011 2012 2013 2014 2015
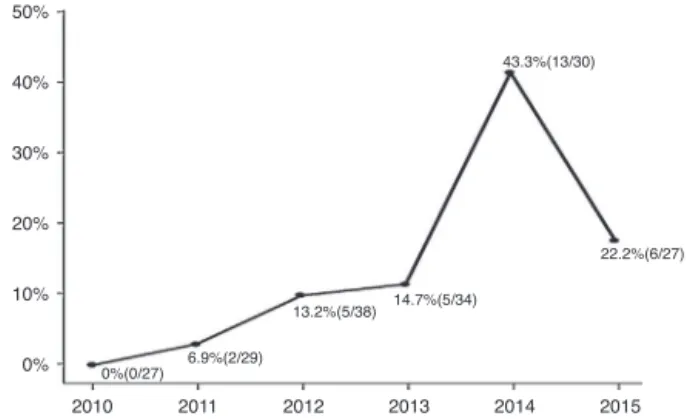
Figure 1 Incidence of CA ESBL-producing UTIs (% of total UTIs).CA, communityacquired; ESBL, extended-spectrum -lactamase;UTI,urinarytractinfection.Note:2015dataarefor January-Juneonly;pfortrend<0.001.
ESBL-producingbacteriacausingUTIswere0%in2010,6.9% in 2011,13.2%in 2012,14.7%in 2013,43.3%in 2014,and 22.2% in 2015. The yearlyincidence rates of CA-ESBL UTI increasedduringthestudyperiod,andthep-valueforthe trendwassignificant(p<0.001;Fig.1).
Baselineandclinicalcharacteristics
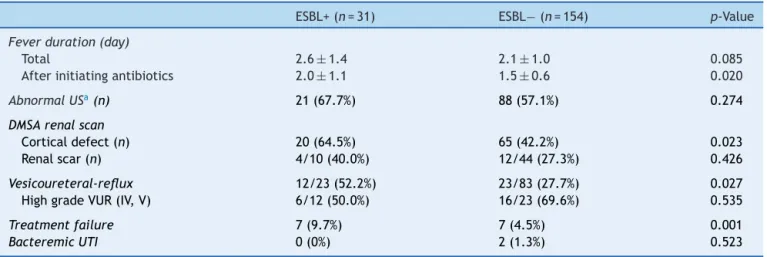
The CA-EBSL and CA non-ESBLUTI groups consisted of 31 (17%) and154 (83%)patients, respectively. The mean age washigherintheCA-ESBLUTIgroupthan inthenon-ESBL UTI group (4.2±2.8 vs. 3.1±2.3 months, p=0.018). E. coliwasthedominantpathogeninbothgroups: the ESBL-production proportionbetweenE. coliandKlebsiellaspp. didnotdiffer(Table1).Nodifferencesinsexorlaboratory findings were observed between the two groups. Defer-vescenceaftertreatment initiationwaslongerin CA-ESBL UTI thanin CA non-ESBLUTI (2.0±1.1vs. 1.5±0.6days,
p=0.020;Table1).USabnormalitiesdidnotdifferbetween thegroups. CorticaldefectsonDMSA scanweremore fre-quentintheCA-ESBLthanintheCAnon-ESBLUTIgroup(64.5
vs.43.5%,p=0.023);however, presenceofrenalscarsdid notsignificantlydiffer(40.0vs.27.3%,p=0.426;Table2). Ofthe23patientswithCA-ESBLUTI,12(52.2%)were diag-nosed withVUR, whose rate wassignificantly higher than that intheCA-non-ESBLUTI group(p=0.027). Bacteremic UTIwasobservedintwopatients (1.3%)withCAnon-ESBL UTI.Earlytreatment failurewasmorefrequentinthe CA-ESBLUTIgroupthanintheCAnon-ESBLUTIgroup(22.6vs. 4.5%,p=0.001).
Antibioticsresistancerates
Table1 Baselinecharacteristicsofpatients.
ESBL+(n=31) ESBL−(n=154) p-Value
Age(months) 4.2±2.8 3.1±2.3 0.018
Gender
Male 23 120 0.651
Female 8 34
Laboratoryfindings
WBC(103/mm3) 14.4±7.0 15.5±7.8 0.466
CRP(mg/dL) 4.6±3.6 4.0±3.4 0.436
Urinalysis
Pyuria 28(90.3%) 152(98.7%) 0.009
Hematuria 17(54.8%) 131(85.1%) <0.001
Protein 8(25.8%) 84(54.5%) 0.004
Nitrite 14(45.2%) 56(36.4%) 0.357
Pathogens
E.coli 25 116 0.526
Klebsiellaspp. 6 38
Underlyingconditions
Renalabnormalitiesa 15(48.4%) 39(25.3%) 0.010
Anyb 2(6.5%) 11(7.1%) 0.891
Previousmedicalcondition
Useofantibiotics 9/30(30.0%) 22/120(18.3%) 0.158
PreviousUTI 5(16.1%) 3(1.9%) 0.001
Recenthospitalization 7(22.5%) 17(11.0%) 0.081
WBC,whitebloodcount;CRP,C-reactiveprotein;ESBL,extended-spectrum-lactamase;UTI,urinarytractinfection. a Renalabnormalitiesincludevesicoureteral-reflux,hydronephrosis,anddysplastickidney.
b Cardiac,respiratory,andneurologicaldiseases.
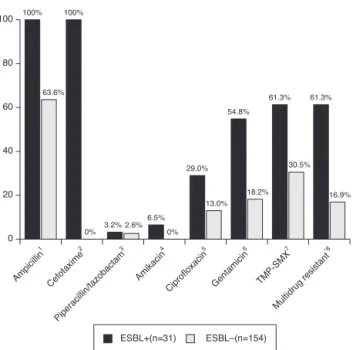
31ESBLisolates(61.3%)wereresistanttoatleasttwogroups ofnon--lactamantibioticagents.
Riskfactors
Regarding possible risk factors, age, renal abnormalities, previous UTI, and recent hospitalization were associated withCA-ESBLUTI(Table1).Thelogisticregressionanalysis
identifiedurinarytractabnormalityandpreviousUTIhistory asindependentriskfactors,whichwerefoundtoincrease theriskby2.7-and10.3-fold,respectively(Table3).
Discussion
The aim of this study was to highlight the emergence of CA-ESBL UTIs in Korean infants and to assess the clinical
Table2 ClinicalcourseofCA-ESBLUTIandCAnon-ESBLUTI.
ESBL+(n=31) ESBL−(n=154) p-Value
Feverduration(day)
Total 2.6±1.4 2.1±1.0 0.085
Afterinitiatingantibiotics 2.0±1.1 1.5±0.6 0.020
AbnormalUSa(n) 21(67.7%) 88(57.1%) 0.274
DMSArenalscan
Corticaldefect(n) 20(64.5%) 65(42.2%) 0.023 Renalscar(n) 4/10(40.0%) 12/44(27.3%) 0.426
Vesicoureteral-reflux 12/23(52.2%) 23/83(27.7%) 0.027
HighgradeVUR(IV,V) 6/12(50.0%) 16/23(69.6%) 0.535
Treatmentfailure 7(9.7%) 7(4.5%) 0.001
BacteremicUTI 0(0%) 2(1.3%) 0.523
ESBL, extended-spectrum -lactamase; UTI, urinary tract infection; US, ultrasonography; DMSA, dimercaptosuccinic acid; VUR, vesicoureteral-reflux.
Ampicillin 1 Cefotaxime 2 Piperacillin/tazobactam 3 Amikacin 4 Ciprofloxacin 5 Gentamicin 6 TMP-SMX 7 Multidrug resistant *8 0 20 40 60 100% 63.6% 100%
0% 3.2% 2.6% 6.5% 29.0% 54.8% 18.2% 61.3% 30.5% 61.3% 16.9% 13.0% 0% 80 100 ESBL+(n=31) ESBL–(n=154)
Figure 2 Antibiotic resistance of bacterial isolates caus-ing UTI. UTI, urinary tract infection; TMP-SMX, trimetho-prim/sulfamethoxazole.*Multidrugresistant,resistanttomore thantwo non--lactamantibiotics.Significancecalculated by Fisher’sexacttest:1p<0.001;2p<0.001;3p=1.000;4p=0.002; 5p=0.005;6p<0.001;7p<0.001;8p<0.001.
characteristics and possible risk factors for CA-ESBL UTI in infants. An increasing incidence of multidrug-resistant bacteria has been reported not only in hospital-acquired infections but alsoCA infections, mostly UTIs.8 Thus,the
choice of appropriate antibiotics has become both more complicated and may delay appropriate therapy.16,17 This
studyanalyzed185casesofinfantileCAUTI,andshowedan increasingtrendintheoccurrenceofCA-ESBLUTI. Signifi-cantdifferenceswereobservedindefervescencetimeand corticaldefectonDMSAscansinCA-ESBLUTI.IntheCA-ESBL UTIcases,urinarytractabnormalities,includingVUR,were morefrequent,andtheratesofresistancetonon--lactam antibioticswererelativelyhigh.Urinarytractabnormalities andUTIhistorywerefoundtobeindependentriskfactors.
Over the past two decades, there has been wide use of extended broad-spectrum antibiotics to counter the increasingratesofESBL-producingbacteriainpatientswith UTI worldwide.7,18 E. coli and Klebsiella spp., the most
commonUTIpathogens, havevariousantibioticresistance mechanisms, including enhanced drug efflux, alterations of the drug target, and production of plasmid-mediated
Table3 Logisticregressionofriskfactorsassociatedwith CA-ESBLUTIininfants.
Riskfactors Oddsratio(95%CI) p
Age 0.866(0.733---1.025) 0.094
Renalabnormalities 2.741(1.137---6.606) 0.025 Recenthospitalization 1.964(0.390---9.894) 0.413 PreviousUTI 10,295(1404---75,492) 0.0
ESBL,extended-spectrum-lactamase;UTI,urinarytract infec-tion.
-lactamases.19 Resistance is usually due to -lactamase
enzymescalledESBLs.Thepatternsofantibioticresistance differ temporally and regionally.18,20,21 The rates of
ESBL-producing E. colirange from2.2%in a 2011 Swissstudy18
to 55.0% in a 2009 Chinese study.20 Several factors are
involved in the rapid spread of ESBL-producing bacteria in countrieswithlow useof antibiotics,including acquisi-tionfromfood,22 person-to-persontransmissionfromfecal
carriers,23 disseminationofESBL-producingbacteriainthe
environment,24andtheexistenceofreservoirs,suchas
long-termcarecenters.25
Most studies have determined that the risks factors for CA-ESBL-producing bacterial infections generally are recenthospitalization,previousUTIepisodes,urinarytract abnormalities,underlyingdisease,UTIwithKlebsiellaspp., anduse ofcephalosporinUTI antimicrobialprophylaxis.7---9
The use of antimicrobial prophylaxis is an important risk factor to increase antibiotic resistance; TMP-SMX mini-mallydecreasedantimicrobialsusceptibilitiescomparedto cephalosporin.26Asonlytwopatientsinthisstudyreceived
theantimicrobialprophylaxis,itwasnotpossibleassessthe riskofantimicrobialprophylaxis.Inthepresentstudy, uri-narytractabnormalities andUTIhistorywerefoundtobe independentriskfactorsforfutureCA-ESBLUTIininfants. However, a high number of CA-ESBL-producing bacterial infections occurinpatients withoutobviousrisk factors.27
Infact,inthepresentstudy,approximately60%ofpatients withCA-ESBLUTIhadnorisk factors.Thisresultmightbe relatedtotheconstantincreaseinthenumberof healthy carrierscolonizedwithESBL-producingbacteria.23
A major concern regarding ESBL-producing bacteria is thehighrateofcross-resistancetonon--lactamantibiotics suchasciprofloxacin,aminoglycosides,nitrofurantoin,and TMP-SMX. In thisstudy, 61% ofpatients showed antibiotic resistancetoatleasttwosuitablenon--lactamantibiotics used to treat UTI. Similar results have been reported by otherinvestigators.28Theincreasingincidenceofmulti-drug
resistancebyESBL-producingbacteriacouldbecomea prob-lemforthetreatmentofUTI.
Manystudieshavereportedthatinfectionbythese bacte-ria might lead to a delay in appropriate therapy and a concomitantincreaseintheratesoftreatmentfailureand comorbidity.21,29Proposinganappropriateempirical
antibi-otic treatment for CA-ESBL UTI is difficult, and initial empiricalantibiotictherapyisoftenunsuccessful. Addition-ally,whenESBL-producingbacteriaareisolated,thereare almostnooptionsfororaltherapytoimprovepatient symp-toms. In the present study, treatment failure was more frequent in the CA-ESBL UTI group; however, there was nosignificant inter-group differenceinclinical manifesta-tions such as bacteremic UTI or renal scarring. Resistant strains were not associated with worsening of renal out-come in the present study,but previous studiesindicated that ESBL-producing bacterialinfectionincrease therates oftreatmentfailureanddeath.21,27,29
Several studies have shown increasing recognition of ESBL-producing bacteria asa cause of CA infection. Most data on CA-ESBL infections are based on adult popula-tions,andrelativelyfewpediatricstudiesareavailable.8,9,30
UTIsisincreasing,itisimportanttounderstandtherelevant epidemiologicalchangesininfants.
This study has some limitations. First, this was retro-spectivestudy;therefore,somedataweremissingfromthe medicalrecords.Second,thisstudyentailedasingle-center analysiswitharestrictednumber ofpatients.The sample sizeoftheCA-ESBLUTIgroupwassmall,thusimposing lim-itations on statistical power. Third, VCUG wasperformed onlywhenimagestudyfindingswereabnormal.Inorderto achieveabetterunderstandingoftheclinicalcharacteristics and determine the risk factors for UTIs caused by ESBL-producingbacteriaininfants,additional,cohortprospective studiesbasedonalargepopulationarerequired.
In conclusion, the incidence of UTI caused by ESBL-producing bacteria has increased gradually in Korean infants.UrinarytractabnormalitiesandpreviousUTI infec-tionwerefound tobesignificant independentrisk factors associatedwithCA-EBSLUTI.Forsuchpatients,recognition oftheriskfactorsforESLB-producingUTImayhelpto deter-mineappropriateguidelinesforitsmanagementandmore attention to the choice of empirical antibiotic therapy is needed.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
Thisstudywassupportedbyagrant(HCRI16916-1)Chonnam NationalUniversityHwasunHospitalInstituteforBiomedical Sciencel.
References
1.LivermoreDM.Defininganextended-spectrumbeta-lactamase. ClinMicrobiolInfect.2008;14:3---10.
2.Kuster SP, Hasse B, Huebner V, Bansal V, Zbinden R, Ruef C,etal. Risksfactorsfor infectionswithextended-spectrum beta-lactamase-producingEscherichiacoliandKlebsiella pneu-moniaeat a tertiarycare university hospital in Switzerland. Infection.2010;38:33---40.
3.KnotheH,ShahP,KrcmeryV,AntalM,MitsuhashiS.Transferable resistancetocefotaxime,cefoxitin,cefamandoleand cefurox-imeinclinicalisolatesofKlebsiellapneumoniaeandSerratia marcescens.Infection.1983;11:315---7.
4.LivermoreDM,HawkeyPM.CTX-M:changingthefaceofESBLs intheUK.JAntimicrobChemother.2005;56:451---4.
5.Coque TM, Baquero F, Canton R. Increasing prevalence of ESBL-producing Enterobacteriaceae in Europe.Euro Surveill. 2008;1:3,pii:19044.
6.Wiener J, Quinn JP, Bradford PA, Goering RV, Nathan C, Bush K, et al. Multiple antibiotic-resistant Klebsiella and
Escherichiacoliinnursinghomes.JAMA.1999;281:517---23. 7.CalboE,RomaníV,XercavinsM,GómezL,VidalCG,QuintanaS,
etal.Riskfactorsforcommunity-onseturinarytractinfections dueto Escherichia coli harbouring extended-spectrum beta-lactamases.JAntimicrobChemother.2006;57:780---3. 8.FanNC,ChenHH,ChenCL,OuLS,LinTY,TsaiMH,etal.Riseof
community-onseturinarytractinfectioncausedby extended-spectrum-lactamase-producingEscherichiacoliinchildren.J MicrobiolImmunolInfect.2014;47:399---405.
9.TopalogluR, Er I,DoganBG,Bilginer Y,Ozaltin F,BesbasN, etal.Riskfactorsincommunity-acquiredurinarytract infec-tions causedbyESBL-producing bacteria inchildren. Pediatr Nephrol.2010;25:919---25.
10.OsthoffM,McGuinnessSL,WagenAZ,EisenDP.Urinarytract infectionsduetoextended-spectrumbeta-lactamase-producing Gram-negativebacteria:identificationofriskfactorsand out-comepredictorsinanAustraliantertiaryreferralhospital.Int JInfectDis.2015;34:79---83.
11.RobertsKB,SubcommitteeonUrinaryTractInfection,Steering CommitteeonQualityImprovementandManagement.Urinary tractinfection:clinicalpracticeguidelineforthediagnosisand managementoftheinitialUTIinfebrileinfantsandchildren2 to24months.Pediatrics.2011;128:595---610.
12.KallenR.Imagingstudiesafterafirstfebrileurinarytract infec-tioninyoungchildren.NEnglJMed.2003;348:1812---4. 13.Medical versus surgical treatment of primary vesicoureteral
reflux: report of the International Reflux StudyCommittee. Pediatrics.1981;67:392---400.
14.National Committee for Clinical Laboratory Standards. Per-formance standards for antimicrobial susceptibility testing. Twelfth informational supplement: NCCLS document M100-S12. Wayne, PA:National Committee for ClinicalLaboratory Standard;2002.
15.Thomson KS, Sanders CC. Detection of extended-spectrum beta-lactamasesinmembersofthefamilyEnterobacteriaceae: comparison of the double-disk and three-dimensional tests. AntimicrobAgentsChemother.1992;36:1877---82.
16.RamphalR,AmbrosePG.Extended-spectrumbeta-lactamases and clinical outcomes: current data. Clin Infect Dis. 2006;42:S164---72.
17.Simões e Silva AC, Oliveira EA. Update on the approach of urinary tract infection in childhood. J Pediatr (Rio J). 2015;91:S2---10.
18.Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extended-spectrum-lactamase-producingGram-negative pathogensin community-acquired urinary tract infections: an increasing challengeforantimicrobialtherapy.Infection.2011;39:333---40. 19.TenoverFC.Mechanismsofantimicrobialresistanceinbacteria.
AmJInfectControl.2006;34:S3---10.
20.Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Hsueh PR, Paterson DL. Emergence of high levels of extended-spectrum-beta-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the Study for Monitor-ing Antimicrobial Resistance Trends (SMART) program, 2007. AntimicrobAgentsChemother.2009;53:3280---4.
21.Oteo J, Pérez-Vázquez M, Campos J. Extended-spectrum [beta]-lactamase producing Escherichia coli: changing epi-demiologyandclinicalimpact.CurrOpinInfectDis.2010;23: 320---6.
22.BenSlamaK,JouiniA,BenSallemR,SomaloS,SáenzY,Estepa V,etal.Prevalenceofbroad-spectrumcephalosporin-resistant
EscherichiacoliisolatesinfoodsamplesinTunisia,and charac-terizationofintegronsandantimicrobialresistancemechanisms implicated.IntJFoodMicrobiol.2010;137:281---6.
23.Rodríguez-Ba˜no J, López-Cerero L, Navarro MD, Díaz de Alba P, Pascual A. Faecal carriage of extended-spectrum beta-lactamase-producing Escherichia coli: prevalence, risk factorsandmolecularepidemiology.JAntimicrobChemother. 2008;62:1142---9.
24.ReinthalerFF,FeierlG,GallerH,HaasD,LeitnerE,MascherF, etal.ESBL-producingE.coliinAustriansewagesludge.Water Res.2010;44:1981---5.
26.ChengCH,TsaiMH,HuangYC,SuLH,TsauYK,LinCJ,etal. Antibiotic resistancepatterns ofcommunity-acquiredurinary tractinfectionsinchildrenwithvesicoureteralrefluxreceiving prophylacticantibiotictherapy.Pediatrics.2008;122:1212---7. 27.Rodríguez-Ba˜no J, Picón E, Gijón P, Hernández JR, Ruíz
M, Pe˜na C, et al. Community-onset bacteremia due to extended-spectrumbeta-lactamase-producingEscherichiacoli: riskfactorsandprognosis.ClinInfectDis.2010;50:40---8. 28.Özc¸akar ZB, Yalc¸ınkaya F, Kavaz A, Kadıo˘glu G, Elhan AH,
AysevD,etal.UrinarytractinfectionsowingtoESBL-producing
bacteria:microorganismschange–clinicalpatterndoesnot.Acta Paediatr.2011;100:e61---4.
29.Picozzi SC, Casellato S, Rossini M, Paola G, Tejada M, Costa E, et al. Extended-spectrum beta-lactamase-positive
Escherichiacolicausingcomplicatedupperurinarytract infec-tion:urologistshouldactintime.UrolAnn.2014;6:107---12. 30.KizilcaO,SiraneciR,YilmazA,HatipogluN,OzturkE,KiyakA,