www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Intensive
care
unit:
results
of
the
Newborn
Hearing
Screening
夽,夽夽
Inaê
Costa
Rechia
a,∗,
Kátia
Pase
Liberalesso
b,
Otília
Valéria
Melchiors
Angst
b,
Fernanda
Donato
Mahl
a,
Michele
Vargas
Garcia
b,c,
Eliara
Pinto
Vieira
Biaggio
b,caHumanCommunicationDisorders,UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil bSpeechTherapy,UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil
cSciencesDepartment,UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
Received6July2014;accepted7January2015 Availableonline29October2015
KEYWORDS
Hearingloss; Newborn;
Newbornscreening; Intensivecareunits
Abstract
Introduction:Procedures forextendingthelifeofnewbornsarecloselyrelatedtopotential causesofhearing loss,justifyingtheidentificationandunderstandingofriskfactorsforthis deficiency.
Objective:Tocharacterizethepopulation, analyzethefrequencyofriskfactorsfor hearing loss,andassesstheaudiological statusofinfantsattendedinaNewborn HearingScreening program(NHS).
Methods:Thiswasaretrospectivestudythatanalyzedmedicalrecordsof140patientsfrom aneonatalintensive careunit, identifyingthefrequencyofriskfactorsforhearinglossand audiological status,utilizingtransient otoacoustic emissionsandbrainstem auditory evoked potential(BAEP).
Results:Prematuritywaspresentin78.87%ofcases;45%oftheinfantswereunderweightand 73%receivedototoxicmedication.Audiologically,11.42%failedtheNHS,and5%ofcasesfailed retest;ofthese,onehadresultscompatiblewithhearinglossonBAEP.
Conclusion:A higherrateoflowbirthweight,andprematuritywasobservedininfantswho underwentscreeningandhadanaudiological diagnosisby thethirdmonth oflife.Onlyone newbornpresentedachangeinaudiologicalstatus.Theauthorsemphasizetheimportanceof auditorymonitoringforallinfants,consideringthisasahigh-risksampleforhearingloss. © 2015Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:RechiaIC,LiberalessoKP,AngstOVM,MahlFD,GarciaMV,BiaggioEPV.Intensivecareunit:resultsofthe
NewbornHearingScreening.BrazJOtorhinolaryngol.2016;82:76---81.
夽夽Institution:UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil.
∗Correspondingauthor.
E-mail:inaerechia@gmail.com(I.C.Rechia).
http://dx.doi.org/10.1016/j.bjorl.2015.06.004
PALAVRAS-CHAVE
Perdaauditiva; Recém-nascido; Triagemneonatal; UnidadesdeTerapia Intensiva
UnidadedeTerapiaIntensiva:resultadosdaTriagemAuditivaNeonatal
Resumo
Introduc¸ão: Osprocedimentospara prolongamentodavidadosneonatos estãointimamente relacionadoscompossíveiscausasdedeficiênciaauditiva,justificando-seaidentificac¸ãoeo conhecimentodosindicadoresderiscoparataldeficiência.
Objetivo: Caracterizarapopulac¸ão,analisarafrequênciadosindicadoresderiscoparaa defi-ciênciaauditivaeverificarostatusaudiológicodebebêsatendidosnumprogramadeTriagem AuditivaNeonatal(TAN).
Método: Estudodotiporetrospectivo.Foramanalisados140prontuáriosdaUnidadedeTerapia Intensiva Neonatal,caracterizando apopulac¸ãoestudadae afrequênciadosindicadoresde riscopara deficiênciaauditivaestatus audiológico,e considerandoresultados dasemissões otoacústicastransienteseaavaliac¸ãodiagnósticapormeiodoPotencialEvocadoAuditivode TroncoEncefálico(PEATE).
Resultados: Evidenciou-seprematuridadeem78,87%doscasos,45%exibiambaixopesoe73% estavamsendomedicadoscomagentesototóxicos.Quantoaostatusaudiológico,11,42% fal-haram naTAN. Houve falhanoreteste em 5%dos casos e,destes,um neonato apresentou resultadocompatívelcomdeficiênciaauditivanoPEATE.
Conclusão:Houve maiorporcentual deprematuros debaixopeso querealizaramatriagem etiveramumdiagnóstico audiológicoatéo3◦ mêsdevida.Apenasum neonatoapresentou
statusaudiológicoalterado.Ressalta-seaimportânciadeacompanhamentoauditivodetodos osbebês,considerandoestaamostracomodealtoriscoparadeficiênciaauditiva.
©2015Associac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicado por ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
The detection of speech sounds begins in intrauterine life, and is the first step in language acquisition, since it is known that hearing and language are interdepen-dent but interrelated functions. Auditory experiences are of paramount importance, especially before the second year of life, as this is considered the critical period for language acquisition.1---3 Thus, infants who are born with
hearingimpairment(HI),aredeprivedof contactwiththe worldof sound.In thisway, theright timefor the detec-tion/diagnosis of childhood HI is before the third month oflife,andtheinterventionshouldbeginbeforethesixth month.1,4,5
Studies show thatthe incidence ofsignificant bilateral congenital HI in healthy neonates is about 1---3 infants/ 1000births;conversely,innewbornsreferredfromintensive careunitstheincidenceincreasesto2---4%.5
There are prenatal, perinatal, and postnatal
complications that can cause HI in newborns; these arecalledriskfactorsassociatedwithhearingloss(RFHL), namely:theconcernofparentswithrespecttotheirchild general development and the child’s hearing, speech, or language development; familial history of permanent deafness;neonatalintensivecareunit(NICU)stay>5days; or occurrence of any associated condition, such as the useofototoxicmedication;congenitalinfections(rubella, cytomegalovirus, syphilis, herpes, and toxoplasmosis); craniofacialanomalies; geneticsyndromes; neurodegener-ativedisorders;postnatalbacterialorviralinfections;head trauma;andchemotherapy.4
Hospitalization in NICUs is a very frequent risk factor. Preterm infants are generally underweight, in need for lengthymechanical ventilation,andmayhave hyperbiliru-binemiaat levelsthat require exchangetransfusion, thus makingaNICUstayimperative.6
The Newborn Hearing Screening (NHS) test is a safe andappropriateprocedurefortheearlydetectionofHIin neonatesand infants.7 Thecurrent protocol designates as
a NHS procedure the recording and analysis of transient-evokedotoacousticemissions(TEOAE)forneonateswithout RFHL,andanautomaticbrainstemauditoryevoked poten-tial(aBAEP)studyforthosewhohaveanyRFHL.4,5
TEOAErecordingisarelativelysimple,quick,and objec-tive method for detecting hearing changes of cochlear origin,specifically fromthe outer hair cells. This method does not quantify the HI, but detects the presence of a cochlear dysfunction.8---10 BAEP, which is alsoan objective
method, is obtained with surface electrodes that record neuralactivity generated by the cochlea, auditorynerve, andbrainsteminresponsetoauditorystimuli.5,10
atonceforamedicalotolaryngologicaldiagnosisandafull audiologicalevaluationforearlyrehabilitation.4
Thisstudywasundertakenbecauseofaneedtoidentify andunderstandRFHLs;becausetheincrease/advancement oftechnologyassociatedwiththeproceduresthatseekto extendthelivesofnewbornsandinfantsis closelyrelated totheveryfactorsthatcancausehearingimpairment.
Thus,this study aimedtocharacterize the population, analyzethefrequencyofRFHL,andassesstheaudiological statusofinfantstreated inanNHSprogramreferred from theNICUofauniversityhospital.
Methods
This research is linked to a larger project, called ‘‘Child HearingImpairment:fromdiagnosistointervention,’’which wasapprovedbytheResearchEthicsCommitteeunderNo. 610,506.
This wasaretrospective study,11 thataimedto
investi-gateissuesrelatedtohearinghealthininfantsreferredfrom theNICU.
Thesample analyzedmedicalrecordsofnewborns(NB) and infants who underwent NHS and whocame fromthe NICUduringtheperiodfromSeptember of2012toMayof 2013inauniversityhospital.
The samplearrangement wasmadeonthebasis of eli-gibility criteria. The inclusion criteria for the analysis of clinicalrecordswereasfollows:thebabyshouldhavebeen bornandremainedintheNICUforatleastfivedays,withan NHScarriedoutinthisservice.Clinicalrecordswith incom-plete informationand thosewithout an informed consent signedbytheparentor guardianwereexcludedfromdata collection.This NHSservice providesan informedconsent explainingtothoselegallyresponsibleforthechildthatthe datacollectedonthisservicemaybeusedforfuturestudies, andthatallethicalissuesinvolvedwillbeupheld; nonethe-less,the informedconsentmust be signedat the timeof theirchildcare.
Based on a review of medical records,2097 consulta-tions were retrieved in that period. From this total, 140 medicalrecords were selected, using the inclusion crite-ria.The followingvariableswererecorded:characteristics ofstudypopulation(gestationalage[GA],birthweight,age atNHS);frequencyofRFHLs;audiologicalstatus,basedon theresultsdocumentedinthemedicalrecord,onan anal-ysisofTEOAE, andonadiagnosticassessmentcarriedout withthe useof BAEP; false-positive rate;and prevalence ofHI. Suchdata (presenceof RFHL, andTEOAE andBAEP results)wereorganizedintocategoriesofresponses,which werestoredinaspreadsheetinMicrosoftExcel.Inthenext phase,a data analysis washeld withthe use of the pro-gramPASWStatistic v.18.0forWindows.Inthedescriptive analysis, absolute numbers and frequencies of respective variablesweresought.Foracomparativeanalysisofthe dis-tributionoffrequencies,Fisher’sexacttest andCochran’s test (when three or more categories were present) were used.Forallhypothesis tests, asignificance levelof 0.05 wasset. Significant valueswere marked withan asterisk. Allconfidenceintervalsdeterminedduringthisstudywere establishedwith95%ofstatisticalconfidence.
Table1 Frequencyofriskfactorsforhearingloss(RFHL) associatedwithhospitalizationinaneonatalintensivecare unit.
RFHL Frequency Familyhistory 5(3.6%)a
Ototoxicmedication 103(73%)a
Mechanicalventilation 81(57.9%)a
Hyperbilirubinemia 19(13.6%)a
Congenitalinfections 3(2.1%)a a Descriptiveanalysis.
Results
Atotalof140medicalrecordsofinfantswithNICUstayand with mean GA of 34.76 (range:22---42) weeks were eval-uated. Of these,78.57% (n=110) were pretermnewborns with GA <37 weeks; 20.71% (n=29) were term newborns withGAof37---41weeksand6days;and0.72% (n=1)was apost-term newbornwithGA≥42weeks.Whenthethree
categorieswerecompared,apredominanceofpreterm new-borns(p<0.001;Cochran’stest)wasobserved.
The mean birth weight of these infants was 2299g (630---4620). Ofthese,39.28%(n=55)hadnormal weight, that is, ≥2501g; 45% (n=63) had low-birth weight
(1501---2500g); 12.14% (n=17) had very low birth weight (1001---1500g); 1.43% (n=2) had extremely low birth weight (751---1000g); and 2.15% (n=3) were immatureinfantswith<750g.
ThemeanageatNHSwas66.06days(range:5---492days). Ofthese,77.85%(n=109)underwentscreeningbeforethe third month of life;and 22.15%(n=31) weretested after the third month of life. Thus, a statistically significant difference between these two groups (p<0.001; Fisher’s test) was demonstrated. Due to the tenuous health sta-tus of some newborns, NHS was conducted only when their clinical condition became stable. Thus, some chil-drenunderwentauditoryscreeninginapost-neonatalstage period.
RegardingNHS outcome andcharacterization of audio-logical status,11.42% (n=16) infantsfailedthe firststage of the NHS program carried through TEOAE. Of these 16 babies, 56.25% (n=9) passed the retest, also con-ducted by TEOAE, and 43.75% (n=7) failed the NHS retest, and were referred for BAEP. Of these, 85.71% (n=6) showed results consistent with normal hear-ing, and only 14.29% (n=1) showed results compatible with HI. This infant was referred for further medical examination and subsequent speech therapy, including the fitting of hearing aids. Thus, the false-positive rate, that is, the percentage of infants that failed
in NHS, but who had normal hearing, was 10.71%
(n=15).
TheprevalenceofpediatricHIinthepresentstudywas approximately0.71:100. Table1 shows thedistribution of frequenciesofRFHL inthissample.Itisworthnotingthat thatsomeinfantshadmorethanoneRFHL.
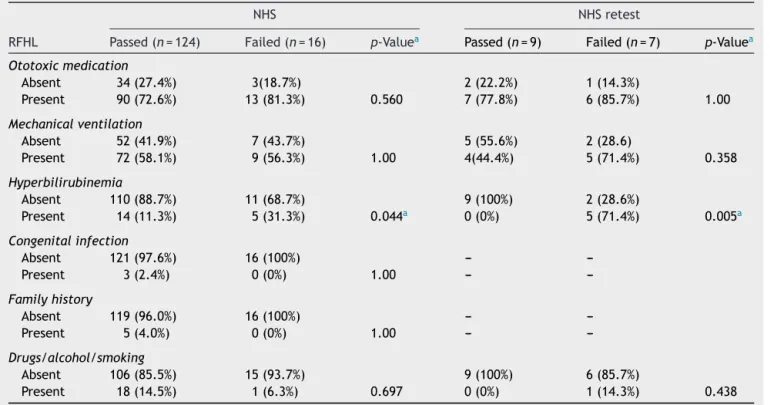
Table2 Riskfactorsforhearingloss(RFHL)andaudiologicalstatus.
NHS NHSretest
RFHL Passed(n=124) Failed(n=16) p-Valuea Passed(n=9) Failed(n=7) p-Valuea
Ototoxicmedication
Absent 34(27.4%) 3(18.7%) 2(22.2%) 1(14.3%)
Present 90(72.6%) 13(81.3%) 0.560 7(77.8%) 6(85.7%) 1.00
Mechanicalventilation
Absent 52(41.9%) 7(43.7%) 5(55.6%) 2(28.6)
Present 72(58.1%) 9(56.3%) 1.00 4(44.4%) 5(71.4%) 0.358
Hyperbilirubinemia
Absent 110(88.7%) 11(68.7%) 9(100%) 2(28.6%)
Present 14(11.3%) 5(31.3%) 0.044a 0(0%) 5(71.4%) 0.005a
Congenitalinfection
Absent 121(97.6%) 16(100%) --- ---Present 3(2.4%) 0(0%) 1.00 ---
---Familyhistory
Absent 119(96.0%) 16(100%) --- ---Present 5(4.0%) 0(0%) 1.00 ---
---Drugs/alcohol/smoking
Absent 106(85.5%) 15(93.7%) 9(100%) 6(85.7%)
Present 18(14.5%) 1(6.3%) 0.697 0(0%) 1(14.3%) 0.438
NHS,NewbornHearingScreening.
a Statisticallysignificantvalues(p<0.05);Fischer’sexacttest.
Discussion
PrematurityisnotclassifiedasaRFHLbyitself,butrather due to the special care in the NICU that these patients generallyrequire,suchastheuseof ototoxicmedication, mechanical ventilation, and specialized consultations.12
Arecentlypublished studyshowed thatGAand NICUstay atbirthareimportantvariablesrelatedtothelikelihoodof hearing screening failure,and that there is a prevalence ofHIinpretermnewborns.Moreover,ininfantswitha con-firmedHI,themeanGAwas31weeks.13AsforGA,another
study alsofoundthat themajority ofthesepatients were preterm.14 These findings make it possible to infer that,
in general, the NICU population consists of underweight pretermnewbornsinneedofspecializedcare.Thisstudy’s dataagreewiththesepreviousstudies,12---14consideringthat
mostofthissampleconsistedofpretermnewborns. Low birth weight is another factor for alterations in child development among primary neonatalhigh-risk fac-tors.Thisstudyassessedthebirthweightofnewbornsand infants treated at the NICU. The mean birth weight was 2299g(630---4620)g;45%(n=63)ofthesamplehadlow-birth weight (1501---2500g). Similarly, another study conducted with a sample of 71 newborns found that, of this total, 52.1%(n=37)hadalow weightbirth,15 whichagreeswith
thepresentfindings.
RegardingthetimefordiagnosisofHIinNBs,itisa gen-eral consensus that such diagnosis should be established early.5 It isknownthat achild withadiagnosis ofHIwho
startsspeechtherapybefore6monthsoflifeismorelikely todevelopaproperhearing,andalsoabetterorallanguage (with statistical significance), when comparedtochildren
diagnosed later.1 In the present study, the mean age at
NHSwas66.06 (5---492)days;77.15% (n=109)of the sam-pleweresubmittedtothisscreeningbeforethethirdmonth oflife.BabieswhofailedthefirststageofNHSprogramwere referredforretesting,withanaudiologicaldiagnosisbefore completionofthethirdmonthoflife,whichisinaccordance withnationalandinternationalrecommendationsregarding thetimeofdiagnosis.1,4,5
Regarding theoutcome of NHS andcharacterization of audiologicalstatus,11.42%(n=16)ofthesamplefailedthe firststageoftheNHSprogramconductedthroughTEOAE.Of these,43.75%(n=7)failedaretest.Infantswhofailedthe retestwere referred for diagnosis andonly 14.29% (n=1) showedresultscompatiblewithHI.Thisfindingemphasizes thefalse-positiverateoftheNHSprogram.
Itisrecommendedthatthefalse-positiveratenotexceed 4%.4,16Inthisuniversityhospital,thefalse-positiveratewas
10.71%(n=15).This highratecanbeexplainedbyfactors suchasexcessivebackgroundnoise,sincetheroomwhere theNHSisperformed doesnothave soundinsulation;and theperformanceof NHSbyan inexperiencedstaff(asthis isateachinghospital,where studentsperformtheir prac-ticalactivitiesandareinaprocessofconstructionoftheir clinicalpractice). Also,theuse ofTEOAE astheNHS pro-cedure could have had an effect since, although BAEP is theprocedurespecifiedforinfantswithRFHL,4that
equip-mentwasnotavailableforcarryingoutthisprocedure.The hospitalhassincepurchasedthisequipmentforusebyNHS service,thusallowingforNHSinaccordancewithnational andinternationalstandards.4,5
abovethe internationallyrecommended level.18 However,
theyareindisagreementwiththefindingsofanother Brazil-ianstudy,thatreportedafalsepositiverateof only1%,19
withinthe targetestablished in the literature.Theirrate waspossiblyachievedbythepresenceofanotolaryngology serviceinthathospital’sNHSprogram,bytheuseofa facili-tatorauricularmaneuver,andbythefactthattheprocedure wasperformedbyhighlyspecializedspeechtherapists.
Inthepresent study,theprevalenceofHIwas0.71:100 livebirths.Another Brazilian studyfound a prevalence of 0.138:100livebirthsforHI.19Conversely,studiesinforeign
languagesfound a prevalence of 2---4% for HIin newborns referredfromNICUs.5
Itis notpossibletomake inferencesregardingthis dif-ference,butitis believedthatfurtherstudieswithlarger sampleswould elucidatemorepreciselytheissuesrelated totheoccurrenceofHIinbabiesreferredfromNICUs.
Table1showsthatthemostprevalentofallriskfactors wasototoxicmedication(73%),whichmayharmanddamage thecochlearfunction,leadingtoHI.20 The presentresults
weresimilartothosefoundinotherstudies,inwhich the most frequent risk factor in the populations studied was theuseofototoxicdrugs.21,22
Duetotheirhealthconditions,manynewbornsneedNICU hospitalizationandmechanicalventilation.Severalaspects have been linked to higher rates of deafness in children submittedtoassistedventilation,includingthenoiselevel of the machine, duration of mechanical ventilation, and the lung diseases involved.23 In the present study, 57.9%
(n=81) of theinfants required mechanical ventilation.Of these, 88.9% (n=72) achieved a passing result, and only 11.1%(n=9)failed theinitial NHS.These resultsare con-sistentwithanotherstudyof200newborns,inwhichthere wasahighprevalenceofmechanicalventilation.Ofthese, 84.5%(n=169)achievedapassingresult,and15.5%(n=31) failedtheNHS.23 Likewise,hyperbilirubinemia hasatoxic
effectoncochlearhaircells,basalnuclei,andcentral audi-tory pathways.24 In the present study, 13.6% (n=19) of
the sample had hyperbilirubinemia. A study with a sam-ple of 2002 newborns found that 3.9% of this population hadsome RFHL. Among these,24.1% had hyperbilirubine-miaand3.9%requiredmechanicalventilationfor overfive days.25
InTable2,theauthorssoughttoexaminetheassociation betweentheNHSresultinthefirststageoftheprogram,and inNHSretest,consideringtheRFHLsfoundinthissample.In thefirststageoftheevaluation,carriedoutthroughTEOAE, 81.3%(n=13)ofthe samplein useofototoxicmedication failedthe NHS.This finding is in agreementwithanother study,inwhich8.6%oftheinfantswhofailedNHShadsome RFHL,andofthese,themostprevalentfactor wastheuse ofototoxicmedication(42.9%).25
Studiesshowthatbabieswhoreceivedexchange transfu-sionduetohighratesofbilirubinmayfailtheNHS.25,26The
structuresof the auditorysystem show high sensitivity to thetoxiceffectsofbilirubin.Amongthehearingproblems causedbytheeffectsofhyperbilirubinemia,auditory neu-ropathy,whichmay(ornot)beassociatedwithotherhearing disorders,isnoteworthy.27Incontrast,inthepresentstudy,
childrenwhopresented suchRFHLhad normalhearing,in accordancewithotherstudiesthatobservednochangesin auditorypathwaysinnewbornswithhyperbilirubinemia.28,29
Considering this study sample, it was found that among theRFHLs associatedwithNICU, congenital infec-tion hadthe lowest occurrence(2.14%). All subjectswith thisRFHLachievedapassingresultinNHS.However,studies showthat,evenwhenasymptomatic,congenitalinfections (rubella, syphilis,cytomegalovirus,herpes,toxoplasmosis, andacquiredimmunodeficiencysyndrome)cancauseHIin theneonateandmaybeassociatedwithlate-onsetHIand/or withprogressionofsomeHIalreadypresentatbirth.30,31
Conclusion
Ofthe140patientsscreenedduringthestudyperiod,there washigher incidenceof preterm newborns withlow birth weight and of NHS and audiological diagnosis performed beforethethirdmonthoflife.Themostfrequentrisk fac-torwasuseofototoxicmedication,whichisoftenassociated withmechanicalventilation;bothwerepresentinthesingle newbornwhopresentedanaudiologicalassessment consis-tent withHI.However,in spite ofan association between hyperbilirubinemiaand‘‘failed’’resultsintestsandretests, BAEPresultsconsistentwithnormalhearingwerenotedfor allsubjectswithsuchRFHL.
Takingintoaccountthatthisstudysamplewasconsidered tobeat high risk for HI,the authorsmust emphasize the importanceofauditorymonitoringuntilthethirdyearoflife ofthechild,duringwhichhearingchangesofprogressive-or late-onsetcharactermaybeidentified.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Yoshinaga-ItanoC,SedeyAL,CoulterDK,MehlAL.Languageof earlyandlateridentifiedchildrenwithhearingloss.Pediatrics. 1998;102:1161---71.
2.HiluMRPB,ZeigelboimBS.Oconhecimento,avalorizac¸ãoda triagemauditivaneonatalea intervenc¸ãoprecocedaperda auditiva.RevCEFAC.2007;9:563---70.
3.Azevedo MF. Desenvolvimento das Habilidades Auditivas. In: BevilacquaMC,etal.,editors.TratadodeAudiologia.SãoPaulo: SantosEditora;2013.p.475---93.
4.LewisDR,Marone SAM,Mendes BCA, CruzOLM, Nóbrega M. Comitêmultiprofissionalemsaúdeauditiva---COMUSA.BrazJ Otorhinolaryngol.2010;76:121---8.
5.JointCommitteeonInfantHearing.Year2007Position State-ment:principlesandguidelinesforearlyhearingdetectionand interventionprograms.Pediatrics.2007;120:898---921. 6.VieiraEP,MirandaEC,AzevedoMF,GarciaMV.Ocorrênciados
indicadores de risco para a deficiência auditiva infantil no decorrer de quatro anos em um programa de triagem audi-tivaneonataldeumhospitalpúblico.RevSocBrasFonoaudiol. 2007;12:214---20.
7.Northern JL, Downs MP. Triagem auditiva em crianc¸as. In: Audic¸ãonainfância.5thed.RiodeJaneiro:GuanabaraKoogan; 2005.p.209---43.
8.KempDT,RyanS,BrayP.Aguidetotheeffectiveuseof otoa-cousticemissions.EarHear.1990;11:93---105.
10.Esteves MCBN, Dell’Aringa AHB, Arruda GV, Dell’Aringa AR, NardiJC. Brainstem evoked response audiometry in normal hearing subjects. Braz J Otorhinolaryngol (Impr). 2009;75: 420---5.
11.GilAC.ComoElaborarProjetosdePesquisa.SãoPaulo.4thed; 2002,176pp.
12.GarciaCFD,IsaacML,OliveiraJAA.Emissãootoacústicaevocada transitória:instrumentoparadetecc¸ãoprecocedealterac¸ões auditivas em recém-nascidos a termo e pré-termo. Braz J Otorhinolaryngol.2002;68:44---52.
13.PereiraPKS,MartinsAS,VieiraMR,AzevedoMF.Programade triagemauditivaneonatal:associac¸ãoentredeficiênciaauditiva efatoresderisco.Pró-Fono.2007;19:267---78.
14.DidoneDD,GarciaMV,KunstLR,VieiraEP,SilveiraAF.Correlac¸ão dos indicadores de risco para deficiência auditiva com a ‘‘falha’’natriagem auditiva neonatal. Saúde(Santa Maria). 2013;1:113---20.
15.Sassada MMY, Ceccon MEJ, Navarro JM, Vaz FAC. Avaliac¸ão auditivade recém-nascidosgravementeenfermosatravés do métododeemissõesotoacústicasevocadastransientes(EOAT) eaudiometriadetroncocerebral(BERA).Pediatria(SãoPaulo). 2005;27:154---62.
16.AmericanAcademyofPediatrics---AAP.Taskforceonnewborn andinfanthearing.Pediatrics.1999;103:527---30.
17.SimonekMCS,AzevedoMF.Respostasfalsopositivasnatriagem auditiva neonatal universal: possíveis causas. Rev CEFAC. 2011;13:292---8.
18.JointCommittee onInfant Hearing.Supplement tothe JCIH 2007 position statement: principles and guidelines for early interventionafterconfirmationthatachildisdeaforhardof hearing.Pediatrics.2013;131:1324---49.
19.FaistauerM,AugustoTAM,FlorianoM,TabajaraCC,MartiniCM, SchmidtVB,etal.Implementac¸ãodoprogramadetriagem audi-tivaneonataluniversalemhospitaluniversitáriodemunicípio daregiãoSuldoBrasil:resultadospreliminares.RevAMRIGS, PortoAlegre.2012;56:22---5.
20.OliveiraTMT,AzevedoMF,VieiraMM,ÁvilaCRB.Triagem audi-tivacomsonsnãocalibrados:detecc¸ãoprecocedadeficiência auditiva.ActaAWHO.1995;14:88---92.
21.GarzaMS,PoblanoA,RobledoGA,FernándezCLA.Potenciales provocadosauditivosemni˜nosconriesgoneonatalde hipoacu-sia.RevPanamSaludPública.1997;1:119---24.
22.Barreira-Nielsen C, Futuro HAN, Gattaz G. Processo de implantac¸ãode ProgramadeSaúdeAuditiva emduas mater-nidadespúblicas.RevSocBrasFonoaudiol.2007;12:99---105. 23.Lima GML, Marba STM, Santos MFC. Triagem auditiva em
recém-nascidosinternadosemUTIneonatal.JPediatr.2006;82: 110---4.
24.deAlmeidaFS,PialarssiPR,MonteACM,SilvaJVda.Emissões otoacústicasepotenciaisevocadosdotroncocerebral:estudo emrecém-nascidoshiperbilirrubinêmicos.BrazJ Otorhinolaryn-gol.2002;68:851---8.
25.DantasMBS,AnjosCAL,CamboimED,PimentelMCR.Resultados deumprogramadetriagemauditivaneonatalemMaceió.Braz JOtorhinolaryngol.2009;75:58---63.
26.HosonoS,OhnoT,KimotoH,NagoshiR,ShimizuM,NozawaM, etal.Follow-upstudyofauditorybrainstemresponsesininfants withhighunboundbilirubinlevelstreatedwithalbumininfusion therapy.PediatrInt.2002;44:488---92.
27.Martinho AC, Lewis DR. Achados audiológicos em crianc¸as com hiperbilirrubinemia neonatal: um enfoque na neuropa-tiaauditiva/dessincroniaauditiva.DistúrbComun(SãoPaulo). 2005;17:183---90.
28.CianciarulloMA,DuranteAS,CarvalloR,VoegelsGT,VazFAC. Perda auditiva neonatal associada a hiperbilirrubinemia por deficiênciadeglicose-6-fosfatodesidrogenase:relatodecaso. Pediatria(SãoPaulo).2005;27:126---32.
29.ÖgünB, Serbetc¸ioglu B,DumanN,ÖzkanH,KirkimG. Long-termoutcomeofneonatalhyperbilirubinemia:subjectiveand objective audiological measures. ClinOtolaryngol Allied Sci. 2003;28:507---13.
30.Dahle AJ,Fowler KB,Wright JD,BoppanaSB, BrittWJ, Pass RF.Longitudinalinvestigationofhearingdisordersinchildren withcongenitalcytomegalovirus.JAmAcadAudiol.2000;11: 283---90.