www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
Validation
of
two
US
risk
scores
for
percutaneous
coronary
intervention
in
a
single-center
Portuguese
population
of
patients
with
acute
coronary
syndrome
Ana
T.
Timóteo
a,∗,
André
V.
Monteiro
a,
Guilherme
Portugal
a,
Pedro
Teixeira
a,
Helena
Aidos
b,c,
Maria
L.
Ferreira
a,
Rui
C.
Ferreira
aaCardiologyDepartment,SantaMartaHospital,CentroHospitalardeLisboaCentral,Lisbon,Portugal bMinalytics,AdvancedSolutionsforDataMiningandAnalytics,Lisbon,Portugal
cInstitutodeTelecomunicac¸ões,InstitutoSuperiorTécnico,Lisbon,Portugal
Received4May2015;accepted13September2015 Availableonline1February2016
KEYWORDS Riskstratification; Scores; Acutecoronary syndromes; Coronaryangioplasty Abstract
Introduction:NewscoreshavebeendevelopedandvalidatedintheUSforin-hospitalmortality riskstratificationinpatientsundergoingcoronaryangioplasty:theNationalCardiovascularData Registry(NCDR)riskscoreandtheMayoClinicRiskScore(MCRS).Wesoughttovalidatethese scores inaEuropean populationwithacute coronarysyndrome(ACS)andtocompare their predictiveaccuracywiththatoftheGRACEriskscore.
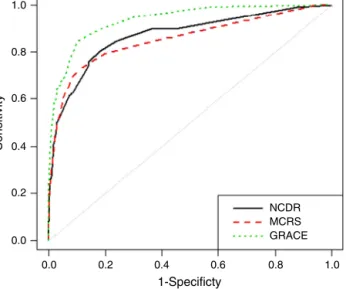
Methods:Inasingle-centerACSregistryofpatientsundergoingcoronaryangioplasty,weused theareaunderthereceiveroperatingcharacteristiccurve(AUC),agraphicalrepresentation of observed vs. expected mortality, andnet reclassification improvement (NRI)/integrated discriminationimprovement(IDI)analysistocomparethescores.
Results:Atotalof2148consecutivepatientswereincluded,meanage63years(SD13),74% maleand71%withST-segmentelevationACS.In-hospitalmortalitywas4.5%.TheGRACEscore showedthebestAUC(0.94,95%CI0.91---0.96)comparedwithNCDR(0.87,95%CI0.83---0.91, p=0.0003)andMCRS(0.85,95%CI0.81---0.90,p=0.0003).Inmodelcalibrationanalysis,GRACE showedthebestpredictivepower.WithGRACE,patientsweremoreoftencorrectlyclassified thanwithMCRS(NRI78.7,95%CI59.6---97.7;IDI0.136,95%CI0.073---0.199)orNCDR(NRI79.2, 95%CI60.2---98.2;IDI0.148,95%CI0.087---0.209).
Conclusion: TheNCDRandMayoClinicriskscoresareusefulforriskstratificationofin-hospital mortalityinaEuropeanpopulationofpatientswithACSundergoingcoronaryangioplasty. How-ever,theGRACEscoreisstilltobepreferred.
© 2016SociedadePortuguesade Cardiologia.Publishedby ElsevierEspaña,S.L.U.Allrights reserved.
∗Correspondingauthor.
E-mailaddress:anatimoteo@yahoo.com(A.T.Timóteo).
http://dx.doi.org/10.1016/j.repc.2015.09.018
PALAVRAS-CHAVE Estratificac¸ão derisco; Scores; Síndromescoronárias agudas; Angioplastia coronária
Validac¸ãodedoisscoresderiscoamericanosparaaintervenc¸ãocoronária percutâneanumestudounicêntricodapopulac¸ãoportuguesaparadoentes comsíndromecoronáriaaguda
Resumo
Introduc¸ão:ForamvalidadosnovosscoresnosEUparaestratificac¸ãoderiscodemortalidade hospitalarem doentessubmetidos aangioplastiacoronária:daNationalCardiovascular Data Registry(NCDR)edaMayoClinic(MC).Procurámosvalidarestesscoresnumapopulac¸ãoEuropeia comSíndrome CoronáriaAguda (SCA)ecomparar asuaacuidade preditiva comoscore de GRACE.
Métodos: RegistodeSCAdeumúnicocentrodedoentessubmetidosaangioplastiacoronária. Utilizaram-seascurvasReceiverOperatingCharacteristics(ROC)eaAreaUnderCurve(AUC), amortalidadeobservadaeesperadaeaanálisedoNetReclassificationIndex(NRI)/Integrated DiscriminationImprovement(IDI).
Resultados: Foramincluídos2148doentesconsecutivos.Idademédiade63(DP13)anos,74% dosexomasculinoe71%comSCAcomelevac¸ãoST.Amortalidadehospitalarfoide4,5%.Oscore
GRACEfoioquemostroumelhorAUC(0,94,IC95%0,91---0,96)comparativamentecomoNCDR (0,87,IC95%0,83--- 0,91,p=0,0003)eoMC(0,85,IC95%0,81---0,90,p=0,0003).Naanáliseda calibrac¸ão,oGRACEmostrouomelhorpoderpreditivo.ComoscoreGRACE,osdoentesforam mais corretamenteclassificados comparativamentecom odaMayo Clinic(NRI78,7, IC 95% 59,6---97,7;IDI0,136,IC95%0,073---0,199)eNCDR(NRI79,2,IC95%60,2---98,2;IDI0,148, IC95%0,087---0,209).
Conclusão:OsscoresNCDReMCsãoúteisnaestratificac¸ãoderiscoparamortalidadehospitalar numapopulac¸ãoeuropeiadedoentescomSCAsubmetidosaangioplastiacoronária.Contudo, oscoreGRACEcontinuaaseroideal.
©2016SociedadePortuguesadeCardiologia.PublicadoporElsevierEspaña,S.L.U.Todosos direitosreservados.
Introduction
Riskstratification isessentialinthemanagementof acute coronarysyndromes(ACS),particularlyinnon-ST-elevation ACS. ACS patients are a heterogeneous group of patients
in terms of risk, which has important implications for
managementstrategies.Earlyriskstratificationistherefore essential.
The Global Registry of AcuteCoronary Events (GRACE) scoreisthemostwidelyusedriskscoreduetoitshigh pre-dictiveaccuracy.1TwogroupsintheUShavedevelopedmore
recentrisk scores for stratificationof patients undergoing coronaryangioplasty,includingpatientswithACS.2,3
WesoughttovalidatetheseUSriskscoresinaEuropean populationofpatientswithACSandtocomparetheir pre-dictiveaccuracywiththatoftheclassicalGRACEriskscore.
Methods
Allconsecutiveadultpatients(aged≥18years)includedin a single-center registry on ACS between January 1, 2005 andOctober 31, 2013 wereeligible. This isa continuous, prospective and observational registry. Inclusion criteria were a history of chest pain at rest or other symptoms suggestive of an ACS within 24 hours before admission associated with new or presumed new ECG changes (sig-nificant ST-T wave changes or left bundle branch block) and/ordynamicchangesinlevelsofbiomarkersof myocar-dialnecrosis.ST-elevationmyocardialinfarction(STEMI)was
definedaspersistent (>20 minutes)ST-segmentelevation. Allothercaseswereconsiderednon-ST-elevationACS.
Datawere recordedinadatabase thatincluded demo-graphic, clinical and patient managementcharacteristics, as well as hospital outcome. Hypertension, diabetes and hyperlipidemiaweredefinedaseitherpreviouslyknownor onspecific therapy. Patientswere classifiedas smokersif theyhadsmokedduringtheprevioussixmonthsandwere self-reported.
Decisions regarding patient management strategy, includingreferralforcoronaryangiographyandmyocardial revascularization, either by percutaneous coronary inter-vention(PCI)orbycoronaryarterybypassgrafting(CABG), werelefttothediscretionoftheattendingphysician.Only patientsundergoingPCIwereeligibleforthepresentstudy. For each patient a score was retrospectively assigned according to the National Cardiovascular Data Registry (NCDR) risk score, the Mayo Clinic risk score (MCRS) and theGlobalRegistryofAcuteCoronaryEvents(GRACE) risk score.1---3
Theprimaryendpointwasall-causemortalityduringthe indexhospitalization.
Other outcomes were also recorded in the study pop-ulation: stroke/transient ischemic attack (TIA) and major bleeding. Stroke/TIA was defined as the presence of new neurological symptoms with signs of ischemia or bleeding on computed tomography or magnetic reso-nance imaging. Major bleeding was defined according to the Global Use of Strategies to Open Occluded Coro-nary Arteries (GUSTO) criteria asintracranial bleedingor
bleeding that caused hemodynamic compromise requiring intervention.4
Informed consentwasobtainedfromeachpatient.The studyprotocolconformstotheethicalguidelinesofthe1975 DeclarationofHelsinkiandwasapprovedbytheinstitution’s humanresearchcommittee.
Statisticalanalysis
Categoricalvariablesarereportedaspercentagesand con-tinuousvariablesasmeans(standarddeviation[SD]).
Concerningthevariablesincludedintheriskscores,we foundmissingdatain6.6%ofpatientsforheartrate,6.3% forsystolicbloodpressureand3.7%forcreatinineon admis-sion in the study population. Qualitative left ventricular ejection fractionwas also missingin 8.3%. A missing val-uesanalysiswasperformed,whichshowedthatthesevalues weremissingcompletely atrandom, which wasconfirmed byLittle’sMCARtest(p=0.137).Amultipleimputation tech-nique basedonaMarkov chainMonteCarloapproachwas usedtoestimate themissingvalues for each ofthe miss-ing data points in the study, including death. A primary modelincludedimputedvariables,withasecondarymodel that excluded patients with missing variables to deter-mine the consistency of the general findings with each approach.Theimputationofmissingvaluesdidnotchange themeansofthevariables.
Goodness of fit for each model was assessed with the Hosmer-Lemeshowtest.Inthistest,ahigh(non-significant) p-valueindicatesthatthemodelisperformingwellandhas a good fit. Since we aimed to compare different models usingthesamedataandpredictingthesameoutcome,we also analyzed and compared pseudo R-squared statistics. A higher pseudo R-squared value indicates which model better predicts the outcome. Discriminative ability was assessed by the area under the ROC (receiver operating characteristic) curve (AUC). The AUC provides a measure ofthemodel’sabilitytodiscriminatebetweensubjectswho experiencetheoutcomeofinterestandthosewhodonot. TocomparetheAUCofeachof thesemodels,themethod describedbyDeLongetal.wasused.5Calibrationwastested
withacomparisonoftheobservedfrequenciesofpatients withthe event of interest withthe expectedfrequencies basedonthevaluesoftheestimatedprobabilitiesobtained bythelogisticregressionmodels.
Continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI) indices were also calculated. The net proportion of patients whodied (with events) withhigherprobabilities ofdeath (NRIevents) andofpatientswhodidnotdie(withoutevents)withlower probabilitiesofdeath(NRInonevents)werecalculated consid-ering eachgroup ofmodels.NRItotal isthe sumofNRIevents andNRInoneventsandquantifiesthecorrectnessofupwardand downwardreclassificationormovement ofpredicted prob-abilities asa result of usinga different risk score.6 IDIis
a measure of the improvement in prediction and may be viewedasthedifferencebetweenimprovementinaverage sensitivityandaverage1-specificity.6
IBMSPSSStatisticssoftware(version21,Armonk,NY)was used for all statistical analyses. Model comparisons were made using the R Project for Statistical Computing open
sourceprogramming language.7---9 Allstatistical testswere
two-sidedwithavalueof0.05forstatisticalsignificance.
Results
Atotalof2148patientswereincludedinthepresentstudy. Baselinecharacteristics are detailedin Table 1. Risk fac-torsand previouscardiovascular diseasedistributionwere similartootherstudiesandACSregistries.Therewasa pre-dominanceofSTEMI.Treatmentandoutcomearepresented inTable2.There were96in-hospitaldeaths (4.5%)inthe studysample.
Table1 Baselinecharacteristicsofthestudypopulation. Overall(n=2148) Age(years) 62(13) Malegender(%) 74.1 Riskfactors(%) Hypertension 62.8 Hyperlipidemia 50.0 Diabetes 23.7 Smoking 41.9 Previoushistory(%) MI 12.5 PCI 9.7 CABG 2.7 PAD 2.8 Stroke/TIA 4.6 Initialpresentation Heartrate(bpm) 78(19) SBP(mmHg) 135(28) Killipclass>1(%) 9.7 STEMI(%) 70.9 Creatinine(mg/dl) 1.0(0.6)
CABG: coronaryarterybypassgrafting;MI: myocardial infarc-tion; PAD: peripheral arterial disease; PCI: percutaneous coronaryintervention;SBP:systolicbloodpressure;STEMI: ST-elevationmyocardialinfarction;TIA:transientischemicattack.
Table2 Treatmentandcomplications.
Overall(n=2148) Treatment(%) Aspirin 99.4 Clopidogrel 97.9 ACEI/ARB 87.9 Beta-blocker 84.5 Statin 94.6 PCI 100.0 CABG 0.2 Complications(%) Stroke 1.1 Mechanicalcomplication 2.3 Majorbleeding 1.1
ACEI:angiotensin-convertingenzymeinhibitor;ARB:angiotensin receptorblocker;CABG: coronaryarterybypassgrafting; PCI: percutaneouscoronaryintervention.
1.0 1.0 1-Specificty Sensitivity 0.8 0.8 NCDR MCRS GRACE 0.6 0.6 0.4 0.4 0.2 0.2 0.0 0.0
Figure1 Areaunderthecurveforthethreemodels.GRACE: GlobalRegistryofAcuteCoronaryEventsriskscore;MCRS:Mayo Clinicriskscore;NCDR:NationalCardiovascularDataRegistry riskscore.
TheMCRSshowedadequategoodnessoffit(p=0.337)and discriminative accuracy (AUC 0.85, 95% confidence inter-val[CI] 0.81---0.90) (Figure 1). Calibration was also good, exceptforpatientswithhighscores,inwhompredicted mor-talitywaslowerthan that observed(Figure2). The NCDR riskscorealsopresentedadequategoodnessoffit(p=0.474) andgooddiscrimination(AUC0.87,95%CI0.83---0.91). Cal-ibrationwasalmost perfect.Finally, theGRACE riskscore also showed adequate goodness of fit (p=0.482) and the highest discriminative ability (AUC 0.94, 95% 0.91---0.96) with excellent calibration. Comparing the GRACE risk score with the other scores, GRACE enabled significantly betterreclassificationofpatientsintheirriskclass,witha NRI>75%(Tables3and4).PseudoR-squaredstatistics con-firmedthatGRACEisthebestpredictiveriskscore:GRACE R2=0.497;NCDRR2=0.337;MCRSR2=0.339.
Discussion
Risk stratification is an important step in the manage-ment of ACS patients, who are a heterogeneous group in term of characteristics and risk, particularly the sub-group with non-ST-elevation ACS. It is thus essential to
Table 3 Statistics for model improvement (comparingGRACEandMayoClinicriskscores).
ContinuousNRI(%) NRIevents 27.1(8.3---45.9) NRInonevents 51.6(48.6---54.6) NRItotal 78.7(59.6---97.7) IDIstatistics 0.136(0.073---0.199) AUC(95%CI) MCRS 0.85(0.81---0.90)
GRACEriskscore 0.94(0.91---0.96)
Difference(p) <0.001
Goodnessoffit(MCRS)a 0.337
Goodnessoffit(GRACEriskscore)a 0.482
95%confidenceintervalsareshowninbrackets.
AUC:areaunderthereceiveroperatorcharacteristiccurve;IDI: integrateddiscriminationimprovement;MCRS:MayoClinicrisk score;NRI:netreclassificationimprovement.
a Hosmer-Lemeshowgoodnessoffittest(p-value).
Table 4 Statistics for model improvement (comparing
GRACE and National Cardiovascular Data Registry risk
scores). ContinuousNRI(%) NRIevents 26.0(7.3---44.8) NRInonevents 53.2(50.2---56.1) NRItotal 79.2(60.2---98.2) IDIstatistics 0.148(0.087---0.209) AUC(95%CI) NCDRriskscore 0.87(0.83---0.91)
GRACEriskscore 0.94(0.91---0.96)
Difference(p) <0.001
Goodnessoffit(NCDRriskscore)a 0.474
Goodnessoffit(GRACEriskscore)a 0.482
95%confidenceintervalsareshowninbrackets.
AUC: area under the receiver operator characteristic curve; CI:confidenceinterval;IDI:integrateddiscrimination improve-ment; NCDR: National Cardiovascular DataRegistry; NRI: net reclassificationimprovement.
a Hosmer-Lemeshowgoodnessoffittest(p-value).
performearlyriskstratificationtooptimizedecision-making for appropriate management of these patients, including thebesttimeforrevascularizationandtheideal combina-tionofantithrombotictherapies.Althoughthesetreatments
0.500 0.500 0.500 0.800 0.900 0.900 0.800 0.800 0.700 0.700 0.600 0.600 0.500 0.500 0.400 0.400 0.300 0.300 0.200 0.200 0.100 0.100 0.000 0.000 0.800 0.700 0.700 0.600 0.600 0.500 0.450 0.450 0.400 0.400 0.400 0.400 0.350 0.350 0.300 0.300 0.300 0.300 0.250 0.250
Predicted Predicted Predicted
GRACE risk score NCDR risk score
Mayo Clinic risk score
Observed0.200 Observed Observed
0.200 0.200 0.200 0.150 0.150 0.100 0.100 0.100 0.100 0.050 0.050 0.000 0.000 0.000 0.000
Figure 2 Calibration of the three scores (plots of predicted vs. observed probability of death for the three scores). NCDR:NationalCardiovascularDataRegistry.
improveoutcome,theycanincreasebothcomplicationsand costs. For this reason, informed decisions are important, andforthisriskscoresarehelpfultools.
SeveralriskstratificationscoresforACShavebeen pub-lished sincethe 1990s.The first was the TIMI risk scores for STEMIandunstable angina/non-STEMI.10,11 These were
developedfromcohortsofpatientsincludedinrandomized clinicaltrials(RCTs).ThelaterPURSUITriskscorewasalso based onan RCT, which can limit itsapplication anduse becausereal-worldcohortshavedifferentcharacteristics.12
The GRACE risk score1 was published in 2003, based
on the GRACE multicenter ACS registry database that includedthewholespectrumofACS,reflectingareal-world cohortofpatients.Duetoitshighpredictiveaccuracyitis nowadaysthemostwidelyusedriskscoreinACS.13
Morerecently,boththeMayoClinicandtheNational Car-diovascularDataRegistrydevelopedriskscoresforpatients undergoing coronary angioplasty.2,3 Both scores included
patientswithACS.AlthoughtheseUSscoresweredeveloped fromPCIregistries,thevariablesselectedweremainly clini-calinnature;noangiographicdatawasusedforriskscoring. Thus,thevariables selectedfor thesenewriskscores are very similar to those usedin the GRACE risk score. Both scoreshave beenvalidatedinUS populations,14 but notin
European populations, particularlyin the context of ACS, andsowesoughttovalidatebothriskscoresandtocompare themwiththeclassicalGRACEriskscore.
Allthescoresshowedmoderatepredictiveaccuracyfor in-hospital all-causemortality. However,the GRACE score hadthebestperformance,withsignificantlybetter discrim-inativeaccuracyasshownbyROCcurveanalysis.SinceROC curveanalysisisconsidered insufficienttocompare differ-ent prediction models, it is recommended to perform a reclassification study of one model compared to another. Patientreclassification wasbetter forGRACE accordingto theirobservedrisk,thatis,patientswitheventsweremore oftencorrectlyreclassifiedtoahigherrisklevelandpatients withouteventstoalowerrisklevel.
Thereareseveralpossibleexplanationsfortheseresults. Firstly,theUS scores werenotdeveloped fromcohortsof patients with ACS but from larger registries of patients undergoingPCI.Inthesestudygroups, only25---40%of the patientshad ACS.2,3,14 This explains severaldifferent
clin-ical characteristics of the patients in both US registries comparedtoourpopulationofpatientswithACS:our pop-ulationhasfewerfemales,fewerdiabeticpatientsandless previous history of myocardial infarction, PCI, peripheral arterialdiseaseandcerebrovasculardisease.Therewasalso a significant proportion of patients with STEMI, which is alsoanimportantdifferencecomparedtoothercohortsof ACS patients. In addition, the scores were developed for medium-term mortality (30-day and 1-year) and we vali-datedthemforshort-termmortality(in-hospital).
Limitations
Ourstudyhassomelimitations.Althoughourstudy popula-tionwasobtained fromaclinical registryasfor theMayo Clinic,NCDRandGRACEriskscores,theobservationaland non-randomizednatureofthestudymightlimitour conclu-sions,particularlyforotherEuropeancohortswithdifferent
characteristics.OnlypatientsundergoingPCIwereincluded inthe study cohort.Thus ourresults donotapply toACS patients who were not revascularized. Furthermore, our studypopulationissomewhatdifferentfromothercohorts, particularlyitspredominanceofSTEMIpatients(70.9%),and thus our results cannot be directly extrapolated to other cohorts.
Conclusions
InalargeEuropeancohortofpatientswithACS,theNCDR score and the MCRS are useful for in-hospital mortality riskstratificationinpatientsundergoingPCI.However,the GRACErisk score hasthe bestpredictive accuracy and as suchitshouldremainthepreferredriskstratificationscore.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the Global Registry of Acute Coronary Events.ArchInternMed.2003;163:2345---53.
2.PetersonED,DaiD,DeLongER,etal.,onbehalfoftheNCDR RegistryParticipants.Contemporary mortalityriskprediction forpercutaneouscoronaryintervention.Resultsfrom588,398 proceduresintheNationalCardiovascularDataRegistry.JAm CollCardiol.2010;55:1923---32.
3.SinghM,RihalCS,LennonRJ,etal.Bedsideestimatesofrisk frompercutaneouscoronaryinterventions:thenewMayoClinic riskscores.MayoClinProc.2007;82:701---8.
4.Sabatine MS, Morrow DA, Giugliano RP, et al. Association ofhemoglobinlevelswithclinicaloutcomesinacutecoronary syndromes.Circulation.2005;111:2042---9.
5.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areasundertwoormorecorrelatedreceiveroperating char-acteristic curves: a non-parametric approach. Biometrics. 1988;44:837---45.
6.PencinaMJ,D’AgostinoRB,SteyerbergEW.Extensions ofnet reclassification improvement calculations tomeasure useful-nessofnewbiomarkers.StatMed.2011;30:11---21.
7.R Development Core Team. R: a language and environ-ment for statistical computing. Vienna, Austria: R Foun-dation for Statistical Computing; 2008, ISBN 3-900051-07-0 http://www.R-project.org
8.Kundu S, Aulchencko YS, van Duijn CM, et al. PredictABLE: an R packagefor the assessmentof risk prediction models. EurJEpidemiol.2011;26:261---4.
9.Robin X, Turck N, Hainard A, et al. pROC: an open-source packageforRandS+toanalyzeandcompareROCcurves.BMC Biometrics.2011;12:77.
10.AntmanEM,CohenM,BernikPJLM,etal.TheTIMIriskscore forunstableangina/non-STelevationmyocardialMI:amethod for prognostication and therapeutic decision making.JAMA. 2000;284:835---42.
11.MorrowDA,AntmanEM,CharlesworthA,etal.TIMIriskscorefor ST-elevationmyocardialinfarction:aconvenient,bedside, clin-icalscoreforriskassessmentatpresentation:anintravenous nPAfortreatmentofinfarctingmyocardiumearlyIItrial sub-study.Circulation.2000;102:2031---7.
12.Boersma E, Pieper KS, Steyerberg EW, et al., for the PURSUITInvestigators.Predictorsofoutcomeinpatientswith acutecoronarysyndromeswithoutpersistentST-segment ele-vation. Results from aninternational trialof 9461 patients. Circulation.2000;101:2557---67.
13.de Araujo Gonc¸alves P, Ferreira J, Aguiar C, et al. TIMI, PURSUIT,andGRACEriskscores:sustainedprognosticvalueand
interaction withrevascularization in NSTE-ACS. EurHeart J. 2005;26:865---72.
14.Singh M, Peterson ED, Milford-Beland S, et al. Validation of the Mayo Clinic risk score for in-hospital mortality afterpercutaneous coronaryinterventionsusingtheNational Cardiovascular Data Registry. Circ Cardiovasc Intervent. 2008;1:36---44.