1. Master; Legal Risk Supervisor.
2. Medical Doctor; Cardiovascular Surgeon. 3. Medical Doctor; Anesthesiologist.
4. Medical Doctor; Pediatric Cardiologist - Hospital Santa Catarina Blumenau.
5. Medical Doctor; Cardiovascular Surgeon.
6. Master; Chief of the Cardiovascular Surgery Service - Hospital Santa Catarina Blumenau.
Decio Cavalet Soares ABUCHAIM1,Silvana BERVANGER2,Sergio Augusto MEDEIROS3,Juliana Spengler ABUCHAIM4,Martin BURGER5,Djalma Luis FARACO6
RBCCV 44205-1156
Extubação precoce na sala de operação após cirurgia cardíaca infantil
Early extubation of children in the operating room
after cardiac surgery
Abstract
Introduction: Early extubation is related to short lenth
of hospitalization and less complications.
Objective: Data analisys from children extubated in the
operating room after cardiac surgery with CPB.
Methods: Retrospective data analisys.
Results: From March 2006 to January 2008, 15 children
submitted to heart surgery were extubated at surgery room. Age in months was 4 to 216 (76.1 months). CPB time: 30 to 95 min (51.4 min), anoxia: 14 to 67 min (35.2 min). One patient had respiratory acidosis.
Conclusion: Early extubation in seleted patients is
possible.
Descriptors: Cardiopulmonary bypass/methods.
Anesthesia. Heart defects, congenital.
Work performed at the Hospital Santa Catarina, Blumenau, SC. Mailing address: Décio Cavalet Soares Abuchaim. Alameda Rio Branco, 805/401 – Jd. Blumenau – Blumenau, SC, Brazil – CEP: 89300-010. E-mail: decioabu@terra.com.br
Article received on June 26, 2009 Article approved on December1, 2009
Resumo
Introdução: A extubação precoce está relacionada à
diminuição do tempo de internação e de complicações.
Objetivo: Análise das características clínicas e evolução
imediata dos pacientes extubados em sala após cirurgia cardíaca infantil com CEC.
Métodos: Análise retrospectiva dos dados.
Resultados: Entre março de 2006 e janeiro de 2008, 15
pacientes, com idade de 4 a 216 meses (média 76,1 meses) foram extubados em sala. A duração da CEC variou de 30 a 95 minutos (média 51,4 min) e anóxia de 14 a 67 minutos (média 35,2 min). Um paciente apresentou acidose respiratória.
Conclusão: Extubação precoce é factível em casos
selecionados.
Descritores: Circulação extracorpórea/métodos. Anestesia.
morphine 0.05 to 0.1 mg. The anesthesia before and after CPB was maintained by sevorane and, during CPB, by propophol.
After median thoracotomy and heart exposure, it was administered a dosage of heparin 5 mg/kg, performed cannulation of the aorta and both cavas with diameters appropriate to the body surface of each patient and CPB carried out under moderate hypothermia at 25°C. The oxygenator (Edwards Life Sciences) was determined by the body surface. The cardioplegia used was the cold blood type with solution of ST Thomas (Braile Biomédica), administered in the aorta after clamping, induction dosage of 30ml/kg and repeated each 20 minutes with dosage of 20ml/kg. The hematocryt of CPB was maintained at a high level (24). The decision for extubation was made jointly by the anesthesiologist and the surgeon, at the end of thoracorraphy, individually, after evaluation of: hemodynamic stability (without vasoactive drugs), rhythm (sinus), presence of hemorrhage, cardiopathy type and age (over neonatal period).
At the end of surgery, the patients were transferred to the neopediatric intensive care unit, using a Venturi oxygen mask at 50% and there were collected biochemical exams after 30 minutes of arrival.
The Aristotle Score Risk was determined after filling out the clinical data in the chart available at the site www.aristotleinstitute.org [2].
The statistical analysis was performed with the Student’s t test, considered significant with P value lower than 0.05.
RESULTS
In the period from 3/29/2006 to 1/29/2008, 70 patients aged less than 18 years of age were operated at the Hospital Santa Catarina - Blumenau, with diagnostic of congenital cardiopathy. Among these, 20 patients were submitted to procedures without CPB (ligation of arterial conduit, section of vascular ring, bandage of pulmonary artery, correction of aortic coarctation and pericardial window) and 50 patients were submitted to procedures with CPB (atriosseptoplasty, ventriculosseptoplasty, atrioventricular septal defect, Ebstein anomaly, Jatene operation, supravalvar aortic stenosis, partial septal defect, double outlet right ventricle, subaortic membrane, correction of complex cyanotic cardiopathies using procedures type modified Blalock-Taussig, Glenn or Fontan, intracardiac foreign body, Tetralogy of Fallot, cor triatriatum. Fifteen children, aged 4 to 216 months (mean 76.1 months), were submitted to extubation in the operating room after correction of congenital cardiopathies, using cardiopulmonary bypass. There were excluded the cases of extubation for cyanotic cardiopathies, submitted to palliative surgeries and acyanotic cardiopathies corrected without CPB.
INTRODUCTION
Extubation is a critical moment in the postoperative approach of patients submitted to heart surgery. The consequences of the disease in the heart, surgical size, and physiological alterations related to the use of cardiopulmonary bypass (CPB), use of analgesics, hypothermia and inherent instabilities to the complete or partial correction of cardiopathies are factors that must be considered for the decision of ventilatory discontinuation. When extubation is performed still in the operating room, it requires a coordinated action of the assistance groups, with adequate communication of the multiprofessional team consisted by the surgeon, anesthesiologists, intensivists, physiotherapists and nurses; managing properly pain, ventilatory and hemodynamic instabilities [1].
In selected cases, this process, associated to procedures regulated by protocols established throughout hospitalization, promotes a decrease in hospital expenses, hospitalization period and complicacies, without affecting the assistance quality, being known as fast track approach. The objective of this work is analyzing the risk profile, clinical and laboratorial evolution of patients extubated in the operating room after cardiac surgery in children using CPB.
METHODS
The data from the files of children that were submitted to cardiac surgery with cardiopulmonary bypass and extubated in the operating room, for correction of congenital cardiopathies at Hospital Santa Catarina de Blumenau (SC), were acquired in a retrospective manner, by the data base TASY (Wheb Informática). The following data was collected: age, cardiopathy type, surgery performed, time of cardiopulmonary bypass, time of anoxia, values of gas partial pressure in the first gasometry performed at ICU and presence of complicacies.
The surgical technique consisted of standard procedures of the service of asepsis and antisepsis, continuous monitoring of artery and venous pressure, capnography, peripheral oxymetry, noninvasive pressure, telethermometry (nasopharyngeal and rectal) and vesical probing.
The male gender predominated, including nine (60%) cases. The diagnostic of the patients was always determined by echocardiographic diagnostic and surgery referral was carried out by the classic determinations of literature. The interatrial communication type ostium secundum (IAC OS) was observed in six patients, among these, one presenting branch stenosis and pulmonary ring; interventricular communication (IVC) in six, presenting a muscular type,
and the rest were the perimembranous type, among these, one association with pulmonary valvar stenosis. We observed a presentation of cor triatriatum, double outlet right ventricle (DORV) and relapse of the subaortic membrane (Table 1).
The time of CPB ranged from 30 to 95 minutes, with mean of 51.4 min and the time of anoxia was 14 to 67 min, with mean of 35.26 min.
Table 1. Diagnostics, procedures and age of patients in months.
Diagnostic IAC OS IVC IVC EP IAC OS EP IVC SUBAO MEMB IAC OS IVC IAC OS IVC IAC OS IVC DORV Cor Triatriatum IAC OS Surgery atriosseptoplasty ventriculosseptoplasty
ventriculosseptoplasty and pulmonary commissurotomy
atriosseptoplasty and enlargement of branch and pulmonary commissurotomy ventriculosseptoplasty resection atriosseptoplasty ventriculosseptoplasty atriosseptoplasty ventriculosseptoplasty atriosseptoplasty ventriculosseptoplasty tunnelization LV-AO resection atriosseptoplasty
Age in months 216 16 10 67 159 111 82 30 13 162 27 5 4 192 48
IAC OS: Interatrial communication type ostium secundum, IVC: Interventricular communication, SUBAO MEMB: Subaortic membrane, DORV: Double outlet right ventricle, LV-AO: Left ventricle-aorta
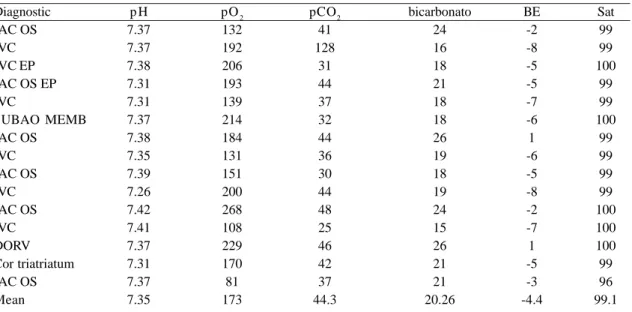
Table 2. Gasometrical data, the bottom line represents the mean value of partial pressure of gases.
Diagnostic IAC OS IVC IVC EP IAC OS EP IVC SUBAO MEMB IAC OS IVC IAC OS IVC IAC OS IVC DORV Cor triatriatum IAC OS Mean p H 7.37 7.37 7.38 7.31 7.31 7.37 7.38 7.35 7.39 7.26 7.42 7.41 7.37 7.31 7.37 7.35 pO2 132 192 206 193 139 214 184 131 151 200 268 108 229 170 81 173 pCO2 41 128 31 44 37 32 44 36 30 44 48 25 46 42 37 44.3 bicarbonato 24 16 18 21 18 18 26 19 18 19 24 15 26 21 21 20.26 BE -2 -8 -5 -5 -7 -6 1 -6 -5 -8 -2 -7 1 -5 -3 -4.4 Sat 99 99 100 99 99 100 99 99 99 99 100 100 100 99 96 99.1
After transferring the patients from the operating room to the ICU, with Venturi mask at 50%, the gasometry, along with other routine biochemical exams, was collected (Table 2). One patient presented respiratory acidosis with mild hypoxemia (PO2 81 mmHg), with progressive recovery after 30 minutes, without the need of ventilatory support or chemical reversion of anesthetic agents.
No patient required vasoactive drugs for hemodynamic support. The Venturi mask at 50% is usually applied after extubation, with oxygen flow at 15 l/min. Its use is suspended after the arterial gasometry analysis, allowing the progression to nasal oxygen, using a spectacle-type nasal catheter holder and, afterwards, natural air. The patients are only discharged from the ICU if their oxygenation is adequate without additional oxygen.
Three patients presented significant comorbidities, being Down’s syndrome, complete palatine fissure and reoperation. There were no postoperative complications or death. One extubation was involuntary, with no need of reintubation, the same was observed in patients selectively extubated.
The risk score determined by the Aristotle system varied in the basic mode from 3 to 10.3 (mean 5.48) and the advanced mode from 3 to 10.3 (mean 5.94) - Table 3.
The ICU internment ranged from 1 to18 days (mean of 3.2 days) and the hospital internment from 4 to 20 days (mean of 7.5 days). The prolonged internment time was subordinated to the need of nitroprussiate for the control of high blood pressure, according data in Table 4.
In patients with high risk score over 6, the hospital internment time was significantly longer (P = 0.04), differently from the ICU internment time. There was no correlation between the CPB time, clamping with the hospital and ICU internment time (P not significant).
DISCUSSION
There is no exact definition about what moment extubation can be considered early and this concept can be extended to patients with extubation after arrival at the Intensive Care Unit [3].In this work, we considered early extubation when performed in the operating room.
The use of the fast track approach has been encouraged for its potential benefits, especially in simple correction procedures such as interatrial communication, ventricular or persistence of arterial channel [1,4], although it can be
Table 3. Results of the Aristotle Risk Score with diagnostic.
Diagnostic
IAC OS IVC IVC EP IAC OS EP IVC
SUBAO MEMB IAC OS IVC IAC OS IVC IAC OS IVC DORV Cor triatriatum IAC OS Mean
Basic Aristotle
3 6 6 7,8
6 6,3
3 6 3 6 3 6 10,3
6,8 3 5.48
Advanced Aristotle
3 6 8 8,8
6 9,8 3,5 6 3 6 3 6 10,3
6,8 3 5.94
IAC OS: Interatrial communication type ostium secundum, IVC: Interventricular communication, SUBAO MEMB: Subaortic membrane, DORV: Double outlet right ventricle, LV-AO: Left ventricle-aorta
Table 4. ICU and hospital internment time.
Diagnostic
IAC OS IVC IVC EP IAC OS EP IVC
SUBAO MEMB IAC OS IVC IAC OS IVC IAC OS IVC DORV Cor triatriatum IAC OS Mean
ICU time
1 2 2 3 2 2 2 2 1 2 2 5 18
2 2 3.2
Hospital time
6 7 7 11
6 6 6 6 5 4 6 8 20
5 4 7.5 dias
performed in complex cardiopathies and reoperations [5]. Preisman et al. [6], comparing two groups of patients, extubated in the operating room or selectively in the postoperative unit, found no differences among mortality, reoperation due to bleeding, incidence of radiological alterations and septical or cardiologic complications. They observed a significant difference in the ICU and hospital internment time in the early group.
In our analysis, we decided to exclude the operated patients for presenting cyanotic cardiopathies; by observing that these patients would not present oxygenation similar to the rest of acyanotic cardiopathies, as it can be observed in the postoperative of the Glenn or Fontan operation, in which early extubation is acknowledgedly beneficial. Similarly, patients holding permeability of the arterial channel and vascular ring were also not included in this study for not suffering the harmful effects known in CPB, in these surgeries, except for patients operated in the neonatal period or premature babies, we always perform the extubation in the operating room.
In Brazil, Báucia & Barbero-Marcial [7], out of 441 children submitted to surgical interventions, including complex lesions and preoperative pulmonary hypertension, extubated 372 (84%) in the operating room. The postoperative complications observed presented no correlation with the procedure and there was a low rate of pulmonary complications. They concluded that most of children can be extubated early, with safety and low pulmonary complications secondary to mechanical ventilation, reduced period of ICU internment, hospitalization, children and family stress, and hospital expenses.
Essential components for the execution of the system would be techniques minimally invasive, anesthetic drugs of short duration, modified ultrafiltration and transesophagic echocardiography, enabling extubation from 80 to 90% of patients [1]. The use of electroencephalogram bispectral allows the evaluation of the degree of anesthesia and, therefore, the adequate moment for extubation [3]. The use of spinal block apparently does not alter the possibility of extubation; however, it may enable a good postoperative analgesia [8-10]. We routinely use rachianesthesia in patients over 1 year, regardless of the intention of extubation in the operating room. In these series, therefore, three patients did not receive it.
Kloth & Baum [8], in 102 children submitted to consecutive cardiac surgeries with CPB, achieved 88% of extubation in the operating room. Those late extubated were younger and presenting higher anesthetic risk. The use of spinal block with morphine did not alter the possibility of extubation and none requested special ventilatory care, reintubation or increase in the dosage of vasoactive drugs.
Mixed acidosis was occasional and did not require treatment, as we observed in one case o four experience.
Davis et al. [11] consider that the factors associated with the success of extubation in the first 24 hours of postoperative are: age over 6 months, absence of pulmonary hypertension, gestational age higher than 36 weeks and absence of cardiac insufficiency. Intraoperative factors had less relevance. On the other hand, Vida et al. [12] did not consider pulmonary hypertension to be ill-advised, extubating in the operating room 65% of a 100 patients with pulmonary hypertension and subaortic IVC.
Székely et al. [13] studied the predictors of prolonged mechanical ventilation, in 411 patients operated within a year, in order to determine factors associated to ventilation longer than 61 hours and longer than 7 days. After 61 hours, 25% (103) of the patients were still under ventilation and the factors associated were the time of CPB, the relation PaO2/FiO2 after CPB, transfusions and the hydric balance of the first day. The 38 cases that remained for more than 7 days were due to open thorax, use of nitric oxide for pulmonary hypertension, tracheobronchomalacia and peritoneal dialyses, low cardiac output syndrome and neurological events [13]. Neirotti et al. [5] reported that preoperative intubation is also a significant factor for mechanical ventilation permanence, and Prakanrattana et al. [14] related extubation with hydric balance 1/3 lower than daily recomended.
Barash et al. [15] extubated, immediately after surgery, 142 of 197 (72%) patients submitted to cardiac surgery with and without CPB (43%). There were 6% of pulmonary complications, with five (4%) reintubations, with one death not related to the function pulmonary. Schüller et al. [16] defined that early extubation presents minimal risk in selected cases, being successful in 52% of those with 3 and 12 months and 88% of those over 12 months. Out of 4 patients; 2 were reintubated and 2 died. Other authors also observed similar rate [17]. There was no need for reintubation among our cases.
REFERENCES
1. Lake CL. Fast tracking in paediatric cardiac anaesthesia: an update. Ann Card Anaesth. 2002;5(2):203-8.
2. The Aristotle Institute. Disponível em: http:// www.aristotleinstitute.org
3. Pinto Jr VC, Nunes RR, Sardenberg CRC, Branco KC, Souto Maior MM, Maia MAG, et al. Extubação imediata em cirurgia cardíaca: avaliação pelo eletroencefalograma. Rev Bras Cir Cardiovasc. 2003;18(1):53-9.
4. Soler M, Raszynski A, Kandrotas RJ, Sussmane JB, Aznavorian R, Wolfsdorf J. Fewer interventions in the immediate post-extubation management of pediatric intensive care unit patients: safety and cost containment. J Crit Care. 1997;12(4):173-6.
5. Neirotti RA, Jones D, Hackbarth R, Paxson Fosse G. Early extubation in congenital heart surgery. Heart Lung Circ. 2002;11(3):157-61.
6. Preisman S, Lembersky H, Yusim Y, Raviv-Zilka L, Perel A, Keidan I, et al. A randomized trial of outcomes of anesthetic management directed to very early extubation after cardiac surgery in children. J Cardiothorac Vasc Anesth. 2009;23(3):348-57.
7. Báucia JA, Barbero-Marcial M. Extubação precoce em cirurgia cardíaca infantil: procedimentos e resultados em seis anos de experiência. Rev Bras Cir Cardiovasc. 1992;7(3):215-20.
8. Kloth RL, Baum VC. Very early extubation in children after cardiac surgery. Crit Care Med. 2002;30(4):787-91.
9. Leyvi G, Taylor DG, Reith E, Stock A, Crooke G, Wasnick JD. Caudal anesthesia in pediatric cardiac surgery: does it affect outcome? J Cardiothorac Vasc Anesth. 2005;19(6):734-8.
10. Figueira Moure A, Pensado Castiñeiras A, Vázquez Fidalgo A, Fernández Goti C, Diéguez Fernández M, Sanduende Otero Y, et al. Early extubation with caudal morphine after pediatric heart surgery. Rev Esp Anestesiol Reanim. 2003;50(2):64-9.
11. Davis S, Worley S, Mee RB, Harrison AM. Factors associated with early extubation after cardiac surgery in young children. Pediatr Crit Care Med. 2004;5(1):63-8.
12. Vida VL, Leon-Wyss J, Rojas M, Mack R, Barnoya J, Castañeda AR. Pulmonary artery hypertension: is it really a contraindicating factor for early extubation in children after cardiac surgery? Ann Thorac Surg. 2006;81(4):1460-5.
13. Székely A, Sápi E, Király L, Szatmári A, Dinya E. Intraoperative and postoperative risk factors for prolonged mechanical ventilation after pediatric cardiac surgery. Paediatr Anaesth. 2006;16(11):1166-75.
14. Prakanrattana U, Valairucha S, Sriyoschati S, Pornvilawan S, Phanchaipetch T. Early extubation following open heart surgery in pediatric patients with congenital heart diseases. J Med Assoc Thai. 1997;80(2):87-95.
15. Barash PG, Lescovich F, Katz JD, Talner NS, Stansel HC Jr. Early extubation following pediatric cardiothoracic operation: a viable alternative. Ann Thorac Surg. 1980;29(3):228-33.
16. Schüller JL, Bovill JG, Nijveld A, Patrick MR, Marcelletti C. Early extubation of the trachea after open heart surgery for congenital heart disease. A review of 3 years’ experience. Br J Anaesth. 1984;56(10):1101-8.
17. Vricella LA, Dearani JA, Gundry SR, Razzouk AJ, Brauer SD, Bailey LL. Ultra fast track in elective congenital cardiac surgery. Ann Thorac Surg. 2000;69(3):865-71.
CONCLUSION