IN BRIEF REPORT
Health of Psychiatry Residents: Nutritional Status, Physical
Activity, and Mental Health
Matias Carvalho Aguiar Melo1&Veralice Meireles Sales de Bruin1&
Francisco das Chagas Medeiros1&José Abraão Pinheiro Santana2&
Alexandre Bastos Lima2&Elizabeth De Francesco Daher1
Received: 2 June 2015 / Accepted: 22 October 2015 / Published online: 16 November 2015 #Academic Psychiatry 2015
Abstract
Objective This study aims to analyze mental health, nutrition-al status, and physicnutrition-al activity in psychiatry residents.
Methods Sixty-two residents were invited and 59 participated (95.2 % response). Depressive, anxious, and social phobic symptoms; alcohol use; and nicotine dependence were mea-sured. Body mass index and lifestyle were also evaluated.
ResultsAlmost half of psychiatry residents were overweight or obese, and 61 % reported a sedentary lifestyle. Furthermore, 33.9 % of residents had high scores for anxiety; 30.5 % for social phobia; and 19 % for depression. In addition, 81.4 % reported alcohol use, and 22 % had harmful alcohol use. High scores for anxiety were associated with lower atten-tion and worse relaatten-tionship with preceptors, and high scores of depressive symptoms were related to a worse relationship with patients and preceptors. Anxiety was associated with
depres-sive symptoms (p<0.001) and social phobia (p=0.006).
ConclusionThe findings of this study highlight high rates of overweight/obesity, physical inactivity, and depressive and anxiety symptoms in psychiatric residents.
Keywords Medical education . Psychiatry . Nutrition . Physical activity . Mental health
The health of physicians and medical students requires special attention. It can reflect on relationships with patients and impair
their diagnosis and treatment [1]. Physicians and medical
students often delay search for professional help, and
self-diagnosis and self-treatment are common practices [2]. Rates
of stress, depression, and suicide in physicians and medical
students are high [3], and studies show that medical students
have higher rates of overweight, obesity, and physical inactivity
when compared to students in other fields [4]. Medical
resi-dents combine a double load of stress. They are at the same time physicians and students. Although still in training, they
assume great responsibilities [5]. Few studies focus on
resi-dents’health. Therefore, this study aims to analyze psychiatric
symptoms, nutritional status, and physical activity in psychiatry residents.
Methods
We conducted a cross-sectional study based on questionnaires and self-administered scales from December 2013 to July 2014. We invited all psychiatry residents of four institu-tions located in northeastern Brazil to participate. Admissions in a residency program for at least 1 month was the inclusion criterion, and vacation or absences for health reasons were exclusion criteria.
We d e s i g n e d a s t r u c t u r e d q u e s t i o n n a i r e w i t h sociodemographic and professional information, including weight, height, and frequency and type of physical activity. We also used five validated scales. Residents assessed their performance on the following criteria: assiduity, punctuality, theoretical knowledge, practical knowledge, attention, relation-ship with patients, relationrelation-ship with colleagues, relationrelation-ship with preceptors, and overall performance. Each item was clas-sified into three categories: unsatisfactory, satisfactory, or high-ly satisfactory. A sedentary lifestyle was defined as activities with duration less than 30 min three times per week (for anaer-obic exercise) and five times per week (for aeranaer-obic exercise).
* Matias Carvalho Aguiar Melo matcarv01@yahoo.com.br
1
Federal University of Ceará, Fortaleza, Ceará, Brazil
2
Public Health School of Ceará, Fortaleza, Ceará, Brazil Acad Psychiatry (2016) 40:81–84
We estimated the nutritional status by body mass index (BMI), which is calculated by dividing the weight by the square of the height. Nutritional status was classified as
un-derweight (BMI <18.5 kg/m), normal weight (BMI 18.5–
24.9) overweight (BMI 25–29.9), and obese (BMI >30).
Obesity can be stratified into mild (BMI 30–34.9), moderate
(BMI 35–39.9), and severe (BMI >40).
We scored depressive symptoms by the Beck Depression Inventory-II (BDI-II). It is composed of 21 self-applied ques-tions, and each item ranges from 0 to 3 points. A score greater than 10 suggests depression.
We measured anxiety symptoms with the Beck Anxiety Inventory (BAI). It assesses 21 symptoms for 1 week, scaled
0–3, with increasing gradation of anxiety. The sum of scores
indicates the degree of anxiety: 0–7=minimal anxiety, 8–15=
mild anxiety, 16–25=moderate anxiety, and 26–63=severe
anxiety. In this study, our definition of anxiety was a score of 8 or above. The Social Phobia Inventory (SPIN) lists 17 phobic symptoms reported in the last week. A total score of 19 points or above suggests social anxiety disorder.
We used the Alcohol Use Disorders Identification Test (AUDIT), which is composed of ten questions, to gather data on intensity, frequency, harmful use, symptoms of addiction, and loss of use of the substance. We adopted eight as the cutoff score to harmful use of alcohol.
The Fagerström Test is a scale with six items, each ranging from 0 to 10 points, that stratifies nicotine dependence into
five levels: very low (0–2 points), low (3–4 points), moderate
(5 points), high (6–7 points), and very high (8–10 points).
The research was approved by two local research ethics
committees in Brazil. We guaranteed participants’anonymity
and avoided exposure of data that could identify or embarrass them. Participation was voluntary. All participants signed an informed consent form, and the residents were free to leave the study at any time.
Statistical Analysis
We calculated mean BMI scores and subsequently defined two groups. Residents with BMI of 25 or more were classified as overweight/obese, whereas others were classified with nor-mal weight. We analyzed differences in sociodemographic or occupational data and academic performance, comparing both
groups. We used thettest (for continuous variables) and the
chi-square test (for dichotomous variables). In cases where the chi-square could not be used by the size or distribution of the
sample, we chose the Fisher’s exact test.
Residents were also divided into sedentary living or not on the basis of responses to the amount of physical activity and compared the two groups again, as described above. The same procedure was repeated with the BDI-II, BAI, SPIN, and AUDIT according to the cutoff points of each scale. All the
statistical analyses were performed using SPSS Version 17.0.
Statistical significance was considered atpvalue <0.05.
Results
We invited 62 residents to participate; 1 declined and 2 could not be contacted. Therefore, 59 participated (response rate, 95.2 %). Most were male (61.4 %) and single (68.4 %) and younger than 30 years (64.4 %). Among psychiatry residents, 44.1 % were first year residents; 28.8 %, second year; and 22 %, third year; and 5.1 % were in the fourth (optional) year on child and adolescent psychiatry.
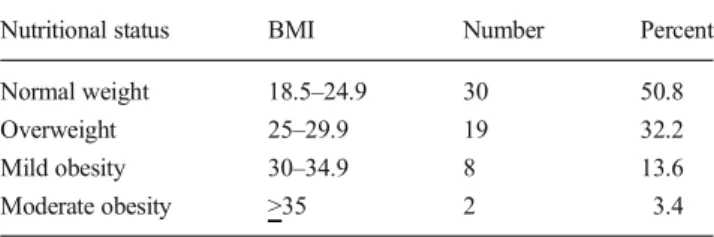
The BMI ranged from 18.5 to 35.07 (mean=25.8). Among
participants, 49.2 % had high BMI values (Table1). None had
BMI below the recommended values. Considering gender, 62.1 % of men were overweight or obese, in comparison with 27.3 % of women. There was a relationship between gender and
overweight/obesity (p=0.010). The mean BMI was 23.9 for
fe-males and 26.9 for fe-males but no association between BMI and sociodemographic variables or academic performance.
In physical activity, 37.3 % did not exercise even once a week and 61 % were sedentary. Among residents who partic-ipated in physical activities, 56.7 % engaged in body building, 10.8 % walking, 5.1 % running, and 5.1 % dancing and 16.2 % practiced other activities. Married residents had a more
sedentary lifestyle (p=0.020). There was no association
be-tween sedentary lifestyle and other sociodemographic vari-ables, nutritional status, or academic performance.
Depressive symptoms ranged from 0 to 31 points in the BDI-II with a mean of 6.71. Among the participants, 19 % scored more than 10 points in BDI-II cutoff level. We found no association with sociodemographic variables, nutritional status, and sedentary lifestyle.
We scored symptoms of anxiety from 0 to 25 points on the BAI, with a mean of 6.2. Among participants, 33.9 % scored more than 7 points in the BAI (cutoff level). In this group, 75 % had mild anxiety symptoms, 20 % moderate anxiety symptoms, and 5 % severe anxiety symptoms. Residents who scored more than 7 points on the BAI were also more
sedentary (p= 0.048). We found no association with
sociodemographic variables and nutritional status.
Table 1 Nutritional status of psychiatry residents
Nutritional status BMI Number Percent
Normal weight 18.5–24.9 30 50.8
Overweight 25–29.9 19 32.2
Mild obesity 30–34.9 8 13.6
Moderate obesity >35 2 3.4
In SPIN, social phobia scores ranged from 0 to 45 points (mean=13.78). According to this scale, 30.5 % of residents had 19 points or more, suggesting social anxiety disorder. Higher scores for social phobic symptoms were associated
with single marital status (p= 0.006). No association was
found with other sociodemographic variables, nutritional sta-tus, and sedentary lifestyle. Symptoms of anxiety were
signif-icantly associated with depressive symptoms (p<0.001) and
social phobia (p=.003). There was no significant association
between depressive symptoms and social phobia (p=0.195).
Regarding academic performance, residents with scores greater than 7 points in the BAI were associated with less
attention (p=0.012) and worse relationships with preceptors
(p=0.013). Residents with higher scores for depressive
symp-toms on the BDI were associated with worse relationship with
patients (p=0.047) and preceptors (p=0.016). Social phobia
was not related to any specific area of academic performance. Three psychiatry residents (5.1 %), all male, smoked. Two residents had 1 or 2 points in the Fagerström Test (minimal nicotine dependence); the third scored 5 in this scale (moder-ate nicotine dependence). Among residents, 81.4 % used al-cohol and 22 % scored 8 points or more in AUDIT, suggesting a harmful alcohol use. The AUDIT scores ranged from 0 to 16 points (mean=4.4). We did not find any association with harmful alcohol use and sociodemographic variables, nutri-tional status, or sedentary lifestyle, nor did we find statistically significant association concerning academic performance.
Discussion
This is the first study that investigates physical and mental health specifically in psychiatry residents who, despite little experience, are chronically subjected to daily stress with pa-tients who have mental disorders.
Almost half of psychiatry residents were overweight or obese. This value is higher than that found in the local youth population. When stratified for gender, the percentage of over-weight or obesity corresponds to 27.3 % in women and 62.1 % men. This large discrepancy between genders is not identified in the general adult population in Brazil. Another study, how-ever, found an inverse association between both educational
levels and BMI in women but not men [6].
The percentage of residents who reported that they did not practice physical activities (37.3 %) was much higher than that in the local population, even when considering only people with the same education level (22.5 %). This finding is in keeping with other studies concerning lower physical activity in medical students and a progression of physical inactivity
throughout medical school [7].
The high rates of depressive and anxiety symptoms in-dicate the need to care for the mental health of psychiatric residents. Depression and anxiety can result in serious
damage to residents and to patients. Overwork and respon-sibilities, lack of time, fear of making mistakes, and per-fectionism justify high levels of anxiety in this population
[8]. We identified an association between depression and
worse relationships with patients and preceptors. This find-ing seems consistent because depression affects mood and social interaction. It can cause poorer treatment adherence
and worse outcomes among patients [9].
Symptoms of anxiety were significantly associated with lower attention and poorer relationship with preceptors. Subjected to attention tests, students with higher levels of anxiety are more susceptible to errors, slow performances,
and lower effectiveness of learning [10]. The relationship with
tutors, teachers, or superiors has not been analyzed in other studies. This study showed a consistent relationship between anxiety symptoms and physical inactivity. Physical activity inhibits release of free radicals, has an anti-inflammatory func-tion, and acts on neuroplasticity by modulating the expression of neurotrophins. Therefore, exercise may improve symptoms
of anxiety [11].
Symptoms of anxiety also were associated with social pho-bic and depressive symptoms. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, characterizes so-cial phobia by anxiety symptoms in performance situations and interpersonal contact. The comorbidity of anxiety disor-ders and depressive episodes is well documented. Furthermore, affective and anxiety symptoms can integrate a
similar clinical pathophysiology and treatment [12].
More than 80 % of respondents consumed alcohol. According to AUDIT, 22 % were alcohol dependent. These high rates support a progression of alcohol consumption among medical students throughout the university and
after graduation [13].
The study has some limitations. The small sample can hin-der extrapolation to other populations. Specificities of the lo-cal population and residency programs must be considered. In Brazil, where this study was conducted, psychiatry residency lasts 3 years, with a workload of 60 h per week and a salary around US$1100, monthly. Many residents work outside the residency, which can contribute to increased stress and higher rates of anxiety and depression. Another important aspect is the absence of a control group of residents from other special-ties, which could clarify if some of these features are specific to psychiatry residents or common to other residents. Furthermore, the self-reported information can affect the reli-ability of the data, mainly academic performance.
In summary, this study highlights high levels of weight, physical inactivity, and depressive and anxiety symptoms in psychiatric residents. In addition, psychiatric symptoms were associated with poor performance in specific academic fields. Studies comparing residents of other specialties are suggested. Prospective studies that follow residents over the years could provide additional information.
Acknowledgments The authors wish to thank all the psychiatry resi-dents for participating in the study.
Compliance with Ethical Standards The research was approved by two local research ethics committees in Brazil. We guaranteed partici-pants’anonymity and avoided exposure of data that could identify or embarrass them. Participation was voluntary. All participants signed an informed consent form, and the residents were free to leave the study at any time.
Disclosure This study was funded by the authors. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
1. Steinbrook R. The debate over residents’work hours. N Engl J Med. 2002;347:1296–302.
2. Montgomery AJ, Bradley C, Rochfort A, Panagopoulou E. A re-view of self-medication in physicians and medical students. Occup Med. 2011;61:490–7.
3. Bright RP, Krahn L. Depression and suicide among the physicians. C u r r p s y c h i a t r y. 2 0 11 ; 1 0 . Av a i l a b l e a t h t t p : / / w w w. currentpsychiatry.com/home/article/depression-and-suicide-among-physicians/b1d152751a0bb7bf9e4c2b5aeb2a416e.html. Accessed 10 May 2015.
4. Mota MC, De-Souza DA, Mello MT, Tufik S, Crispim CA. Lifestyle and medical education: impact on the nutritional profile. Rev Bras Educ Med. 2012;36:358–68.
5. Martins LAN. Residência médica: estresse e crescimento. 1st ed. São Paulo: Casa do Psicólogo; 2005.
6. Maddah M, Eshraghian MR, Djazayery A, Mirdamadi R. Association of body mass index with educational level in Iranian men and women. Eur J Clin Nutr. 2003;57:819–23.
7. Dabrowska-Galas M, Plinta R, Dabrowska J, Skrzypulec-Plinta V. Physical activity in students of the Medical University of Silesia in Poland. Phys Ther. 2013;93:384–92.
8. Silva GCC, Koch HA, Sousa EG, Gasparetto E, Buys RC. Anxiety and depression among medical residents in radiology and diagnos-tic imaging. Rev Bras Educ Med. 2010;34:1999–2006.
9. Zolnierek KBH, Dimatteo MR. Physician communication and pa-tient adherence to treatment: a meta-analysis. Med Care. 2009;47: 826–34.
10. Mancevska S, Pluncevic-Gligoroska J, Dejanova B, Petrovska S, Bozinovska L. Attention and learning in medical students with high anxiety. Neurosci Lett. 2011;500:46–7.
11. Moylan S, Eyr HA, Maes M, Baune BT, Jacka FN, Berk M. Exercising the worry away: how inflammation, oxidative and nitro-gen stress mediates the beneficial effect of physical activity on anxiety disorder symptoms and behaviours. Neurosci Biobehav Rev. 2013;37(4):573–84.
12. Hirschfeld RMA. The comorbidity of major depression and anxiety disorders: recognition and management in primary care. Prim Care Companion J Clin Psychiatry. 2001;3(6):244–54.
13. Newbury-Birch D, White M, Kamali F. Factors influencing alcohol and illicit drug use amongst medical students. Drug Alcohol Depend. 2000;59(2):125–30.