Department of Plastic and General Surgery Turku University Hospital and University of Turku Turku, Finland.
List of original publications
Abbreviations
Abstract
Tumor resection with microscopically negative margins was achieved in 79% of the 96 patients who underwent surgery with curative intent. Of the patients with sarcoma resections, five (31%) died of sarcoma and another four (25%) developed local recurrence or new distant metastases.
Suomenkielinen tiivistelmä
Rekonstruoidut verisuonet peitettiin viidellä potilaalla latissimus dorsi -mikrovaskulaarisella läpällä ja kolmella paikallisella lihasläpällä. Makroskooppisesti selkeillä marginaaleilla leikattujen kasvaimien histologinen alatyyppi ja aste ovat merkittäviä sairauskuolleisuuden ennustajia.
Introduction
Provided that clear margins are achieved with the resection, the need for vascular reconstruction is not associated with a worse prognosis. (Schwarzbach et al. 2006) However, the operation is demanding and involves significant perioperative morbidity. While they previously faced proximal femoral amputation of hip disarticulation, limb-sparing surgery is now possible for the majority of these patients. (Davis et al. 2017, Fujiki et al. 2020).
Review of the literature
- Soft tissue sarcomas
- Histological classification of soft tissue sarcomas
- Grading of soft tissue sarcomas
- Staging of soft tissue sarcomas
- Diagnosis of soft tissue sarcomas
- Treatment of soft tissue sarcomas
- Surgical treatment
- Vascular reconstructions
- Radiotherapy in the treatment of soft tissue sarcomas
- Chemotherapy in the treatment of soft tissue sarcomas
- Follow-up of soft tissue sarcomas
- Follow-up of oncovascular reconstructions
The presence of the DDIT3 fusion protein has been suggested to inhibit adipocyte differentiation. (Kuroda et al. 1997). The specific translocation type does not seem to predict any aspect of the disease course (Antonescu et al. 2001).

Aims of the study
Patients and methods
- Patients
- Surgery
- Adjuvant treatments
- Systematic review of literature
- Follow-up
- Statistical methods
The patients were identified by reviewing all patients with retroperitoneal sarcoma operated on by members of the oncovascular surgical team during that period. A core needle biopsy was performed to confirm the diagnosis preoperatively in the 40% of patients who considered preoperative adjuvant treatment. Eight patients underwent soft tissue sarcomas resections in which some of the major vessels in the proximal thigh were sacrificed.
Preoperative radiotherapy was given to seven (7%) patients and postoperative radiotherapy to 5 (5%) during the treatment of the primary tumor. Six (75%) of the patients had radiotherapy for the primary or recurrent tumor operated on, three preoperatively and three postoperatively. The location of the first metastases was recorded for each of the patients in the included series.
The follow-up of the vascular grafts was designed for each patient on a case-by-case basis.

Results
Study I
- Histopathology
- treatment results
- Systematic review of literature
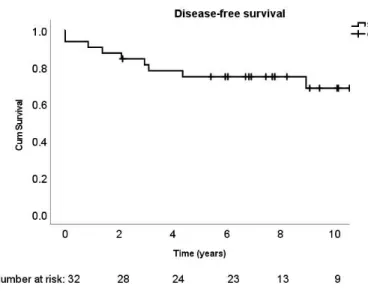
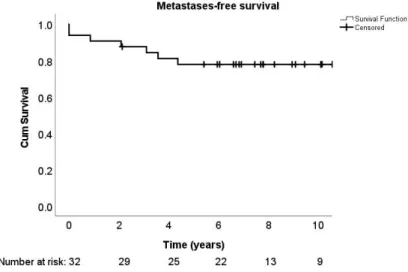
Metastases were detected in seven patients (22%), including two patients (6%) who had primarily metastatic disease. The locations of metastases were: patient 1) lung and chest, which later recurred in the same place, patient 2) first intra-abdominal and supraclavicular lymph nodes, then subcutaneous, then intra-abdominal, lung and spine, patient 3) intra-abdominal, patient 4) first intra-abdominal, then further intra-abdominal and subcutaneous around the scar, patient 5) brain, patient 6) intra-abdominal and contralateral soft tissue of the thigh, patient 7) first intra-abdominal, then bone. Overall, nine patients had local recurrence or metastases during follow-up, with a five-year disease-free survival of 75 ± 8% (Figure 5).
Six patients died of myxoid liposarcoma during follow-up with a 5-year disease-specific survival of 87 ± 6%. Fourteen articles describing unique patient series with at least ten patients with metastatic myxoid liposarcoma were identified for the analysis. The series included a total of 1853 patients with myxoid liposarcoma who had metastatic disease (Table 10).
Of note, for twelve of the series, lung and pleural metastases were reported together, or the potential inclusion of pleural metastases in the lung metastasis counts was not revealed.
Study II
- Histopathological diagnosis
- Perioperative complications
- Treatment results
Complications were: pneumonia, pulmonary embolism, pneumothorax, one abdomen left open for subsequent closure due to challenging hemostasis after heparinization due to aortic stricture, one wound dehiscence, one patient requiring relaparotomy for postoperative bleeding, and two stomas. patients experiencing leg weakness due to spinal cord ischemia and nerve damage. Five-year local recurrence-free survival was 37 ± 5% in 96 patients who had a complete macroscopic resection of a primary liposarcoma. Treatment for a local recurrence was considered successful in 53 (77%) patients of whom 45 (85%) developed one or more further recurrences during follow-up.
Histological tumor grade increased during one or more recurrences in 17 (25%) patients. Local recurrence-free survival by tumor type in 96 patients with retroperitoneal liposarcoma resected with curative intent. Local recurrence-free survival according to tumor stage in 96 patients with retroperitoneal liposarcoma whose tumor was resected with curative intent.
Local recurrence-free survival due to tumor multifocality in 96 patients with retroperitoneal liposarcoma whose tumor was curatively removed.

Study III
- Histopathology
- Perioperative complications
- Vascular complications on follow-up
- treatment results
- Systematic review of literature
- IVC reconstructions
- Aortic reconstructions
- Renal vein reconstructions
- Iliac artery and vein reconstructions
- Other reconstructions
Embolectomy and stenting were performed and the graft remained open for the remainder of follow-up. Three of the patients had no imaging studies to assess graft patency at follow-up. Surgical outcomes, vascular complications at follow-up and oncological outcomes for retroperitoneal sarcoma resections and vascular reconstructions.
In three patients, metastases were present at the time of surgery and in four other patients metastases developed during follow-up. One of the patients who died with recurrent disease also had metastases at the time of surgery and one developed metastases during follow-up. Furthermore, the absence of imaging data during follow-up may have led to under-reporting of asymptomatic occlusions.
A 15-month follow-up was reported for this patient, but no details of venous patency or oncological outcome were specified. (Gage et al. 2012) In particular.

Study IV
- Histopathology
- Perioperative complications
- Patency of vascular grafts on follow-up
- Functional outcomes
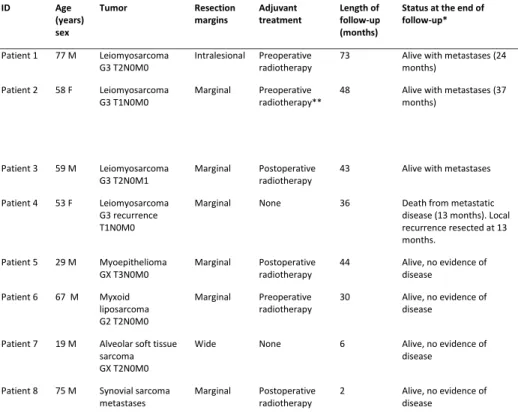
Patient demographics, details of treatment and follow-up of lower limb soft tissue sarcoma patients treated with vascular and soft tissue reconstructions by the Helsinki University Sarcoma Team from 2014 to 2020. Assessment of femoral or iliac graft patency by duplex ultrasonography was available for seven of eight patients, with a follow-up of months (Table 20). Patient 3's arterialized autologous vein graft had obstruction at 19 months, and a new arterial bypass graft was performed after failed angioplasty.
The new graft was found to be obstructed with sufficient collateral circulation to maintain leg vitality at 23 months. With the above interventions, the twelve-month patency rate achieved for arterial grafts was 100% and the 24-month patency rate 83 ± 15%. Three of the patients had edema with more than 10% increase in volume compared to the nonoperated leg, one with all appropriate use of compression garments.
Graft patency and functional outcomes for patients with soft tissue sarcoma who underwent tumor removal and vascular reconstruction *Volume difference compared to non-operated side.
Discussion
Metastatic pattern of myxoid liposarcomas and its implications for
Incomplete surgical resection, on the other hand, does not confer better disease-free survival than chemotherapy. (Nevala et al. 2019, Nakamura et al. 2021). The presence of a single pulmonary metastatic lesion is associated with improved survival. (Chudgar et al. 2017, Nakamura et al. 2021). The literature review identified two centers that routinely use whole-body MRI in the standard follow-up of patients with MLS. (Gouin et al. 2019, Visgauss et al. 2021) Most centers, including ours, have used MRI only to image the primary tumor site for local recurrence.
Similar findings have previously been reported in a series involving a series of retroperitoneal soft tissue sarcomas. (Hassan et al. 2004) These findings support a surgical approach aimed at absolute complete removal of the tumor if the location of the tumor does not allow the inclusion of marginal margins without damage to adjacent structures. This is consistent with previous reports identifying grade as a predictor of survival in retroperitoneal soft tissue sarcomas (Lewis et al. 1998, Chouliaras et al. 2019). Also in other institutes, a trend of more frequent metastasis of higher-grade retroperitoneal liposarcomas was observed (Chouliaras et al. 2019).
Histological subtype was a third factor predicting disease-specific survival in our population, a finding also observed in larger series of retroperitoneal soft tissue sarcomas (Singer et al. 2003, Hassan et al. 2004) (Tan et al. 2016 ).
Safety of oncovascular surgery in the treatment of soft tissue sarcomas
In the 110 patients with retroperitoneal vascular reconstructions included in the present review, graft patency at follow-up was reported to be 90%. Accordingly, three of the ten homografts in the review population closed during follow-up. The patency of the vascular grafts was evaluated in seven of our patients with superficial femoral vessel reconstruction.
The occlusion rate was higher for the vein grafts, with only two of the grafts patent after two years. In arterial bypass grafts for arteriosclerosis, graft patency is dependent on the distal vasculature, not graft properties (Albäck et al. 1998). The physician-assessed median MSTS score of 70% reflected a mild deterioration in limb strength and mobility.
Of the eight patients with femoral tumors, resection with wide or marginal margins was achieved in seven.
Conclusions
Acknowledgements
Lecturer Tiina Jahkola and lecturer Susanna Kauhanen, who supported me throughout the training and who were extremely helpful in expanding my research and teaching skills. Arguably, this dissertation might have been completed more quickly without the unrelated research projects, but a lot of fun would have been missed. My colleagues at the Department of plastic surgery, who with their passion for their work remind me again and again how big our specialty is.
My parents Tuulikki and Kari, and my siblings Anniina and Valtteri, who supported me through my various career decisions and reminded me that there is a lot of life outside of medicine. My husband Olivier: In the acknowledgments of my Cambridge PhD dissertation, I thanked him for treating me like a princess.
34;Concurrent arterial and venous reconstruction with resection of lower extremity sarcomas." Annals of Vascular Surgery. 34;Heparin-bound Dacron or polytetrafluoroethylene for femoropopliteal bypass grafting: A multicenter trial." Journal of Vascular Surgery. 34; Arterial reconstruction for en bloc resection of soft tissue sarcoma: a single tertiary center experience.” Annals of Vascular Surgery.
34;Radical resection of inferior vena cava tumors with vascular reconstruction and renal autotransplantation." Surgery. 34;Liver resection for metastatic soft tissue sarcoma: An analysis of prognostic factors." European Journal of Surgical Oncology (EJSO. 34; Surgical results of vascular reconstruction in soft tissue sarcomas of the lower extremities." Journal of Vascular Surgery.
34;Resection of retroperitoneal tumors with inferior vena cava involvement without caval reconstruction."Journal of Surgical Oncology. 34;Long-term results of a prospective randomized trial of adjuvant brachytherapy in soft tissue sarcoma." Journal of Clinical Oncology. 34; Primary leiomyosarcoma of the inferior vena cava: reports of infrarenal and suprahepatic caval involvement. "Journal of Vascular Surgery.