PRIMARY VERSUS SECONDARY IMPLANTATION OF SCLERAL
FIXATED POSTERIOR CHAMBER INTRAOCULAR LENS
Shashidhar S1, Suresh Babu G2, Shruthi Chandra3, Manasa Penumetcha4
HOW TO CITE THIS ARTICLE:
Shashidhar S, Suresh Babu G, Shruthi Chandra, Manasa Penumetcha. ”Primary Versus Secondary Implantation of Scleral Fixated Posterior Chamber Intraocular Lens”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 32, August 10, 2015; Page: 4760-4770, DOI: 10.18410/jebmh/2015/668
ABSTRACT: AIM: To assess and compare the visual outcome of primary and secondary implantation of scleral fixated posterior chamber intraocular lens (SFIOL). METHODS: This is a retrospective study of 45 eyes of 44 patients who had undergone SFIOL procedure from July 2008 to February 2014. SFIOLs were implanted as a primary procedure or as a secondary procedure and the results which included the visual outcome in the two groups were compared and analyzed. RESULTS: There were 18 and 27 eyes in which SFIOL was implanted as primary and secondary procedure, respectively. Follow up ranged from 3-24 months. Mean log MAR post-operative best corrected visual acuity in primary procedure was not significantly different (0.39(SD=0.21)) from that of secondary procedure (0.42(SD=0.25)) (p = 0.64). Post-operative best corrected visual acuity of 6/18 or better was achieved in 66.67% and 70.37% in primary SFIOL and secondary SFIOL group, respectively. In primary group 12 eyes (66.67%) had early complications as compared to 9eyes (33.33%) in the secondary group (p = 0.03). Late complications were observed in 5 eyes (27.78%) of primary SFIOL and 1 eye (3.70%) of secondary SFIOL. CONCLUSION: Secondary implantation of SFIOL seems to have a lower early complication rate than primary implantation although the final visual acuity and late complication rate are not significantly different. Hence, SFIOL offers a novel approach towards visual rehabilitation of aphakic patients who have zonular dehiscence or lack capsular support.
KEYWORDS: SFIOL: Scleral fixated intraocular lens, BCVA: Best corrected visual acuity, log MAR: Logarithm of minimum angle of resolution.
INTRODUCTION: Rehabilitation of aphakic eyes in the absence of adequate capsular support remains a major challenge. Lack of lens capsule support after complicated cataract surgery or trauma has been reported as an indication for scleral fixation of PCIOL in several studies. ACIOL implantation may also not be feasible due to extensive iris and anterior chamber angle damage in these eyes. Iris-sutured IOLs carry the risk of post-operative inflammation (CME, uveitis) and iris atrophy with pigment dispersion syndrome. The universally accepted indication for scleral fixated intraocular lens implantation is aphakia in a patient who is not a good candidate for anterior chamber intraocular lens implantation and iris fixated IOLs.1,2
MATERIALS AND METHODOLOGY: This is a retrospective study of consecutive patients treated from July 2008 – February 2014. A total 45 eyes of 44 patients were included in the study. Of these 40 patients underwent SFIOL implantation with anterior vitrectomy while 4 patients had to undergo 3 ports pars plana vitrectomy before SFIOL implantation.
These eyes were selected because they did not have sufficient posterior capsule/zonular support for posterior chamber lens implantation and/or sufficient iris for anterior chamber lens implantation or iris fixated IOL, and all had a minimum follow up of 3 months.
Inclusion Criteria:
1. Post Intracapsular cataract extraction aphakia/complicated cataract surgery with posterior capsular dehiscence.
2. Patients who have undergone lensectomy with posterior segment surgery.
3. Traumatic subluxation/dislocation of crystalline cataractous lens.
4. Congenital conditions with subluxated/dislocated crystalline/cataractous lens.
5. Subluxated/dislocated posterior chamber intraocular lens.
Exclusion Criteria: Corneal opacity, chronic uveitis, optic nerve pathology and macular pathology interfering with final visual outcome.
PATIENT EVALUATION: Patient demographics, pre-operative and post-operative snellen’s best corrected visual acuity (BCVA), nature and complications of surgery as well as postoperative complications were noted. The BCVA was converted into logarithm of the minimum angle of resolution (log MAR) units for statistical analysis. Visual acuity of hand movements and light perception was arbitrarily assigned equivalent of 1.7 and1.8 log MAR units, respectively. For statistical analysis, unpaired t test and sample t tests were performed. A p value of 0.05 or less was considered to be statistically significant.
PROCEDURE: All cases underwent abexterno 2 point Scleral fixation using Modified Basti’s
suturing technique.
POST OPERATIVE EVALUATION: Patients were evaluated on first post-operative day then subsequently at 1 week, 4 weeks and 3 months post-surgery. At each visit all patients were submitted to detailed evaluation including the visual acuity, anterior and posterior segment examination and refraction.
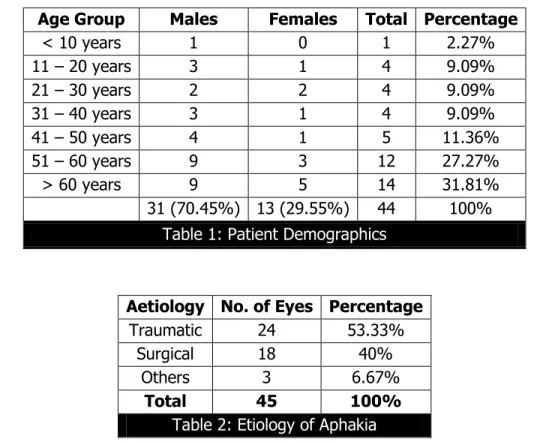
Age Group Males Females Total Percentage
< 10 years 1 0 1 2.27%
11 – 20 years 3 1 4 9.09%
21 – 30 years 2 2 4 9.09%
31 – 40 years 3 1 4 9.09%
41 – 50 years 4 1 5 11.36%
51 – 60 years 9 3 12 27.27%
> 60 years 9 5 14 31.81%
31 (70.45%) 13 (29.55%) 44 100%
Table 1: Patient Demographics
Aetiology No. of Eyes Percentage
Traumatic 24 53.33%
Surgical 18 40%
Others 3 6.67%
Total 45 100%
Table 2: Etiology of Aphakia
Indiactions for surgery was aphakia in 40% with the remaining being subluxated and dislocated crystalline and intraocular lenses. (Table 3). Out of the 9 patients with dislocated cataractous/crystalline lens, 7(77.78%) were posteriorly dislocated lenses and 2(22.22%) were anteriorly dislocated.
Indications for Surgery No. of Eyes Percentage
Aphakia 19 42.22%
Subluxated Lens 13 28.89%
Decentered IOLs 2 4.44%
Dislocated Lens 9 20%
Dislocated IOLs 2 4.44%
Total 45 100%
Table 3: Indications for Surgery
corrected visual acuity logMAR was 0.33±0.44 (range of Snellen visual acuity 5/60-6/6). All the patients had a minimum of 3 lines improvement in the final visual acuity as recorded on the Snellens visual acuity chart, compared to the pre-operative best corrected visual acuity. The preoperative best corrected visual acuity and the post-operative best corrected visual acuity were compared using paired-t test statistical method and the p value calculated was <0.0001. This value is extremely statistically significant.
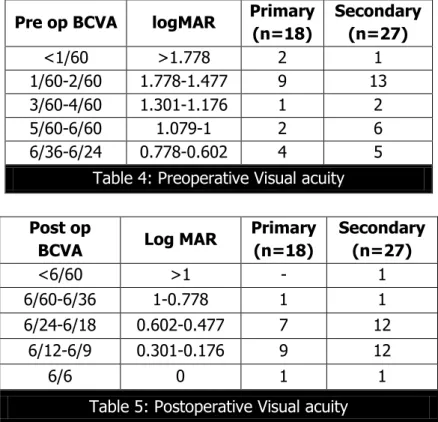
Pre op BCVA logMAR Primary (n=18)
Secondary (n=27)
<1/60 >1.778 2 1
1/60-2/60 1.778-1.477 9 13
3/60-4/60 1.301-1.176 1 2
5/60-6/60 1.079-1 2 6
6/36-6/24 0.778-0.602 4 5
Table 4: Preoperative Visual acuity
Post op
BCVA Log MAR
Primary (n=18)
Secondary (n=27)
<6/60 >1 - 1
6/60-6/36 1-0.778 1 1
6/24-6/18 0.602-0.477 7 12
6/12-6/9 0.301-0.176 9 12
6/6 0 1 1
Table 5: Postoperative Visual acuity
Between the two groups of primary and secondary implantation the mean post-operative best corrected visual acuity log MAR was 0.39±0.21 and 0.42±0.25. The p value was 0.64 which was not statistically significant, which meant that the final visual outcome in both the types of procedure did not differ significantly. Post-operative best corrected visual acuity of 6/18 or better was achieved in 12 out of 18 cases (66.67%) and in 19 eyes out of 27(70.37%), in the primary and secondary group, respectively.
Intraoperative Complications (Table 6):
Intra Op Complications Primary SFIOL Secondary SFIOL Percentage
Hyphaema 4 8.89%
Hypotony 3 6.67%
Suture breakage 2 4.44%
Total 9 20%
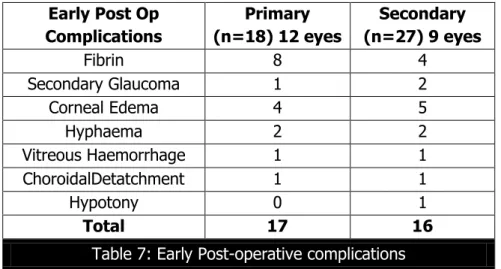
The early post-operative complications were seen in 21 eyes (46.67%), with same eye showing multiple complications in 9 patients. The incidence of early postoperative complications was higher in the primary group (17 complications in 12 eyes (66.67%)) than the secondary group (16 complications in 9 eyes (33.33%)). The p value was 0.03, which was statistically significant (Fisher’s exact test) (Table 7).
Early Post Op Complications
Primary (n=18) 12 eyes
Secondary (n=27) 9 eyes
Fibrin 8 4
Secondary Glaucoma 1 2
Corneal Edema 4 5
Hyphaema 2 2
Vitreous Haemorrhage 1 1
ChoroidalDetatchment 1 1
Hypotony 0 1
Total 17 16
Table 7: Early Post-operative complications
On comparing the incidence and number of late postoperative complications between the two groups, even though primary group had higher incidence of late complications the difference between the two groups was not statistically significant (Table 8).
Late Complications (After 1 month)
Primary (n=18)
Secondary (n=27)
Glaucoma 2 0
Pupil Deformation 0 0
Persistent Uveitis
(AC cells > 1+) 1 0
Cystoid Macular Edema 1 0
IOL Decentration 1 1
Total 5 1
Table 8: Late Postoperative Complications
DISCUSSION: The design, fixation site and indications for IOL implantation have changed a lot since their introduction by Harold Ridley. In the absence of capsular support and zonular deficiency anterior chamber lens/iris fixated lenses are advocated, but they do have complications.To avoid these complications, methods to trans sclerally fixated posterior chamber lenses to the ciliary sulcus have been developed. Malbran and co-authors were the first to report SFIOLs in aphakic patients.
The decision for trans-scleral PCIOL fixation should be individualized based on the risks and benefits. The procedure itself is difficult and has increase operative time, risk of intra ocular haemorrhage, suture exposure as complications3,4 Previous studies have not definitely set surgical
indications and optimal timing for management of dislocated intraocular lenses. The management approach depends on surgeon preferences and individual case specifications, including integrity of capsule remnants, type of intraocular lenses, and coexisting ocular pathology. In this study, age and sex distribution correlates with study done by Ghaseminejadet al.2
Of the 45 eyes, scleral fixated intraocular lens was implanted as a primary procedure in 18 eyes (40%) and as a secondary procedure in 27 eyes (60%). The median interval from the initial surgery to the definitive procedure was 60 days (range 14–180 days). Eyes with longer duration between the initial surgery and definitive procedure had better visual outcome. That could have been due to lack of inflammation, normalization of intraocular pressure and resolution of post-operative corneal edema.
The pre-operative visual acuity logarithm of minimum angle of resolution (logMAR) was 1.39±0.43 (range of Snellen visual acuity, 1/60–6/36). In the study done by Shouman et al5, the
pre-operative mean best corrected visual acuity logarithm minimum angle of resolution was 1.67 (Range of Snellen visual acuity, 1/60 – 6/60) which was similar to the range of visual acuity in our study. Between the two groups of primary and secondary intraocular lens implantation, the mean logMAR was 1.43±0.45and 1.37±0.42 respectively. The p value was 0.63 which was not statistically significant, which meant that the groups were similar with respect to preoperative visual acuity.
Between the two groups of primary and secondary implantation the mean post-operative best corrected visual acuity logMAR was 0.39±0.21 and 0.42±0.25. The p value was 0.64 which was not statistically significant, which meant that the final visual outcome in both the types of procedure did not differ significantly. Post-operative best corrected visual acuity of 6/18 or better was achieved in 12 out of 18 cases (66.67%) and in 19 eyes out of 27(70.37%), in the primary and secondary group, respectively. In a study done by Lee et al,6 mean logMAR post-operative
best corrected visual acuity in primary group was not significantly different from that of secondary group. Post-operative best corrected visual acuity of 6/12 or better was achieved in 58.6% and 76.0% in primary and secondary group, respectively, which was similar to our study. The various complications encountered were grouped as intraoperative complications, early post-operative complications and late post-post-operative complications.
The intra operative complications were seen in 9 eyes (20%). 4 eyes (8.89%) had minimal ooze while passage of needles which led to hyphaema and vitreous hemorrhage post operatively, 3 eyes (6.67%) had hypotony, and in 2 eyes (4.44%) there was suture breakage during the procedure. The cause of bleeding usually is damage to long posterior ciliary arteries, iris circle artery and hyper vascular tissue of ciliary body.
Hypotony was noted in 3 cases out of which one underwent primary procedure and the other two patients underwent secondary procedure. According to Woo et al, risk factors for intraoperative hypotony are young age of patient, previous vitrectomy with base dissection.7 Out
correlated well with Woo et al regarding the risk factors for intraoperative hypotony. Hypotony was managed in all three cases by intracameral injection of viscoelastic agents per-operatively. To prevent persistence of this complication postoperatively, after washing the viscoelastic out of the anterior chamber, air was injected in the anterior chamber. At the end of procedure, the intraocular pressure was maintained fairly well.
The early post-operative complications were seen in 21 eyes (46.67%), with same eye showing multiple complications in 9 patients. Fibrin reaction is a result of extensive intraoperative uveal tissue manipulation. Though iris tissue handling and trauma to pars plana occurs in all patients, extensive fibrin reaction is seen in patients when the eye is already inflamed due to previous inflammation following surgery or trauma or in diabetics. In our study, 7 out of the 12 patients had history of trauma. This explained the intense post-operative reaction. Kwong and Kanigowska K in their study documented anterior uveitis in 5 eyes (16.7%) which was mainly due to iris manipulation8.This lower incidence was attributed to increased interval between the initial
and secondary procedure which helped for the inflammation to subside.
Secondary glaucoma in the early postoperative period was documented in 3 patients (6.67%). One patient had associated fibrin reaction in anterior chamber which would be responsible for the rise in intraocular pressure. Since the indication for surgery was anteriorly dislocated lens, it was presumed that the lens might have damaged the fine angle structures leading to compromised aqueous outflow. By the 1st month of follow up the intraocular pressure had normalized and the gonioscopy did not reveal any angle abnormalities. In the study by Mazhryet al9 the incidence of glaucoma was on lower side (4%). This was almost similar to our
study. The incidence of secondary glaucoma postoperatively was high in studies done by Arkins and Steinert10 (22%) and Holland and co-workers11 (24%). This lower incidence in our study and
that done by Mazhry et al may be related to better selection of the patients as most of the patients were planned as primary or secondary procedure combined with vitrectomy only, where as in the studies by Arkins et al and Holland et al the procedure was combined with penetrating keratoplasty.
Corneal edema was seen on the first postoperative day in 9 patients. There was evidence of descemet’s detachment postoperatively in one patient. In two of the nine eyes, the indication for surgery was anteriorly dislocated cataractous lens which was in the anterior chamber for 48 hours before the patient reported to the hospital. This endothelial-lenticular touch would have led to endothelial cell loss contributing to the corneal edema. The other causes for corneal edema were coexisting raised intraocular pressure, hyphaema and anterior iridocyclitis in these patients. According to Lin et al,12 transient corneal edema occurred due to high or low intraocular pressure,
vitreous loss, fluid stream during anterior vitrectomy, or postoperative anterior uveitis. This corneal edema resolved during the follow-up period.12 This was consistent with our study as the
aetiology was similar in our patients and also the corneal edema resolved during the follow up period.
Hyphaema and vitreous hemorrhage was seen in 4 eyes (8.89%) and 2 eyes (4.44%) respectively. In a study done by Amoozadeh J et al,13 they observed 2 innocent vitreous
intraocular lenses noted the most common intraoperative and early post-operative complication was vitreous haemorrhage in 8 eyes (16%) followed by hyphaema in five eyes (10%). In our study the incidence was comparable to the study done by Mazhri et al. This was probably because majority patients underwent abexterno two point fixation using Basti modification. In abexterno two point fixation we used 26 gauge needle for passage through a point 1.5mm posterior to limbus which causes least trauma to the ciliary body, decreases the intraoperative ooze and thereby decreases postoperative incidence of hyphaema and vitreous hemorrhage. Hidemann and Dunn reported 11% incidence of vitreous haemorrhage and hyphaema14. Vitreous
haemorrhage cleared in all the patients within 1-3 weeks with no residual complications while hyphaema resolved within 3-7 days in all the cases.
Choroidal detachment confirmed on B- scan ultrasound was seen in 2 patients (4.44%). Both of these patients had intraoperative hypotony which might have been the cause for the choroidal detachment. In both these patients there was no wound leak detected. The scan showed serous choroidal detachment in both the cases. It was managed by a short course of oral steroids. At follow up of 1 month the detachment had subsided in one patient and his vision had improved from hand movements to 6/24. The other patient also had some persistent uveitis along with the detachment. His detachment subsided by 3 months.
The incidence of early postoperative complications was higher in the primary group (17 complications in 12 eyes (66.67%)) than the secondary group (16 complications in 9 eyes (33.33%)). The p value was 0.03, which was statistically significant (Fiesher’s exact test). This was in accordance with the results of study done by Lee et al.6 In their study, in the primary
group, 25(83.3%) eyes had a total of 55 early complications, while in the secondary group, 16 (64%) eyes had 26 early complications (p=0.028). The difference in early complications was statistically significant.
The late post-operative complications were observed in 6 patients (13.33%). Two patients had secondary glaucoma of which one of them had severe fibrin reaction with hyphaema in early post-operative period which did not subside with treatment. The patient had been irregular with usage of medication leading to persistence of inflammation and raised intraocular pressure. The inflammation and intraocular pressure were both brought under control by 3 weeks.
Cystoid macular edema confirmed by OCT was seen at 1 month follow up in one patient. Although macular edema is present in all patients during the first post-operative hours, cystoid macular edema usually begins 1-3 months post operatively.15 Vitreous adherent to the
post-operative wound or left within the anterior chamber may become entangled with the intraocular lens, lead to traction on the retina, produce chronic inflammation and cystoid macular edema.15,16
Inflammation itself can produce cystoid macular edema. Incidence of CME is reported to be quiet high in some of the studies as reported by Arkins and Steinert10 (9-36%). It was only 2% in the
study done by Mazhry et al while 6% has been reported by McCluskey and Harrisburg24 in their
32 patients. Qazi mentioned 1.66% in his study.17 This was in agreement with study by Mazhryet
al9 and interestingly it was comparable to even routine PC IOL implantation (2%).24 In our study
Malposition of the intraocular lens includes decentration and tilt.18 There were two
patients (4.44%), one in each group, who developed decentration of the intraocular lens. In the presence of loose suture to the sclera, the scleral fixated PCIOL can be tilted or decentred causing glare or diplopia to the patient.19,20 5-10% incidence of IOL tilt or decentration has been
reported in the literature.10 This decentration in our study was clinically significant only in 1 eye
(2.22%). In study by Mazhri et al9 it was 8% and it was clinically significant only in one eye. This
decentration in their study occurred 2 weeks post operatively and was related to trauma and accompanied by vitreous haemorrhage.9 Our results were similar to this study though our
patients did not have history of postoperative trauma. Lee et al6 in their study of comparison of
outcomes of primary and secondary implantation of scleral fixated posterior chamber intraocular lens concluded that the difference between the two groups was not statistically significant (unpaired Student’s t test, p=0.07).
On comparing the incidence and number of late postoperative complications between the primary and secondary groups in our study, primary group had higher incidence of late post-operative complications but the BCVA were not statistically significant (p=0.15, using unpaired Student’s t test).
There are more sight threatening complications such as corneal edema, glaucoma, and cystoid macular edema in primary group. This may be attributed to the prolonged surgical time in primary SFIOL implantation, as extra time is already used in the first part of the operation during cataract extraction.
CONCLUSION: Comparison of final visual outcome in primary versus secondary scleral fixation of intra ocular lens implantation revealed no statistically significant difference between the groups, even though the primary group showed statistically significant higher incidence of early post-operative complications. Therefore, we concluded that scleral fixation of posterior chamber intraocular lens is an effective means of visual rehabilitation of patients with aphakia and those lacking capsular/zonular support and may be done as a primary or secondary procedure with special care of the primary group in the early post-operative period.
REFERENCES:
1. Roger F Steinert, Martin S Arkin. Chap 41. Secondary intraocular lens implantation and stabilization. In: Roger F Steinert, editor. Cataract surgery.3rd ed. Saunders Elsevier; 2010. p. 487-99.
2. Khosro A, Hamid A. Trans-scleral fixation of Posterior chamber intraocular lens combined with Vitreoretinal surgery. Iranian Journal of Ophthalmic research 2006; 1(2): 96-100. 3. Johnston R, Charteris D, Horgan S, Cooling R. Combined pars planavitrectomy and sutured
posterior chamber implant. Arch Ophthalmol 2000; 118: 905-10.
4. Solomon K, Gussler JR, Gussler C, Van Meter WS. Incidence and management of complications of transsclerally sutured posterior chamber lenses. J Catarct refract Surg 1993; 19: 488-93.
5. Shouman A, Hashem A, Marzouk M, Zakzook E. Journal of American Science 2010; 6(10): 852-859.
6. Lee VYW, Yuen HKL, Kwok AKH. Comparison of outcomes of primary and secondary implantation of scleral fixated posterior chamber intraocular lens.Br J Ophthalmol. 2003 December; 87(12): 1459–62.
7. Woo SJ, Park KH, Hwang JM, Kim JH, Yu YS, Chung H. Risk factors associated with sclerotomy leakage and post-operativehypotony after 23- gauge transconjunctivalsutureless vitrectomy. Retina 2009; 29(4): 456-63.
8. Kanigowska K, Gralek M, Karczmarewicz B. Transsclerally fixated intraocular artificial lenses in children- longterm postoperative complication. KilnOczna 2007; 109: 286-7.
9. Mazhry Z, Kadri WM. Classification and Evaluation of secondary posterior chamber intraocular lens implantation Scleral fixation of intraocular lens. Pak J Ophthalmol 2010; 26(3): 148-153.
10.Arkin MS, Steinert RF. Sutured posterior chamber intraocular lenses. In: Jacobiec FA, Adamis AP, Volpe NJ. Eds International Ophthalmology Clinics. Controversies in Ophthalmology: Current therapies and Emerging Technologies. Boston: Little, Brown and Company. 1994; 34: 67-86.
11.Holland EJ, Daya SM, Evenglista A, et al. Penetrating keratoplasty and transscleral fixation of posterior chamber lens. Am J Ophthalmol.1992; 114: 182-7.
13.Amoozadeh J, Naderi AR, Rahmini F. Results and Complications of sclera fixated (sutured) posterior chamber intraocular lens implantation. ActaMedicaIranica 2001; 39(4): 195-198. 14.Heidemann DG, Dunn SP. Visual results and complications of transsclerally sutures
intraocular lenses in penetrating keratoplasty. Ophthalmic Surg. 1990; 21: 60.
15.Price FW, Whitson WE. Visual result of suture fixated posterior chamber lenses during penetrating keratoplasty. Ophthalmology 1989; 96: 1239-40.
16.Soong KH, Mush DC, Kowel V, Meyer RF. Implantation of posterior chamber intraocular lenses in the absence of lens capsule during penetrating keratoplasty. Arch ophthalmol 1989; 107: 660-664.
17.Qazi ZA. Retrospective study of 62 patients with transscleral fixation of IOL (Paper presented at Lahore Ophthalmo 95 held by Ophthalmological Society of Pakistan in December 1995).
18.Oshika T, Sugita G, Miyata K, Tokunga T, Samejina T, Okamoto C, Ishii Y. Influence of tilt and decentration of scleral- sutured intraocular lens on ocular higher order wavefeont aberration. Br J Ophthalomol 2007; 91(2): 185-188.
19.K. Hayashi, H. Hayashi, F. Nakao, and F. Hayashi. Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans-scleral suture fixation surgery. Ophthalmology 1999; 106(5): 878–889.
20.Durak A, Oner HF, Kocak N, Kaynak S. Tilt and decentration after primary and secondary transsclerally sutured posterior chamber intraocular lens implantation. J Cataract Refract Surg 2001; 27(2): 227-232.[114]
4. Resident, Department of
Ophthalmology, Ophthalmic Hospital & Regional Institute of Ophthalmology, Bangalore Medical College & Research Institute.
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Shashidhar S, Associate Professor,
Department of Ophthalmology,
Ophthalmic Hospital & Regional Institute of Ophthalmology, A. V. Road,
Opposite Central Police Station, Chamarajpete, Bangalore-560002, Karnataka, India.
E-mail: swamyshashidhar@gmail.com
Date of Submission: 31/07/2015. Date of Peer Review: 01/08/2015. Date of Acceptance: 02/08/2015. Date of Publishing: 06/08/2015.
AUTHORS:
1. Shashidhar S. 2. Suresh Babu G. 3. Shruthi Chandra 4. Manasa Penumetcha
PARTICULARS OF CONTRIBUTORS:
1. Associate Professor, Department of Ophthalmology, Ophthalmic Hospital & Regional Institute of Ophthalmology, Bangalore Medical College & Research Institute.
2. Associate Professor, Department of Ophthalmology, Ophthalmic Hospital & Regional Institute of Ophthalmology, Bangalore Medical College & Research Institute.
3. Resident, Department of