* Corresponding author: Joji Kawabe, M.D., Ph.D., Department of Nuclear Medicine, Graduate School of Medicine, Osaka City University.1-4-3, Asahimachi, Abenoku, Osaka City, Japan. Tel: 545-8585; Tel: 81-6-6645-3885; Fax: 81-6-6646-0686; E-mail: kawabe@med.osaka-cu.ac.jp
© 2013 mums.ac.ir All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Subcutaneous
Extravasation
of
Sr
89:
Usefulness
of
Bremsstrahlung
Imaging
in
Confirming
Sr
89
Extravasation
and
in
the
Decision
Making
for
the
Choice
of
Treatment
Strategies
for
Local
Radiation
Injuries
Caused
by
Sr
89
Extravasation
Joji Kawabe* , Shigeaki (igashiyama , Kohei Kotani , Atsushi Yoshida ,
(iroyuki Tsushima , Takashi Yamanaga , Daisuke Tsuruta , Susumu
Shiomi
Department of Nuclear Medicine, Graduate School of Medicine, Osaka City University. Department of Radiological Sciences, )baraki Prefectural University of (ealth Sciences Department of Radiology, Osaka City University (ospital
Department of Dermatology, Graduate School of Medicine, Osaka City University
A R T I C L E I N F O
Article type: Case Report
Article history:
Received: ‐May‐ Revised: ‐Jul‐ Accepted: ‐Jul‐
Keywords: Sr‐
Extravasation
Local radiation injury Bremsstrahlung imaging
A B S T R A C T
A male patient in his s presented at our clinic with pain caused by bone metastases of the primitive neuroectodermal tumor, and Sr‐ was administrated to palliate the pain. After receiving the injection, the patient complained of a slight burning pain at the catheterized area. Slight reddening and small circular swelling diameter, . cm were observed at the catheterized area. Sr‐ extravasation was suspected. To estimate the amount of subcutaneous Sr‐ leakage, bremsstrahlung imaging was immediately performed. We speculated that the skin‐absorbed dose from subcutaneous infiltration of Sr‐ was . Gy. The mildest clinical sign of local radiation injury was erythema. The received dose was higher than Gy, and the time of onset was from to weeks. )n our patient, local radiation injuries LR)s did not occur. Though requiring further verification, subsequent bremsstrahlung imaging and estimation of the skin‐absorbed dose from the subcutaneous infiltration of Sr‐ are useful in confirming Sr‐ extravasation and in the decision making for the choice of treatment strategies for LR)s caused by Sr‐ extravasation. Please cite this paper as:
Kawabe J, (igashiyma S, Kotani K, Yoshida A, Tsushima (, Yamanaga T, Tsuruta D, Shiomi S. Subcutaneous Extravasation of Sr‐ : Usefulness of Bremsstrahlung )maging in Confirming Sr‐ Extravasation and in the Decision Making for the Choice of Treatment Strategies for Local Radiation )njuries Caused by Sr‐ Extravasation. Asia Oceania J Nucl Med Biol. ; : ‐ .
Introduction
Reports on cases of local radiation injuries LR)s caused by the extravasation of therapeutic radionuclides are rare. )n a PubMed search, a report on Y‐ extravasation was found , but none on Sr‐ extravasation. With the increasing use of therapeutic radionuclides, a corresponding
Extravastio Asia Ocean bremsstr the amo predict t
Case Rep
A male with pa primitive administ was int cubital v confirmi patient chloride the injec burning reddenin
. cm Extravas in acco managem immedia catheter skin‐abs subcutan was sub Forte ga high‐res height photope scan ve acquired Generall week energy c images w injection anterior be obtai of the m anterior Figure whole‐bo Figure scintigra the brem uptake absorbed leakage Yamaguc manual extravas were de RO) ; RO) ; RO) ; RO) , RO cou on of Sr-89
nia J Nucl Med B rahlung imag ount of subcu the severity o
port
e patient in h ain caused b
e neuroectod trated to pa travenously vein, using a ing retrograd was slowly
Sr‐ with ction, the pa
pain at th ng and small were observ sation of the ordance wit ment of p ate warming
ized area we orbed dos neous leakag bsequently p amma camer olution LE( analyzers w ak, with a w elocity of d in a
ly, bremsstra after Sr‐ collimator ‐
were obtain n, using LE( view of the ned on brem mistake of th detector of t e a shows ody scan o b depicts th aphy. As oppo msstrahlung
arrow in d dose of Sr
was calcula chi et al ,
for the sation . R etermined ba pixe pixels a pixels O) and RO) unts, respect
iol. 2013; 1(2):56 ging to identi utaneous Sr‐ of a possible L
his s presen by bone me dermal tumor alliate the pa catheterized a ‐G winge de blood flow injected wit ‐mL saline tient compla he catheteriz circular swe ved at the ca
injected fluid th the ma ossible extr g and mas ere started. T
e of Sr‐ ge, bremsstr performed, u ra fitted wit (R collimat were set window wid
mm/min. × word ahlung imagin injection, us ‐ . (owever ed immediat (R collimator whole‐body msstrahlung i he photopeak the pulse‐heig the posteri n bremsstra he posterior osed to the b scan showe the elbow a r‐ from th ated using t , in acco managemen Regions of i ased on who els , the ab and the back
Figure c . T provided tively. Mean
6-59.
ify and estim ‐ leakage a LR).
nted at our cl etastases of
r, and Sr‐ w ain. The pati d at the ri ed needle. A w in the vein, th MBq . After receiv ained of a sli zed area. Sli elling diame atheterized a d was suspect anual for ravasation, ssaging of To estimate from rahlung imag
using an AD th a low‐ene
tor. The pu at a ‐k dth of % a . )mages w d mode mat ng is perform sing a mediu r, in our case,
tely after Sr rs. (owever, y scan could maging beca k setting of ght analyzer. or view of ahlung imag r view on b bone scintigr ed an abnor area. The sk he subcutane
the method rdance with nt of poss interests RO ole‐body upt bnormal upt kground upt Total counts , a Counts of mate and inic the was ient ight fter the q of ving ight ight eter, rea. ted; the the the the ging DAC ergy ulse‐ keV and were trix. med um‐ the r‐ an not ause the the ging. one ram, mal kin‐ eous by the ible O)s take take take s of and the thr res Fig bre b. P c. T upt T am est { abs the ret , = for dos be T Sr‐ W T D − A A U S . hyd the and vis rad est tim aft the inf
ree RO)s pr spectively.
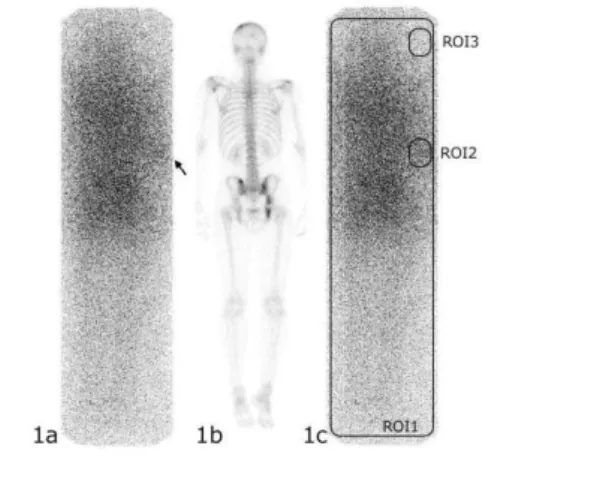
gure 1. a. Pos
msstrahlung im Posterior view on The regions of in
ake.
The injected mount of su
timated to b × . × . }} sorption time e skin was tention in the
; the swolle . cm× . rmula of the
se from the calculated by The skin‐abso ‐ infiltratio While: T=effective ha Dr=skin‐abso Gyn− Gyn A=subcutane Area= contam Using above f Skin absored / . × . A dermatolo drocortisone e follow‐up c d swelling in
ible. General diation injur timated skin me of onset o er injection. e skin‐absor filtration of S ovided .
sterior view of aging.
n bone scintigrap nterests RO)s d
Sr‐ dose w ubcutaneous be about .
‐ × . . )t was e of Sr‐ in
minutes e site of injec en area was a cm× . . )n manual , subcutaneou y the followin orbed dose fr on mGy =T/
alf‐life secon orbed dose r
ous leakage d minated area
formula in ou d dose = {
= . Gy
ogist applied and covering checkup the n n the injury lly the mildes ry is eryth dose is high of symptoms )n our p rbed dose
r‐ and it w
Ka
, . an
the whole‐bod
phy.
determined for w
was MBq Sr‐ leak
MBq = / presumed nto the blood
effective ha ction, se approximatel n accordance , the skin‐a us Sr‐ leaka ng formula: rom the subc
. ×A/Are
nds , , atio
dose MBq cm ur patient:
/ /
d lotions co g to the injur next day, the
site were n st clinical sig hema. The
er than Gy is from to patient, we c from subc was . Gy.
awabe J et al
57 nd . ,
dy scan on
Kawabe J et al Extravastion of Sr-89
58 Asia Oceania J Nucl Med Biol. 2013; 1(2):56-59.
predicted correctly that LR)s would not occur in our patient.
Discussion
Since the first report (3) of LRI caused by subcutaneous Tl-201 extravasation in 2001, the methods of measuring skin-absorbed dose from the subcutaneous Sr-89 infiltration have been evaluated and improved, (3, 7, 10) leading to the development of safety manuals for the management of therapeutic radionuclide extravasation. (2, 11) Williams et al (1) indicated that morbidity of LRIs may be reduced by identifying extravasation at the intravenous injection site of the radionuclide and by providing early treatment immediately after confirming the extravasation.
Safety guidelines for suspected Sr-89 extravasations, have the following recommendations (1, 2, 10, 11):
1) Mark the region of extravasation (if possible, take a photograph of the region).
2) Perform warming to promote vasodilatation and possible removal and dilution of the extravasated Sr-89 and to relieve pain.
3) Consider administration of steroids.
4) As soon as possible, monitor the remaining fraction of the skin-absorbed dose from the subcutaneous Sr-89 infiltration by bremsstrahlung imaging.
5) Consult a dermatologist.
In the manual, performing bremsstrahlung imaging was not mentioned. Skin-absorbed dose of Sr-89 from subcutaneous leakage was calculated in accordance with the method of Yamaguchi et al (3, 7, 8) as described by Kobayashi et al (3). Yamaguchi et al assumed that the amount of radionuclide extravasation is approximately one-third of the whole quantity. In the manual (2, 3) the average ratio of Sr-89 extravasations was assumed to be 30%. However, the ratio varies according to each case. We actually measured the ratio by bremsstrahlung images. Yamaguchi et al supposed that the contaminated area of the Sr-89 from subcutaneous leakage was 10 cm2. According to the inspection, instead of 10 cm2, we supposed that the contaminated area was the small circular swelling (diameter, 0.5 cm) in the catheterized area in order not to underestimate the skin-absorbed dose from the subcutaneous Sr-89 infiltration. Other calculating methods of skin absorbed doses due to subcutaneous leakage of radioactive pharmaceuticals were proposed by Minsky et al (12), Shapiro et al (13) and ICRU Report 56 (8) and so on. Kobayashi et al illustrated that the calculating method by yamaguchi et al was the most suitable for the supposition of the skin absorbed doses.
In this case, the square ROI (ROI 1) and the background ROI (ROI 3) were determined instead of the ROI surrounding the whole body uptake,
because it was difficult to determine along the counter of the whole body uptake correctly and in order to remove the influences from the environment background and scatter radiations. As a result, overestimation of uptake and absorbed dose may be seen. Determination of square ROI was very easy and objective. This measurement of the ratio of Sr-89 extravasation was thought to be clinically useful. More study maybe needed to accurately define ROI in these patients.
In our case, bremsstrahlung imaging was performed immediately after radionuclide injection, which had 2 benefits. First, it allowed us to confirm the occurrence of extravasation. Second, it enabled us to perform quantitative measurement of the ratio of Sr-89 extravasation. The measurement was clinically useful for the treatment strategy and the prediction of prognosis of this patient. The bremsstrahlung imaging technique that we used in the present case requires further technical evaluation. Oda et al (14) indicated that setting the energy window at 75 keV (window width of 50%) with the use of a medium energy low penetration collimator (MELP) collimator is optimal for imaging. Next time, the pulse-height analyzers may be set at 75 keV photo-peak with a window width of 50% with MELP collimator.
Conclusion
When subcutaneous extravasation is suspected after injection of Sr‐ , we would recommend performing bremsstrahlung imaging immediately and starting supportive treatment early.
References
1. Williams G, Palmer MR, Parker JA, Joyce R. Extravazation of therapeutic yttrium‐ ‐ ibritumomab tiuxetan zevalin : A case report. Cancer Biother Radiopharm ;
: ‐ .
. Committee for Radionuclide Therapy of Japan Radioisotope Association. Q ‐ Treatment of the extravasation of Sr‐ , Q&A of the part of safety management in Manual of palliative treatment with Sr‐ for painful bone metastases Ver. JAPANESE . Tokyo: Committee for Radionuclide Therapy of Japan Radioisotope Association, . . Kobayashi M, Asada Y, Suzuki S, Koga S.
Estimation of skin absorbed doses due to subcutaneous leakage of radioactive pharmaceuticals. Nihon (oshasen Anzenkanrigakukaishi ; : ‐ . . Uchiyama M, Narita (, Makino M, Sekine (,
Mori Y, Fukumitsu N et al. Strontium‐ therapy and imaging with bremsstrahlung in bone metastases. Clin Nucl Med
Extravastion of Sr-89 Kawabe J et al
Asia Oceania J Nucl Med Biol. 2013; 1(2):56-59. 59
. Narita (, Uchiyama M, Ooshita T, (irase K, Makino M, Mori Y et al. )maging of strontium‐
uptake with bremsstrahlung using Na) scintillation camera. Kaku)gaku ;
: ‐ .
. Narita (, (irase K, Uchiyama M, Fukushi M. New knowledge about the bremsstrahlung image of strontium‐ with the scintillation camera. Ann Nucl Med ; : ‐ . . Yamaguchi ), Togashi A. Dosimetric
Consequences of )nterstitial Extravasation Following i.v.Administration of Tl‐
.(okenbutsuri ; : ‐ .
. )nternational Commission on Radiation Units and measurements. Dosimetry of external beta rays for radiation protection )CRU report . Bethesda: )CRU, .
. )nternational atomic energy agency. Diagnosis and treatment of radiation injuries. Vienna: )AEA, .
. Fukuda Y. [Discussions about radiation injuries]. Kaku)gaku ; : ‐ .
. Committee for Radionuclide Therapy of Japan Radioisotope Association. ‐ Dose and )njection, Clinical use in Manual of palliative treatment with Sr‐ for painful bone metastases Ver. JAPANESE . Tokyo: Committee for Radionuclide Therapy of Japan Radioisotope Association, . . Minsky BD, Siddon RL, Recht A, Nagel JS.
Dosimetry of aqueous P after soft‐tissue infiltration following attempted intravenous administration. (ealth Phys ; : ‐ . . Shapiro B, Pillay M, Cox P(. Dosimetric
consequences of interstitial extravasation following i.v.administration of a radiopharmaceutical.Eur J Nucl Med ;
: ‐ .
. Oda (, (ara (, Ueda O, Kawamata (, Sakai (, Katou Y et al. Underlying examination in the imaging of Sr bremsstrahlung radiation. Nihon (oshasen Gijutsu Gakkai Zasshi
; : ‐ .