r e v b r a s r e u m a t o l . 2016;56(5):384–390
ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
A
prospective
study
predicting
the
outcome
of
chronic
low
back
pain
and
physical
therapy:
the
role
of
fear-avoidance
beliefs
and
extraspinal
pain
Aloma
S.A.
Feitosa,
Jaqueline
Barros
Lopes,
Eloisa
Bonfa,
Ari
S.R.
Halpern
∗Servic¸odeReumatologia,HospitaldasClínicas,UniversidadedeSãoPaulo(USP),SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received15May2015 Accepted11November2015 Availableonline22March2016
Keywords:
Fear-avoidancebeliefs Extraspinalpain Therapeuticresponse Chroniclowbackpain
a
b
s
t
r
a
c
t
Objective:Toidentifytheprognosticfactorsforconventionalphysicaltherapyinpatients withchroniclowbackpain(CLBP).
Methods:Prospectiveobservationalstudy.
Participants:OnehundredthirteenpatientswithCLBPselectedattheSpinalDisease Outpa-tientClinic.
Mainoutcomemeasures:PainintensitywasscoredusingtheNumericRatingScale(NRS),and functionwasmeasuredusingtheRoland-MorrisDisabilityQuestionnaire(RMDQ). Results:TheFear-AvoidanceBeliefsQuestionnaireworksubscaleresults(FABQ-work;odds ratio[OR]=0.27, 95% confidence interval [CI] 0.13–0.56, p<0.001) and extraspinal pain (OR=0.35, 95% CI 0.17–0.74, p=0.006)wereindependently associated witha decreased responsetoconventionalphysicaltherapyforCLBP.
Conclusion:WeidentifiedhighFABQ-workandextraspinalpainscoresaskeydeterminants ofaworseresponsetophysicaltherapyamongCLBPpatients,supportingtheneedfora specialrehabilitationprogramforthissubgroup.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Estudo
prospectivo
de
fatores
prognósticos
em
lombalgia
crônica
tratados
com
fisioterapia:
papel
do
medo-evitac¸ão
e
dor
extraespinal
Palavras-chave:
Crenc¸asdeevitac¸ãoemedo Dorextraespinal
Respostaterapêutica Lombalgiacrônica
r
e
s
u
m
o
Objetivo:Identificarosfatoresprognósticosparaafisioterapiaconvencionalempacientes comlombalgiamecânicacomumcrônica(LMC).
Métodos:Estudoprospectivoobservacional.
Participantes:Foram selecionados pelo Ambulatório de Doenc¸as da Coluna Vertebral 113pacientescomlombalgiamecânicacomumcrônica.
Medidas de desfecho principais:A intensidade da dor foi pontuada utilizando a Escala NuméricadeDor(END)eafunc¸ãofoimedidausandooQuestionárioRoland-Morrisde Incapacidade(RMDQ).
∗ Correspondingauthor.
E-mail:ariradu@einstein.br(A.S.Halpern). http://dx.doi.org/10.1016/j.rbre.2016.03.002
Resultados: OsresultadosdasubescalatrabalhodoFear-AvoidanceBeliefsQuestionnaire (FABQ-trabalho; odds ratio [OR]=0,27, intervalo de confianc¸a de 95%[IC 95%] 0,13–0,56, p<0,001)edador extraespinal(OR=0,35,IC0,17–0,74, p=0,006)estiveram independen-temente associados a uma diminuic¸ão na respostaà fisioterapia convencional paraa lombalgiacrônica.
Conclusão: ForamidentificadosescoreselevadosnaFABQ-trabalhoedorextraespinalcomo determinantes-chaveparaumapiorrespostaàfisioterapiaempacientescomLMCoque apoiaanecessidadedeumprogramadereabilitac¸ãoespecialparaestesubgrupo.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Chronic lowback pain (CLBP)is oneof the mostcommon causesofmusculoskeletalsystem-relateddisability,anditis associatedwithhighlevelsofhealthcareresourceutilization.1 TheimpactofCLBPinBrazilisthoughttoparallelthe situ-ationintheNorthernhemisphere,althoughaccuratedataare lacking.ThenumberofBrazilianswhoaredisabledbyCLBPis veryhigh;reportsestimatethatapproximately10million peo-pleinBrazilareaffected.2CLBPrepresentsthemainreasonfor disabilitybenefitrequestsandisthethirdmostcommoncause ofdisability-relatedretirementinBrazil.3
Treatment for CLBP is usually conservative. Scientific evidence consistently favors pharmacological agents and rehabilitationastheprimarytreatmentoptions4,5;however, theresponsetophysicaltherapyisrathervariableand unpre-dictable.
Althoughstudieshaveindicatedthe efficacyof rehabili-tationcomparedwithnotreatment,fewhavedemonstrated the superiorityofany particularrehabilitationprogram for CLBP.6–9 Inaddition,relapse ratesafterinitialimprovement from rehabilitationare high,7 whereas the long-term cost-effectivenessofphysicalrehabilitationanditsactualimpact onrecoveryintermsofenablingpatientstoreturntotheir normalactivitiesremainsunknown.8
SincetheQuebecTaskForce’sreportin1987,many inter-nationalguidelineshavebeenpublished.10–14Althoughthese guidelines were produced in different countries, most of theissuesrelatedtotherapeuticinterventionweresimilar.13 Supervisedexercisewas generally recommended, although most guidelines did not propose a specific set of exer-cises.Physicaltherapistsuse abroadarray ofconservative, nonpharmacologic therapeuticinterventions, few ofwhich are consistently or widely recommended across various guidelinesdespitethestrongevidencefavoringtheuseof ther-apeuticexercisesforchroniclowbackpain.
In 2006, the European guidelines for the management ofchronic nonspecific low back pain were published. The goal of the COST B13 working group was toprovide a set ofrecommendationsthatcouldsupportexistingandfuture guidelines.14 Oneofthemajorstrengths ofthisguidelineis itsmultinationalandmultidisciplinarynature.Theauthors proposedthatchroniclowbackpainshouldnotbe consid-eredasingleclinicalentityandemphasizedtheneedtoassess prognosticfactorsbeforetreatment.
In 2007, the Multinational Musculoskeletal Inception CohortStudy(MMICS)publishedalistoffactorsthatitdeemed
necessarytoexamineinfuturestudiesofprognostic indica-torsforchronicityinpatientswithCLBP.9Theneedtoidentify suchfactorsisunderstandablebecausealthoughonly5%of CLBPpatientsdevelopdisabilities,75%ofallexpensesrelated to low back pain are devoted to that population.1 Conse-quently, most studies on identifying prognostic factors for chronicityanddisabilityhavefocusedonacutelowbackpain patients,andveryfewstudieshavefocusedonthe prognos-ticfactorsfortreatmentresponseinpatientswithestablished CLBP.
Thestudy hypothesisis thatsomebaseline characteris-tics may identify subgroup of CLBP patients with distinct response ratesto treatment. Therefore, weevaluated CLBP patients’ clinicalresponsestoaseriesofsessionsof super-visedphysicalactivityandassessedvariousfactorsincluded intheMMICSrecommendationstodeterminetheirabilityto identifytheprognosticfactorsfortreatmentresponseto con-ventionalphysicaltherapy.
Methods
Patients
Participantswererecruitedthroughadvertisementsdesigned byourpressoffice.Allpotentialparticipantswerescreenedby thesamerheumatologist(ASRH)betweenJanuaryandMarch 2009.ParticipantswhowerediagnosedwithnonspecificCLBP andmettheinclusionandexclusioncriteriawererecruited. Theinclusioncriteriawereagebetween18and80years,pain betweenthe last riband thegluteal foldthatpersistedfor morethanthreemonths,painthatwascontinuousorpresent mostofthetimeandwaspatient’smainpain-related com-plaint,andtheprovisionofinformedconsent.Theexclusion criteriawere adiagnosisofsystemicinflammatorydisease, the presenceofcharacteristicradicularpain, pain originat-ingintheperipheraljoints,osteoarticulardeformitiesinthe lower limbs,decompensated heartfailure, neoplasia inthe previousfiveyears,previouslumbarspinesurgery,systemic diseasethatmightinterferewiththeinterpretationofresults basedonmedicalopinion,aninabilitytounderstand ques-tionnairesandexplanationsortocomplywiththetreatment, physicaltherapyforLBPthatinvolvedphysicalexercisesinthe previousfiveyears,psychiatricdisorders,andfibromyalgiaor painnotlocatedinthelumbarspineasthemainpain-related complaint.
386
rev bras reumatol.2016;56(5):384–390referredtousfromotherdepartmentswithinthehospitaland fromanetworkofprimaryorsecondarycareunitslinkedto thehospital.
Alloftheparticipantssignedaninformedconsentform, andthestudywasapprovedbytheResearchEthics Commit-tee.
Thisstudycompliedwiththeethicalprinciplesofthe Dec-larationofHelsinki(2008)andtheapplicablelocallawsand regulations.Thisresearchwasapprovedbythe localethics andresearchcommittee(ResearchProtocol1110/07).
Physicaltherapyintervention
The treatment consisted of 10 individual sessions: two sessions per week for five weeks. Each session included core-strengtheningexercises(i.e.,exercisesthatinvolvedthe abdominal,pelvicfloor,gluteal,diaphragmaticandpelvic gir-dle muscles), stretching exercises and postural orientation exercises.Allassessmentsandphysicaltherapysessionswere performedbythesamephysicaltherapist.
Assessments
Thepatients’responsestophysicaltherapywereassessedin termsofchanges inpainintensity usingthe Numeric Rat-ing Scale (NRS), which has a range of 0–10, and in terms ofCLBP-relateddisabilityusingtheRoland-MorrisDisability Questionnaire(RMDQ),whichhasarangeof0–24.The partici-pantswereassesseduponinclusioninthestudy,immediately afterthetenphysicaltherapysessions(firstevaluation)and threemonthsafterthefirstevaluation(secondevaluation).
Fortheresponderanalysis,thepatientsweredividedinto responder and nonrespondergroupsaccording tothe indi-vidualchangesinthepainintensityanddisabilitymeasures ateachevaluation.Apatientwasconsideredaresponderif he/sheshowedadecreaseofatleasttwopointsintheNRS score15oratleastfourpointsintheRMDQscore.16Wealso expressedtheresultsasthepercentageofchangefromthe scoreobtainedatbaseline.
Socio-demographicdatawerecollected,acomplete phys-icalexaminationwas performed, and the duration ofpain was assessed at baseline. In addition, all of the partici-pants answered standardizedquestionnaires to assess the factors included inthe MMICS guidelines (smoking, physi-calactivity,occupationalfactors,depression,andcatastrophic thinking) and completed the Fear-Avoidance Beliefs Ques-tionnaire (FABQ). The FABQ contains two subscales that were separatelyevaluated: fear-avoidancebeliefsrelated to work(FABQ-work)andphysicalactivity(FABQ-physical).Fear
Table1–Demographic,anthropometricandclinicaldata.
Variables All(n=113)
Age,years 53.0(12.2)a
Female,n(%) 81(71.7)
BMI,kg/m2 27.9(5.1)a
Smoking,n(%) 16(14.2)
Painbelowtheknee,n(%) 73(64.6)
Physicalactivity,n(%) 90(79.6)
Irritability,n(%) 13(11.5)
Depression,n(%) 83(73.5)
Catastrophicthinking,n(%) 35(31.0)
FABQ-physical,n(%) 13(11.5)
FABQ-work,n(%) 46(36.3)
Extraspinalpain,n(%) 35(31.0)
BMI,bodymassindex;FABQ-physical,fear-avoidancebeliefs sub-scaleforphysicalactivity≥15;FABQ-work,fear-avoidancebeliefs subscaleforwork≥34.
a Dataareexpressedasthemean(standarddeviation).
avoidancerelatedtophysicalactivitywasconsideredeither present (score ≥15) or absent (<15), while fear avoidance relatedtoworkwasconsideredpresentiftheFABQ-workscore was≥34.TheBrazilianversionsofallofthesequestionnaires werepreviouslyvalidated.17–20
Thepatientswereconsideredtohaveextraspinalpainif theyhadchronicpaincomplaintsinadditiontoLBPbutdid notfulfillthecriteriaforfibromyalgia.
Statisticalanalysis
The sample size followed the criteria for multiple logistic regressionanalysiswithatleast5–12patientsineachofthe 12explanatoryvariables.
Thenormalityofthedatadistributionwasanalyzedwith the Kolmogorov–Smirnov test, and parametric tests were applied.Quantitativedatawereexpressedasthemean(SD), whereasqualitativedatawereexpressedinabsolutenumbers andrelativefrequency.
Thecombinedinfluenceofthevariablesandtimeof eval-uation on the patient response wasassessed witha fitted modelthatusedgeneralizedestimationequations(GEE)with anormalmarginaldistributionandanidentitylinkfunction, assumingsymmetricmatrixcomponentcorrelationsbetween timepoints.
Onlystatisticallysignificantvariableswereretainedinthe finalmodels.Thefitofeachmodelwasverifiedwithresidual analysesthatusedCook’sdistanceordevianceresiduals.The significancelevelwassetat5%.
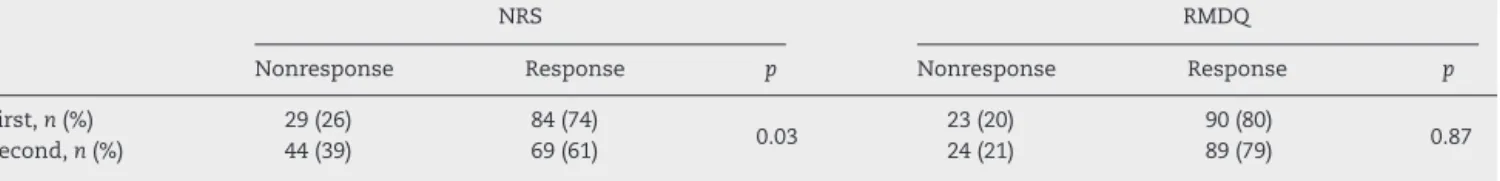
Table2–ResponsetophysicaltherapyforchroniclowbackpainmeasuredwiththeNumericRatingScale(NRS)andthe Roland-MorrisDisabilityQuestionnaire(RMDQ)ateachevaluationtime.
NRS RMDQ
Nonresponse Response p Nonresponse Response p
First,n(%) 29(26) 84(74)
0.03 23(20) 90(80) 0.87
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(5)
:384–390
387
NRS RMDQ
First Second p First Second p
Non-responder Responder Non-responder Responder Non-responder Responder Non-responder Responder
n=29 n=84 n=44 n=69 n=23 n=90 n=24 n=89
Age,yearsa 53.9(13.9) 52.7(11.6) 53.3(12.3) 52.8(12.2) 0.71 53.5(11.6) 52.8(12.4) 54.1(10.0) 52.7(12.7) 0.65
Female 20(68.9) 61(72.6) 33(75) 48(69.5) 0.81 15(65.2) 66(66.7) 17(70.8) 64(71.9) 0.61
BMI,kg/m2a 27.0(5.0) 28.3(5.1) 28.0(5.5) 27.9(4.8) 0.62 26.9(5.3) 28.2(5.0) 28.1(5.9) 27.9(4.8) 0.60
Smoking 5(17.2) 11(13.1) 7(15.9) 9(13) 0.58 5(21.7) 11(12.2) 4(16.7) 12(13.5) 0.36
Painbelowtheknee 20(69.0) 53(63.1) 33(75.0) 40(58.0) 0.13 17(73.9) 56(62.2) 17(70.8) 56(62.9) 0.30
Physicalactivity 21(72.4) 69(82.1) 34(77.3) 56(81.2) 0.37 18(78.3) 72(80.0) 19(79.2) 71(79.8) 0.88
Irritability 6(20.6) 7(8.3) 7(15.9) 6(8.7) 0.09 3(13.0) 10(11.1) 4(16.7) 9(10.1) 0.50
Depression 22(75.9) 61(72.6) 34(77.3) 49(71.0) 0.51 19(82.6) 64(71.1) 19(79.2) 64(71.9) 0.29
Catastrophicthinking 10(34.5) 25(29.8) 17(38.6) 18(26.1) 0.25 11(47.8) 24(26.7) 9(37.5) 26(29.2) 0.12
FABQ-physical 3(10.3) 10(11.9) 7(15.9) 6(8.7) 0.52 3(13.0) 10(11.1) 4(16.7) 9(10.1) 0.47
FABQ-work 16(55.2) 25(29.8) 26(59.1) 15(21.7) <0.001 10(43.5) 31(34.4) 13(54.2) 28(31.5) 0.09
Extraspinalpain 14(48.3) 21(25.0) 21(47.7) 14(20.3) 0.002 12(52.2) 23(25.6) 9(37.5) 26(29.2) 0.06
BMI,bodymassindex;FABQ-physical,fear-avoidancebeliefsquestionnairesubscaleforphysicalactivity≥15;FABQ-work,fear-avoidancebeliefsquestionnairesubscaleforwork≥34. p<0.05inbold.
388
rev bras reumatol.2016;56(5):384–390Results
From217inquiries,130peoplewithCLBPwereselected. Sev-enteenpatients withdrewbefore the end ofthe scheduled consultationsandwereexcluded.Onehundredthirteen sub-jects completed the study. The main reason reported for withdrawal was difficulty commuting to the rehabilitation centerasoftenasrequired.
Thesampleconsistedof81womenand32menbetween 21 and 80 years old. The cohort consisted of 40% house-wives and pensioners, 16% cleaning personnel, 10% office employeesand31%otheroccupations.Only3%were unem-ployed.ThemeanBMIvaluewas27.9kg/m2,rangingfrom18 to47.ThedurationofCLBPrangedfromthreemonthsto40 years(±0.76years).Additionaldemographic,anthropometric andclinicalcharacteristicsofthesepatientsarepresentedin Table1.
TheresponsetophysicaltherapyasassessedwiththeNRS decreased from the first tothe second evaluation (74%vs. 61%,p=0.03).WhenassessedwiththeRMDQ,thefrequency ofresponsewas similarforboth evaluations(80%vs. 79%, p=0.87;Table2).
TheparticipantswithahighFABQ-workscorehadapoorer outcomeatbothevaluationsbasedontheNRSresults(55% nonrespondersvs. 30%responders and 59%nonresponders vs.22%responders,p<0.001).Thesameresultswereobserved forthepatientswithextraspinalpain(48%vs.25%and48%vs. 20%,p=0.002;Table3).ThehigherFABQ-workscoresandthe greaterfrequencyofextraspinalpainaccordingtotheRMDQ didnotreachstatisticalsignificance(Table3).
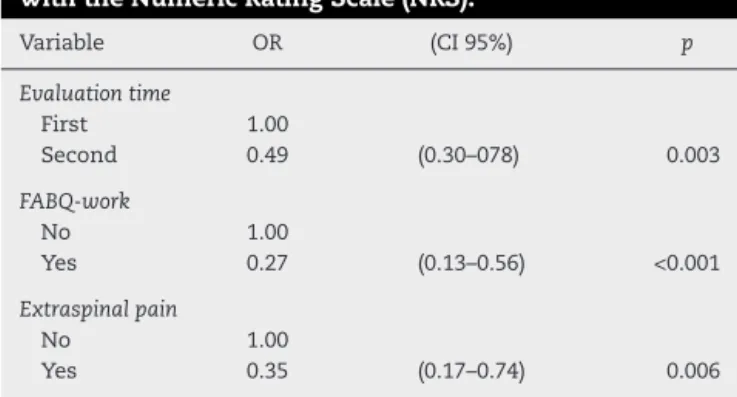
In the final model analysis, the presence of work-related fear avoidance and extraspinal pain remained as independentfactorsassociatedwithnonresponse(OR=0.27, 95% CI=0.13–0.56; p<0.001and OR=0.35, 95% CI 0.17–0.74; p=0.006,respectively;Table4).
Table4–Finalmodeloftheprognosticfactorsforthe responsetoconventionalphysicaltherapyassessed withtheNumericRatingScale(NRS).
Variable OR (CI95%) p
Evaluationtime
First 1.00
Second 0.49 (0.30–078) 0.003
FABQ-work
No 1.00
Yes 0.27 (0.13–0.56) <0.001
Extraspinalpain
No 1.00
Yes 0.35 (0.17–0.74) 0.006
OR,oddsratio;CI,confidenceinterval;FABQ-work,fear-avoidance beliefssubscaleforwork≥34.
Inaddition, weanalyzedthe resultasthe percentageof change intheresponsefrom baseline.BoththeRMDQ and NRSresponserateswerenegativelyinfluencedbyextraspinal painandfearavoidancerelatedtowork(Table5).
Discussion
This study is oneof the few prospectivestudies to assess theprognosticfactorsrelatedtophysicaltherapyforpatients with CLBP.Wefoundthat work-relatedfear avoidance and extraspinalpainnegativelyinfluencedtheoutcome.
Functional disability resulting from CLBP has increased despitenewinterventions.Comparisonsamongstudieshave been obstructed by the use of varied definitions and out-comemeasures.21Inthesamemanner,therearenogolden rulesthatpredicttheresponsetotreatmentforCLBP.22Inthis study,patientswereconsideredrespondersiftheyshoweda
Table5–Bivariateandmultivariateanalysisofthefactorsthatinfluencetheresponsetophysicaltherapy,assessedwith theNumericRatingScale(NRS)andtheRoland-MorrisDisabilityQuestionnaire(RMDQ)andmeasuredasthepercentage ofchangefromthebaseline.
NRS RMDQ
Bivariate Multivariate Bivariate Multivariate
Estimate(SE) p Estimate(SE) p Estimate(SE) p Estimate(SE) p
Age,years 0.19(0.27) 0.499 0.2(0.22) 0.365
Female −7.9(7.35) 0.282 −1.95(5.94) 0.743
BMI,kg/m2 0.03(0.66) 0.964 0.21(0.53) 0.700
Smoking 3.15(9.53) 0.741 −2.63(7.68) 0.732
Painbelowtheknee −10.44(6.89) 0.130 −8.33(5.55) 0.133
Physicalactivity 4.15(8.25) 0.615 7.18(6.62) 0.278
Irritability −11.54(10.37) 0.266 −12.68(8.31) 0.127
Depression −8.48(7.49) 0.257 −13.56(5.93) 0.022
Catastrophicthinking −6.04(7.17) 0.400 −7.84(5.75) 0.173
FABQ-physical 0.56(10.43) 0.958 −2.97(8.39) 0.723
FABQ-work −17.33(6.72) 0.010 −13.8(6.53) 0.035 −13.5(5.42) 0.013 −10.66(5.27) 0.043
Extraspinalpain −23.92(6.83) <0.001 −21.47(6.79) 0.002 −19.16(5.5) <0.001 −17.26(5.48) 0.002
BMI,bodymassindex;FABQ-physical,fear-avoidancebeliefsquestionnairesubscaleforphysicalactivity≥15;FABQ-work,fear-avoidancebeliefs questionnairesubscaleforwork≥34.
decreaseofatleasttwopointsintheNRSscoreorfourpoints intheRMDQscore.Alternatively,weevaluatedtheresponse asthe%ofchangefrombaselineandfoundsimilarresults. Nevertheless,wedidnotperformsensitivityanalyses.Future studiesshouldaddressthisissueinmoredetailtosupportour conclusions.
FABQ-work scores emerged as an important variable despitetheinclusionofalargeproportionofhousewivesinthe studypopulation.Ourfindingssupportthoseofotherstudies withthesuggestionthatindividualizedphysicaltherapy pro-gramsthatfocusondifferentoccupationalactivitiesshould betested.23,24
Inthelast decade,it hasbeenunclear whether psycho-logicalfactorsmeritedinterventionstoreducetheburdenof chronicbackpain.25Whenitwaspublishedin2007,theMMICS suggestedincludingfearavoidanceandother psychological factors(catastrophizinganddepression)inprospective inves-tigationsintothetransitionfromacutetochronicbackpain.9 Thefactorsthatwereincorporatedlargelyreflectedthe opin-ionofexpertsandthereforeweresomewhatsubjectivedespite representingaconsensus.Theimpactofthesecomponents onthetreatmentstrategyforchronicbackpain(andnotonly intheearlystages)islesswellestablished.Inourstudy,fear avoidance,butnototherpsychologicalfactors,influencedthe outcomes.
Extraspinal pain was another important factor that affectedthetreatmentresponse.PatientswithLBPasthemain complaintdidbetterwhentheyhadnoothersitesofpain. Ithasbeenalreadysuggestedthatindividualswithchronic painoftenpresentwithmorethanonepainfulcondition,26but theimportanceofthisobservationtotreatmentandprognosis remainsunclear.
Inourstudy,mostofthepatientsimprovedsignificantly with physical therapy. The protocol used consisted of a seriesofexercisesthatarecommonlyappliedandthathave a well-established level of efficacy in the literature.27 It is worth mentioning that the responserate, asmeasured by the NRS, decreasedafter threemonthsoftreatment; how-ever,thisphenomenonwasnotobservedfortheRMDQ,which suggests thatphysicaltherapy had morelastingeffectson functionthan onpainperception.Perhapsphysicaltherapy programsaffectpatients’abilitytocopewithpain.Thisissue shouldbeevaluatedinfuturestudieswithlongerfollow-up periods.
Unfortunately,thesampleusedinthis studyincluded a largeproportionofhousewives,whichpreventsthe extrapo-lationoftheseresultstootherpopulations.Althoughalarge numberofpatientswere assessed,CLBPisaverycommon condition;thus,evenlargerstudiesmustbeconductedin var-iousemploymentandbiopsychosocialcontexts.Itshouldbe mentionedthatthestudylasted onlythreemonths; conse-quently,itdidnotaddresstheneedforre-treatmentorthe long-termdurationoftheresponse, norwasit designedto addresstheimportantquestionofpatients’abilitytoreturn towork.
Epidemiologicalstudieshaveshownthatthespectrumof musculoskeletaldisordersindevelopingcountriesissimilar tothatobservedinindustrializedcountries,buttheburdenof diseasetendstobehigherbecauseofdelaysindiagnosisor alackofaccesstoadequatehealthcarefacilitiesforeffective
treatment.28InBrazil,mostpatientswithCLBPwillreceive aprescriptionforlimitedsessionsofphysicaltherapyinan almostuniversal manner;however, theresultsofourstudy suggest thatphysicaltherapy,suchasothertreatmentsfor CLBP,shouldbeindividualizedaccordingtospecificpatient characteristics.
Fear avoidance could be a barrier to recovery from chronicbackpainregardlessofthetreatmentmodality.We believe that fear avoidance should be routinely tested to help practitioners and researchers define better treatment strategies.
Inconclusion, weidentified fear-avoidancebeliefs about workandthepresenceofextraspinalpainascharacteristicsof subgroupsofpatientswhomayrequirecustomizedtreatment protocolsandspecialrehabilitationprogramsforCLBP.
Funding
Coordenac¸ãodeAperfeic¸oamentodePessoaldeNívelSuperior (CAPES)(ASAF).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.GoreM,SadoskyA,StaceyBR,TaiKS,LeslieD.Theburdenof chroniclowbackpain:clinicalcomorbidities,treatment patterns,andhealthcarecostsinusualcaresettings.Spine. 2012;37:E668–77.
2.SalvettiMdeG,PimentaCA,BragaPE,CorrêaCF.Disability relatedtochroniclowbackpain:prevalenceandassociated factors.RevEscEnfermUSP.2012;46:16–23.
3.MeziatFilhoN,SilvaGA.Disabilitypensionfrombackpain amongsocialsecuritybeneficiaries,Brazil.RevSaudePublica. 2011;45:494–502.
4.DuffyRL.Lowbackpain:anapproachtodiagnosisand management.PrimCare.2010;37:729–41.
5.ChouR.Pharmacologicalmanagementoflowbackpain. Drugs.2010;70:387–402.
6.VanMiddelkoopM,RubinsteinSM,KuijpersT,VerhagenAP, OsteloR,KoesBW,etal.Asystematicreviewonthe effectivenessofphysicalandrehabilitationinterventionsfor chronicnon-specificlowbackpain.EurSpineJ.2011;20:19–39. 7.WestromKK,MaiersMJ,EvansRL,BronfortG.Individualized
chiropracticandintegrativecareforlowbackpain:thedesign ofarandomizedclinicaltrialusingamixed-methods approach.Trials.2010;11:24.
8.SchaafsmaFG,WhelanK,vanderBeekAJ,vander
Es-LambeekLC,OjajärviA,VerbeekJH.Physicalconditioning aspartofareturntoworkstrategytoreducesicknessabsence forworkerswithbackpain.CDSRev.2013;8:CD001822. 9.PincusT,SantosR,BreenA,BurtonAK,UnderwoodM, MultinationalMusculoskeletalInceptionCohortStudy Collaboration.AreviewandproposalforaCoresetoffactors forprospectivecohortsinlowbackpain:aconsensus statement.ArthritisRheum.2008;59:14–24.
390
rev bras reumatol.2016;56(5):384–39011.DagenaisS,TriccoAC,HaldemanS.Synthesisof
recommendationsfortheassessmentandmanagementof lowbackpainfromrecentclinicalpracticeguidelines.SpineJ. 2010;10:514–29.
12.PillastriniP,GardenghiI,BonettiF,CapraF,GuccioneA, MugnaiR,etal.Anupdatedoverviewofclinicalguidelinesfor chroniclowbackpainmanagementinprimarycare.Joint BoneSpine.2012;79:176–85.
13.KoesBW,vanTulderM,LinCW,MacedoLG,McAuleyJ,Maher C.Anupdatedoverviewofclinicalguidelinesforthe managementofnon-specificlowbackpaininprimarycare. EurSpineJ.2010;19:2075–94.
14.AiraksinenO,BroxJI,CedraschiC,HildebrandtJ,
Klaber-MoffettJ,KovacsF,etal.Europeanguidelinesforthe managementofchronicnonspecificlowbackpain.EurSpine J.2006;15Suppl.2:S192–300[Chapter4].
15.FarrarJT,YoungJPJr,LaMoreauxL,WerthJL,PooleRM. Clinicalimportanceofchangesinchronicpainintensity measuredonan11-pointnumericalpainratingscale.Pain. 2001;94:149–58.
16.CecchiF,NegriniS,PasquiniG,PaperiniA,ContiAA,ChitiM, etal.Predictorsoffunctionaloutcomeinpatientswith chroniclowbackpainundergoingbackschool,individual physiotherapyorspinalmanipulation.EurJPhysRehabil Med.2012;48:371–8.
17.PardiniR,MatsudoS,AraújoT,MatsudoV,AndradeE, BraggionG,etal.Validationoftheinternationalphysical activity(IPAQ–version6):apilotstudyinyoungBrazilians. RevBrasCiencMovBrasilia.2001;9:45–51.
18.BatistoniSS,NeriAL,CupertinoAP.ValidityoftheCenterfor EpidemiologicalstudiesdepressionscaleamongBrazilian elderly.RevSaudePublica.2007;41:598–605.
19.SardaJJ,NicholasMK,PereiraIA,PimentaC,AsghariA,Cruz RM.Validationofthescaleofpaincatastrophizingthoughts. SãoPaulo:ActaFisiatra.2008;15:31–6.
20.AbreuA,FariaCD,CardosoSM,Teixeira-SalmelaLF.The Brazilianversionofthefearavoidancebeliefsquestionnaire. CadSaudePublica.2008;24:615–23.
21.DeyoRA,DworkinSF,AmtmannD,AnderssonG,Borenstein D,CarrageeE,etal.ReportoftheNIHTaskForceonResearch standardsforchroniclowbackpain.SpineJ.2014;14: 1375–91.
22.HenschkeN,vanEnstA,FroudR,OsteloRW.Responder analysesinrandomisedcontrolledtrialsforchroniclowback pain:anoverviewofcurrentlyusedmethods.EurSpineJ. 2014;23:772–8.
23.PatelS,NgunjiriA,SandhuH,GriffithsF,ThistlewaiteJ,Brown S,etal.Designanddevelopmentofadecisionsupport packageforlowbackpain.ArthritisCareRes.2014;66:925–33. 24.MainCJ,GeorgeSZ.Psychologicallyinformedpracticefor
managementoflowbackpain:futuredirectionsinpractice andresearch.PhysTher.2011;91:820–4.
25.PincusT,VlaeyenJW,KendallNA,VonKorffMR,Kalauokalani DA,ReisS.Cognitive-behavioraltherapyandpsychosocial factorsinlowbackpain:directionsforthefuture.Spine (Phila,PA1976).2002;27:E133–8.
26.DavisJA,RobinsonRL,LeTK,XieJ.Incidenceandimpactof painconditionsandcomorbidillnesses.JPainRes. 2011;4:331–45.
27.DelittoA,GeorgeSZ,VanDillenLR,WhitmanJM,SowaG, ShekelleP,etal.Lowbackpain.JOrthopSportsPhysTher. 2012;42:A1–57.