© 2014 Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista. Published by Elsevier Editora Ltda. All rights reserved.
Radial vs. Femoral Artery Access in Elderly Patients
Undergoing Percutaneous Coronary Intervention
Cleverson Neves Zukowski
1, Iáscara Wozniak
1, Newton Fernando Stadler de Souza Filho
1,
Emile Alencar Cordeiro
1, Alessandro Rell
1, Marisa Leal
1, Jackson Stadler
1,
José Augusto Ribas Fortes
1, Rodrigo Cerci
2ABSTRACT
Background: Studies demonstrate that radial artery access
reduces the risk of vascular and bleeding complications associ-ated to percutaneous coronary intervention. Our objective was to evaluate in-hospital results of the transradial approach in elderly patients undergoing percutaneous coronary intervention. Methods: Prospective registry including patient’s ≥ 70 years
of age; safety and eficacy endpoints were compared for the radial and femoral artery access groups. Results: We included 255 patients, 117 (52%) treated using the radial approach and 108 using the femoral approach. Except for age, the remain-ing clinical characteristics did not show differences between groups. Male patients prevailed (60%), 36.7% were diabetic and over one third were diagnosed with acute coronary syndrome. Angiographic and procedure-related variables did not show differences between groups. When vascular complication rates were compared only hematomas < 5 cm (5.1% vs. 17.6%; p
< 0.01) were more prevalent with the femoral access. Major bleedings, according to the ACUITY criteria (zero vs. 5.6%;
p = 0.01) and minor bleedings, according to the TIMI criteria (zero vs. 7.4%; p < 0.01), were also more frequent in the femoral group. In-hospital clinical endpoints, death (0.9% vs. 5.6%; p = 0.06) and non-fatal infarction (zero vs. 3.7%; p = 0.05) were more frequent in patients treated by the femoral access. Conclusions: In a non-selected patient population ≥
70 years of age, percutaneous coronary intervention by radial access was associated to a lower incidence of in-hospital clinical endpoints, especially of bleeding events related to the vascular access route.
DESCRIPTORS: Femoral artery. Radial artery. Percutaneous
coronary intervention. Aged.
1 Santa Casa de Curitiba, Pontifícia Universidade Católica de Curitiba, Curitiba, PR, Brazil.
2 Quanta Diagnóstico e Terapia, Curitiba, PR, Brazil.
Correspondence to: Cleverson Neves Zukowski. Rua Francisco Rocha, 1.640/1.104 − Bigorrilho − CEP: 80730-390 − Curitiba, PR, Brazil E-mail: cleverzuk@yahoo.com.br
Received: 05/26/2014 • Accepted: 06/01/2014
RESUMO
Acesso Radial vs. Acesso Femoral em Pacientes com Idade Avançada Submetidos à
Intervenção Coronária Percutânea
Introdução: Estudos demonstram que o acesso via artéria
radial diminui o risco de complicações vasculares e hemor-rágicas associadas à intervenção coronária percutânea. Nosso objetivo foi avaliar os resultados hospitalares da utilização da via radial em pacientes idosos submetidos à intervenção coro-nária percutânea. Métodos: Registro prospectivo, que incluiu pacientes ≥ 70 anos, tendo sido comparados os desfechos de
segurança e de eicácia entre os grupos tratados pelas vias radial e femoral. Resultados: Incluímos 225 pacientes, sendo 117 (52%) tratados por via radial e 108 por via femoral. À exceção da idade, as demais características clínicas não mostraram diferenças entre os grupos. Predominaram os pacientes do sexo masculino (60%); 36,7% eram diabéticos e mais de um terço foi tratado na vigência de quadro de síndrome coronária aguda. As variáveis angiográicas e do procedimento não mostraram diferenças entre os grupos. Na comparação das taxas de complicações vasculares, somente os hematomas < 5 cm (5,1% vs. 17,6%; p < 0,01) foram mais prevalentes no acesso femoral. Sangramentos maiores, pelo critério ACUITY (zero vs. 5,6%; p = 0,01), e menores, pelo critério TIMI (zero vs. 7,4%; p < 0,01), também foram mais frequentes no grupo femoral. Os desfechos clínicos hospitalares óbito (0,9% vs. 5,6%; p = 0,06) e infarto não fatal (zero vs. 3,7%; p = 0,05) incidiram mais frequentemente nos pacientes tratados por via femoral. Conclusões: Em uma população não selecionada de pacientes com idade ≥ 70 anos, a intervenção
coronária percutânea por via radial esteve associada à menor incidência de desfechos clínicos hospitalares, em especial de eventos hemorrágicos relacionados à via de acesso vascular.
DESCRITORES: Artéria femoral. Artéria radial. Intervenção
coronária percutânea. Idoso.
T
he femoral approach has remained, for more than two decades, as the main access route in percuta-neous coronary intervention (PCI). Recent studies show that the choice of radial access is associated with considerable reduction in the risk of vascular and bleeding complications.1-3 Nevertheless, the radialtech-nique still represents less than 10% of the approaches used in PCI worldwide, which can be explained by the demand for greater skill of the interventionist and for a longer learning curve.1 These facts are related
to the characteristics of the vessel (of smaller caliber than the femoral artery), the anatomic variations, and the potential to cause arterial spasm.4
Although increasingly potent antithrombotic and antiplatelet drugs have reduced ischemic events re-lated to PCI, the increase of bleeding complications associated with the procedure can lead to increased morbimortality.1,4,5 In this scenario, no strategy has
caused greater impact than the use of the radial artery rather than femoral access in the reduction of bleeding events related to PCI.6
Among the independent predictors of bleeding related to PCI, older age has been demonstrated as an independent risk factor in several studies.7,8 This fact
should lead to greater use of the radial approach in this population; however, due to the greater degree of atherosclerosis, calciication, and tortuosity of small- and medium-caliber vessels in this age group, PCI by radial approach can lead to higher failure rate, prolonged procedure, use of a greater amount of contrast, and greater exposure to radiation.9
The present study aimed to compare the clinical in-hospital outcome of transradial access use when compared with the femoral approach in patients aged
≥ 70 years submitted to PCI.
METHODS
Population
This study included consecutive patients aged ≥
70 years undergoing PCI in two high-volume hospital services in Curitiba (PR) from January 2012 to November 2013. Clinical and epidemiological data, as well as in-hospital clinical events, were collected and stored in the database, comparing the outcomes of safety and eficacy of the cohort submitted to PCI by radial approach vs. femoral access. The interventionists performing the procedures were skilledin both techniques.
At least 24 hours pre-PCI, patients treated electively received acetylsalicylic acid (loading dose of 300 mg and maintenance dose of 100 mg/day) and clopido-grel (loading dose of 300 mg and maintenance dose of 75 mg/day). Urgency or emergency cases, without enough time for the pre-treatment, received a loading
dose of clopidogrel of 600 mg or ticagrelor (loading dose of 180 mg and maintenance dose of 90 mg every 12 hours). All patients were instructed to maintain the dual antiplatelet therapy for at least one month in the case of bare-metal stent implantation, and for one year, if drug-eluting stents were used.
The stent implantation technique, the vascular access route, stent type, and the medications used during the procedure were chosen at the discretion of the interventionist.
Definitions
Regarding eficacy endpoints, combined cardio-vascular and cerebrocardio-vascular events (ECCAM), death, stroke, acute myocardial infarction (AMI), and target vessel revascularization (TVR) were evaluated, as well as the rates of these isolated events. Death was de-ined as death from any cause that occurred during hospitalization. Periprocedural AMI was deined as the presence of new Q-waves in two or more contiguous leads, or as elevation of creatine kinase MB isoenzyme (CK-MB) at least three times higher than the normal upper level. In cases of AMI, the 20% increase in CK-MB in comparison to previous levels was considered a diagnostic of reinfarction.
Regarding safety outcomes, vascular and bleeding complications were evaluated according to the Throm-bolysis in Myocardial Infarction (TIMI)10 and ACUITY11
criteria. According to ACUITY, bleeding events were considered major (intracranial hemorrhage, intraocular hemorrhage, hematoma ≥ 5 cm in diameter, bleeding
at the puncture site requiring intervention, any appar-ent bleeding with decrease in hemoglobin ≥ 3 mg/dL,
decrease in hemoglobin ≥ 4 mg/dL without apparent
site of bleeding, or need for transfusion) or minor (any bleeding which did not it the above deinition). According to the TIMI criteria, bleeding was considered as major (intracranial hemorrhage, clinically signiicant bleeding associated with a decrease in hemoglobin > 5 g/dL, or fatal bleeding), minor (any clinical signs of bleeding associated with the decrease in hemoglobin of 3 g/dL to 5 g/dL), or minimal (any clinical signs of bleeding associated with a decrease in hemoglobin < 3 g/dL).
STATISTICAL ANALYSIS
Continuous variables were described as means ±
standard deviations and compared by Student’s t-test
for independent variables or the Mann-Whitney test, according to their distribution. Categorical variables were presented as percentages and compared using the chi-squared test or Fisher’s exact test, when appropriate. The effect of the access routeon vascular and bleed-ing complications was determined usbleed-ing a multivariate logistic regression model, adjusted for variables with
inal model was adjusted for the presence of diabetes, gender, and body mass index. Statistically signiicant results were those with p < 0.05. The SPSS version 12.0 (SPSS Inc., Chicago, United States) was used in the analyses.
Ethical aspects
This study was approved by the Ethics Commit-tee of the Pontifícia Universidade Católica do Paraná (PUC-PR), number 459.434, with CAAE identiication number 24075513.8.0000.0020 in the Brazil platform. Patients were included in the study after signing an informed consent.
RESULTS
Between January 2012 and November 2013, 832 consecutive patients underwent PCI at the participat-ing institutions, performed by interventionists skilled in both techniques. Of these, 225 (27%) were aged ≥ 70
years, of whom 117 (52%) were treated by transradial and 108 by femoral approach.
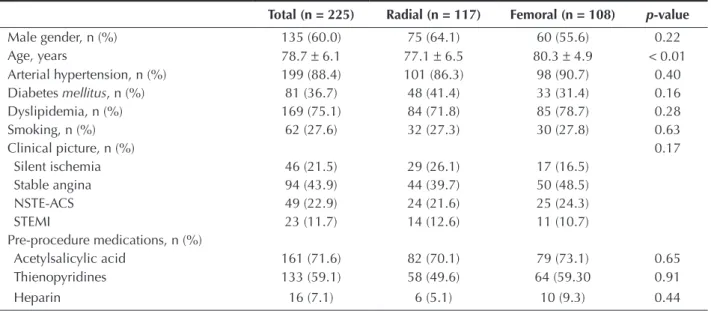
Except for age (77.1 ± 6.5 years vs. 80.3 ± 4.9
years; p < 0.01), the other clinical characteristics did not differ between the groups (Table 1).
The male gender predominated (60%), 36.7% were diabetics, and more than one-third underwent PCI in the presence of an acute coronary syndrome.
Regarding the procedure and angiographic vari-ables (Table 2), approximately half the patients had
involvement of two or three vessels, of which 11.6% were restenotic lesions; 8.0% had bifurcations lesions, and 4.9% had chronic occlusions, with no differences between the groups. Drug-eluting stents were used less often in the transradial than in the femoral group (30.5% vs. 42.3%; p = 0.04). The amount of contrast medium used was 135 ± 28 mL in the radial group and 128 ± 23 mL in the femoral group (p = 0.22). There was no difference between the luoroscopy time between the groups (11.3 ± 6 vs. 10.5 ± 5 minutes; p = 0.47).
The in-hospital clinical outcomes (Table 3) death (0.9% vs. 5.6%; p = 0.06), non-fatal AMI (3.7% vs. 0; p = 0.05), and MACCE (0.9% vs 9.2%; p < 0.01)
were more frequently observed in the group undergoing PCI through the femoral artery. There was no stroke nor TVR in any of the patients analyzed.
In the total sample, 21% of patients had a vascular complication, which ranged from minor hematomas to pseudoaneurysm formation requiring surgical intervention. It is noteworthy that no patient undergoing intervention through the radial access had major bleeding by any of the criteria, and there was no need for surgical correc-tion of vascular complicacorrec-tions in this group.
When comparing the rates of vascular complications, no differences were found between the groups, except for hematomas < 5 cm, which were more prevalent in the femoral access group (5.1% vs. 17.6%; p < 0.01).
Bleeding defined by ACUITY and TIMI scores was numerically more frequent in the femoral group, showing statistical signiicance for the highest ACUITY
TABLE 1 Clinical Characteristics
Total (n = 225) Radial (n = 117) Femoral (n = 108) p-value
Male gender, n (%) 135 (60.0) 75 (64.1) 60 (55.6) 0.22 Age, years 78.7 ± 6.1 77.1 ± 6.5 80.3 ± 4.9 < 0.01
Arterial hypertension, n (%) 199 (88.4) 101 (86.3) 98 (90.7) 0.40 Diabetes mellitus, n (%) 81 (36.7) 48 (41.4) 33 (31.4) 0.16 Dyslipidemia, n (%) 169 (75.1) 84 (71.8) 85 (78.7) 0.28 Smoking, n (%) 62 (27.6) 32 (27.3) 30 (27.8) 0.63
Clinical picture, n (%) 0.17
Silent ischemia 46 (21.5) 29 (26.1) 17 (16.5) Stable angina 94 (43.9) 44 (39.7) 50 (48.5)
NSTE-ACS 49 (22.9) 24 (21.6) 25 (24.3)
STEMI 23 (11.7) 14 (12.6) 11 (10.7)
Pre-procedure medications, n (%)
Acetylsalicylic acid 161 (71.6) 82 (70.1) 79 (73.1) 0.65 Thienopyridines 133 (59.1) 58 (49.6) 64 (59.30 0.91
Heparin 16 (7.1) 6 (5.1) 10 (9.3) 0.44
TABLE 2
Angiographic and procedural characteristics
Total (n = 225) Radial (n = 117) Femoral (n = 108) p-value
Number of vessels, n (%) 0.11
One-vessel 110 (48.9) 60 (51.3) 50 (46.3) Two-vessel 63 (28.0) 27 (23.1) 36 (33.3) Three-vessel 52 (23.1) 30 (25.6) 22 (20.4)
Restenotic lesion, n (%) 26 (11.6) 16 (13.7) 10 (9.3) 0.40 Bifurcation lesion, n (%) 18 (8.0) 11 (9.4) 7 (6.5) 0.47 Chronic occlusion, n (%) 11 (4.9) 5 (4.3) 6 (5.6) 0.76 Ulcerated lesion, n (%) 16 (7.1) 6 (5.1) 10 (9.3) 0.30 Calciied lesion, n (%) 26 (11.6) 16 (13.7) 10 (9.3) 0.40
Sheath caliber, n (%) 0.17
5 F 16 (7.1) 16 (14.0) 0
6 F 195 (86.6) 99 (84.6) 96 (92.3)
7 F 10 (5.3) 2 (1.7) 8 (7.7)
Stent type, n (%) 0.04
Bare metal 189 (63.9) 107 (69.5) 82 (57.7) Drug-eluting 107 (36.1) 47 (30.5) 60 (42.3)
Full revascularization, n (%) 115 (55.0) 64 (57.1) 51 (52.6) 0.57 Contrast volume, mL 131.5 ± 26 135 ± 28 128 ± 23 0.22
Time of luoroscopy, minute 10.9 ± 6 11.3 ± 6 10.5 ± 5 0.47
TABLE 3
In-hospital clinical outcomes
Total (n = 225)
Radial (n = 117)
Femoral
(n = 108) p-value
Death, n (%) 7 (3.1) 1 (0.9) 6 (5.6) 0.06
AMI, n (%) 4 (1.8) 0 4 (3.7) 0.05
MACCE, n (%) 11 (4.9) 1 (0.9) 10 (9.2) < 0.01
Vascular complications, n (%)
Vessel occlusion 1 (0.2) 0 1 (0.9) 0.48
Hematoma < 5 cm 25 (11.1) 6 (5.1) 19 (17.6) < 0.01
Hematoma > 5 cm 5 (2.2) 5 (4.3) 5 (4.6) > 0.99
Retroperitoneal hematoma 1 (0.2) 0 1 (0.9) 0.48 Pseudoaneurysm, nosurgical correction 11 (7.2) 5 (4.3) 8 (7.3) 0.40 Pseudoaneurysm, withsurgical correction 3 (1.3) 0 3 (2.8) 0.11 Bleeding (ACUITY), n (%)
Minor 23 (10.2) 8 (6.8) 15 (13.9) 0.12
Major 6 (2.7) 0 6 (5.6) 0.01
Bleeding (TIMI), n (%)
Minimum 19 (8.4) 8 (6.8) 11 (10.2) 0.47
Minor 8 (3.6) 0 8 (7.4) < 0.01
Major 2 (0.9) 0 2 (1.8) 0.23
criterion (0 vs. 5.6%; p = 0.01), and the lowest of the TIMI criterion (0 vs. 7.4%; p < 0.01).
In the multivariate analysis, female gender was an independent predictor of vascular complications, and age was an independent predictor of bleeding. The only protective factor for the occurrence of the two com-plications was the use of radial access route (Table 4).
DISCUSSION
When comparing radial and femoral access in the performance of the PCI, the ideal strategy should offer reduced vascular and bleeding complications, which obviously affect post-procedure clinical evolu-tion, while avoiding increased procedure time and/or radiation exposure.12,13
The irst studies to compare the radial and femoral techniques suggested that the irst, albeit safer, might not be suitable for widespread use in interventional procedures, as it increased procedure time and the amount of contrast; induced arterial spasm and caused discomfort to the patient; and promoted greater radia-tion exposure.14 However, with the increasing
experi-ence of the interventionist, improved materials, and drug therapy used in the prevention of vasospasm, that which was unreachable became attainable. The most inluential factor regarding technical success has been the interventionist’s experience. In the present study, only interventionists skilled in the radial technique participated in the procedures.
In a previously reported registry, it was demon-strated that a volume > 80 cases/year per surgeon signiicantly decreased failure of the radial approach and the time of procedure.15 Other studies similarly
showed a reduction of radiation exposure, as surgeons’ experience increased.14,16
The use of the radial approach reduces the percent-age of vascular complications when compared to the femoral approach.3,6 In the present study, 11% of patients
had major complications related to the vascular access site, such as pseudoaneurysm, large hematoma (at the puncture site or even retroperitoneal), and vessel oc-clusion. The use of the radial access reduced not only the major vascular complications, but also bleeding complications, deined by the two different pre-speciied classiications. Several analyses have demonstrated the superiority of the radial approach in reducing rates of bleeding, particularly in high-risk populations, such as women,17 the elderly,18 and patients with acute coronary
syndrome.19
Few studies have evaluated the radial vs. femo-ral approach in the subgroup of elderly patients undergoing PCI. These studies included diagnostic procedures in the comparison, which does not require such a vast array of antiplatelet and antithrombotic drugs, a condition that greatly increases the risk of bleeding.9 Another study, which compared the two
approaches in the elderly population undergoing PCI, did not analyze detailed outcomes related to bleed-ing.18 In a national series, of a group with extensive
experien ce in radial access, there was no comparison with a control group of patients treated via femoral approach.20 Thus, the data of this study’s population
corroborate the fact that the greater the potential for bleeding and vascular complications of a patient, the greater the benefit of considering the radial access as a priority when performing PCI.
In the studied population, an overall rate of in-hospital mortality of 3.1% was observed, with a marginal statistical difference between the radial and femoral groups.
Although the RIVAL study, with over 7,000 pa-tients enrolled, demonstrated a reduction in mortality in the subgroup analysis of patients with STEMI, only a population > 17,000 patients could consistently demonstrate this reduction in the presence of acute coronary syndrome.3 The authors consider the higher
overall mortality in the femoral access group a result of selection bias. As this was a pragmatic observational study with broad inclusion, the use of femoral access may have been preferred in clinically more severe patients with hemodynamic instability.
Study limitations
Limitations included: the fact that this was an observational registry of clinical practice, subject to selection bias observed in non-randomized samples; the small number of patients included in the study; and the lack of late clinical follow-up.
TABLE 4
Predictors of vascular complications and bleeding
OR 95% CI p-value
Vascular complications
Radial access 0.26 0.12-0.56 < 0.01
Female gender 2.44 1.16-5.13 0.02 BMI < 22 1.05 0.39-2.81 0.93
Diabetes mellitus 0.63 0.33-1.22 0.17
Bleeding
CONCLUSIONS
In an unselected population of patients aged ≥ 70
years undergoing percutaneous coronary intervention, radial approach was associated with a lower incidence of in-hospital clinical outcomes, especially bleeding events related to the access route.
CONFLICTS OF INTEREST
The authors declare no conlicts of interest.
FUNDING SOURCE
None.
REFERENCES
1. Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or interven-tion and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157(1):132-40.
2. Cantor WJ, Mahaffey KW, Huang Z, Das P, Gulba DC, Glezer S, et al. Bleeding complications in patients with acute coronary syndrome undergoing early invasive man-agement can be reduced with radial access, smaller sheath sizes, and timely sheath removal. Catheter Cardiovasc Interv. 2007;69(1):73-83.
3. Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicentre trial. Lancet. 2011;377(9775):1409-20.
4. Yoo BS, Yoon J, Ko JY, Kim JY, Lee SH, Hwang SO, et al. Anatomical consideration of the radial artery for transradial coronary procedures: arterial diameter, branching anomaly and vessel tortuosity. Int J Cardiol. 2005;101(3):421-7. 5. Zukowski CN, Costa Jr JR, Costa R, Esteves V, Staico R,
Siqueira D, et al. Preditores e impacto clínico intra-hospitalar do sangramento associado à intervenção coronária percutânea. Rev Bras Cardiol Invasiva. 2010;18(3):281-7.
6. Rao SV, Cohen MG, Kandzari DE, Bertrand OF. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55(20):2187-95.
7. Nikolsky E, Mehran R, Dangas G, Fahy M, Na Y, Pockok S. Development and validation of a prognostic risk score for major bleeding in patients undergoing percutaneous coronary intervention via the femoral approach. Eur Heart J. 2007;28(16):1936-45.
8. Collet JP, Montalescot G, Lison L, Choussat R, Ankri A, Drobinski G. Percutaneous coronary intervention after sub-cutaneous enoxaparin pretreatment in patients with unstable angina pectoris. Circulation. 2001;103(5):658-63.
9. Louvard Y, Benamer H, Garot P, Hildick-Smith D, Loubeyre C, Rigattieri S. Comparison of transradial and transfemo-ral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol. 2004;94(9):1177-80.
10. Stone GW, Bertrand M, Colombo A. Acute Catheterization and Urgent Intervention Triage strateg Y (ACUITY) trial: study
design and rationale. Am Heart J. 2004;14(6)8:764-75.
11. TIMI Study Group. TIMI deinitions for commonly used terms in clinical trials [Internet]. Boston; 2010 [cited 2014 Mar 18]. Available from: http://www.timi.org/wp-content/uploads/2010/10/ TIMI-Deinitions.pdf
12. Doyle BJ, Rihal CS, Gastineau DA, Holmes DR Jr. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention:implications for contemporary practice. J Am Coll Cardiol. 2009;53(22):2019-27.
13. Rao SV, Eikelboom JA, Granger CB, Harrington RA, Califf RM, Bassand JP. Bleeding and blood transfusion issues in patients with non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28(10):1193-204.
14. Agostoni P, Biondi-Zoccai GL, De Benedictis M, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures: systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004;44(2):349-56.
15. Spaulding C, Lefevre T, Funck F, Thébault B, Chauveau M, Ben Hamda K, et al. Left radial approach for coronary angiogra-phy: results of a prospective study. Cathet Cardiovasc Diagn. 1996;39(4):365-70.
16. Goldberg SL, Renslo R, Sinow R, French WJ. Learning curve in the use of the radial artery as vascular access in the per-formance of percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn. 1998;44(2):147-52.
17. Rao SV, Ou FS, Wang TY, Roe MT, Brindis R, Rumsfeld JS, et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv. 2008;1(4):379-86.
18. Achenbach S, Ropers D, Kallert L, Turan N, Krähner R, Wolf T, et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008;72(5):629-35.
19. Sciahbasi A, Pristipino C, Ambrosio G, Sperduti I, Scabbia EV, Greco C, et al. Arterial access-site related outcomes of patients undergoing invasive coronary procedures for acute coronary syndromes (from the ComPaRison of Early Invasive and Conservative Treatment in Patients With Non-ST-ElevatiOn Acute Coronary Syndromes PRESTO-ACS] Vascular Substudy). Am J Cardiol. 2009;103(6):796-800.