w w w . e l s e v i e r . p t / r p s p
Original
article
Drug
utilization
research
in
a
primary
mental
health
service
in
Northeast
of
Brazil
Thais
Teles
de
Souza
a,
Wellington
Barros
da
Silva
b,
Jullyana
de
Souza
Siqueira
Quintans
c,
Alexandre
Sherlley
Casimiro
Onofre
d,
Fabiana
Botelho
de
Miranda
Onofre
d,
Lucindo
José
Quintans-Júnior
e,∗aProgramadePós-graduac¸ãoemCiênciasFarmacêuticas,UniversidadeFederaldoParaná,Brazil bDepartamentodeFisiologia,UniversidadeFederaldeSergipe,Brazil
cCampusdeCiênciasdaSaúdedeLagarto,UniversidadeFederaldeSergipe,Brazil dDepartamentodeFisiologia,UniversidadeFederaldeSergipe,Brazil
eDepartamentodeFisiologia,UniversidadeFederaldeSergipe,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:Received30May2011
Accepted20March2012
Availableonline15May2012
Keywords:
Psychosocialcarecenter
Drugutilizationresearch
Mentalhealth
a
b
s
t
r
a
c
t
ThePsychosocialCareCenter(CAPS)isacommunity-basedmentalhealthserviceinBrazil,
whichaimstopromotethepsychosocialrehabilitationofpatients.Accordingly,thisstudy
describesthedruguseevaluationinaprimarymentalhealthserviceinNortheastofBrazil.
Setting:CAPS‘ValterCorreia’,SãoCristovão,Sergipe,Brazil.
Methods:Across-sectionalstudywasconductedbetweenAugust2009andMay2010.
Ini-tially,Medicalrecordswerereviewedandevaluated.Then,weappliedinterviewswiththe
patients(and/ortheirinformal/familycaregivers)attendedattheCAPS.Informationswere
obtainedregardingtodemographicandclinicalfeatures,diagnosesanddrugsprescribed.
AllpatientsregisteredintheCAPSwereincludedinthestudy.Theresultswerestatistically
analyzedusingtheEpiInfoandwerecomparedwithresultsfromliterature.
Results:TheCAPS‘ValterCorreia’consistsof101registeredpatients,themajorityweremale
(58.4%),illiterate(51.5%),withoutmonthlyincome(49.5%)andtheaverageageofthem42.2
years(SD=12.0).Schizophreniawasthemostfrequentmentaldisorder(31.5%).Theaverage
numberofmedicationsbypatientswas3.11(SD=1.41),andtheoldergroupofpatients
(75-80years)presentedthelargestconsumptionofmedications(5.50drugs/patient).The
psychiatricdrugclassmostfrequentlyprescribedwasantipsychotics(44.8%).
Angiotensin-convertingenzymeinhibitorswerethemostprevalentnon-psychiatrictherapeuticclass
(15.8%).Itwasdetected133drug-druginteractions(3.0%mild,54.1%moderate,29.3%severe
and13.5%contraindicated).
Conclusion: Theresultsrevealedtheneedformonitoringthepharmacotherapyofpatients
withmentaldisorderstoencouragetherationaluseofmedications.
©2011EscolaNacionaldeSaúdePública.PublishedbyElsevierEspaña,S.L.Allrights
reserved.
∗ Correspondingauthor.
E-mailaddresses:lucindo jr@yahoo.com.br,lucindo@pq.cnpq.br(L.J.Quintans-Júnior).
0870-9025/$–seefrontmatter©2011EscolaNacionaldeSaúdePública.PublishedbyElsevierEspaña,S.L.Allrightsreserved.
Estudo
de
utilizac¸ão
de
medicamentos
em
um
servic¸o
de
saúde
mental
primário
no
Nordeste
do
Brasil
Palavraschave:
CentrodeAtenc¸ãoPsicossocial
EstudodeUtilizac¸ão
demedicamentos
SaúdeMental
R
e
s
u
m
o
OCentrodeAtenc¸ãoPsicossocial(CAPS)éumservic¸odesaúdementaldebasecomunitária
noBrasil,quevisapromoverareabilitac¸ãopsicossocialdospacientes.Opresenteestudo
descreveaavaliac¸ãodousodemedicamentosemumservicedesaúdementalprimáriono
NordestedoBrasil.
Ambiente:CAPS«ValterCorreia»,SãoCristovão,Sergipe,Brasil.
Métodos:Estudotransversalfoirealizadoentreagostode2009emaiode2010.Inicialmente,
osregistrosmédicosforamrevisadoseavaliados.Emseguida,foramrealizadasentrevistas
comospacientes(e/ouseuscuidadores)atendidosnoCAPS.Informac¸õesforamobtidas
sobreascaracterísticasdemográficaseclínicas,diagnósticosemedicamentosprescritos.
TodosospacientescadastradosnoCAPSforamincluídosnoestudo.Osresultadosforam
analisadosestatisticamenteutilizandooprogramaEpiInfoeforamcomparadoscomos
resultadosdaliteratura.
Resultados:OCAPS“ValterCorreia”écompostopor101pacientescadastrados,amaioriado
sexomasculino(58,4%),analfabetos(51,5%),semrendamensal(49,5%)eamédiadeidade
deleserade42,2anos(DP=12,0).Aesquizofreniafoiotranstornomentalmaisfreqüente
(31,5%).Onúmeromédiodemedicamentosporpacientesfoide3,11(DP=1,41),eogrupo
depacientesmaisvelhos(75-80anos)apresentouomaiorconsumodemedicamentos(5,50
medicamentos/paciente).Aclassedemedicamentospsiquiátricosmaisprescritafoiados
antipsicóticos(44,8%).Aclassedosinibidoresdaenzimaconversoradaangiotensinafoia
maisprevalenteclassenão-psiquiátrica(15,8%).Foramdetectadas133interac¸ões
medica-mentosasfármaco-fármaco(3,0%deseveridadeleve,54,1%moderada,29,3%gravee13,5%
contra-indicada).
Conclusão:Osresultadosdemonstramanecessidadedeacompanhamentoda
farmacoter-apiadepacientescomtranstornosmentaisparaincentivarousoracionaldemedicamentos.
©2011EscolaNacionaldeSaúdePública.PublicadoporElsevierEspaña,S.L.Todosos
direitosreservados.
Introduction
Mentaldisorders representahealthproblemofsocial
rele-vancefortheirhighincidenceinpopulationsfromdifferent
countries and culturally distinct societies. We estimated
17–35%prevalenceofmentaldisordersinBrazilian
popula-tion.However,thesedisordersarestillfarfromreceivingan
adequateimportance.1–4
Inthiscontext,theintroductionofpsychosocialcare
cen-ters(CAPS)wereoneofsomehealthservicescreated,basedon
Brazilianpsychiatricreform.TheCAPSarecharacterizedbya
daycareservice,whichisproposedasanalternativetoa
psy-chiatrichospital.Itsmainobjectiveistoofferapsychosocial
rehabilitationtotheirpatients.5
The sociodemographic characteristics of CAPS patients
haveanimportantinfluencetoimprove theirassistance.2,6
Moreover, psychotropicdrugs cause adverse events,which
compromisestheadherencetotreatmentandthenthequality
oflife.7
Somestudieshavedemonstratedtherelationshipbetween
theprocessofuseofdrugs,morbidityandmortalityrelated
todrugsandasthesemaytriggeradversereactions.Inthese
studies,problemssuchasadversereactions,non-compliance,
overdoseorinadequatetherapyarefactorsthatleadtofailure
oftherapy.Ifthisisnotdetectedandresolved,itcanleadto
death.8–15
Thus,itisnecessarytoevaluatethedrugutilizationin
men-talhealthcareinordertoassessdrugtherapy,detecttherisk
factorsassociatedwiththeuseofmedicationsandpromote
therationaluseofdrugs.Drugutilizationresearcharedefined,
accordingtoWHO,asstudiesonmarketing,distribution,
pre-scription,anduseofdrugsinasociety,withspecialemphasis
ontheresultingmedical,socialandeconomicconsequences.
Thesestudieshaveastheirmainobjectivethepromotionof
therationaluseofdrugs.16,17
In recent years, literature has highlighted the
involve-mentofthepharmacistinprogramstooptimizetheeffects
of medications, through monitoring the use of drugs. The
applicationofrationalcriteriacanensuregreatercompliance
withtherapy,effectivenessandsafetyofmedicationsusedby
patients.18–20
Aim
of
study
Thepresentstudyaimedtoevaluatetheuseofmedications
bypatientsinaprimarymentalhealthservicelocatedinacity
attheNortheastofBrazil.
Methods
Weconducted,inanunprecedentedwayinSergipestate,a
typeIpsychosocialcarecenter(CAPS)‘ValterCorreia’inSão
Cristovão,Sergipe,Brazil.AllpatientsregisteredintheCAPS
(and/ortheirinformal/familycaregivers)wereincludedinthe
study.
CAPS type I is a unit for own psychosocial care with
therapeuticworkshopsand otherformsofcareand
opera-tionalcapacitytoprovidehealthcarecoveragetoapopulation
between20,000and 70,000inhabitants,workingundertwo
shifts,developingdailyactivitiesinmentalhealth.21
Data was collected from patient medical records, such
associodemographics,clinicalcharacteristicsand
pharmaco-logicaltreatments.Sociodemographicdataincludedpatient
gender,age,educationalstatus,occupationalactivity,benefits
orpensions,incomeandmaritalstatus.Diagnoses
(accord-ingtotheICD-10 internationalclassificationofmentaland
behavioraldisorders)22 and thepatient’s psychiatric
admis-sionhistoryweretheclinicalcharacteristicsobtained.Details
ofallpsychiatricprescribedmedicationswerealsocollected,
including dose, frequency, administrationroutes and
ther-apeutic indications. Drugswere classified accordingto the
anatomicaltherapeuticchemical(ATC)classificationsystem
andthedefineddailydose(DDD).TheATC/DDDsystemisa
widelyusedtoolforexchangingandcomparingdataondrug
consumptionatinternational,nationalorlocallevels.23
Inaddition,personalinterviewswereperformed(appliedto
thepatientsand/ortheirinformal/familycaregivers)and
col-lectiveinterviews(appliedtogroupsofpatientsand/ortheir
informal/familycaregivers),inordertocompareinformations
registered on records, collect the missing data on records,
identifyfeaturesontheuseofmedicationsandcharacterize
theperceptionofpatients abouttheirhealthproblemsand
theirtreatments.Theinterviewswereconductedbya
gradu-atestudentinpharmacy,previouslytrained.
TheprotocolswereapprovedbytheEthicsCommitteeon
HumanResearchattheFederalUniversityofSergipe.Patients
participatinginthestudywereinformedabouteverystepand
agreedtoparticipateinthesurveythroughatermofinformed
consent.
The programs EPI-INFO (version 3.5.1-obtained from
www.cdc.gov/EpiInfo)andExcel(Microsoft®)wereusedto
sta-tisticalanalysis.ThestudyprotocolwasapprovedbytheEthics
CommitteeofFederalUniversityofSergipe.
Duringthedevelopmentofthisstudy,itwas ministered
lectures,homevisits,workshopsandmeetingsforpatients,
informal/familycaregivers,andforthemultidisciplinaryteam
of the CAPS. The themes approached the rational use of
medications,mentaldisorder, psychopharmacology,
medic-inal plants, hygiene, handicraft, culture, integration, social
inclusion,first aid and use ofalcohol, tobacco and others
drugs.
Results
101registeredpatientsweredistributedinintensive(13.86%),
semi-intensive(52.48%)andnon-intensive(33.66%)regimeat
CAPSValterCorreia.Thoseregimesaredefinedbytheir
clini-calconditions,basedonclinicalcareandtherapyofpatients.
According to their needs, patients belonging to intensive
regimerequire dailycarebyaspecialized multidisciplinary
Table1–Sociodemographicsdataofpatientsattendedat
CAPSValterCorreia(n=101).
Variables AF(RF%)* Gender Male 59(58.40) Female 42 (41.60) Educationalstatus Analphabet 52(51.50)
Uncompletedprimaryschool 36(35.60) Primaryschool 1(0.99) Uncompletedsecondaryschool 8(7.90) Secondaryschool 4(3.96) Occupationalactivity None 91(90.10) Housemaid 1(0.99) Homemaker 4(3.96) Bricklayer 2(1.98) Fishman 3(2.97) Benefit/pensions Receive 51(50.50) Noreceive 50(49.50) Income(monthly) Noincome 50(49.50) 1minimumwage($28,736) 49(48.50) 2minimumwage($57,471) 1(0.99) 3minimumwage($86,207) 1(0.99) Maritalstatus Single 77(76.20)
Marriedorlivingasmarried 17(16.80)
Divorced 2 (1.98)
Widowed 5(4.95)
∗ AF–Absolutefrequency,RF%–Relativefrequencyinpercentage.
team (up to 25 days/month), patients belonging to
semi-intensiveregimerequirefrequentcare(upto12days/month)
andpatientsbelongingtonon-intensiveregimerequireless
frequentattendance(upto3daysofthemonth).
The mean age of patients was 42.18±12.01-years-old,
medianof42years.Table1describesthedistributionofother
importantsocio-demographicparameters.
Schizophrenia was the most prevalent mental disorder
(31.53%).Thementaldisorderprofilepresentedbythepatients
attendedontheCAPS,accordingwiththeinternational
clas-sification of mental and behavioral disorders (ICD-10)22 is
describedinTable2.
Somepatientspresentedotherdiseasesassociatedto
men-taldisorders,suchasarterialhypertension(18.81%),diabetes
mellitus(10.9%),gastritis(10.9%),asthma(4.0%),othersheart
problems(7.9%)andhypothyroidism(2.2%).
Regarding to the pharmacotherapeutic profile, Table 3
exhibits the therapeutic classes of psychiatric drugs used
by patients attended at CAPS. Table 4 describes the
the-rapeutic classes of non-psychiatricdrugs used by patients
attendedatCAPS,accordingtotheWHO-ATC/DDD
method-ology.Thepsychiatricdrugclassmostfrequentlyprescribed
wasantipsychotics(44.8%)andthenon-psychiatricdrugclass
mostprevalentwasangiotensin-convertingenzymeinhibitors
Table2–MentaldisordersdiagnosedatCAPSpatients
accordingtoICD-10(n=101).
ICD Mentaldisorders AF(RF%)a
F06 Othermentaldisordersdue tobraindamageanddysfunction andtophysicaldisease
5(4.50)
F10 Mentalandbehaviouraldisorders duetouseofalcohol
20 (18.02) F20 Schizophrenia 35(31.53) F21 Schizotypaldisorder 3(2.70) F25 Schizoaffectivedisorders 3(2.70) F29 Unspecifiednonorganicpsychosis 8(7.21) F31 Bipolaraffectivedisorder 7(6.31) F32 Depressiveepisode 1(0.90) F71 Moderatementalretardation 9(8.11) F72 Severementalretardation 4(3.60)
G40 Epilepsy 4(3.60)
Others 12(10.81)
Total 111(100)b
a AF– Absolutefrequency,RF%– Relativefrequencyinpercentage. b Itisobservedthatsomepatientshavemorethanonemental
disorder.
Table3–Therapeuticclassesofpsychotropicdrugsused
bypatientsattendedatCAPSValterCorreia,accordingto
ATCclassification.
ATC Therapeuticclass AF(RF%)*
N03A ANTIEPILEPTICS 26(9.63) N03AA Barbituratesandderivatives 12 (4.44) N03AB Hydantoinderivatives 2(0.74) N03AE Benzodiazepinederivatives 8(2.96) N03AF Carboxamidederivatives 16(5.93) N04A ANTICHOLINERGICAGENTS 18(6.67) N04AA Tertiaryamines 18(6.67) N05A ANTIPSYCHOTICS 121(44.81) N05AA Phenothiazineswithaliphatic
side-chain
46(17.04) N05AC Phenothiazineswithpiperidine
structure
6(2.22) N05AD Butyrophenonederivatives 65(24.07)
N05AN Lithium 2(0.74)
N05AX Otherantipsychotics 2(0.74) N05B ANXIOLYTICS 22(8.15) N05BA Benzodiazepinederivatives 22(8.15) N06A ANTIDEPRESSANTS 23(8.52) N06AA Non-selectivemonoamine
reuptakeinhibitors
16(5.93) N06AB Selectiveserotoninreuptake
inhibitors
7(2.59) R06A ANTIHISTAMINESFORSYSTEMIC
USE
43(15.93) R06AD Phenothiazinederivatives 43(15.93) V03A ALLOTHERTHERAPEUTIC
PRODUCTS
5(1.85) V03AA Drugsfortreatmentofchronic
alcoholism
5(1.85)
Total 219(100)
∗ AF–Absolutefrequency,RF%–Relativefrequencyinpercentage.
Table4–Therapeuticclassesofnon-psychotropicdrugs
usedbypatientsattendedatCAPSValterCorreia,
accordingtoATCclassification.
ATC Therapeuticclass AF(RF%)*
A02B Drugsfortreatmentofpepticulcer 3(7.89) A04A Antiemeticsandantinauseants 2(5.26) A06A Laxatives 2(5.26) A07D Antipropulsives 1(2.63) A10B Oralbloodglucoseloweringdrugs 1(2.63) B03A Ironpreparations 1(2.63) B03B VitaminB12andfolicacid 2(5.26) C01D Vasodilatorsusedincardiac
diseases
1(2.63) C02A Antiadrenergicagents,centrally
acting
1(2.63) C03A Low-ceilingdiuretics,thiazides 1(2.63) C03C High-ceilingdiuretics 1(2.63) C07A Betablockingagents 3(7.89) C09A Aceinhibitors,plain 6(15.79) C09C AngiotensinIIantagonists,plain 1(2.63) G03A Hormonalcontraceptives
forsystemicuse
1(2.63) G03G Gonadotropinsandother
ovulationstimulants
1(2.63) G04B Otherurologicals,incl.
antispasmodics
1(2.63) H02A Corticosteroidsforsystemicuse,
plain
1(2.63) M03A Musclerelaxants,peripherally
actingagents
3(7.89) R03A Adrenergics,inhalants 1 (2.63) R03C Adrenergicsforsystemicuse 1(2.63) R03D Otheranti-asthmaticsforsystemic
use
1(2.63) R05C Expectorants,excl.combinations
withcoughsuppressants
1(2.63) R06A Antihistaminesforsystemicuse 1(2.63)
Total 38(100)
∗ AF–Absolutefrequency,RF%–Relativefrequencyinpercentage.
The average number of medications (psychotropic and
non-psychotropic) usedbypatientswas3.11±1.41
medica-tions/patients,median3(Table5).
Table 6 shows the percentage ofdrug interactions
pre-sented bypacientsoftheCAPS,according tothedegreeof
severity.
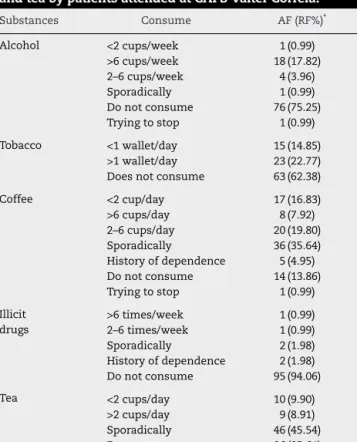
With respecttoconsumptionof otherssubstances, it is
observedinTable7theprofileofusealcohol,tobacco,illicit
drugsandteas.
Discussion
TheCAPSisanopenandcommunityserviceofmentalhealth
ontheunifiedhealthsystem(SUS)inBrazil.Itsmainobjective
istoestablishareferenceplacetotreatmentforpeoplewith
mentaldisorders,whoneedanintensivecarerelatedtotheir
severityand/orpersistencedemand.5
101registeredpatientsatCAPS‘ValterCorreia’were
dis-tributed in intensive (13.86%), semi-intensive (52.48%) and
non-intensive (33.66%) regime.Theaverageage ofpatients
Table5–Meannumberofmedications(psychotropic
andnon-psychotropic)usedbypatientsattendedat
CAPSValterCorreia,accordingtotheagegroup.
Agegroup(years) Averageamountof
medicationsused/patient 20–24 2.33±1.21 25–29 3.89±1.17 30–34 2.82±1.01 35–39 2.62±0.96 40–44 2.91±1.20 45–49 2.70±1.42 50–54 3.88±1.96 55–59 3.50±0.71 60–64 3.00±0.71 65–69 3.00±0.00 70–74 3.00±0.00 75–80 5.50±0.00
Valuesareexpressedasmean±standarddeviation.
Table6–Druginteractions(drug–drug)presentedby
patientsattendedatCAPSValterCorreia,classifiedby
degreedseverity. Typeofinteraction AF(RF%)* Light 4(3.01%) Moderate 72(54.13%) Several 39(29.32%) Contraindicated 18(13.54%) Totaly 133(100%)
∗ AF– Absolutefrequency,RF%–Relativefrequencyinpercentage.
Table7–Consumeofalcohol,tobacco,coffee,illicitdrugs
andteabypatientsattendedatCAPSValterCorreia.
Substances Consume AF(RF%)* Alcohol <2cups/week 1(0.99) >6cups/week 18(17.82) 2–6cups/week 4(3.96) Sporadically 1(0.99) Donotconsume 76(75.25) Tryingtostop 1(0.99) Tobacco <1wallet/day 15(14.85) >1wallet/day 23(22.77) Doesnotconsume 63(62.38) Coffee <2cup/day 17(16.83) >6cups/day 8(7.92) 2–6cups/day 20(19.80) Sporadically 36 (35.64) Historyofdependence 5(4.95) Donotconsume 14(13.86) Tryingtostop 1(0.99) Illicit drugs >6times/week 1(0.99) 2–6times/week 1(0.99) Sporadically 2(1.98) Historyofdependence 2(1.98) Donotconsume 95(94.06) Tea <2cups/day 10(9.90) >2cups/day 9(8.91) Sporadically 46(45.54) Donotconsume 36(35.64)
∗ AF–Absolutefrequence,RF%–Relativefrequencyinpercentage.
otherstudies,whichclaimthatmentaldisordersaffectpeople
ofallages,withtheprevalenceon30–49years.24,25The
pres-enceofmentaldisorderatthisagegroupinfluencestheway
oflife,interruptingproductivityasaresultofdisabilitycaused
bydisease.24
ItisobservedinTable1thatthe CAPSconsistedmainly
ofmalepatients(58.50%),whichdiffersfromothersstudies
thatindicatetheprevalenceoffemales.24,26
Mostpatientsweresingle(76.20%),childless(54.50%),
illit-erate(51.50%),withoutoccupation(90.10%),withoutbenefits
(49.50%)andwithoutmonthlyincome(49.50%).Theseresults
suggestthatthepresenceofmentaldisordercaninfluencethe
culturalbackgroundofpeopleandthechancetoattendschool
islow,whichcanmakeitdifficulttoenteratuniversityand
gainagoodjob.AccordingtoOMS(2001)2,fivefromtencauses
ofinabilityontheworldarementaldisorder.
Regardingtothenosologicalprofiles,Table2revealsthat
therearepatientswithmorethanonetypeofmentaldisorder
andthatschizophreniaisthemostprevalentmentaldisorder
(31.53%).
Schizophreniaisoneofthemostseriousneuropsychiatric
diseasesandaffectsabout1%ofworldpopulation.Currently,
thereisnospecificpreventionforthisdisease.Neurolepticor
antipsychoticdrugsareusedastheprimarytreatmentforall
stagesofthedisease.27
Depressive episodes are common mental disorders on
Brazilianpopulation,28–31 butwefoundinonly0.90%ofour
CAPSpatients.Thisdifferenceshouldbecausedduetothe
introduction of a newmodel ofpsychiatric care, which is
still suffering transition in Brazil. Part of the population,
who suffers from moodand anxiety disorders, isprobably
under-diagnozed. Another part, even receiving the correct
medicaldiagnosis,choosestoreceiveambulatorytreatment
withoutresorttotheCAPS,whichcouldbeinconsequenceof
stigmasfear.
Consumption of alcohol and others drugs is an
impor-tant cause of disorder. Mental behavioral disorders due
the consumptionofalcoholwere foundin18.02%,due the
consumptionofmultipledrugsandotherspsychoactive
sub-stancesin0.90%andduetotheuseofcocainein0.90%.Those
patientsshouldbeindicatedforanADtypeofCAPS.
Thepsychiatricdrugclassmostfrequentlyprescribedwas
antipsychotics (44.8%), described in Table 3.
Angiotensin-convertingenzymeinhibitors(ACEI)werethemostprevalent
non-psychiatric drug class (15.8%) (Table 4). Those results
are in consistence with the most prevalent diseases,
schizophreniaforantipsychoticsandhypertensionforACEI
medications.
There iscurrently avery large numberof antipsychotic
medications,with differentprofileofsideeffects, but with
similarpotencywhenuseinequivalentdoses.However,there
areindividualdifferencesonefficacy,toleranceandcost.
Par-ticularcontextshouldbeusedtochoosetheadequatedrug.
Theaveragenumberofmedicationsusedbypatientswas
3.11±1.41medications/patients.Thelargestconsumptionof
medicationswasfoundinthe75–80yearsgroup,5.5
medica-tionsforpatient(Table5).Thesedataareinwiththeliterature.
Elderlypopulationismarkedbyahigherfrequencyofchronic
degenerative diseases. It has greater demand for health
populationtogreatriskswiththepracticeofpolypharmacy
andadverseeffectsofmedications.32
Inregardtodruginteractions,33–353.0%mild,54.1%
mod-erate,29.3%severeand13.5%contraindicated(Table6).Those
results demonstrate the need to evaluate possible
inter-ventions,sincedruginteractions may,amongother things,
increase undesired medications effects, lead to ineffective
therapyandendangerthelifeofpatient.36–39
ItisobservedinTable7that24.75%ofpatientsconsumed
alcohol,37.62% tobacco, 86.14%caffeine, 5.94%illicitdrugs
and64.36%tea.Itisnecessaryafurtherdetailedstudy,since
thesesubstancescaninteractwithseveralmedications.
Themedicationshaveanimportantroleinthehealth
sys-tem,theycansavelivesorremovethesignsandsymptoms
ofnumerousdiseases.40However,thedrugsmayincreasethe
costsofhealthcareifusedimproperly.41AccordingtoWHO
data,hospitalsspend15%–20%oftheirbudgetstodealwith
thecomplicationscausedbymisuseofmedications.42
In this context, pharmacists are professionals who can
activelyparticipateinthemultidisciplinaryteam,makethe
managementofpharmacotherapy,assesstheuseof
medica-tions,provideguidelines andperformpharmacotherapeutic
monitoringofpatients,whichcontributetotherationaluseof
medicationsandimprovethequalityoflifeofpatients.43
Conclusion
Our resultsrevealed the need formonitoring the
pharma-cotherapyofpatientswithmentalandbehavioraldisordersto
encouragetherationaluseofmedications.Thismonitoringis
necessary,sincethesepatientsarepolymedicated,haveother
comorbidities,andusedrugsthatcauseadverseeffects,which
compromisethe adherence oftreatment and consequently
theirqualityoflife.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
Acknowledgments
Wewouldlike tothankthe Fundac¸ãodeApoio àPesquisa
eà Inovac¸ãoTecnológica do Estadode Sergipe/FAPITEC-SE
andNational CouncilofTechnologicalandScientific
Devel-opment(ConselhoNacionaldeDesenvolvimentoCientíficoe
Tecnológico/CNPq/Brazil)forthefellowshipsupport.
r
e
f
e
r
e
n
c
e
s
1. AlvesDSN.Reestruturac¸ãodaatenc¸ãoemsaúdemental:
situac¸ãoatual:diretrizeseestratégias.In:AmaranteP,editor.
Psiquiatriasocialereformapsiquiátrica.RiodeJaneiro:
Fiocruz;1994.p.197–204.
2. Organizac¸ãoPan-AmericanadeSaúde.Organizac¸ãoMundial
daSaúde.Relatóriosobreasaúdenomundode2001:Saúde
mental:novaconcepc¸ão,novaesperanc¸a.Geneva:OPAS;2001.
3. PinheiroKAT,HortaBL,PinheiroRT,HortaLL,TerresNG,Silva
RA.Commonmentaldisordersinadolescents:apopulation
basedcross-sectionalstudy.RevBrasPsiquiatr.2007;29:241–5.
4.LimaMCP,MenezesPR,CarandinaL,CesarCLG,BarrosMBA,
GoldbaumM.Transtornosmentaiscomunseusode
psicofármacos:impactodascondic¸õessocioeconômicas.Rev
SaúdePública.2008;42:717–23.
5.MinistériodaSaúde.MinutaPortariaNAPS/CAPS,de02de
Decemberde1999,Brasília,DF:MinistériodaSaúde;1999.
6.TavaresM,TakedaS.Organizac¸ãodeServic¸osdeAtenc¸ão
PrimáriadeSaúde.In:DucanBB,SchmidtMI,PankowJS,
editors.Medicinaambulatorial:condutasclinicasematenc¸ão
primaria.2nded.PortoAlegre:ArtesMédicas;1996.p.2229.
7. LaraDR,AbreuPB.Esquizofrenia.In:KapczinskiF,QuevedoJ,
IzquierdoI,editors.Basesbiológicasdostranstornos
psiquiátricos.PortoAlegre:Artmed;2000.p.109–17.
8.BatesDW,CullenDJ,LairdN,PetersenLA,SmallSD,ServiD,
etal.Incidenceofadversedrugeventsandpotentialadverse
drugevents.JAMA.1995;274:29–34.
9.HeplerCD,StrandLM.Opportunitiesandresponsibilitiesin
pharmaceuticalcare.AmJHospPharm.1990;47:533–43.
10.ErnstFR,GrizzleAJ.Drug-relatedmorbidityandmortality:
updatingthecost-of-illnessmodel.JAmPharmAssoc(Wash).
2001;41:192–9.
11.HafnerJWJR,BelknapSM,SquillanteMD,BucheitKA.Adverse
drugeventsinemergencydepartmentpatients.AnnEmerg
Med.2002;39:258–67.
12.MorrisCJ,CantrillJA,HeplerCDP.Preventingdrugrelated
morbidity:determiningvalidindicators.IntJQualHealth
Care.2002;14:183–98.
13.Dall’AgnolRSA.Identificac¸ãoequantificac¸ãodosproblemas
relacionadoscommedicamentosempacientesquebuscam
atendimentonoservic¸odeemergênciadoHCPA.PortoAlegre:
UniversidadeFederaldoRioGrandedoSul.Faculdadede
Farmácia;2004.Dissertac¸ãodeMestradoemCiências
Farmacêuticas.
14.SpinaE,SantoroV,D’ArrigoC.Clinicallyrelevant
pharmacokineticdruginteractionswithsecond-generation
antidepressants:anupdate.ClinTher.2008;30:1206–27.
15.VillaTCS,BrunelloMEF,ArcêncioRA,SassakiCM,AssisEG,
GonzalezRIC.Fatorespreditivosaosresultadosdesfavoráveis
notratamentodatuberculose:revisãointegrativada
literatura(2001-2005).OnlineBrazilianJournalofNursing.
Specialnumberforundergraduateresearches[Internet].2008
Spring[access27April2011].Availableat:http://www.
objnursing.uff.br/index.php/nursing/issue/view/12
16.LaporteJR,TognoniG.Principiosdeepidemiología
delmedicamento.2nded.Barcelona:Masson-Salvat;1993.
17.LeiteSN,VieiraM,VeberAP.Estudosdeutilizac¸ãode
medicamentos:umasíntesedeartigospublicadosnoBrasil
eAméricaLatina.CiêncSaúdeColetiva.2008;13:793–802.
18.BrookO,HoutH,NieuwenhuyseH,HeerdinkE.Impactof
coachingbycommunitypharmacistsondrugattitude
ofdepressiveprimarycarepatientsandacceptability
topatients:arandomizedcontrolledtrial.Eur
Neuropsychopharmacol.2003;13:1–9.
19.GranadosFM,YangüasEP.Criteriosdeoptimizacióndela
terapiaantipsicótica:margenterapéutico.FarmHosp.
2004;28:214–24.
20.CostaLF,SousaLG,OliveiraAM,FonsecaCA.Atenc¸ão
farmacêuticaparaportadoresdecuidadosespeciais.REF.
2006;3:19–21.
21.MinistériodaSaúde.Portaria336/GM,de19deFebruary
de2002,Brasília,DF:OMinistério;2002.
22.WorldHealthOrganization.TheICD-10Classificationof
MentalandBehaviouralDisorders:diagnosticcriteria
forresearch.Geneva:WHO;1993.
23. WorldHealthOrganization.TheAnatomicalTherapeutic
Dose(DDD)[access:10February2012].Availableat:
http://www.whocc.no/atcdddindex/.
24.MachadoVMMC.Atuac¸ãodoenfermeirojuntoaosusuários
docentrodeatenc¸ãopsicossocialCAPSgeralnacidadede
Sobral-CE.Ceará:UniversidadeEstadualValedoAcaraú
(UVA);2006.MonografiadeEspecializacãoemSaúde
Mental.
25.CardosoL,GaleraSAF.Doentesmentaiseseuperfildeadesão
aotratamentopsicofarmacológico.RevEscEnfermUSP.
2009;43:61–7.
26.PelisoliCL,MoreiraAK.Caracterizac¸ãoepidemiológicados
usuáriosdoCentrodeAtenc¸ãoPsicossocialCasaAberta.Rev
PsiquiatrRioGdSul.2005;27:270–7.
27.PáduaAC,GamaCS,LobatoMI,AbreuPB.Esquizofrenia:
diretrizesealgoritmoparaotratamentofarmacológico.In:
CordioloAV,etal.,editors.Psicofármacos:consultarápida.
PortoAlegre:Artmed;2005.p.343.
28.RegierDA,NarrowWE,RaeDS.ThedefactoUSmental
andaddictivedisordersservicesystem:epidemiologic
catchmentareaprospective1yearprevalenceratesof
disordersandservices.ArchGenPsychiatry.1993;50:
85–94.
29.KesslerRC,McgonagleKA,ZhaoS,NelsonCB,HughesM,
EshlemanS,etal.Lifetimeand12-monthprevalenceof
DSM-IIIRpsychiatricdisordersintheUnitedStates.ArchGen
Psychiatry.1994;51:8–19.
30.JenkinsR,LewisG,BebbingtonP,BrughaT,FarrellM,GillB,
etal.TheNationalPsychiatricMorbiditySurveyofGreat
Britain:initialfindingsfromthehouseholdsurveys.Psychol
Med.1997;27:775–89.
31.AndersonIM.Selectiveserotoninreuptakeinhibitorsversus
tricyclicantidepressants:ametaanalysisofefficacy
andtolerability.JAffectDisord.2000;58:19–36.
32.AndersonGM,BeersMH,KerlukeK.Auditingprescription
practiceusingexplicitcriteriaandcomputerizeddrugbenefit
claimsdata.JEvalClinPract.1997;3:283–94.
33.BaxterK.Stockley’sdruginteractions.Chicago:Editora
PharmaceuticalPress;2009.
34.LacyCF,ArmstrongLL,GoldmanMP,LanceLL.Medicamentos
Lexi-CompManole.SãoPaulo:Ed.brasileira.Manole;2009.
35.ThomsonReutersHealthcare.Finddruginteractions
[homepagenaInternet].NewYork,NY:Micromedex
HealthcareSeries;2012[access10Jun2010].Availableat:
http://newmdx.csis.com.tw/home/dispatch
36.CamposERC,BardinaNB,VejaMA,LeeBF.Interacciones
medicamentosas:erroresenlamedicacion.RevCubaFarm.
1990;24:281–7.
37.FonsecaAL.Interac¸õesmedicamentosas.RiodeJaneiro:
EPUC;1994.
38.OgaS,BasileAC.Medicamentosesuasinterac¸ões.SãoPaulo:
Atheneu;1994.
39.NiesAS,SpielbergSE.Principlesoftherapeutics.In:Gilman’s
G,editor.Thepharmacologicalbasisoftherapeutics.9thed.
NewYork:McGraw-Hill;1996.p.43–62.
40.NoelleL.Bioethicsand21stcentury:viewpointofthejurist.
PresseMed.2002;31:565–70.
41.PepeVLE.CastroCGSO.Ainterac¸ãoentreprescritores,
dispensadoresepaciente:informac¸ãocompartilhadacomo
possívelbenefícioterapêutico.CadSaúdePública.
2000;16:815–22.
42.AgenciaNacionaldeVigilanciaSanitaria(Brasil).Parcerias
paradiminuiromauusodemedicamentos.RevSaúde
Pública.2006;40(1):191–4.
43.DolderC,SymanskiB,WootonT,MckinseyJ.Pharmacist
interventionsinaninpatientgeriatricpsychiatryunit.AmJ