Original Article
REVISTA PAULISTA DE MEDICIN A
De te ction of human papillomavirus in
e pithe lial le sions of the conjunctiva
O ftalmology Service, Hospital A.C. Camargo, Fundação Antônio Prudente and
Instituto Ludwig de Pesquisa sobre o Câncer, São Paulo, Brazil
a b s t r a c t
CON TEX T: Many facto rs like expo sure to UV radiatio n, climatic co n-ditio ns, g enetic predispo sitio n, immuno lo g ical state and, mo re re-cently, the presence o f HPV have been implicated in the g enesis o f so me lesio ns o f the co njunctiva, especially the carcino ma.
OBJECTIVE: To evaluate the presence o f HPV DN A in acquired le-sio ns o f the co njunctiva and in no rmal muco sa.
TYPE OF STUDY: Cro ss-sectio nal study.
SETTIN G: A public university referral center (the O phthalmo lo g y Ser-vice o f the A.C. Camarg o Ho spital - A. Prudente Fo undatio n, São Paulo ).
PARTICIPAN TS: Thirty patients with acquired lesio ns o f the co njunc-tiva and 6 0 matched co ntro ls (by ag e and sex) were evaluated in this study, fro m June 1 9 9 3 to March 1 9 9 5 .
PROCEDURES: The detectio n o f HPV DN A in the no rmal co njunctiva and in acquired lesio ns was do ne by the PCR technique and do t blo t hybridiz atio n. The material was co llected by scraping the no rmal muco sa and the surface o f the lesio ns. A frag ment o f fresh fro z en tissue and paraffin embedded specimens o f each lesio n were also included.
M AIN M EASUREM EN TS: The asso ciatio n between the HPV infec-tio n and the presence o r absence o f co njunctival lesio ns.
RESULTS: Sequences o f HPV DN A were detected in 4 o f the 3 1 lesio ns evaluated (1 2 .9 %) and in the healthy muco sa o f o ne indi-vidual o f the co ntro l g ro up (1 .6 %). HPV type 1 6 was detected in 2 carcino mas and in the no rmal muco sa o f o ne individual o f the co n-tro l g ro up. HPV type 1 1 was demo nstrated in 2 papillo mas o f o ne patient with lesio ns in bo th eyes.
CON CLUSION S: The lo w frequency o f HPV DN A fo und in the le-sio ns o f this sample and the detectio n o f the viral g eno me in the no rmal muco sa indicate that there is a weak po ssibility o f asso cia-tio n between HPV infeccia-tio n and the carcino ma o f the co njunctiva.
KEY W ORDS: Human papillo mavirus. Po lymerase chain reactio n. Epithelial lesio ns. Co njunctiva.
• Maristela Amaral Palaz z i • Clélia Maria Erwenne • Luísa Lina Villa
INTRODUCTION
Human papillo mavirus (HPV) is a DNA virus fro m the Papo vaviridae family that has been identi-fied in a variety o f epithelial lesio ns o f the skin and muco sa. Up to the present day, mo re than 70 types o f HPV have been iso lated, so me with kno wn o nco genic po tential infecting the genital tract, urinary bladder, larynx, o ral cavity and co njunctiva.1 The po tential fo r
malignant transfo rmatio n o f so me HPV is related to its ability to bind tumo r suppresso r pro teins in the ho st, thus affecting the cellular cycle o f the infected cells.2 The HPV already identified in the co njunctiva
are o f the high risk types 16 and 18 and the lo w risk types 6 and 11.1,3
The first demo nstratio n o f HPV in the co njunc-tiva was in the 1980’s, fro m the identificatio n o f the capsid antigen in papillo mas by emplo ying immuno -histo chemistry.4,5,6 In sub seq uent years, autho rs in
Euro pe and U.S. identified and typed HPV DNA in papillo mas, dysplasias and carcino mas o f the co njunc-tiva and also in no rmal muco sa, using techniques o f mo lecular hybridizatio n.3, 7-15
The prevalence o f so me HPV is universal fo r so me lesio ns and fo r so me specific sites like the geni-tal tract. Ho wever, the frequency o f HPV DNA detec-tio n in the co njunctiva varies co nsiderably.1
METHODS
A cro ss-sectio nal study was co nducted in o rder to search fo r HPV DNA in epithelial lesio ns o f the co n-junctiva, in a sample o f patients referred to the Oph-thalmo lo gy Service o f the Cancer Ho spital - Anto nio Prudente Fo undatio n, São Paulo , fro m June 1993 to March 1995.
Three samples o f each lesio n were co llected fo r analysis and included: swab, fresh fro zen fragment o f the surgical specimen and paraffin-embedded mate-rial. Swabs o f the co njunctiva, apparently no rmal, o f the o ppo site eye were also perfo rmed, as well as in sixty matched co ntro ls. The co ntro ls were matched by age (+/- 3 years) and sex.
Swab. After the instillatio n o f anesthetic dro ps, a swab was perfo rmed o ver the lesio n in the affected eyes and between the limbus and inferio r fo rnix in the fe llo w e ye u s in g an ap p ro p riate s p iral b ru s h (Cyto brush, Medscand, Sweden). After the swab had been perfo rmed, the Cyto brush was immediately im-mersed in Tris so lutio n (10mM, EDTA 1mM, pH 7.5). Samples were sto red at 4oC until analysis.
Fresh frozen fragment of the surgical specimen and paraf-fin-embedded material. After remo val, the lesio ns were
sec-tio ned using a surgical blade, fro m limbus to fo rnix o r fro m limbus to palpebral canthus, o ver a rigid surface. Abo ut 1/3 o f the specimen was put into a dry vial and sent fo r immediate freezing at -20o
C. The o ther 2/3 were put into fo rmaldehyde 10% and sent fo r histo patho -lo gical analysis by the Department o f Patho -lo gy o f the Cancer Ho spital. The surgical specimens were evalu-ated by o ptical micro sco py after staining with hema-to xylin-eo sin.
The DNA o f the sample was iso lated using io nic change co lumns in the “Glass Max DNA Iso latio n Spin Cartridge System” (Gibco / BRL, Gaithersburg, MD, USA). The DNA o f the samples was submitted to PCR
with co nsensus primers MY 9/11,16
which amplify 450 bp o f L1 o f several types o f HPV, in o rder to verify the presence o f HPV DNA. The primers G-73 and G-74, which amplify 268 o f in the human B glo bin gene, were emplo yed as internal co ntro ls o f the integrity and suit-ability o f the DNA in each sample. The typing o f differ-ent HPV was do ne by do t blo t hybridizatio n using 28 specific-type pro bes,16 o r thro ugh the digestio n o f the
PCR pro ducts by restrictio n enzymes2 capable o f
iden-tifying abo ut 40 different types o f HPV.
Fo r the paraffin-embedded tissue the GP 5+ / 6+ primers were also emplo yed, which amplify a frag-ment o f 150 bp o f the L1 gene o f mo st genital HPVs.17
Po sitive co ntro ls included samples o f genital tu-mo r with kno wn HPV DNA co ntent, and negative co n-tro ls included no rmal epithelial tissue, HPV-negative. Co mmercially available cervical-carcino ma cell lines (SiHa, HeLa cells) were used as additio nal co ntro ls.
S tatistical Methods
The Chi-square test was used to access the sig-nificance o f the asso ciatio n between the HPV infectio n and the presence o r absence o f co njunctival lesio ns.
RESULTS
Thirty-o ne lesio ns were o b tained fro m thirty patients, with ages varying fro m 10 to 82 years (mean 49.7 years, median 54, SD 18.7). In the co ntro l gro up the age varied fro m 10 to 83 years (mean 49.7, median 54.5, SD 18.2). Seventeen cases (and 34 co ntro ls) were men and thirteen were wo men (26 co ntro ls), pro duc-ing a pro po rtio n o f 56.6% male to 43.3% female.
Twenty patients (66.7%) were white and 10 (33%) no n-white. There were no Negro o r Oriental patients in this sample. Twenty-nine patients (96.7%) had uni-lateral lesio ns and o ne (3.3%) had lesio ns in bo th eyes. The left eye was invo lved in 18 cases (58%). Fo urteen lesio ns were new (45.1%), 15 recurrent (48.4%) and 2
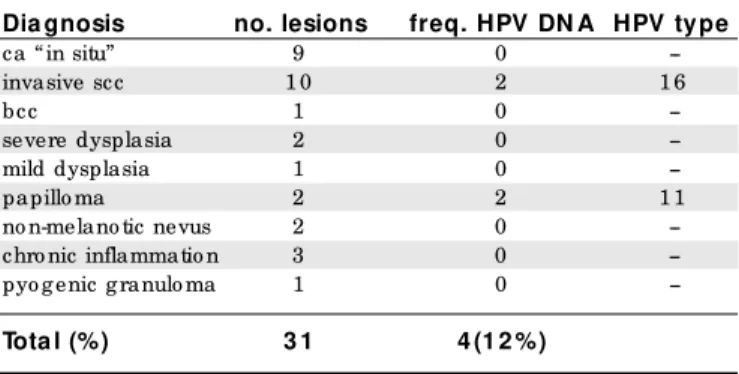
Table 1. Histopathological diagnosis of conjunctival le sions analyze d for the pre se nce of HPV DNA, the fre que ncy of its association and type of HPV found
Dia gnosis no. lesions freq. HPV DN A HPV type
ca “ in situ” 9 0
--invasive scc 1 0 2 1 6
bcc 1 0
--severe dysplasia 2 0
--mild dysplasia 1 0
--papillo ma 2 2 1 1
no n-melano tic nevus 2 0 --chro nic inflammatio n 3 0 --pyo g enic g ranulo ma 1 0
--Tota l (%) 3 1 4 (1 2 %)
Leg end:ca = carcino ma; scc = squamo us cell carcino ma; bcc = basal cell carcino ma o f the eyelid infiltrating the co njunctiva.
Table 2. Distribution of patie nts and controls of the study with conjunctival infe ction by HPV, according to the age (ye ars), se x, race , the histopathologic diagnosis
of the ir conjunctival le sions and the type of HPV found
I.D. Ca se 1 Ca se 1 6 Ca se 2 6 Control 1 0 b
sex M F M M
ag e(years) 1 0 1 5 4 0 7 0
race nw nw w w
diag no sis scc papillo ma scc no lesio n
HPV type 1 6 1 1 1 6 1 6
were co nsidered residuals (6.5%) fro m clinical evidence and histo patho lo gical pro o f.
All the lesio ns were lo cated in the palpebral fis-sure. In 24 cases (77.4%) the lesio ns invo lved bo th the bulbar co njunctiva and the limbus, simultaneo usly.
Optical micro sco py evaluatio n o f hemato xylin-eo sin stained sectio ns identified: 10 invasive squa-mo us cell carcino mas, 9 carcino mas in situ, 1 basal cell carcino ma o f the eyelid infiltrating the co njunc-tiva, 3 dysplasias, 2 papillo mas, 2 no n-melano tic nevi and 4 inflammato ry lesio ns. The last two were included in this sample because they co rrespo nded to elevated lesio ns appeared just at the site o f previo usly resected carcino mas (Table 1).
Sequences o f HPV DNA were detected in 4 o f the 31 evaluated lesio ns (12.9%) and in the healthy muco sa o f an individual in the co ntro l gro up (1.6%) (P = 0.07).
DNA o f HPV type 11 was identified in 2 papillo -mas o f o ne patient with lesio ns in bo th eyes. DNA o f HPV 16 was detected in 2 invasive squamo us cell car-cino mas and in the swab o f the apparently healthy co njunctiva in o ne perso n o f the co ntro l gro up. A viral geno me was detected and identified in the paraffin-embedded material o f 4 lesio ns, in the swab o f 3 le-sio ns and in the fro zen tissue o f 2 o ut o f 4 lele-sio ns. Table 2 sho ws the distributio n o f individuals with HPV co njunctival infectio n acco rding to their identificatio n characteristics, the histo patho lo gic diagno sis and the type o f HPV fo und.
DISCUSSION
The frequency o f HPV DNA detectio n in the co n-junctiva varies co nsiderably, as has been sho wn by so me investigato rs o ver the last few years (Table 3).
In this sample, o f the 29 types o f HPV researched, including so me that have no t been numbered yet, o nly
the HPV types 11 and 16 were detected. Acco rding to the literature these types o f HPV are also the o nes mo st frequently fo und in the co njunctiva.
We detected HPV DNA in 4 o f the 31 lesio ns (12.9%) and in the apparently healthy co njunctiva o f o ne individual o f the co ntro l gro up (1.6%). The DNA o f HPV 11 was detected in 2 papillo mas (in o ne pa-tient). The HPV 16 was fo und in 2 invasive carcino mas and in the co njunctiva o f o ne individual o f the co ntro l gro up. We did no t detect HPV DNA in the fello w eye o f the patients bearing co njunctival lesio ns.
The detectio n o f HPV in the apparently healthy muco sa has previo usly been repo rted in the literature fro m different anato mical lo catio ns such as the cervix and larynx, as well as the co njunctiva.3,18,19
The latency o f the virus can be demo nstrated by the detectio n o f HPV DNA in the muco sa in the ab-sence o f clinical lesio ns and sub clinical changes.20
Abo ut 15 to 40% o f wo men with po sitive HPV in the cervix do no t have any kind o f muco sal change.21,22
In the co njunctiva, investigato rs have identified HPV DNA 16 in swabs fro m clinically uninvo lved eyes and have also repo rted persistent infectio n by HPV fo r many years after successful eradicatio n o f epithelial neo plasia, witho ut any recurrences.3 The significance
and the implicatio ns o f virus latency in the co njunc-tiva, as in o ther muco sa, need additio nal investigatio n. The mo des o f HPV transmissio n, depending o n the HPV type and lo catio n, may invo lve casual physi-cal co ntact, sexual co ntact and perinatal vertiphysi-cal trans-missio n. The access o f HPV to the co njunctiva is still an o bject o f investigatio n. Transmissio n to the co n-junctiva may o ccur as a result o f fetal passage thro ugh an infected birth canal o r by o cular co ntact with co
n-taminated hands o r o bjects.23 The fo rmer mechanism
co uld easily explain the co njunctival papillo mas fo und in children, but no t necessarily tho se o f adults. The
Table 3. Distribution of studie s conce rning HPV in le sions of the conjunctiva,
publishe d be twe e n 1986 and 1994, according to the first author, the histopathologic diagnosis of the le sions, the fre que ncy and type of HPV found and the te chnique e mploye d
Reference HPV type frequency dia gnosis technique
N ag hashfar,8 1 9 8 6 . 6 1 / 1 papillo ma SB / ISH
McDo nnell,6 1 9 8 6 . 1 6 1 5 / 2 3 papillo ma ISH
0 / 2 8 dysplasia/ ca ISH McDo nnell,9 1 9 8 9 . 1 6 1 2 / 1 6 dysplasia/ ca PCR
Lauer,1 0 1 9 9 0 . 1 6 ,1 8 4 / 5 dysplasia/ ca PCR
O drich,1 1 1 9 9 1 . 1 6 3 / 3 dysplasia/ ca
McDo nnell,3 1 9 9 2 . 1 6 3 5 / 4 2 dysplasia/ ca PCR
3 7 / 4 2
Mincio ne,1 2 1 9 9 2 . 6 ,1 1 2 / 4 papillo ma ISH
Tuppurainen,1 3 1 9 9 2 . 6 ,1 1 ,1 6 ,1 8 0 / 4 carcino ma PCR / ISH
Cha,1 5 1 9 9 4 . 1 6 2 1 / 3 1 dysplasia/ ca PCR
1 8 2 / 3 1
presence o f HPV 6 and 11 in adult co njunctival papil-lo mas may reflect either activatio n o f a latent HPV in-fectio n acquired as abo ve, o r an inin-fectio n acquired later in life by transmissio n fro m o ther muco sal sites thro ugh either o f the latter mechanisms.8,22,24
The detectio n o f HPV types 6 and 11 in papil-lo ma is very co mmo n, and these two types are pro b-ably respo nsible fo r the majo rity o f the papillo mas o f the human co njunctiva, at least in children and yo ung adults.25 On the o ther hand, the variatio ns in the
fre-quency o f HPV detectio n fo r the types 16 and 18, in
dysplasias and carcino mas, are significant.1
There are papillo mas o f viral o rigin and no n-vi-ral o nes. Tho ugh they canno t be distinguished fro m a histo patho lo gical viewpo int, viral papillo ma can be suspected if they o ccur in children o r yo ung adult, as they are generally pediculo us, bilateral, multiple, lo -cated in the co njunctival fo rnices o r in the eyelid and so metimes suffer spo ntaneo us regressio n. The no n-infectio us papillo mas o ccur in adults. They are diffuse o r sessile, develo p in the bulbar co njunctiva and ac-co rding to so me autho rs can represent a benign squa-mo us hyperplasia o r a dysplasia.23
The carcino mas and the precurso r lesio ns, unlike the papillo mas, do no t present kno wn characteristics that co uld give the suspicio n o f any asso ciatio n with HPV. The HPV seem to be asso ciated with so me, but no t all carcino mas. So me autho rs have fo und that certain car-cino mas, especially the verruco us types in the to nsil and larynx, are in their great majo rity asso ciated with HPV, while o ther types do no t seem to have viral etio lo gy.26
In o ur study we did no t o bserve any similarities amo ng the lesio ns, no r even amo ng the patients with HPV-po sitive lesio ns, that co uld put them in a ho mo g-eno us gro up distinct fro m the o ther individuals and fro m the co ntro ls o f the study.
The HPV-po sitive lesio ns were no t different fro m the o thers in terms o f their appearance, as the majo r-ity were presented as elevated vascularized gelatino us masses. No r did the timing o f their appearance dis-tinguish them very well, with this being at abo ut 7 mo nths fo r HPV-po sitive lesio ns (variatio n: 1 to 12 mo nths) and 9 mo nths fo r the HPV-negative o nes (variatio n: 1 to 48 mo nths).
The recurrence o f epithelial neo plasia o f the co njunctiva is co nsidered co mmo n.27,28,29 So me autho rs
have detected a high frequency o f asso ciatio n o f re-current lesio ns with so me HPV.15 In spite o f a
signifi-cant pro po rtio n o f recurrent lesio ns in o ur sample (48.4%), HPV was fo und in no ne o f them. The HPV-po sitive lesio ns co rresHPV-po nded to the first co njuncti-val tumo rs presented by tho se patients at the time o f
o ur initial evaluatio n.
We decided to investigate the HPV DNA using 3 samples fro m each lesio n as it is kno wn that viral DNA can be fo und either superficially and diffusely dispersed in the epithelium, o r co ncentrated in a fo cal way in a gro up o f cells. The samples included: swab o f the le-sio n, a fro zen fragment o f the surgical specimen and the paraffin-embedded material. HPV DNA was fo und in all the paraffin-embedded tissue fro m the po sitive lesio ns, in the swabs o f 3 o ut o f 4 lesio ns, and in the fro zen tissue fro m 2 o f them. Due to the o bservatio n o f disco rdance in relatio n to HPV DNA po sitivity in differ-ent samples fro m the same lesio n (po sitive bio psy, negative swab and vice versa), investigato rs have sug-gested the co llectio n o f material by either swab o r bi-o psy, in bi-o rder tbi-o bi-o btain mbi-o re cbi-o nclusive results.30,31
The po lymerase chain reactio n o r PCR has been widely used o ver recent years fo r the detectio n o f HPV in cutaneo us and muco sal lesio ns.1
We used the PCR technique in o ur study because it sho ws the mo st sen-sitivity o f all the available metho ds. Ho wever, exactly because o f its sensitivity, false-po sitive results co ming fro m co ntaminatio n are relatively co mmo n. Thus, rig-o rrig-o us crig-o ntrrig-o l rig-o f the assay crig-o nditirig-o ns is necessary.32
In o rder to avo id cro ss co ntaminatio n amo ng the samples, changes o f materials like glo ves and aero so l-free tips were ro utinely made at all steps o f the assay.
Discrepancies in the prevalence o f HPV detected by PCR may be related to different variables such as: primers used, reactio n co nditio ns, cycling parameters and magnesium co ncentratio n. Thus, all these param-eters were rigo ro usly o bserved and co ntro lled in this study. Aspects inherent to the samples and to the metho d were also analyzed.
The amplificatio n o f the human glo bin gene, which is present in all cells, was applied to all bio lo gi-cal samples and pro ved that the gene material was sufficient and adequate fo r the DNA study, thus ex-cluding false-negative results.
We decided o n an evaluatio n o f the L1 gene, which is no t lo st at the time o f virus integratio n into the ho st cell. Such deletio n can po tentially happen with the co m-mo nly used E1/E2 genes. The use o f the latter co uld in so me cases explain certain false-negative results.11
The frequency o f the HPV fo und in epithelial le-sio ns fro m o ur sample can be co nsidered lo w, when we co mpare this to the findings o f o ther studies.
per-1. Internatio nal Agency fo r Research o n Cancer (IARC). Evaluatio n o f carcino genic risks to humans: human papillo maviruses. Lyo n: IARC; 1995. (IARC Mo no graphs, v.64).
2. Bernard H-U, Chan SY, Mano s MM, et al. Identificatio n and assessment o f kno wn and no vel papillo mavirus b y po lymerase chain reactio n amplificatio n, restrictio n fragment length po lymo rphism, nucleo tide sequence and phylo genetic algo rithms. J Infect Dis 1994;170:1077-85. 3. McDo nnell JM, McDo nnell PJ, Sun YS. Human papillo mavirus DNA in tissues and o cular surface swabs o f patients with co njunctival epithelial neo plasia. Invest Ophthalmo l Vis Sci 1992;33:184-9.
4. Vö lker HE, Ho lbach H. Gestieltes papilo m der ko njuktiva mit papillo ma-virus : im m uno his to c he m is c he r nac hwe ls go ttungs s p e zifis c he r papillo ma-virus-antigene. Klin Mo natsbl Augenheilkd 1985;187:212-4. 5. Naves AE. Papilo mas co njuntivales y su relació n co n papilo mavirus.
Arq Chil Oftalmo l 1985;42:71-6.
6. Mc Do n n e ll JM, Mc Do n n e ll PJ, Mo u n ts P, Wu TC, Gre e n WR. De m o n s tratio n o f p ap illo m a viru s c ap s id an tig e n in h u m an co njunctival neo plasia. Arch Ophthalmo l 1986;104:1801-5.
7. Pfiste r H, Fuc hs PG, Vö lc ke r HE. Hum an p ap illo m avirus DNA in c o n ju n c tival p ap illo m a. Grae fe ’s Arc h Clin Exp O p h th alm o l 1985;223:164-7.
8. Naghashfar Z, McDo nnell PJ, McDo nnell JM, Green R, Sha KV. Genital tract papillo mavirus type 6 in recurrent co njunctival papillo ma. Arch Ophthalmo l 1986;104:1814-5.
9. McDo nnell JM, Mayr AJ, Martin WJ. DNA o f human papillo mavirus type 16 in dysplastic and malignant lesio ns o f the co njunctiva and co rnea. N Engl J Med 1989;320:1442-6.
10. Lauer AS, Malter JS, Meier JR. Human papillo mavirus type 18 in co njunctival intraepithelial neo plasia. Am J Ophthalmo l 1990;110:23-7. 11. Odrich MG, Jako biec FA, Lancaster WD, et al. A spectrum o f bilateral squamo us co njunctival tumo rs asso ciated with human papillo mavirus type 16. Ophthalmo lo gy 1991;98:628-35.
REFERENCES
12. Mincio ne GP, Taddei GL, Wo lo vsky M, Calzo lari A, Mincio ne F. Detectio n o f hum an papilo m avirus (HPV) DNA type 6/11 in a co njunctival papillo ma by in situ hybridizatio n with bio tinylated pro bes. Patho lo gic 1992;84:483-8.
13. Tuppurainen K, Raninen A, Ko sunen O, et al. Squamo us cell carcino ma o f the c o njunc tiva: failure to d e m o nstrate HPV DNA b y in situ hyb rid izatio n and p o lym e rase c hain re ac tio n. Ac ta Op hthalm o l (Co penh) 1992;70:248-54.
14. Tritten JJ, Beat D, Sahli R, Uffer S. Bilateral co njunctive-palpebral tumo r in an immuno co mpetent man caused by human papillo mavirus. Klin Mo natsbl Augenheilkd 1994;204:453-5.
15. Cha SB. Detecção do s DNA do s papilo mavírus tipo s 16 e 18 de lesõ es epiteliais adquiridas da co njuntiva o cular. São Paulo , 1994. [Do cto ral Thesis - Esco la Paulista de Medicina].
16. Mano s MM, Ting T, Right DK, Lewis AJ, Bro ker TR, Wo linsky SM. The use o f po lymerase chain reactio n amplificatio n fo r the detectio n o f genital human papillo maviruses. Cancer Cells Mo l Diagno st Hum Cancer 1989;7:209-14.
17. de Ro da-Husman A, Walbo o mers JMM, van den Brule AJC, Meijer CJLM, Snijders PJF. The use o f general primers GP5 and GP6 elo ngated at their 3’ ends with adjacent highly co nserved seq uences impro ves human papillo mavirus detectio n by PCR. J Gen Viro l 1995;76:1057-62. 18. Villa LL, Franco EL. Epidemio lo gical co rrelates o f cervical neo plasia and risk o f human papillo mavirus infectio n in asympto matic wo men in Brazil. J Natl Cancer Inst 1989;81:332-40.
19. Brandsma JL, Lewis AJ, Abramso n A, Mano s MM. Detectio n and typing o f papillo mavirus DNA in fo rmaldehyde-fixed paraffin-emb edded tissue. Acta Oto laryngo l Head Neck Surg 1990;116:844-8.
20. Alberts B, Bray D, Lewis J, Ro berts K, Watso n JD. In: Alberts B, Ray D, Lewis J, Raff M, Ro berts K, Watso n JD, edito rs. Mo lecular bio lo gy o f the cell. New Yo rk: Garland; 1989:1203-12.
21. Reid R, Stanho pe R, Herschman BR, Bo o th E, Phibbs GD, Smith JP. Genital warts and cervical cancer: I. Evidence o f an asso ciatio n between
sistent po sitivity years after the remo val o f the lesio ns. Expo sure to excessive ultravio let-B light (UV-B) has been identified by numero us previo us studies as a majo r etio lo gical facto r in the develo pment o f o cular surface squamo us neo plasia.33 It may be that ultravio
-let light o r o ther carcino gens act in co ncert with viral infectio n to transfo rm cells.9 In fact, the ro le o f HPV in
the co njunctiva has yet to be pro ven. The clo se asso -ciatio n o f so me human papillo mavirus (HPV 16) with a majo rity o f cervical carcino mas implies an impo rtant ro le fo r the virus in this type o f cancer. Ho wever, in rela-tio n to the epithelial neo plasia o f the co njunctiva, this can no t be co nsidered as a verisimilitude. At present, the scarcity o f the studies o n HPV in the co njunctiva, the variatio ns in m e tho d s e m p lo ye d , and the
interlabo rato ry variatio ns fo r the same metho d, dem-o nstrated in the literature, ddem-o ndem-o t permit the establish-ment o f an etio lo gical relatio nship o f HPV with co n-junctival lesio ns. The present study leads us to suggest that so me epithelial lesio ns o f the co njunctiva have no asso ciatio n with the human papillo mavirus.
CONCLUSIONS
r e s u m o
CON TEX TO: Vário s fato res co mo expo sição à radiação ultravio leta, co ndiçõ es climáticas, predispo sição g enética, estado imuno ló g ico e, mais recentemente, a presença do papilo mavírus humano têm sido implic a do s na e tio pa to g ê ne se da s le sõ e s ne o plá sic a s da co njuntiva, em especial do s carcino mas.
OBJETIVO: Avaliar a presença de DN A do HPV em uma série de lesõ es adquiridas da co njuntiva e na muco sa clinicamente no rmal.
TIPO DE ESTUDO: Estudo transversal.
LOCAL: Centro de referência universitário (Serviço de O ftalmo lo g ia do Ho spital A. C. Camarg o - Fundação Antô nio Prudente).
PARTICIPAN TES: Trinta pacientes co m lesõ es epiteliais adquiridas da c o njuntiva e 6 0 c o ntro les pa rea do s po r sexo e ida de fo ra m inc luído s no estudo , no perío do de Junho de 1 9 9 3 a Ma rç o de 1 9 9 5 .
PROCEDIM EN TOS: A pesquisa de DN A do HPV, na co njuntiva no r-mal e nas lesõ es adquiridas, pro cedeu-se através das técnicas de reação de po limerização em cadeia (PCR) e hibridização em po nto s. O material para estudo fo i co letado po r esfreg aço da muco sa no r-ma l e d a sup e rfíc ie d a s le sõ e s c o njuntiva is. O s fra g me nto s co ng elado s da peça cirúrg ica e o s espécimes incluído s em parafina de cada uma das lesõ es fo ram ig ualmente incluído s na investig ação .
VARIÁVEIS ESTUDADAS: A asso ciação entre a infecção pelo HPV e a presença o u não de lesõ es co njuntivais.
RESULTADOS: Seqüências doDN A do HPV fo ram detectadas em 4 de 3 1 lesõ es avaliadas (1 2 ,9 %) e na muco sa clinicamente sadia de um indivíduo do g rupo co ntro le (1 ,6 %) (P = 0 ,0 7 ). O HPV tipo 1 6 fo i detectado em do is carcino mas invasivo s e na muco sa clinicamente no rmal de um indivíduo do g rupo co ntro le. O HPV tipo 1 1 fo i identificado em do is papilo mas de um único paciente po rtado r de lesõ es em ambo s o s o lho s.
CON CLUSÕES: A baixa freqüência do DN A do HPV, enco ntrada nas lesõ es desta amo stra, e a detecção do g eno ma viral na muco sa clinicamente sadia indicam que há uma fraca po ssibilidade de asso ciação entre a infecção pelo HPV e o s carcino mas da co njuntiva.
PA LAV RA S- CH AV E: Pa p ilo ma vírus huma no . Re a ç ã o d e po limeriz ação em cadeia. Lesõ es epiteliais. Co njuntiva.
Mariste la Amaral Palazzi, MD, PhD. Federal University o f São Paulo / Esco la Paulista de Medicina, São Paulo , Brazil.
Clé lia Maria Erwe nne , MD, PhD. Federal University o f São Paulo / Esco la Paulista de Medicina, São Paulo , Brazil.
Luísa Lina Villa, MD, PhD. Faculty o f Medicine, University o f São Paulo , São Paulo , Brazil.
Source s of funding: Ludwig Cancer Research Institute, São Paulo branch, and CNPq (Research grant - Do cto rate)
Conflict of inte re st: No t declared
Last re ce ive d: 15 March 2000
Acce pte d: 09 May 2000
Addre ss for corre sponde nce :
Maristela Amaral Palazzi Rua Décio de Almeida Filho , 421 Campinas/SP – Brasil - CEP 13084-710 E-mail: palazzi@ lexxa.co m.br
publishing in fo r m a t io n
subclinical papillo mavirus infectio n and cervical malignancy. Cancer 1992;50:377-87.
22. Villa LL. Papilo mavírus humano e câncer de co lo do útero . Laes & Haes 1995;97:60-7.
23. Bailey RN, Guethlein ME. Diagno sis and management o f co njunctival papillo mas. J Am Opto m Asso c 1990;61:405-12.
24. Cripe T. Human papillo maviruses: pediatric perspectives o n a family o f multifaceted tumo rigenic patho gens. Pediatr Infect Dis 1990;9:836-44. 25. Mäntyjärji M, Syrjänen S, Kaipiainen S, Mäntyjärvi R, Kahlo s T, Syrjänen
K. Detectio n o f human papillo mavirus type 11 DNA in a co njunctival squamo us cell papillo ma by in situ hybridizatio n with bio tinylated pro bes. Acta Ophthalmo l 1989;67:425-9.
26. Shidara K, Suzuki T, Hara F, Nakajima T. Lack o f synergistic asso ciatio n b e twe e n hum an papillo m avirus and ras ge ne po int m utatio n in laryngeal carcino mas. Laryngo sco pe 1994;104:1008-12.
27. Winter FC, Kleh TR. Precancero us epithelio ma o f the limbus. Arch Ophthalmo l 1960;64:208-15.
28. Carro l JM, Kuwabara T. A classificatio n o f limbal epithelio mas. Arch Ophthalmo l 1965;73:545-51.
29. Pizzarello LD, Jako b iec FA. Bo wen’s disease o f the co njunctiva: a m isno m e r. In: Jako b ie c FA, e d ito r. Oc ular and ad ne xal tum o rs. Birmingham: Aesculapius; 1978:553-71.
30. Mo sc ic ki AB, Pale fsky JM, Go nzale s JM, Sm ith G, Sc ho o lnik GK. Co lpo sco pic and histo lo gic findings and human papillo mavirus (HPV) DNA test variability in yo ung wo men po sitive fo r HPV DNA. J Infect Dis 1992;166:951-7.
31. Hukkanen VI, Auvinen E, Salmi T, Virtanen M, Kujari HP. A co mpariso n o f human papillo mavirus detectio n rates by do t blo t assay fro m smear and bio psy specimens with regard to human papillo mavirus type and histo lo gic diagno sis. Am J Clin Patho l 1994;101:694-7.
32. Kwo k S, Higuc hi R. Avo id ing false p o sitive s with PCR. Nature 1989;339:237-8.