ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Case
report
Miliary
tuberculosis:
a
severe
opportunistic
infection
in
juvenile
systemic
lupus
erythematosus
patients
Priscilla
S.
Freire
a,
João
D.
Montoni
a,
Aline
S.M.
Ribeiro
a,
Heloísa
H.
Marques
b,
Thais
Mauad
c,
Clovis
A.
Silva
a,d,∗aPediatricRheumatologyUnit,InstitutodaCrianc¸a,SchoolofMedicine,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil bPediatricInfectiousDiseasesUnit,InstitutodaCrianc¸a,SchoolofMedicine,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil cDepartmentofPathology,SchoolofMedicine,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil
dDivisionofRheumatology,InstitutodaCrianc¸a,SchoolofMedicine,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received20December2013 Accepted14April2014
Availableonline28November2014
Keywords:
Tuberculosis Immunosuppressive Infection
Children
Systemiclupuserythematosus
a
b
s
t
r
a
c
t
Introduction:Oneofthemainissuesinjuvenilesystemiclupuserythematosus(JSLE)patients isinfection,suchastuberculosis(TB).Ofnote,SLEpatientsaresusceptibletopulmonaryand extrapulmonaryTB.However,toourknowledge,thiscontagiousdiseasewasrarelyreported inpediatriclupuspopulation,particularlydiffuseormiliaryTB.Therefore,fromJanuary1983 toDecember2011,5,635patientswerefollowed-upatourPediatricRheumatologyUnitand 285(5%)ofthemmettheAmericanCollegeofRheumatologyclassificationcriteriaforSLE.
Casereports:Four(1.4%)ofourJSLEpatientshaddisseminatedTBandweredescribedherein. Allofthemwerefemalegender,receivedBCGvaccinationanddidnothaveahistoryofTB householdcontact.ThemedianofcurrentageatTBdiagnosisandtheperiodbetweenJSLE andTBdiagnosiswere17yearsold(range14–20)and5.5years(range2–7),respectively.All patientsdevelopedmiliaryTBduringthecourseofthedisease.ThemedianofSLEDisease ActivityIndex2000(SLEDAI-2K)was4(2–16)andthepatientsweretreatedwith immuno-suppressiveagents (glucocorticoid,azathioprineand/orintravenouscyclophosphamide). TwoofthempresentedsepsisandTBdiagnosiswasonlyestablishedatautopsy,especially withlungs,centralnervoussystemandabdominalinvolvements.Anti-TBtherapy (isoni-azid,rifampicinandpyrazinamide)wasindicatedintheothertwoTBcases,howeverthey deceased.
Discussion:MiliaryTBisarareandsevereopportunistinfectioninpediatriclupus popula-tion.ThisstudyreinforcestheimportanceofroutinesearchesforTBinJSLEpatients.
©2014ElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthor.
E-mails:clovis.silva@icr.usp.br,clovisaasilva@gmail.com(C.A.Silva).
http://dx.doi.org/10.1016/j.rbre.2014.04.007
Tuberculose
miliar:
infecc¸ão
oportunista
grave
em
pacientes
com
lúpus
eritematoso
sistêmico
juvenil
Palavras-chave:
Tuberculose Imunossupressor Infecc¸ão Crianc¸as
Lúpuseritematososistêmico
r
e
s
u
m
o
Introduc¸ão: Umdosprincipaisproblemasnolúpuseritematososistêmicojuvenil(LESJ)é a infecc¸ão,comoatuberculose(TB).É importanteobservarquepacientescomLESsão suscetíveisàtuberculosepulmonareextrapulmonar.Noentanto,deacordocomoquese sabe,essadoenc¸acontagiosaéraramenterelatadanapopulac¸ãopediátricacomlúpus, par-ticularmenteaTBdifusaoumiliar.Dejaneirode1983adezembrode2011,5.635pacientes foramacompanhadosnaUnidadedeReumatologiaPediátrica;285deles(5%)preencheram oscritériosdeclassificac¸ãoparaLESdoAmericanCollegeofRheumatology.
Relatosdecaso:Quatro(1,4%)denossospacientescomLESJtinhamtuberculosedisseminada eforamdescritosnesteestudo.Todoseramdosexofeminino,receberamavacinaBCGe nãotinhamhistóriadecontatodomiciliarcomaTB.Amedianadaidadenomomento dodiagnósticodaTBeoperíodoentreosdiagnósticosdeLESetuberculoseforamde17 anos(variac¸ãode14a20)e5,5anos(variac¸ãodedoisasete),respectivamente.Todasas pacientesdesenvolveramtuberculosemiliarduranteocursodadoenc¸a.AmediananoSLE DiseaseActivityIndex2000(SLEDAI-2K)foide4(2a16)easpacientesforamtratadascom agentesimunossupressores(glicocorticoides,azatioprinae/ouciclofosfamidaintravenosa). Duasdelasapresentaramsepseeodiagnósticodetuberculosesófoideterminadona necrop-sia,comenvolvimentoespecialmentedospulmões,dosistemanervosocentraledoabdome. Aterapiaantituberculose(isoniazida,rifampicinaepirazinamida)foiindicadanosoutros doiscasosdeTB;porém,aspacientesforamaóbito.
Discussão: ATBmiliaréumainfecc¸ãooportunistararaegravenapopulac¸ãopediátricacom lúpus.Esteestudoreforc¸aaimportânciadepesquisasderotinaparaTBempacientescom LESJ.
©2014ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Infectionsareveryimportantissuesinjuvenilesystemiclupus erythematosus (JSLE) patients, such as tuberculosis (TB).1 Thisisanendemicchronicinfectiousdisease2 anditisthe
second cause of death due to contagious diseases in the
world.3
Ofnote, SLEpatientshaveanincreasedsusceptibility to pulmonaryandextrapulmonaryTB,4–8withapooroutcome.6 TBhasbeenespeciallydescribedinadultactiveSLEpatients receivingimmunosuppressiveagents,6andmaymimiclupus clinicalfindings.7Toourknowledge,thistransmissibledisease israrelyreportedinpediatriclupuspopulation,particularly diffuseormiliaryTB.4
Therefore, from January 1983 to December 2011, 5635
patients were followed-up at our service and 285 (5%) of
them met the American College of Rheumatology (ACR)9
classification criteria for SLE. Four (1.4%) of our JSLE
patients had diffuse TB. The TB diagnoses were
per-formedfrom1996to2009andtheseweredescribedherein.
This study was approved by the Local Ethics
Commit-tee of our University Hospital. The demographic data,
clinical manifestations, disease activity and disease
dam-age indexes, laboratory exams and therapeutic regimen
at miliary TB diagnosis in JSLE patients are described in
Table1.ThemedianofcurrentprednisonedoseatTB
diag-nosiswas30mg/day(15–60)(Table1).
Case
reports
Case1
A20-year-oldgirlwasdiagnosedwithSLEat17yearsand11 monthsbased onthe followingACR classificationcriteria:9 photosensitivity,ulcersoftheoralmucosa,arthritisinknees, psychosis, granular casts and immunologic tests: antinu-clearantibody(ANA)1:200,antidouble-strandedDNA(anti-ds DNA) 1:40 (normal cut-off <1:10) and anti-cardiolipin (ACL) IgM63MPL(normalcut-off <10).Intradermalreaction puri-fiedproteinderivative(PPD)testwas0mm.TheSLEDisease Activity Index 2000(SLEDAI-2K) was 22.10 She was treated with prednisone (60mg/day), chloroquine(250mg/day) and azathioprine (100mg/day). During the next two years, she received chloroquine(250mg/day). At the age of 20 years,
shewas onremissionand wasadmittedtothe emergency
departmentduetothreedaysofsevereacuteabdominalpain, feverandcutaneousvasculitis(tendernodulesinthehands).
Pneumoperitoneum was diagnosed and she was promptly
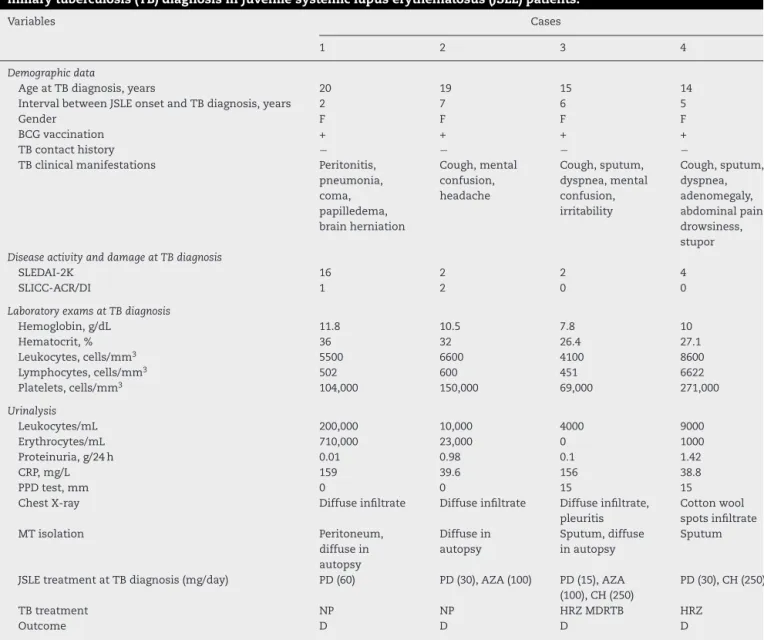
Table1–Demographicdata,clinicalmanifestations,diseaseactivity,diseasedamage,laboratoryexamsandtreatmentat
miliarytuberculosis(TB)diagnosisinjuvenilesystemiclupuserythematosus(JSLE)patients.
Variables Cases
1 2 3 4
Demographicdata
AgeatTBdiagnosis,years 20 19 15 14
IntervalbetweenJSLEonsetandTBdiagnosis,years 2 7 6 5
Gender F F F F
BCGvaccination + + + +
TBcontacthistory − − − −
TBclinicalmanifestations Peritonitis, pneumonia, coma, papilledema, brainherniation
Cough,mental confusion, headache
Cough,sputum, dyspnea,mental confusion, irritability
Cough,sputum, dyspnea, adenomegaly, abdominalpain, drowsiness, stupor
DiseaseactivityanddamageatTBdiagnosis
SLEDAI-2K 16 2 2 4
SLICC-ACR/DI 1 2 0 0
LaboratoryexamsatTBdiagnosis
Hemoglobin,g/dL 11.8 10.5 7.8 10
Hematocrit,% 36 32 26.4 27.1
Leukocytes,cells/mm3 5500 6600 4100 8600
Lymphocytes,cells/mm3 502 600 451 6622
Platelets,cells/mm3 104,000 150,000 69,000 271,000
Urinalysis
Leukocytes/mL 200,000 10,000 4000 9000
Erythrocytes/mL 710,000 23,000 0 1000
Proteinuria,g/24h 0.01 0.98 0.1 1.42
CRP,mg/L 159 39.6 156 38.8
PPDtest,mm 0 0 15 15
ChestX-ray Diffuseinfiltrate Diffuseinfiltrate Diffuseinfiltrate, pleuritis
Cottonwool spotsinfiltrate MTisolation Peritoneum,
diffusein autopsy
Diffusein autopsy
Sputum,diffuse inautopsy
Sputum
JSLEtreatmentatTBdiagnosis(mg/day) PD(60) PD(30),AZA(100) PD(15),AZA (100),CH(250)
PD(30),CH(250)
TBtreatment NP NP HRZMDRTB HRZ
Outcome D D D D
BCG,bacillusCalmette-Guérin;LAP,lymphadenopathy;CRP,C-reactiveprotein;NP,notperformed;MT,Mycobacteriumtuberculosis;-negative;+ positive;PPD,intradermalreactionpurifiedproteinderivative;H,isoniazid;R,rifampicin;Z,pyrazinamide;PD,prednisone;AZA,azathioprine; CH,chloroquinediphosphate;MDRTB,multi-drugresistantTB;S,survived;D,deceased.
10 µm
Fig.1–IsolationofMycobacteriumtuberculosisinlungs (case1).
Fig.2–Granulomatousinflamationandcaseousnecrosis
was1.Sixdayslater,shedevelopedpneumoniaandsepsisand wastreatedwithceftriaxoneandvancomycin.Aftertwodays, shehad coma(Glasgowstatus6) andbilateral papilledema
wasobserved. Urgentbraincomputed tomography
demon-stratedbrainherniationandshedeceased.Tendaysafterher death,theTBdiagnosiswasestablishedatautopsyfindings
demonstrated miliary TB with granulomatous inflamation
and caseousnecrosis with acid-fast bacillus, and isolation ofMycobacteriumtuberculosisinmeninges,lungs(Fig.1), peri-toneum, spleen (Fig. 2), ovary and fallopian tubes. TheM. tuberculosis was alsoisolated in cerebrospinal fluid culture (CSF)culture15 daysafterdeath.Other datarelatedtothe patientduringthetuberculosisperiodarepresentedinarein
Table1.
Case2
A19-year-oldgirlwasdiagnosedwithSLEat12years accord-ingtothefollowingACRclassificationcriteria:9 malarrash, mucosalulcers,pericarditis,proteinuria6.3g/24h,ANA(1:560, densefinespeckled pattern), anti-dsDNA (1:160)and
anti-Smantibodies.ThePPDtestwas0mmand SLEDAI-2Kwas
16.10Renalbiopsyshowedfocalproliferativelupusnephritis. Shewastreatedwiththreepulsesofintravenous methylpred-nisolone(1.0g/day),prednisone(60mg/day)andchloroquine (250mg/day)incombinationwithsevenmonthlyintravenous cyclophosphamide (IVCYC) (0.5–1.0g/m2/month) doses fol-lowed by every 3 months doses for a period of 2.5 years. Duringthe next 5years,shewas onremission. Attheage of19,shedevelopedvertebrallumbarfracture.Intradermal reactionpurifiedproteinderivative(PPD)testwas0mmand diffuse infiltrate in the chest X-ray (Table 1). SLEDAI-2K10 was12,SLICC/ACR-DI11 was2and shereceivedprednisone (30mg/day)and azathioprine100mg/day. At that moment, lumbardual-energy X-rayabsorptiometry (DXA) showed z
-score of −4 and she was treated with alendronate and
calcitonin.Neither fevernorweightlosswasreported. Two
2000 µm
Fig.3–Granulomatousinflamationandcaseousnecrosis inlungs(case2).
200 µm
Fig.4–Granulomatousinflamationandcaseousnecrosis inliver(case2).
weekslater,shepresentedwithintermittentmildcough, men-talconfusion,headacheanddevelopedacutepneumoniaand sepsis, and deceased after one week, despite broad spec-trum antibioticstherapy(ceftriaxoneandvancomycin).The TBdiagnosiswasestablishedatautopsyandrevealedacute pneumoniawithalveolarhemorrhage,miliaryTBwith gran-ulomatous inflammation,containingcaseousnecrosiswith isolationofM.tuberculosisinculturesoflungs(Fig.3),lymph nodes,spleenandliver(Fig.4).M.tuberculosiswasnotisolated inspine.
Case3
A15-year-oldgirlwasdiagnosedwithSLEat9years accord-ing tothe followingACR classificationcriteria:9 arthritisin knees,serositis(pleuritisandpericarditis),lymphopenia, pro-teinuria 1.1g/day,ANA(1:560, densefinespeckledpattern), anti-dsDNA(1:60),andACLIgG(45GPL)antibodies.ThePPD test was0mm. TheSLEDAI-2K10 was18,including nephri-tisdescriptors.Shewastreatedwithprednisone(60mg/day), azathioprine(150mg/day)andchloroquine(250mg/day). Dur-ing the next 6 years, the patient presented mild disease activity and atthe age of15, shehad cough, sputum and
dyspnea and chest X-ray showed diffuse lung infiltrates
withunilateralpleuritis.Atthatmomentshewasreceiving prednisone(15mg/day),azathioprine(100mg/day)and chloro-quine (250mg/day). No family history of TBwas reported. The TB diagnosis was established according to culture of
sputum with M. tuberculosis and PPD test of 15mm. The
SLEDAI-2K10 was 2 and SLICC/ACR-DI11 was 0. She was
treated with rifampicin, isoniazid and pirazinamide. One weeklater,shedevelopedabdominalpainandvomiting.The aspartateaminotransferase(AST)was939IU/L(normal5–26), alanineaminotransferase (ALT)215IU/L (normal19–44) and gamma-glutamyltranspeptidase(GGT)1582g/dL(10–22).Due tohepatotoxicity,theanti-TBtherapywassuspended. There-fore,anotherscreeningtestwasperformedandafter10days, sputumculture showedmulti-drugresistant M. tuberculosis
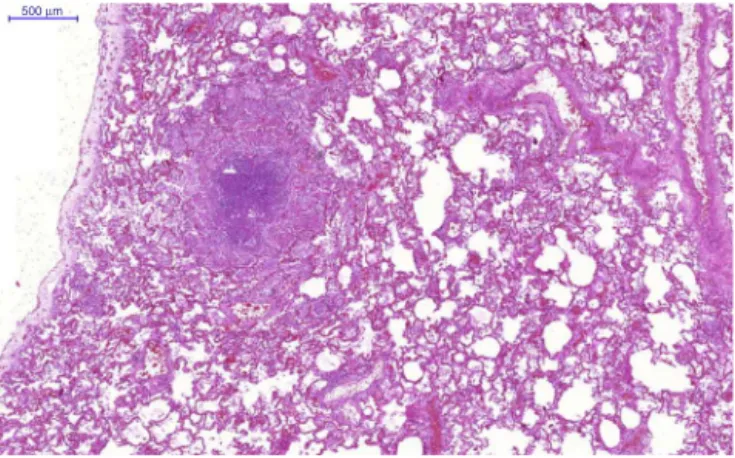
500 µm
Fig.5–Granulomatousinflamationandcaseousnecrosis inlungs(case3).
mentalconfusion,irritabilityanddeceased.Theautopsy
find-ingsshowed miliaryTBwithgranulomatous inflammation,
caseousnecrosisand isolationofM. tuberculosisincultures oflungs(Fig.5),spleen,liverandbonemarrow.
Case4
A14-year-oldgirlwasdiagnosedwithSLEat9yearsaccording tothefollowingACRclassificationcriteria:9arthritisinknees, mucosalulcers,hemolyticanemiaandlymphopenia, protein-uria1.5g/24h,granularurinarycasts,ANA(1:240),anti-dsDNA (1:160)antibodiesandlupusanticoagulant.ThePPDtestwas 0mm.TheSLEDAI-2K10was16,includingnephritis descrip-tors.Shewastreatedwithintravenousmethylprednisolone pulses (1.0g/day), prednisone (60mg/day) and chloroquine (250mg/day). Onemonth afterthis treatment, the protein-uriareducedandwedidnotperformrenalbiopsy.Duringthe next5years,thepatientremained moderatedisease activ-ity andatthe age of14,shehadcough, fever,diffuseand severeabdominalpain,sputumanddyspneawithcotton-wool spotsinfiltrateonchestX-ray,anddisseminatedadenomegaly. NofamilyhistoryofTBwasreported.Atthattimeshewas underprednisone(30mg/day)andchloroquine(250mg/day). TheTBdiagnosiswasestablishedaccordingtosputum cul-turewithMycobacteriumtuberculosis.SLEDAI-2K10was4and SLICC/ACR-DI11was0.Shewastreatedwithrifampicin, iso-niazidandpirazinamide.Despitetheanti-TBtreatment,one daylater,shedevelopeddrowsiness,stupor,severedyspnea andrespiratoryinsufficiency,requiringmechanicventilation. Fivedayslatershedied.Herparentsdidnotgivetheirconsent foranautopsyprocedure.
Discussion
Toourknowledge,thiswasthefirststudythatevaluated dis-seminatedTBinpediatricJSLEpopulation,andshowedthat miliary TBwas a rare and severe opportunist infection in patientsunderimmunosuppressivetherapy.Thesepatients werefollowed-upinonlyoneofthetertiaryPediatric Univer-sityHospitalsinalargecityofBrazil.
Importantly, our 285 JSLE patients received the bacil-lus Calmette-Guérin (BCG) vaccination at neonatal period, as indicated in all Brazilian newborn. Since this infection is prevalent in our country,2 these patients are routinely assessedfortuberculosisaccordingtoTBhouseholdcontact history, undergo PPDtestand chest X-raybefore
immuno-suppressive treatment. Our cases probably presented new
primary TBinfections, sincethe PPDtest was 0mm when
immunosuppressivetherapieswereperformed.
Tuberculosis is a contagious disease in which the defi-nitediagnosisrequirestheidentificationofM.tuberculosis,as confirmed inall ofour cases.Itisspread byexpectoration ofairbornedropletsofpeoplewithactivediseasewhichare inhaledandlodgedinthedistalairways.3Intrinsic immuno-logicalabnormalitiesinhumoralandcellularfunctionsmay contributetothisopportunisticinfectioninlupuspatients.1
The reactivation of remote infection can be triggered
due to an immune system abnormalities,2 and
immuno-suppressive disorders are considered risk factors for this disease,suchasHIVinfection,severemalnutrition2andSLE patients.4–8
ThiscontagiousdiseaseinadultSLEpatientsishabitually insidiousandcanrangefromlatentdiseaseandisolated respi-ratorysysteminvolvementtoextrapulmonarTB.4–7,12 Other sites affected inTBlupus patientsare the central nervous system,lymphaticorgans,peritoneum,12genitourinarytract, vertebralbodies,jointsandsofttissues.4,6,7Ofnote, tubercu-losis,particularlyinlungsandmeninges,wasrarelyreported inJSLEpatients,asobservedinourlupuspopulation.4,12
Moreover, disseminated or miliary TB, which involves
manyorganssimultaneously,3hasbeendescribedduringthe disease course,as observedherein. Theprevalenceof this severe diseaseoccurred in0%to15% ofadultSLEpatients suffering from TB.4–7 Diffuse TB may resemble sepsis, as evidencedinourcases,andmaybeunderestimatedinlupus populationduetothefactthatvariousrheumatologicservices donotperformnecropsysystematically.1
Theextra-pulmonaryTBmayalsoberelatedto immuno-suppressive drugs, especially glucocorticosteroid use,7 as observedinourpatients.Furthermore,JSLEclinical
manifes-tations may also mimicpulmonary and disseminated TB.1
Therefore,tuberculosisoughttobeinvestigatedinactivelupus patients.
Thetreatmentofthisinfectiousdiseaseincludesatleast three bactericidal drugs (isoniazid, rifampicin and pyrazi-namide), as administered in our adolescent patients. One limitationofthepresentstudywastheretrospectivedesign, whichincludedpatientsdiagnosedwithTBbefore2009and treated with these three medications. Currently, the first-line four-drugtherapyisrecommendedaccording toWorld Healthy Organization guidelines.13 In Brazil,we have been usingtheseguidelines,includingisoniazid,rifampicin, pyraz-inamideandethambutolinchildrenolderthan9yearsofage, since2010.14
However, despitetreatment, disseminated TBmay have
Thisstudy reinforcesthe importanceof screening with newtestsforTBdiagnosis,suchasQuantiFERON-TBGoldtest whichisanIFN-␥releaseassays,sincePPD,theclassicassay
for latent tuberculosis infection diagnose, has diminished accuracyinimmunosuppressedpatients.15Indeed,recently
astudyshowedthatQuantiFERON-TBGoldassayseemedto
beamoreaccuratetestforthedetectionoflatenttuberculosis infectioncomparedtoPPDtestinSLEpatientsthatreceived BCGvaccinationanddidnotreportTBcontacthistory.16
Inconclusion,miliaryTBisarareandsevereopportunist infectioninpediatriclupuspopulation.Thisstudyreinforces theimportanceofroutinesearchesforTBinJSLE patients, especiallywithlungs,centralnervoussystemandabdominal involvements.AmulticenterJSLEregistrystudytoevaluatethe riskfactorsassociatedwiththisimportantcontagiousdisease willbeperformedinBrazilianpopulationsufferingfromthis chronicdisease.
Conflict
of
interest
Theauthorsdeclarenoconflictofinterest.
r
e
f
e
r
e
n
c
e
s
1. FacoMM,LeoneC,CamposLM,FebrônioMV,MarquesHH,
SilvaCA.Riskfactorsassociatedwiththedeathofpatients
hospitalizedforjuvenilesystemiclupuserythematosus.Braz
JMedBiolRes.2007;40:993–1002.
2. Sant’AnnaCC,HijjarMA.RecentcontributionoftheWorld
HealthOrganizationtocontrolchildhoodtuberculosis.Rev
SaúdePública.2007;41:117–20.
3. FriedenTR,SterlingTR,MunsiffSS,WattCJ,DyeC.
Tuberculosis.Lancet.2003;362:887–99.
4. GhoshK,PatwardhanM,PradhanV.Mycobacterium
tuberculosisinfectionprecipitatesSLEinpatientsfrom
endemicareas.RheumatolInt.2009;29:1047–50.
5. PasotoSG,BorbaEF,BonfaE,ShinjoSK.Lupuspleuritis:a
relevantriskfactorforpulmonarytuberculosis.Lupus.
2010;19:1585–90.
6.SayarliogluM,InancM,KamaliS,CefleA,KaramanO,GulA,
etal.TuberculosisinTurkishpatientswithsystemiclupus
erythematosus:increasedfrequencyofextrapulmonary
localization.Lupus.2004;13:274–8.
7.HouCL,TsaiYC,ChenLC,HuangJL.Tuberculosisinfectionin
patientswithsystemiclupuserythematosus:pulmonaryand
extra-pulmonaryinfectioncompared.ClinRheumatol.
2008;27:557–63.
8.ErdozainJG,Ruiz-IrastorzaG,EgurbideMV,
Martinez-BerriotxoaA,AguirreC.Highriskoftuberculosisin
systemiclupuserythematosus?Lupus.2006;15:232–5.
9.HochbergMC.UpdatingtheAmericanCollegeof
Rheumatologyrevisedcriteriafortheclassificationof
systemiclupuserythematosus.ArthritisRheum.
1997;40:1725.
10.GladmanDD,Iba ˜nezD,UrowitzMB.Systemiclupus
erythematosusdiseaseactivityindex2000.JRheumatol.
2002;29:288–91.
11.GladmanD,GinzlerE,GoldsmithC,FortinP,LiangM,Urowitz
M,etal.Thedevelopmentandinitialvalidationofthe
SystemicLupusInternationalCollaboratingClinics/American
CollegeofRheumatologydamageindexforsystemiclupus
erythematosus.ArthritisRheum.1996;39:363–9.
12.KimJM,KimKJ,YoonHS,KwokSK,JuJH,ParkKS,etal.
MeningitisinKoreanpatientswithsystemiclupus
erythematosus:analysisofdemographics,clinicalfeatures
andoutcomes;experiencefromaffiliatedhospitalsofthe
CatholicUniversityofKorea.Lupus.2011;20:531–6.
13.WorldHealthOrganization.Treatmentoftuberculosis
guidelines;2009.Reportno.:WHO/HTM/TB/2009/420.ISBN:
9789241547833.
14.Manualderecomendac¸õesparacontroledatuberculoseno Brasil.SecretariadeVigilânciaemSaúde/MS.
http://portal.saude.gov.br/portal/arquivos/pdf/manualde
recomendacoestb.pdf
15.Redelman-SidiG,SepkowitzKA.Interferongammarelease
assaysinthediagnosisoflatenttuberculosisinfectionamong
immunocompromisedadults.AmJRespirCritCareMed.
2013;188:422–31.
16.YilmazN,ZehraAydinS,InancN,KarakurtS,DireskeneliH,
YavuzS.ComparisonofQuantiFeron-TBGoldtestand
tuberculinskintestfortheidentificationoflatent