www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
The
importance
of
clinical
monitoring
for
compliance
with
Continuous
Positive
Airway
Pressure
夽
Lucas
B.
Pelosi
a,
Mariana
L.C.
Silveira
b,
Alan
L.
Eckeli
c,
Emilia
M.P.C.
Chayamiti
b,d,
Leila
A.
Almeida
c,
Heidi
H.
Sander
c,
Daniel
S.
Küpper
b,
Fabiana
C.P.
Valera
b,∗aUniversidadedeSãoPaulo(USP),FaculdadedeMedicinadeRibeirãoPreto,RibeirãoPreto,SP,Brazil bUniversidadedeSãoPaulo(USP),FaculdadedeMedicinadeRibeirãoPreto,DepartamentodeOftalmologia, OtorrinolaringologiaeCirurgiadeCabec¸aePescoc¸o,RibeirãoPreto,SP,Brazil
cUniversidadedeSãoPaulo(USP),FaculdadedeMedicinadeRibeirãoPreto,DivisãodeNeurologia,RibeirãoPreto,SP,Brazil dSecretariaMunicipaldaSaúdedeRibeirãoPreto,RibeirãoPreto,SP,Brazil
Received3February2016;accepted23May2016 Availableonline14July2016
KEYWORDS
CPAP; OSAS; Apnea; Compliance; Positivepressure device;
Obstructivesleep apnea
Abstract
Introduction:Obstructivesleepapneasyndromeiscurrentlyapublichealthproblemofgreat importance.Whenmisdiagnosedorimproperlytreated,itcanleadtoseriousconsequenceson patients’ quality oflife. Thegold standardtreatment for cases ofobstructive sleepapnea syndrome, especially inmild to severe and symptomatic cases, is continuous positive air-waypressuretherapy.Compliancewithcontinuouspositiveairwaypressuretherapyisdirectly dependentontheactiveparticipationofthepatient,whichcanbeinfluencedbyseveralfactors.
Objective: Theobjectiveofthisstudyistodescribethefactorsrelated tocompliancewith continuouspositiveairwaypressuretherapy,andtoanalyzewhichassociatedfactorsdirectly influencetheefficiencyofthetreatment.
Methods:Patientswhoreceivedcontinuouspositiveairwaypressuretherapythroughthe Munic-ipalHealthDepartmentofthecityofRibeirãoPretowererecruited.Astructuredquestionnaire wasadministeredtothepatients.Compliancewithcontinuouspositiveairwaypressuretherapy wasassessedbyaveragehoursofcontinuouspositiveairwaypressuretherapyusagepernight. Patients with good compliance (patients using continuous positive airway pressure therapy ≥4h/night)werecomparedtothosewithpoorcompliance(patientsusing<4h/night).
Results:138patientswereanalyzed:77(55.8%)wereconsideredcompliantwhile61(44.2%) werenon-compliant.Thecomparisonbetweenthetwogroupsshowedthatregularmonitoring by aspecialist considerably improved compliancewith continuous positive airwaypressure therapy(oddsratio,OR=2.62).
夽 Pleasecitethisarticleas:PelosiLB,SilveiraML,EckeliAL,ChayamitiEM,AlmeidaLA,SanderHH,etal.Theimportanceofclinical monitoringforcompliancewithContinuousPositiveAirwayPressure.BrazJOtorhinolaryngol.2017;83:439---44.
∗Correspondingauthor.
E-mails:facpvalera@uol.com.br,facpvalera@fmrp.usp.br(F.C.Valera).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.05.013
Conclusion:Compliancewithcontinuouspositiveairwaypressuretherapyisrelatedto educa-tionalcomponents,whichcanbeenhancedwithcontinuousandindividualizedcaretopatients withobstructivesleepapneasyndrome.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE
CPAP; SAOS; Apneia; Adesão;
Aparelhodepressão positiva;
Apneiaobstrutivado sono
AimportânciadoseguimentoclínicoparaadesãoaoCPAP
Resumo
Introduc¸ão:Síndrome daapneiaobstrutiva do sono(SAOS)é,atualmente, um problemade saúdepúblicadesumaimportância.Quandomaldiagnosticadooutratadoinadequadamente, podelevarasériasconsequênciasnaqualidadedevidadopaciente.Otratamentopadrãoouro para casosde SAOS,principalmente noscasosmoderados agrave esintomáticos, éoCPAP (ContinuousPositiveAirwayPressure).AadesãoaoCPAPdependediretamentedaparticipac¸ão ativadopaciente,quepodeserinfluenciadaporváriosfatores.
Objetivo:Oobjetivo deste estudoé descreveros fatores relacionadosàadesão ao CPAP,e analisarquaisfatoresassociadosinfluenciamdiretamentenaeficiênciadotratamento.
Método: ForamrecrutadospacientesquereceberamCPAPpelaSecretariaMunicipaldeSaúde deRibeirãoPreto.Umquestionárioestruturadofoiaplicadoaopaciente.AadesãoaoCPAPfoi avaliadapelamédiadehorasdeusodoCPAPpornoite.Pacientescomboaadesão(pacientes emusodeCPAP≥4horas/noite)foramcomparadosaoscommáadesão(pacientesemuso<4 horas/noite).
Resultados: Noestudo,138pacientesforamanalisados:77(55,8%)foramconsiderados ader-entese61(44,2%)foramnãoaderentes.Acomparac¸ãoentreosdoisgruposdemonstrouque oseguimentoregularcomespecialistamelhorouconsideravelmenteaadesãoao CPAP(Odds Ratio,OR=2,62).
Conclusão:A adesãoao CPAPestárelacionadaacomponentes educacionais,quepodem ser aprimoradoscomassistênciacontínuaeindividualizadaaopacientecomSAOS.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
TheObstructiveSleepApneaSyndrome(OSAS)isnow con-sideredamajorpublichealthproblem,withaprevalence, respectively,of4%and2%inmalesandfemales.1Inarecent
epidemiologicalstudy conducted inthe city of SãoPaulo, theprevalenceofOSASamongadultswas32.8%.2In
undiag-nosedoruntreatedcases,OSAScanleadtosignificantand permanentimpactonthequalityoflifeofpatients,reducing overallcognitivefunction.3Inaddition,OSASisrelatedtoa
highrateofmorbidityandmortality,andisassociatedwith diseasessuchassystemichypertension,4acutemyocardial
infarctionandischemicstroke.
ThepathophysiologyofOSASinvolvestheupperairways during sleep. The main associated factors are anatomic obstructive factors (such as adenotonsillar hypertrophy, base oftongue hypertrophy and neckmasses), neuromus-cularchanges,fatdistributioninthecervicalregion,5oran
associationoftheseconditions.
The gold standard treatment for OSAS, especially in mild to severe and symptomatic cases, is CPAP (Continu-ousPositiveAirwayPressure).6CPAPisanon-invasive,7easy
to use and highly effective treatment. When well suited tothis treatment,the compliantpatientshows significant
improvement inqualityof life,withreductionof daytime sleepiness and8 reduction of cardiovascular risk.8,9
How-ever, this benefit does not occur if the patient does not adhere to treatment. Thus, compliance with treatment is an important negative impasse in the management of OSAS, and directly depends on the involvement of the patient.7
Accordingtothe literature,several characteristics can influence compliancewithCPAP: other healthproblems in addition to OSA, the availability of polysomnography to titratethepressuretobeideallyusedinCPAPand psychoso-cialandeconomicfactors.10
Afew yearsago,anagreementbetweentheSecretaria deSaúdedeRibeirãoPretoandtheHospitaldasClínicasda Faculdade deMedicinadeRibeirãoPreto(HCFMRP)--- Uni-versidade de São Paulo optimized access to CPAP among citizens. Once theequipmenthadbeen prescribedby the specialist, the Health Department provided the CPAP to patients free of charge. Thus, the economic problem, a particularlyimportantobstacleindevelopingcountries,has beeneliminated.11
Methods
Patients whoreceived CPAP from Secretaria Municipal de RibeirãoPretowereinvitedtoparticipateinthestudy.They wereinstructedtoattendtheAmbulatóriodosDistúrbiosdo SonodoHCFMRP,bringingCPAPequipmentwiththem.
Participants who attended the invitation responded to apre-establishedquestionnaireaddressingage,associated diseases such as depression, systemic arterial hyperten-sion (SAH), diabetes, hypothyroidism, acute myocardial infarction(AMI),ischemicstroke(stroke),asthmaand gas-troesophagealreflux(GERD),smoking,drinking,anddrugsin use.ThehistoricaltimeofdiagnosisofOSASandCPAPuse (inyears)wasrecorded,aswellaswhetherthepatientwas usingnasalor facemask.Finally,whetherthepatientwas followedupinpublicorprivatehealthservicewasrecorded. Inaddition,patientswereaskedaboutwhattheyknew abouttheirdisease(OSAS),throughtwoquestions:(a)‘‘Do youknowwhatdiseaseyouhavethatistreatedwithCPAP?’’; (b)‘‘Doyouknowwhatpossiblecomplicationsoccurifthe OSASisnottreatedproperly?’’. Thedegreeofsatisfaction withtreatmentwasapproachedbythequestion:‘‘How sat-isfiedareyouwithyourtreatment?’’Daytimesleepinesswas evaluatedbytheEpworthSleepinessScale(ESS).12,13
The patients were then submitted to the general and ENTphysicalexamination.Thefollowingcomponentswere recorded: body mass index (BMI), neck circumference, rhinoscopy (with observationsof any septaldeviation and characteristics of the nasal conchae) and oroscopy (with gradingoftonsils,palateandtongue,respectively,by Brod-sky,MallampatiandFriedmanClassifications).14Theresults
of diagnostic polysomnography were also recorded, when available.
Compliance withCPAP wasdetermined byaveragingof hoursofusepernight,identifiedonthehourmeterinthe equipment. On the equipment that already provided the average per night,this informationwasrecorded. On the equipmentthat hadonly theinformationof hoursof use, thenumberwasrecordedandthepatientappearedinanew return,onaverageonetotwomonthsafterthefirstvisit, foranewrecordofthehourmeterandcalculationof aver-ageper night.Additionally, thepressure usedin theCPAP (cm/H2O)wasrecorded.
Patientsweredividedintotwogroups:Group1---patients withgoodcompliancewithCPAP(meanCPAP use >4h per night); and Group 2 --- thosewith inadequate compliance (mean CPAP use <4h per night).15 After identifying the
factthatthepatientwasnotin properuseofequipment, patients in Group 2 receivedguidance onthe importance ofitsoptimaluse,andthosewithnomonitoringweretold toreturntotheinstitution/clinicwheretheequipmentwas provided.Patientswithincompletedatawereexcluded.
Thecomparisonbetweenthetwogroupswasperformed throughthefollowingtests:
--- Fisher’s exact test to compare frequency data such as: gender, associated diseases, type of service where he/she was being monitored (public or private), type of mask usedand informationonknowledge or clinical monitoring;
--- UnpairedStudent’sttestwasusedtocomparethedata: age, hours of use of CPAP, Apnea and Hypopnea Index
(AHI),BMI,ESSandyearsofdiagnosis ofOSA anduseof CPAP.
Finally,thenumberofhoursofuseofCPAPwascorrelated withtheparametersofBMI,age,AHI,pressureusedinCPAP andESS.Forthispurpose,Pearsoncorrelationtestwasused. Forallstatisticalanalyzes,thedifferenceswereconsidered significantatp<0.05.
The projectwasapprovedby thelocalEthicsResearch Committeewithnumber06340012.0.0000.5440.
Results
Onehundredandeightypatientsattendedtheconsultation; ofthese,for75patientsasinglevisitwasenoughtogetthe averageofhoursofCPAPuse;fortheother105patients,the secondconsultation wasnecessary toobtain this informa-tion.Ofthese,42wereexcludedbecausetheydidnotattend areturnvisit.Thus,138patientscompletedallphasesofthe study,including63(45.6%)womenand75(54.4%)men.The meanage(±standarddeviation)was58.20±11.02yearsand themeanBMI(±standarddeviation)33.19±6.20kg/m2.
AHIdatawasobtainedfrom83patients,withthemean valuebeing45.52±26.56. Twenty-sevenof thesepatients hadmoderateOSAandcomorbidities,while56hadsevere OSA.Overall, theassociateddiseases werepresent atthe following frequencies: hypertension in 87 patients; DM in 39;depressionin31;hypothyroidismin18;asthmain13;and GERDin19patients.Fivepatientshadahistoryofprevious myocardialinfarction or stroke. Thirty-seven wereor had beensmokers,while13hadalcoholabusehistory.
In general, the percentage of patients receiving CPAP andwhohadcomplianceconsidered adequate was55.8%. Seventy-sevenpatients formed Group 1 (goodcompliance withCPAP)and61Group2(poorcompliancewithCPAP).The averagehoursofCPAPuseinGroup1was6.13±0.15h,and inGroup2of1.05±0.17h.Themeandifferenceamongthe groupswas5h,whichwassignificantlystatistic(p<0.0001, 95%CI4.63---5.53).
Thecomparisonofdemographicsbetweenthetwogroups was not significant, either for age, BMI or AHI diagnosis (Table 1). In83 patients whohadinformationof AHI, the correlation between AHI and the number of hours of use wasnotsignificant(r=0.18;95%CI−0.03to0.38;p=0.09). There was also no significant difference between the groups for gender, presence of hypertension, DM, depression,hypothyroidism,myocardialinfarction,stroke, asthma,andGERD, andthehabitsofsmokingandalcohol
Table 1 Comparison of demographic data between
patientsinGroup1(goodadherencetoCPAP)andofGroup 2(pooradherencetoCPAP),throughStudent’sttest.
Parameter (average±SD)
Group1 Group2 p
Age 57.84±1.36 58.67±1.28 0.65
BMI 32.88±0.66 33.48±0.89 0.59
AHIatdiagnosis 47.6±4.10 40.52±3.92 0.21
Table2 Comparison ofdemographic dataandfrequency ofassociateddiseasesbetweenGroup1(patientswithgood adherencetoCPAP)andGroup2(patientswithpoor adher-encetoCPAP),throughFisher’sexacttest.
Parameter Group1(%) Group2(%) p
Gender 54.5 45.9 NS
SH 62.3 63.9 NS
DM 29.8 26.2 NS
Depression 18.2 27.4 NS
Hypothyroidism 14.3 11.4 NS
PreviousAMI/stroke 2.6 4.9 NS
Asthma 9.0 9.8 NS
GERD 9.0 9.8 NS
Smoking 24.6 29.5 NS
Alcoholabuse 10.3 8.2 NS
SH,systemichypertension;DM,diabetesmellitus; AMI,acute miocardialinfarction;GERD,gastroesophagealrefluxdisease.
consumption(Table2).Althoughtherewasnodifferencein prevalence between the groups, patients withdepression use significantly fewer hours of CPAP than those without depression(4.05±0.27vs.2.24±0.33;p<0.0001).The dif-ferencepersistsbeingnotsignificantforotherdiseases.
Knowledge of the disease, its implications and possi-blecomplicationswerestatisticallydifferentbetweenthe groups.AmongpatientsinGroup1,56of77(72.7%)showed adequateknowledgeofOSAS,whileonly34of61(55.7%)in Group2 mentionedit (p<0.05;95%CI0.99---2.03). Having adequate knowledge about the disease increased compli-ancewithCPAP,withoddsratio(OR)of1.42.
Complaints about adherence were reported by 44 of the 61 patients in Group 2 and 38 of the 77 patients in Group1(p<0.01;95%CI0.49---0.89).AlthoughCPAPmedium pressure was not significantly different between groups (meanCPAPpressureof8.95±0.34cm/H2OforGroup1vs. 9.46±0.27cm/H2OforGroup2,p=0.25;95%CI0.36---1.38), thenumberofhoursofCPAPuseispositivelycorrelatedto itsaveragepressure(r=0.04;p<0.05),suggestingthatthe higherthepressure,themorecompliantthepatientwillbe withtreatment(Fig.1).
The time of diagnosis and CPAP use did not influence compliance:patientsfromGroup1hadadiagnosisofOSAS
CP
AP pressure (cm H
2
O)
Average use of CPAP (hours) 20
15
10
5
0
0 2 4 6 8 10
r<0.05 r=0.04
Figure1 Correlation between the averagehours ofuse of CPAPandCPAPpressureused inthepatients analyzed.Study withPearson’slinearregression.
Epw
or
th Sleepiness Scale
Average use of CPAP (hours) r=–0.19
p<0.05 30
20
10
0
0 2 4 6 8 10
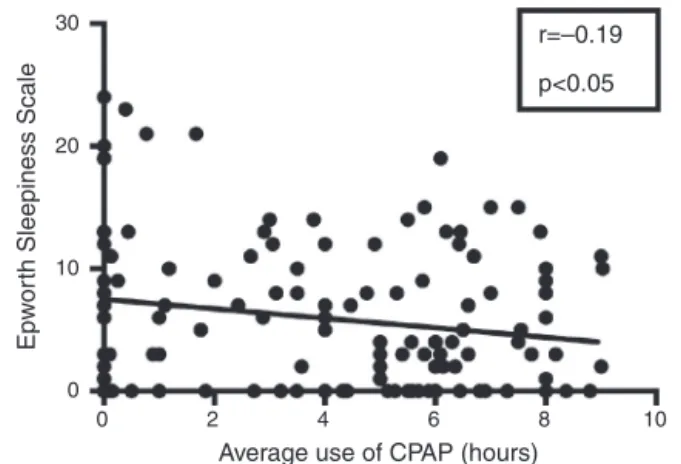
Figure2 CorrelationbetweenaveragehoursofCPAPuseand EpworthSleepinessScaleonpatientsanalyzed.Studywith Pear-son’slinearregression.
foraperiodof3.56±0.32years,whilethosefromGroup2 werediagnosed3.53±0.29years(p=0.94)before.Patients from group 1 received CPAP and were using it for an averageof2.90±0.21yearscomparedto2.91±0.24years forGroup2(p=0.99).
Regular monitoring (at least every 6 months) was reported by 64 of 77 (83.1%) patients of Group 1, com-paredwith26of 61(42.6%)in group2(p<0.0001; 95%CI 1.62---4.25).Regularfollow-upwithaspecialistwasrelated to greater compliance with CPAP, with OR=2.62. This is especially important when one considers that the groups wereinCPAPtreatmentforthesameperiodoftime.
Thecompliancerateamongpatientswhowerereferred bythePrivateMedicalServicewas51.3%andinthePublic Service was60.6%. In this region, there is only one pub-licservicetofollowthesepatientsthatofferstherapywith multidisciplinaryapproach(involvingotolaryngologists, neu-rologists,pulmonologists,physiotherapists,nutritionistsand speechtherapists).This couldexplainthebetter resultin thePublicService.Importantly,thisdifferencewasnot sta-tisticallysignificant.
The average Epworth Sleepiness Scale (ESS) was sig-nificantly lower in Group 1 (4.74±0.57) than in Group 2 (7.56±0.86)(p<0.01;95%CI−4.86to−0.75).Anegative correlationbetweentheaveragehoursofCPAPusepernight andESSwasobserved(r=−0.19;p<0.05)(Fig.2).This infor-mationconfirmsthatthemorethepatientusesCPAPduring thenight,thelesshe/shewillpresentdaytimesleepiness.
The type of mask wasnot related to compliancewith CPAP (p=0.161, 95% CI0.41 to−1.18).Importantly, most patients usednasalmasks(88.3% inGroup 1 and78.7% in Group2),whichgreatlyimpairedthestatisticalcomparison betweenthesetwogroups.
Amongthe138patients,onewasusingBiPAP(with aver-age usage of 0h/night),4 on use of auto CPAP (with use averageof0.27±0.48),54onuseofCPAPwithexpiratory relief (use average of 4.38±0.36) and 79 in use of basic CPAP(useaverageof3.78±0.33).Thecomparisonbetween thelattertwomodesof CPAP(expiratoryreliefandbasic) wasnotsignificant(p=0.22;95%CI−1.57to0.36).
Discussion
Among the different therapeutic modalities for OSA, the positiveimpactofCPAPisclearlyestablished,bothforthe improvementin qualityoflife andthepositive effectson morbidityandmortalityrates.16Patientsundergoing
treat-ment have healthier and more productive lives and are lessexposedtocardiovascularrisksandaccidents.However, CPAPefficiencyinimprovingsleeparchitectureandreducing daytimedrowsinessisstronglyinfluencedbypatient compli-ance.
In studiesthat havedefinedadequate compliancewith the use of CPAP as at least 4h a night, compliance rate ranged from29% to83%.17 Consequently, the main
obsta-clesinCPAPtreatmentaredirectlyrelatedtothisfactor.In arecentstudy,18 itwasshownthattherateofcompliance
withCPAP,usingthesesamecriteriaof thepresent study, wasaround65%amongpatientsinactivefollow-up,avalue greaterthanthatobservedinthecurrentstudy.
The positiveimpactofCPAP inreducingsleepinesswas confirmedinthisstudybysignificantlyhighervaluesinESSin maladaptivepatients.Furthermore,therewasasignificant inversecorrelationbetweenthehoursofCPAPusebynight andESS,thatis,areductionof somnolence.These results corroboratethosedescribedbyPateletal.19who,ina
meta-analysis,showedthat,comparedtoplacebo,thetreatment groupswereabletoreduceESS,onaverage,2.9points.
Inourcohort,patientswithdepressionhadlowerrates of hours of use than patients without depression. This resultwasalsosuggested byLawetal.20 Norelationwith
complianceratewasevidentforotherassociateddiseases. Importantly,exceptforsystemichypertension,other comor-bidities were not common, which makes the statistical analysislessreliable.
Itiswell establishedthatthediagnosisof OSASismost frequentinobese,maleandolderindividuals.21Ontheother
hand,itisimportanttoidentifywhichfactorsareassociated withcompliance withCPAP treatment, and which patient groups have higher risk of quitting therapy. This informa-tion is essential for programming specific approaches to improvetheefficiencyoftherapywithCPAP.After evaluat-ing4281patients,Woehrleetal.22reportedthatcompliance
withCPAP is higher in older and male patients, and con-cluded thatthe age andgender influence the compliance withtreatment,althoughtheydidnotconsiderthesedata clinicallyrelevant.Moreover,Budhirajaetal.23andQueiroz
et al.18 observed no influence of gender on treatment
compliance. In this study, age and gender are not statis-tically correlated to the compliance rate. Regarding BMI, in contrast with what Shapiro et al. mentioned,24 there
was no relationship of this parameter with compliance rate.
There are no studies directly correlating the compli-anceratetoMallampatiScale.Zonatoetal.25demonstrated
a positive correlation between Mallampati Scale andAHI. Queirozetal.18reportedthatahigherAHIatdiagnosiswas
associatedwithhighercompliancerate,probablybecause the most severe OSAS patients are more symptomatic or moreconcernedwiththeimpactofOSAS.Althoughthis asso-ciationwasnotobservedinthepresentstudy,wefound a direct(butoflowintensity)correlationbetweentheCPAP
pressureusedby thepatient, andthe average numberof hoursof use. This correlation suggests that patients with severe obstructive factors are more compliant with CPAP treatment.
Additionally, thetype ofmask (nasal or facial) didnot affect adherence in this cohort; this statistical analysis, however,wasimpairedsincemostofthepatientsusednasal masks.We also did not have any statistical difference of hoursofuseamongpatientswhousebasicCPAPorCPAPwith Expiratoryrelief.These resultsareinline withthose pre-sentedbyBakkeretal.26andKushidaetal.,27butcontradict
thefindingsofChiharaetal.28
Accordingtotheresultsofthisstudy,awarenessofOSAS anditsimplicationsseemstoplayakeyroleincompliance with CPAP. This information is important as it stimulates the need to develop strategies to improve patients’ per-ceptionof theirdisease througheducationalprogramsfor thispopulation.LaPiana etal.29 showedthat educational
programssignificantlyincreasecompliancewithCPAP, espe-ciallyduringthefirstyear.Afterthisperiod,theratetends todecrease.
This study suggests that regular and multidisciplinary monitoring after diagnosis and initiation of therapy sig-nificantly increases the chances of compliance success, probablybyfacilitatingmeasurespresentedtopatients,and becausetemporaryproblemscouldbemoreeasilyresolved whenreadilyidentifiedandproperlyaddressed.
Considering the type of health system in which the patientwasinserted(Publicor Private),therewasno sig-nificantdifference,althoughitisknownthatthereislower complianceamongpatientsoflowersocioeconomicstatus.10
This finding may be explainedby the program developed through the Agreement between HCFMRP and Secretaria MunicipaldeSaúdedeRibeirãoPreto,whichincludesregular monitoringofOSAS patientsina multidisciplinary special-izedsetting.
This is a cross-sectional cohort that did not analyze patients either prospectively or randomly. This made the analysisof some parameterssuch asthe use of the mask not supportable. However, important information can be obtainedfrom thisstudy, in particularon the importance ofcontinuousandsystematicfollow-upofpatientswhoare usingCPAP.
Conclusion
Thefindingsofthisstudystronglysupporteducationaland motivationalcomponentsinfluencingcompliancewithCPAP. Theseaspectscanbeachievedby individualizedand mul-tidisciplinary patient care. The importance of active and regularmonitoringofCPAPuserswasdemonstrated,andit issuggestedthatthe interdisciplinaryapproachfacilitates theidentification of the difficulties facedby the patient. Thiscontinuous approachseemsto considerablyfacilitate compliancewithCPAP.
Conflicts
of
interest
References
1.YoungT,PaltaM,DempseyJ,SkatrudJ,WeberS,BadrS.The occurrenceofsleep-disordered breathingamongmiddle-aged adults.NEnglJMed.1993;328:1230---5.
2.Tufik S,Santos-SilvaR, Taddei JA,Bittencourt LRA. Obstruc-tivesleepapneasyndromeintheSaoPauloEpidemiologicSleep Study.SleepMed.2010;11:441---6.
3.McDaid C,DuréeKH, GriffinSC, Weatherly HL,StradlingJR, Davies RJ, etal. A systematicreview ofcontinuouspositive airway pressureforobstructive sleepapnoea-hypopnoea syn-drome.SleepMedRev.2009;13:427---36.
4.Durán-Cantolla J, Aizpurv F, Martinez-Null C, Barbé-Illa F. Obstructivesleepapnea/hypopnoeaa systemichypertension. SleepMedRev.2009;13:323---31.
5.OlszewskaE,SieskiewiczA,RozyckiJ,RogalewskiM,TarasowE, RogowskiM,etal.Acomparisonofcephalometricanalysisusing radiographsandcraniofacialcomputedtomographyinpatients withobstructivesleepapneasyndrome:preliminaryreport.Eur ArchOtorhinolaryngol.2009;266:535---42.
6.Sullivan CE, Issa FG, Bertron-Jones M, Eves L. Reversal of obstructivesleepapneabycontinuouspositiveairwaypressure appliedtroughthenares.Lancet.1981;18:862---5.
7.AvlonitovE,KapsimalisF,VarouchakisGM,VardavasCI,Behrakis P. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients.SleepBreath.2012;16:563---9.
8.Capodanno D, Milazzo G, Cumbo M, Marchese A, Salemi A, QuartaroneL,etal.Positiveairwaypressureinpatientswith coronaryarterydiseaseandobstructivesleepapneasyndrome. JCardiovascMed.2014;15:402---6.
9.PanoutsopoulosA,KallianosA,KostopoulosK,SeretisC, Koufo-giorga E, Protogerou A, et al. Effect of CPAP treatmenton endothelial function and plasmaCRP levelsin patients with sleepapnea.MedSciMonit.2012;18:CR747---51.
10.SawyerAM,GooneratneNS,MarcusCL,OferD,RichardsKC, WeaverTE.AsystematicreviewofCPAPadherenceacrossage groups:clinicalandempiricinsightsfordevelopingCPAP adher-enceintervention.SleepMedRev.2011;15:343---56.
11.EpsteinLJ,KristoD,StrolloPJ,FriedmanN,MalhotraA,PatilSP, etal.Clinicalguidelineforevaluation,managementand long-termcareofobstructivesleepapneainadults.JClinSleepMed. 2009;15:263---76.
12.YiH,JohnsMW.Anewmethodformeasuringdaytime sleepi-ness:theEpworthsleepinessscale.Sleep.1991;14:540---5.
13.YiH,ShinK,KimJ,KimJ,LeeJ,ShinC.ValidityandReliability ofSleepQualityScaleinsubjectswithobstructivesleepapnea syndrome.JPsychosomRes.2009;66:85---8.
14.LiistroG,RombauxP,BelgeC,Dury M,AubertG, Rodenstein DO. HighMallampati score and nasal obstructionare associ-ated riskfactors for obstructive sleepapnoea. EurRespirJ. 2003;21:248---52.
15.GayP,WeaverT,LoubeD,IberC,PositiveAirwayPressureTask Force,Standards ofPracticeCommittee,etal.Evaluationof
positiveairwaypressuretreatmentforsleeprelatedbreathing disordersinadults.Sleep.2006;29:381---401.
16.AnticNA, CatchesideP,BuchanC,HensleyM, NaughtonMT, Rowland S, et al. The effect of CPAP in normalizing day-timesleepiness,quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34: 111---9.
17.WeaverTE,GrunsteinRR.Adherencetocontinuouspositive air-waypressure therapy:thechallenge toeffective treatment. ProcAmThorSoc.2008;5:173---8.
18.QueirozDL,YuiMS,BragaAA,CoelhoML,KüpperDS,SanderHH, etal.Adherenceofobstructivesleepapneasyndromepatients tocontinuouspositiveairwaypressureinapublicservice.Braz JOtorhinolaryngol.2014;80:126---30.
19.PatelSR,WhiteDP,MalhotraA,StanchinaML,AyasNT. Contin-uouspositiveairwaypressuretherapyfortreatingsleepinessin adiversepopulationwithobstructivesleepapnea:resultsofa meta-analysis.ArchInternMed.2003;163:565---71.
20.LawM,NaughtonM,HoS,RoebuckT,DabscheckE.Depression mayreduceadherenceduringCPAPtitrationtrial.JClinSleep Med.2014;10:163---9.
21.WinakurSJ,SmithPL,Schwartz AR.Pathophysiologyand risk factorsforobstructivesleepapnea.SeminRespirCritCareMed. 1998;19:99---112.
22.WoehrleH,GramlA,WeinreichG.Age-andgender-dependent adherencewithcontinuous positiveairway pressure therapy. SleepMed.2011;12:1034---6.
23.BudhirajaR,ParthasarathyS,DrakeCL,RothT,ShariefI, Bud-hirajaP,etal.EarlyCPAPuseidentifiessubsequentadherence toCPAPtherapy.Sleep.2007;30:320---4.
24.ShapiroGK,ShapiroCM.FactorsthatinfluenceCPAPadherence: anoverview.SleepBreath.2010;14:323---35.
25.Zonato AI, Bittencourt LR, Martinho FL, Júnior JF, Gregório LC,TufikS.Associationofsystematicheadandneckphysical examinationwithseverityofobstructivesleepapnea-hypopnea syndrome.Laryngoscope.2003;113:973---80.
26.BakkerJ,CampbellA,NeillA.Randomizedcontrolledtrial com-paringflexibleandcontinuouspositiveairwaypressuredelivery: effectsoncompliance,objectiveandsubjectivesleepinessand vigilance.Sleep.2010;33:523---9.
27.Kushida CA, Berry RB, Blau A, Carbtree T, Fietze I, Kryger MH,et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titrationprocessonefficacy,adherenceandoutcomes.Sleep. 2011;34:1083---92.
28.ChiharaY,TomomasaT,HitomiT,AzumaM,MuraseK,Toyama Y, et al. Flexible positive airway pressure improves treat-ment adherence compared with auto-adjusting PAP. Sleep. 2013;36:229---36.