Presented with the permission of the Faculty of Health Sciences, University of Eastern Finland for public examination in Auditorium 1, Kuopio University Hospital, Kuopio on 14 April 2023, at 12 noon. However, there is still a lack of clinical evidence of the validity and impact of VR environments in TB operative and anatomy training.
ACKNOWLEDGEMENTS
My beautiful wife Marika, thank you for enduring the moments this project stole from us. This study was funded by the Kuopio University Hospital Research Foundation, State Research Funding of the Kuopio University Hospital (VTR), the Finnish ORL-HNS Foundation, the North Savo Regional Fund, The Finnish Cultural Foundation, The Finnish Society of Ear Surgery, and.
LIST OF ORIGINAL PUBLICATIONS
CONTENTS
1 INTRODUCTION
In recent years, advances in virtual reality (VR) technologies have yielded several promising results with reduced costs. In recent years, training with VR simulators has been shown to be effective in training mastoidectomy techniques for novices (Andersen et al., 2016), and recently it has been demonstrated that a patient-specific.
2 REVIEW OF THE LITERATURE
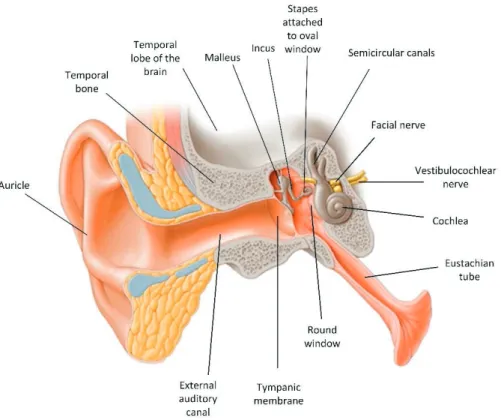
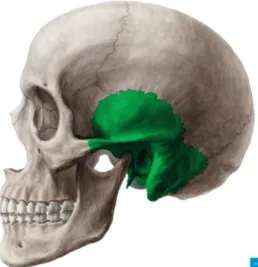
TEMPORAL BONE .1 Anatomy
- Temporal bone surgery
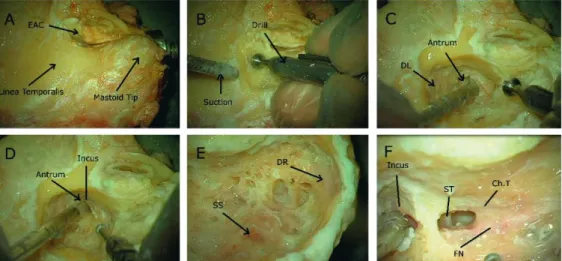
The upper part of the bone forms the tegmen tympani i.e. the roof of the middle ear and the lower part contribute to the external part of the skull base; it has an attachment for the levator veli palatini muscle. Cortex and the superficial landmarks of the bone exposed, B. Dissection by drilling begins according to superficial landmarks, C. The dissection is extended to the mastoid point, F. tympanotomy between the facial nerve and chorda tympani.
SURGERY PLANNING IN TEMPORAL BONE .1 Preoperative planning
- Preoperative imaging
- Imaging techniques
- The challenges in temporal bone anatomy evaluation and planning
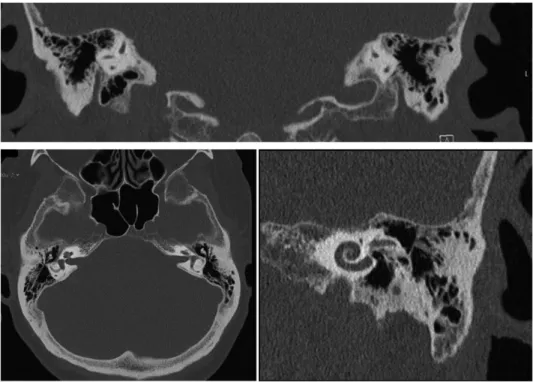
Usually, due to its better resolution and higher image quality, HRCT is still the main modality used for diagnosis and preoperative planning in procedures involving tuberculosis (Thukral et al., 2015). Mastoid pneumatization and volume, which affect the ease of drilling during surgery, can be assessed by imaging (Dexian Tan et al., 2018).
TEMPORAL BONE ANATOMY EDUCATION AND SURGERY TRAINING
- Challenges of traditional training
- Assessment of surgical performance and training
In otology, several performance assessment tools have been introduced specifically for mastoidectomy (Sethia et al., 2017). Welling's scale was used in many studies that proved its validity (Andersen et al.
VR ASSISTED TEMPORAL BONE SURGERY AND TRAINING
- Introduction to VR
- History of VR
- VR in medical use
- VR in temporal bone surgical training
- Patient-specific surgical planning and training in VR
- VR in radiological image interpretation
- Temporal bone anatomy education in VR
- Limitations and challenges of VR in temporal bone
- Adverse effects of VR
Studies from other surgical fields (e.g., neurosurgery, interventional radiology, laparoscopic surgery) support this conclusion (Cates et al., 2016). The use of head-mounted displays has been associated with nausea, oculomotor disturbances, disorientation, and headache (Weech et al.). al., 2019).
3 AIMS OF THE STUDY
4 SUBJECTS AND METHODS
- MATERIALS
- Study I
- Study II
- Study III
- METHODS (I-II)
- Image data viewing methods
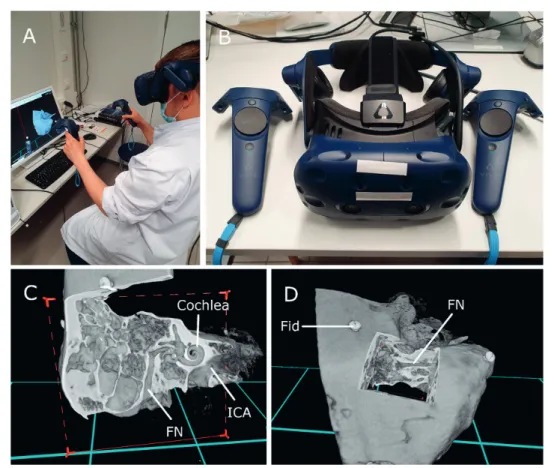
- Tasks performed in VR and cross-sectional viewing A 15-minute standardized instructional session was held for each
- Questionnaires
- METHODS (III)
- Feasibility assessment of VR training
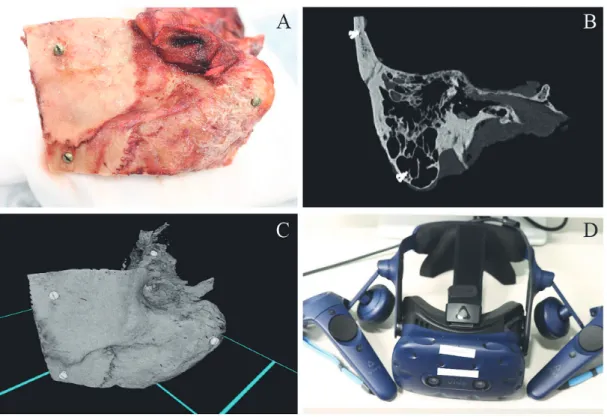
- Image data collection
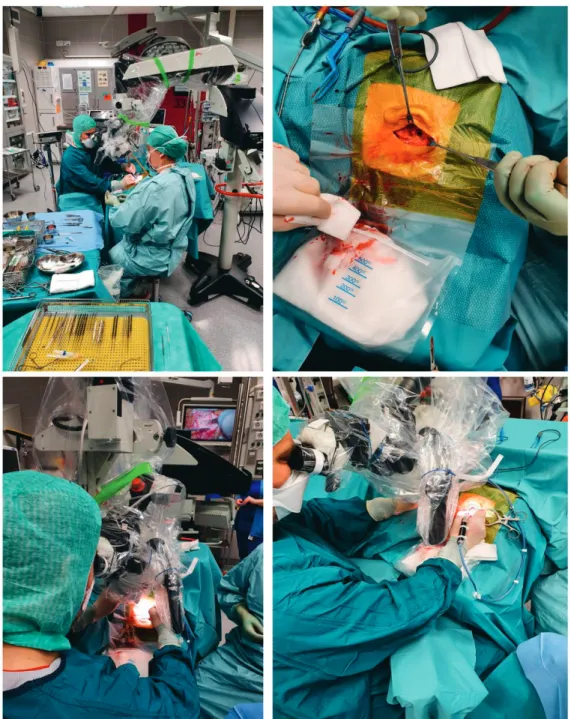
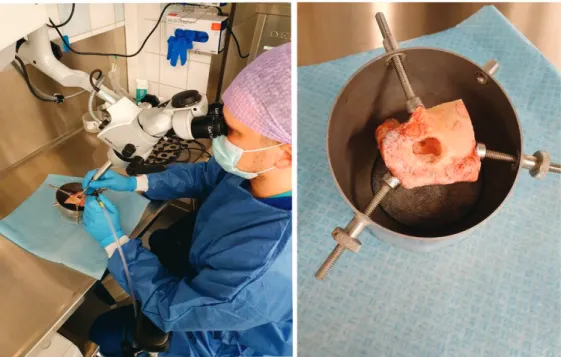
- The dissection course
- VR training
- Dissection training
- Questionnaires and user-experience
- STATISTICAL METHODS
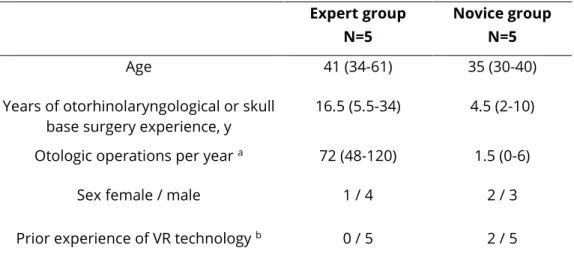
Two of the novice participants had once performed a tuberculosis cadaver dissection prior to the study. Siemens SOMATOM Definition Flash (Siemens Healthcare, Forchheim, Germany) was used to acquire HRCT images of tuberculosis. HRCT images of the TB cadaver used during the course were acquired with a 16-slice CT scanner (BrigthSpeed, GE Healthcare, Chicago, Illinois, USA).
The time required by each participant for dissection of anatomical landmarks on both days of the course was defined as surgical time. On the first day of the course, the time used to expose the incus corpus was collected. The intraclass correlation coefficient (ICC) was used as a measure of correlation between distances measured by different methods.
This test was used in the evaluation of Likert-type questionnaires and in the analysis of the performance results.
5 RESULTS
STUDY I
Statistics evaluating screw fiducial distance measurements obtained either with conventional cross-sectional view (PACS) or those performed in the VR environment. SD=standard deviation, CI=confidence interval, ICC=intraclass correlation coefficient (p<0.001), PACS=conventional cross-sectional method (2D), VR=virtual reality environment, DPM=direct physical measurements with Vernier calipers . Statistics in the evaluation of anatomical distance measurements obtained either with the conventional cross-sectional view (PACS) or with those performed in the VR environment.

STUDY II
STUDY III
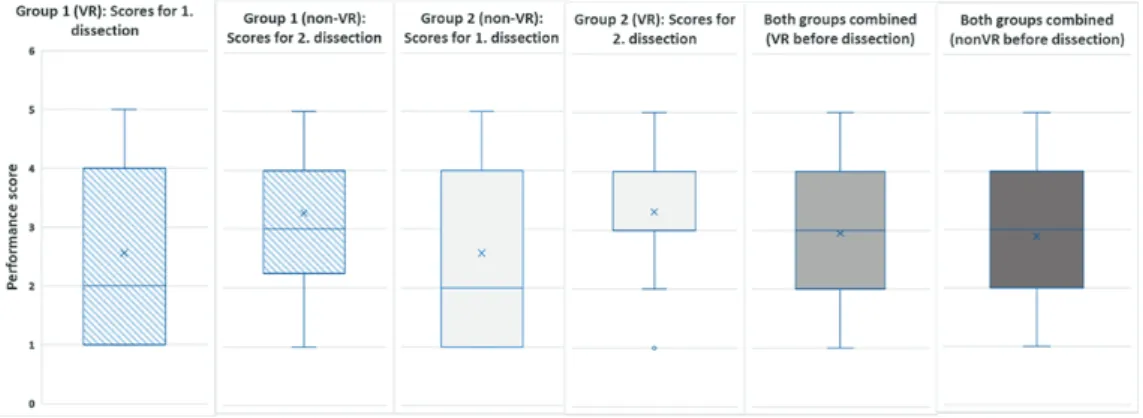
- Objective feasibility
- Subjective feasibility
Analysis of the time spent on landmark dissection showed that the average surgical time to expose each landmark was reduced by Analysis of the free-text responses revealed that participants wanted more time for the VR demonstration, for VR training, and more individual instruction for the anatomical landmark identification task. Their lack of knowledge of tuberculosis anatomy was considered a possible limitation for more effective use of VR.
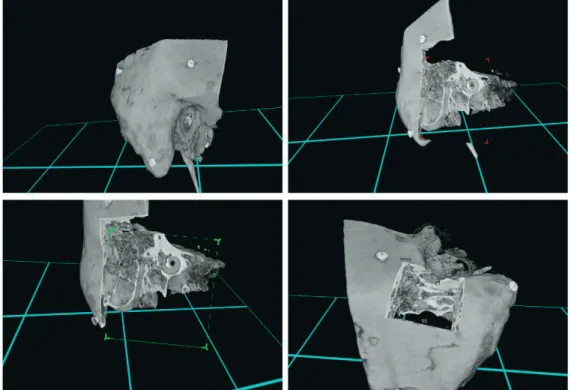
None of the participants reported nausea or other adverse effects during or after VR use. It was generally appreciated that VR helped the participants to better understand the topographical anatomy in 3D and the spatial relationship and distance of anatomical landmarks. More importantly, one possibility that was positively highlighted was that the participants could try different approaches and have the opportunity to repeatedly cut the tubercle at any angle, which is not available with the physical model.
Participants generally agreed that VR training was a novel and feasible method for anatomy teaching, operative training, and planning surgery, ultimately leading to a higher level of understanding of the 3D topography of complex anatomy.
6 DISCUSSION
- THE FEASIBILITY AND ACCURACY OF SIMULATED VR PLANNING
- THE IMPACT OF VR ON EVALUATION PERFORMANCE OF TEMPORAL BONE ANATOMY
- THE IMPLEMENTATION OF VR IN TEMPORAL BONE SURGERY TRAINING
- SUBJECTIVE VALIDITY AND USER-EXPERIENCE OF VR
- STRENGTHS AND LIMITATIONS
- Study I-III
- Study I
- Study II
- Study III
- FUTURE ASPECTS
There are only a few publications that have evaluated the benefits and impact of VR technology on how well residents and experienced otologic surgeons acquire knowledge of TB anatomy (Morone et al., 2019; Sethia and Wiet, 2015). This shows that viewing the image in VR can convey additional information, which leads to a faster understanding of the complex anatomy of TB. Thus, the VR model appears to provide a better basis for understanding the complex anatomy of TB.
Nowadays in the clinic before any surgical intervention is made in the TB, preoperative radiological imaging of the patient's TB region. Rather, VR training has been adopted and applied by experienced otologic surgeons as part of the training provided to residents. These limitations were attributable to the limited time of the dissection course and the access to the facilities.
It is also important to continue to objectively investigate the usefulness and effects of VR for learning the anatomy of tuberculosis in medical students and novice otological surgeons.
7 CONCLUSIONS
Virtual reality in neurosurgery: "Can you see it?" - An overview of the current applications and future potential. Anatomy-specific virtual reality simulation in temporal bone dissection: perceived utility and impact on surgeon confidence. Objective assessment of learning curves for the Voxel-Man TempoSurg temporal bone surgery computer simulator.
Patient-specific virtual and mixed reality for immersive experiential anatomy education and for surgical planning in temporal bone surgery. The impact of competitive learning in multi-person virtual reality on anatomy education: a randomized controlled trial. Improving temporal bone dissection using self-guided virtual reality simulation: results of a randomized blinded control trial.
Could the Virtual Reality Simulator be used as a training aid to improve temporal bone cadaver dissection?
APPENDICES
- Did you experience nausea/vertigo/headache or any other similar problems during the use of VR application?
- What kind of problems did you experineced in VR surgical planning? And in PACS method?
- What would be an adequate time for orientation of the VR equipment?
- What kind of benefits you consider the VR environment has compared to PACS method in surgical planning and in the
- In what other applications VR environment could be applied (e.g
Vertical diameter of bony ear canal (internal meatus) Estimation of tympanic membrane diameter, universal anatomical measurement. Distance from sigmoid sinus to posterior wall of bony ear canal The space available for drilling in e.g. What kind of advantages do you think the VR environment has in comparison to PACS method in surgical planning and in comparison to PACS method in surgical planning and in understanding topographical anatomy of objects.
Appearance of tools Usability of tools Tool performance Haptic feedback Ergonomics Depth perception Quality of graphics Learning anatomy. In your opinion, what are the benefits of the VR environment compared to traditional cross-sectional view in surgical planning and training in understanding the topographical anatomy of objects? Self-assessment of your understanding of temporal bone anatomy in general (scale 1-5) Score 1 represents very poor and 5 represents excellent.
Self-assessment of your understanding of temporal bone anatomy radiologically (scale 1-5) Scores of 1 represent very poor and 5 represent excellent.
ORIGINAL PUBLICATIONS (I – III)
Virtual reality improves the accuracy of preoperative simulated planning in temporal bones: a feasibility and validation study. Virtual reality improves the accuracy of preoperative simulated planning in temporal bones: a feasibility and validation study.
Virtual reality improves the accuracy of simulated preoperative planning in temporal bones: a feasibility and validation study
DPM was later compared with distance measurements performed in a VR and PACS interface. An experienced neuroradiologist and two experienced surgeons assessed the quality of the HRCT images in both a conventional cross-sectional view (PACS) PACS interface and a VR (VR) environment. Transverse HRCT image visualization was performed in a PACS interface (Sectra AB, Linkoping, Sweden).
Of the 26 errors made in cross-gaze, 14 (54%) were mostly due to misidentification of fiducial measurement points (measured distance matched to a distance between other, non-target, fiducial pairs) . View of anatomical structures, depth perception, understanding of anatomical structures (e.g. rotation of the cochlea within the maze), hand-eye coordination (e.g. how easy it is to grasp, move and follow objects) and outcome general understanding of the surgical site (eg, at which angle to approach the round window or the risk of facial nerve injury in the posterior tympanum) in VR were significantly preferred over PACS. Subjects typically reported that accurate identification of fiducials and associated measurements was difficult in cross-gaze.
Therefore, it is also important to investigate the usefulness of a VR environment for learning the anatomy of tuberculosis in medical students and novice otological surgeons.
The effect of virtual reality on temporal bone anatomy evaluation and performance
1 a Setup of the VR interface while performing the task, (b) Head-mounted display and a pair of controllers, (c) and (d) View of a temporal bone in the VR environment. Furthermore, this study revealed a significantly longer learning curve of novice participants with cross-sectional views of complex anatomical structures compared to that in VR. Finally, the user experience of VR surgical training was assessed using a 5-point Likert scale questionnaire.
The feasibility assessment of the pre-dissection VR training had a comparable effect on surgical performance scores with lower mean operative times. In addition, two participants highlighted the somewhat limited quality of the graphics and images in VR. A meta-analysis of the pedagogical effectiveness of three-dimensional visualization technologies in teaching anatomy.Am.
A detailed three-dimensional (3D) understanding of the complex human temporal bone is necessary to adequately learn, plan, and perform surgical procedures.
TOMI TIMONEN