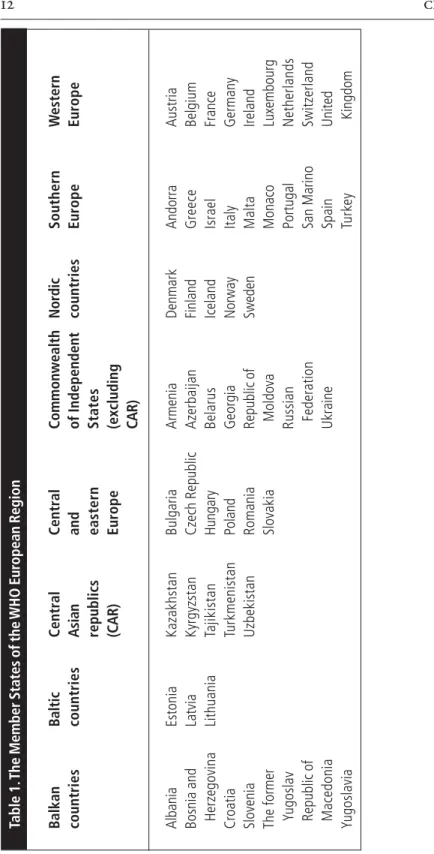
The World Health Organization Regional Office for Europe welcomes requests for permission to reproduce or translate all or part of its publications. These guidelines have been created to facilitate this and to strengthen the role of the health sector.
Acknowledgements
Recommendations
All infants should be exclusively breastfed from birth to about 6 months of age, and for at least the first 4 months of life. Timely introduction of appropriate complementary foods promotes good health, nutritional status and growth of infants and young children during a period of rapid growth and should be a high public health priority.
Introduction
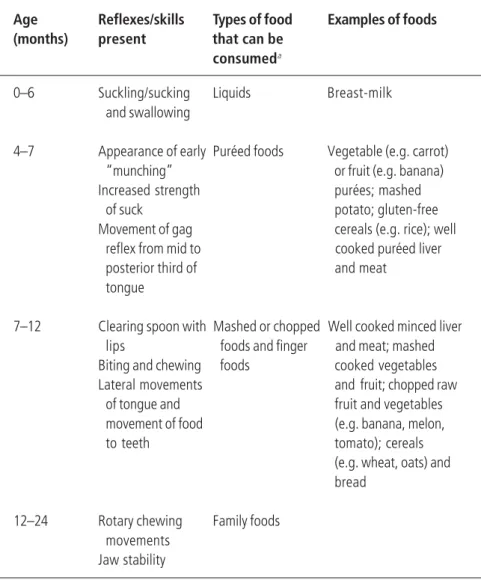
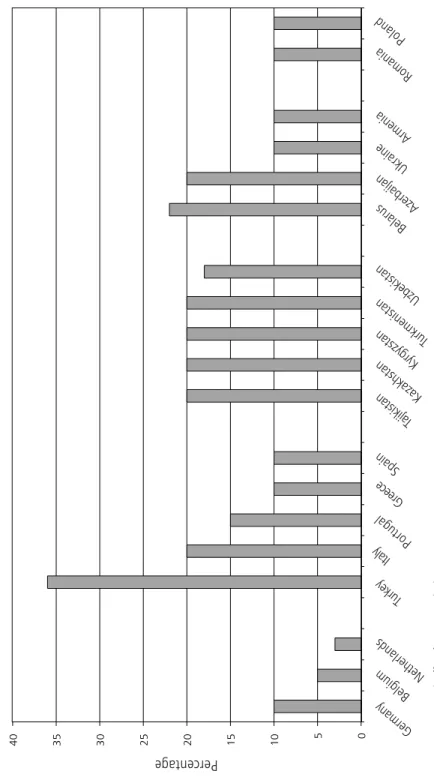
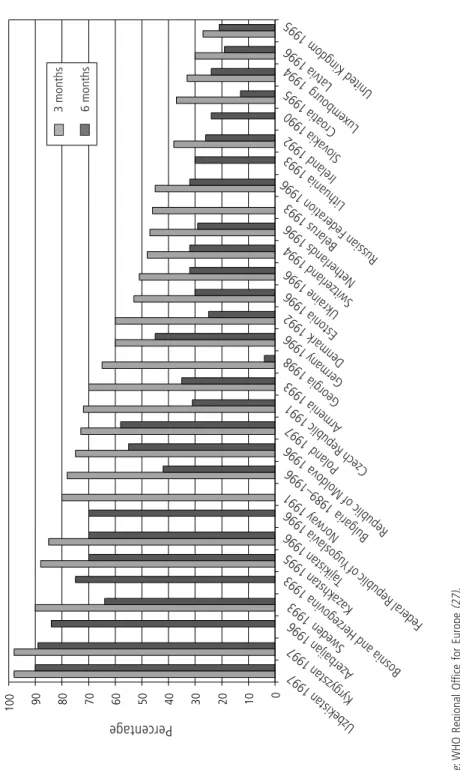
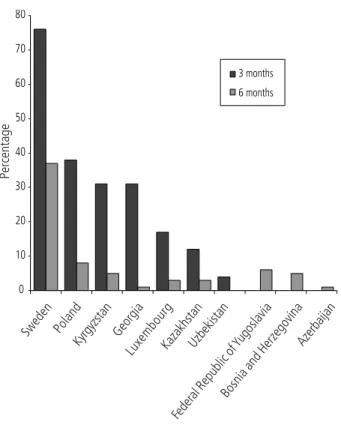
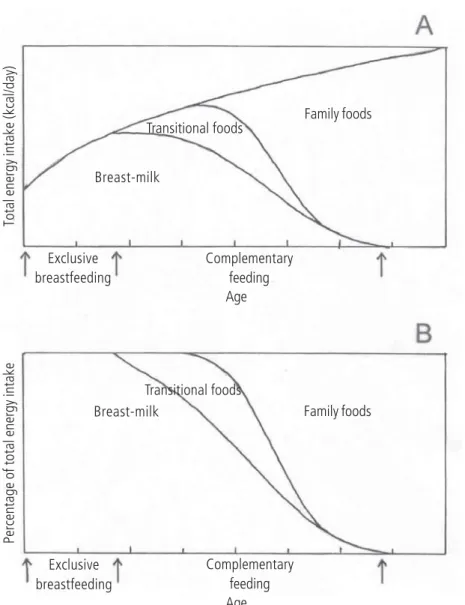
These recommendations provide a standard against which the adequacy of the diet for a population of infants and young children can be assessed. The introduction of complementary foods in relation to the child's age is shown in fig.
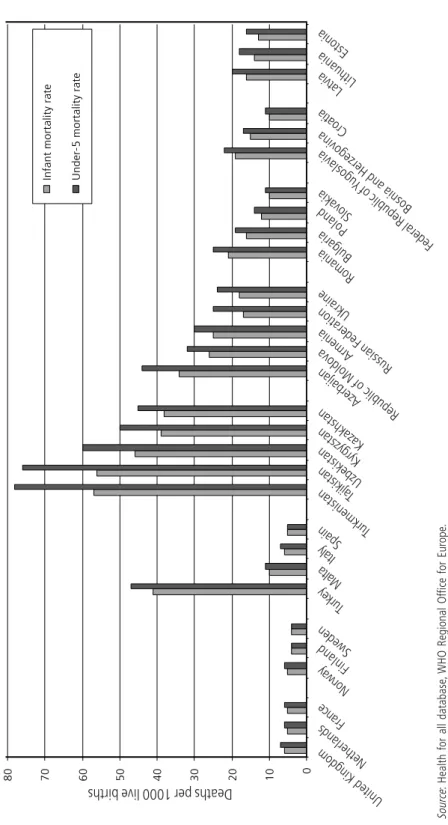
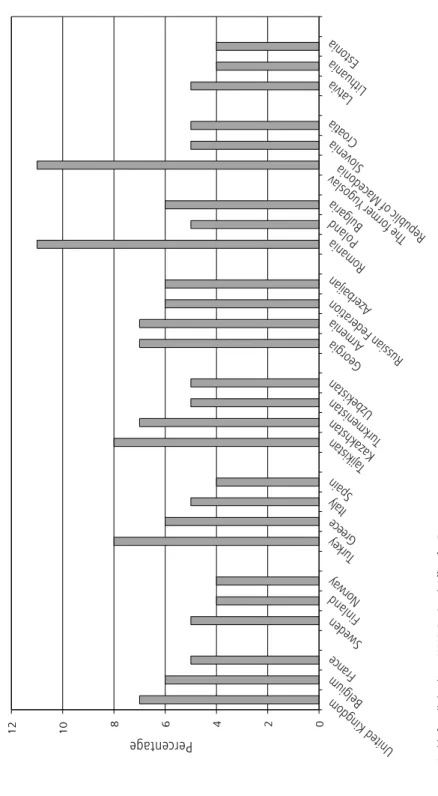
Health and nutritional status and feeding practices
A comprehensive review of the situation in the WHO European Region was carried out in. In the Former Yugoslav Republic of Macedonia, only 8% of children are exclusively breastfed at 4 months of age.
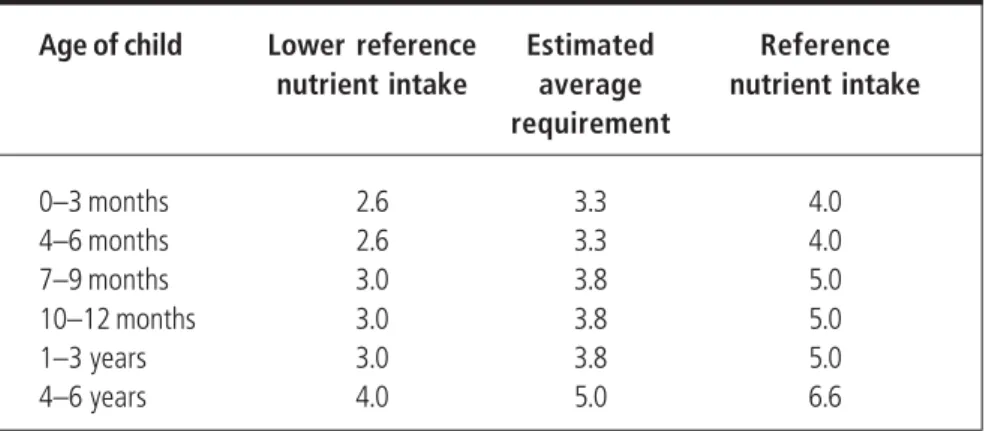
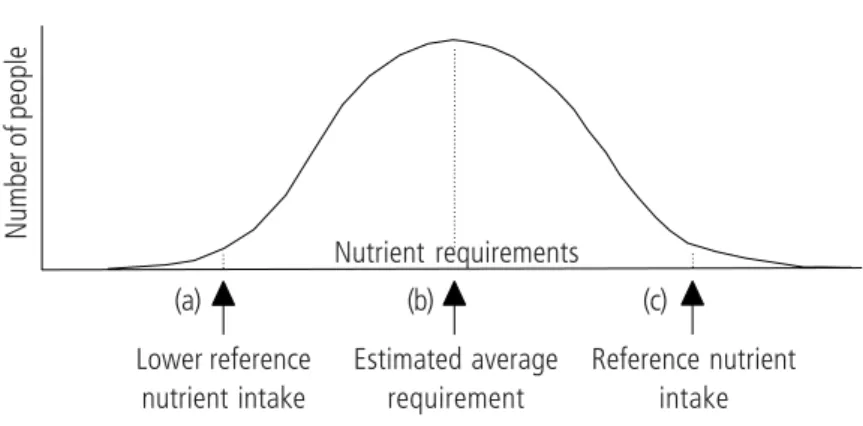
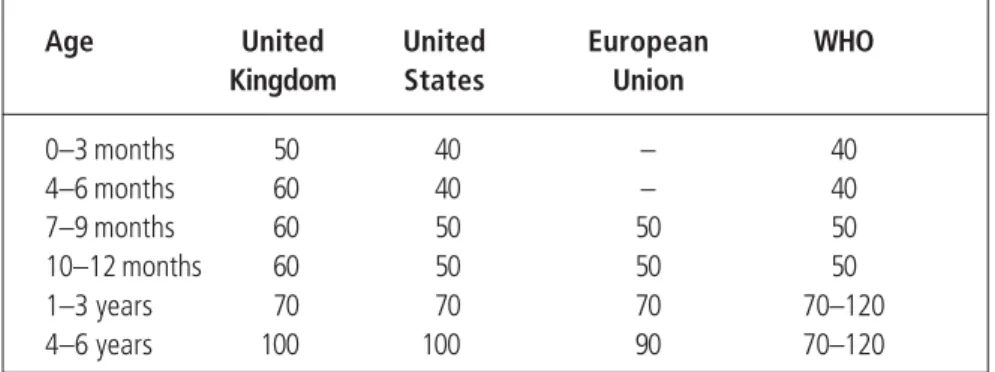
Recommended nutrient intakes
The value at the bottom of the distribution curve is estimated by calculating the mean minus two standard deviations. Report of the Panel on Dietary Reference Values of the Committee on Medical Aspects of Food Policy.
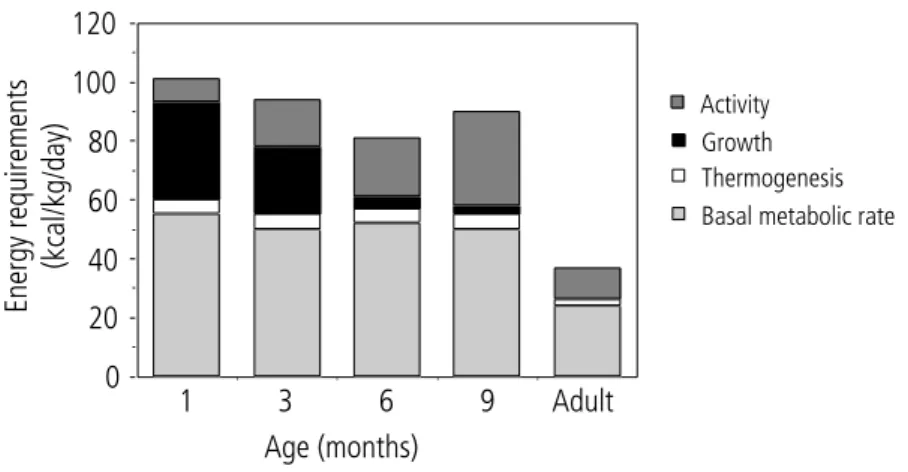
Energy and macronutrients
Fat makes up approximately 50% of the energy in breast milk and is the most important source of energy for infants under 6 months of age. Energy requirements change with physical activity and under stressful environmental conditions, such as temperature extremes and during illness, but precise estimates of the magnitude of these variations are not available for infants and young children. The required energy from complementary foods depends on the energy from the mother's milk and the individual infant's energy needs.
If the energy intake is less than the individual's energy needs, physical activity and/or growth rate will be reduced. Adding fat or sugar increases the energy density without increasing the viscosity of the food (Fig. 13). The amount of fat that can be added to a diet without reducing micronutrient intake to a level below the recommended intake depends on the total micronutrient content of the diet.
Not all of the protein in human milk is "nutritive," as some functional proteins such as secretory IgA can be found in feces. Fat can make a significant contribution to the energy density of the mixed diet and, because it does not normally increase the viscosity of the feed, it can be used to increase the energy density without resulting in an excessively thick preparation. Bacterial fermentation products of dietary fiber can also directly affect bowel habit.
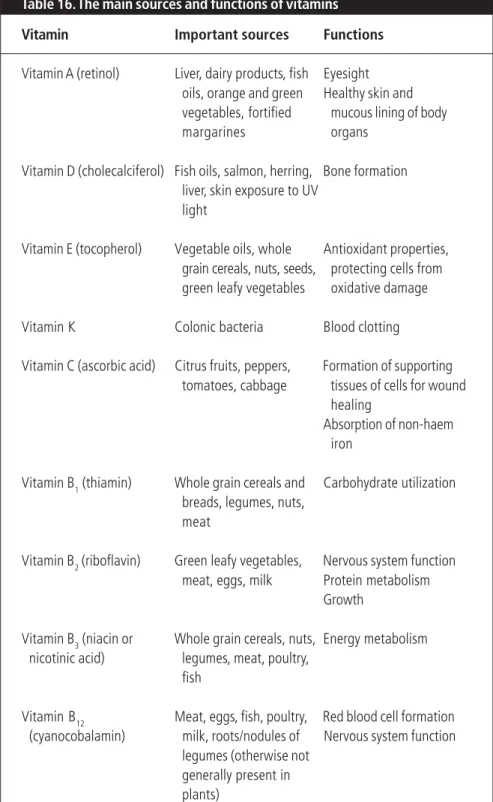
Vitamins
Babies are born with vitamin A stores in the liver and this, together with intakes of vitamin A from breast milk, will meet the requirements until about 6 months of age. If the vitamin A status of the mother is sufficient, breast milk is also an important source of vitamin A after the age of 6 months. For children in populations with a high prevalence of vitamin A deficiency, complementary foods are an important source of vitamin A after 6 months of age.
Infants and young children are vulnerable to the adverse effects of both vitamin A deficiency and excess. In the WHO European Region, clinically apparent vitamin A deficiency does not appear to be a problem, although data on the prevalence of deficiency of vitamin A in the region are limited. In populations with a high prevalence of vitamin A deficiency, high priority should be given to its reduction because of its association with morbidity.
The toxicity of vitamin C is low and there is no health risk at a high intake. The clinical manifestations of rickets vary with age and with the duration of vitamin D deficiency. High intakes of vitamin D can be toxic at any age, and infants are particularly vulnerable.
Appendix
Minerals other than iron
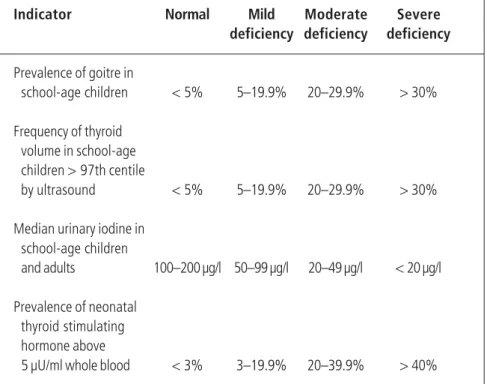
Iodine deficiency is the world's largest cause of preventable brain damage and mental retardation (3). In populations where iodine deficiency disorders are widespread and severe enough to cause hypothyroxinemia during pregnancy, the physiological transfer of thyroid hormones from mother to fetus is reduced. In addition, iodine deficiency that occurs during late pregnancy and persists during lactation leads to low iodine content in breast milk and possible perinatally acquired hypothyroidism in the breastfed child.
In regions with endemic iodine deficiency disorders, prevention of both brain damage and hypothyroidism in the breastfed infant requires iodine. The solution to iodine deficiency has focused on two main strategies, iodine supplementation and iodine fortification. As an interim measure until an effective universal iodized salt system is fully operational, iodine supplementation may be considered in endemic regions to immediately prevent the adverse effects of iodine deficiency on the central nervous system.
Where mild to moderate iodine deficiency disorders exist, pregnant and lactating women should be given iodine supplements until their iodine intake reaches 200–300 µg/day. Elimination of iodine deficiency disorders (IDD) in Central and Eastern Europe, the Commonwealth of Independent States and the Baltic states. The use of iodized oil and other alternatives for the elimination of iodine deficiency disorders.
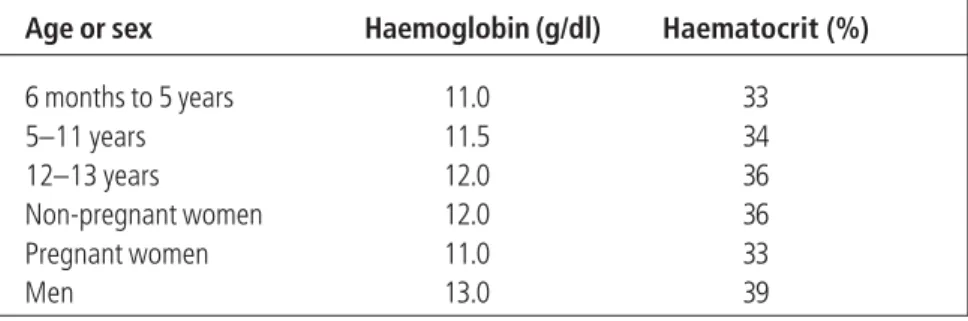
Control of iron deficiency
Prevention of iron deficiency in infants and young children is possible with the relatively simple nutritional strategies described below. Thus, the use of serum ferritin levels may lead to an underestimation of the prevalence of iron deficiency in populations where infection is common. However, if not, iron deficiency should not be ruled out due to the possibility of poor compliance or inconsistent iron intake and absorption.
Hookworm infection is a common cause of iron deficiency anemia in many countries and can be prevented through preventive measures and treatment (see page 121). This difference is due to the low bioavailability of iron and the small percentage of iron normally absorbed: usually only 5%–15% of dietary iron. However, in populations with a high prevalence of iron deficiency anemia, monitoring and treatment programs should be established.
VERSTER, A., ED.Guidelines for the management of iron deficiency in countries of the Eastern Mediterranean, Middle East and North Africa. Iron requirement and prevalence of iron deficiency in term infants during the first six months of life. Prevention of iron deficiency anemia: comparison of high and low iron formulas in term healthy infants at six months of life.
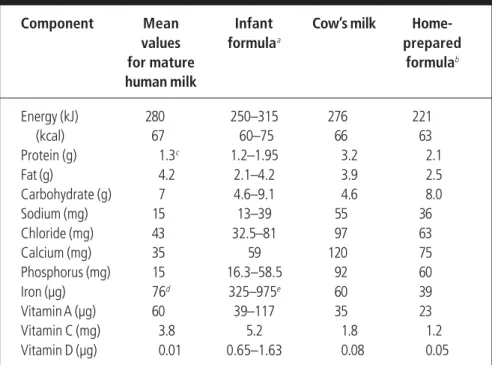
Breastfeeding and alternatives
The vitamin D status of the newborn depends on the vitamin D status of the mother during pregnancy and lactation. Iron concentrations in human milk are not related to maternal iron status and are relatively unaffected by maternal dietary iron content. Human milk also contains many other protective and trophic factors that may play a role in the protection and maturation of the digestive tract.
Most of the protective effects of breastfeeding against infectious diseases are passive, that is, the immunoprotective factors in breast milk protect the mucosal surfaces of the digestive and respiratory tracts and thus reduce the risk of infection. To ensure an optimal quality and quantity of breast milk without harming the health of the mother, it is therefore important to optimize the mother's nutritional status during pregnancy and lactation. On the contrary, for the first year of life, breast milk should still be a main source of food, and should preferably provide between one third and one half of the average total energy intake by the end of the first year.
The effect of the Initiative on the duration of breastfeeding and the incidence of infection has been investigated in a large-scale study in Belarus (M.S. Kramer, personal communication, 1999). The cup rests lightly on the infant's lower lip, and the edges of the cup touch the outermost part of the infant's upper lip. If used, teats should not be dipped in sweet foods such as jam and honey because of the risk of tooth decay (see Chapter 11).
Handbook of Resolutions and Decisions of the World Health Assembly and the Executive Board, Vol. Hepatitis C virus RNA present in saliva but absent in the breast milk of the mother who is a hepatitis C carrier.
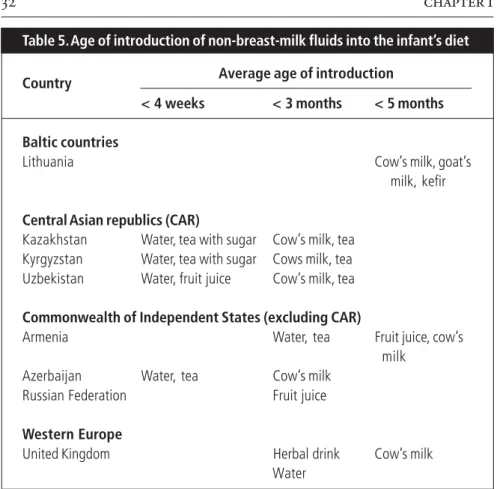
Complementary feeding
Children are physically able to consume family foods by 1 year of age, after which they no longer need to be modified to meet the child's special needs. As the baby grows and becomes more active, breast milk alone is not enough to meet the baby's full nutritional and psychological needs. Likewise, "4 months" refers to the end, not the beginning, of the fourth month of life.
In Chapter 3, estimates of the average amounts of energy required from complementary foods at different ages were defined. The physical properties of the starch are discussed in relation to the thickness of the complementary staple food. Based on this, possible modifications to the preparation of the basic lump are suggested, which should help to produce a food that is neither too thick for the infant to consume nor so thin that the energy and nutrient density is reduced.
Once the baby has accepted spoon feeding, new tastes and textures can be added to increase the variety of the diet and help develop motor skills (Table 42). Similarly, when introducing lumpier foods, a baby's known favorite food should be mixed with a new coarser-textured food (such as carrots with small, noticeable lumps). In the last months of the complementary feeding period, feeding the baby should be combined with self-feeding.