www.jped.com.br
ORIGINAL
ARTICLE
Preterm
premature
rupture
of
the
fetal
membranes:
association
with
sociodemographic
factors
and
maternal
genitourinary
infections
夽
,
夽夽
Arnildo
A.
Hackenhaar
a,∗,
Elaine
P.
Albernaz
a,
Tânia
M.
V.
da
Fonseca
baPost-graduationprograminHealthandBehaviour,UniversidadeCatólicadePelotas,Pelotas,RS,Brazil bHealthSciences,UniversidadeFederaldoRioGrande,RioGrande,RS,Brazil
Received9May2013;accepted10June2013 Availableonline29October2013
KEYWORDS
Prematureruptureof
fetalmembranes;
Premature;
Socialconditions;
Maternalage;
Femaleurogenital
disorders
Abstract
Objective: thisstudyaimedtoinvestigatetheincidenceofprematureruptureoffetal mem-branesinpretermsingletonpregnanciesanditsassociationwithsociodemographicfactorsand maternalself-reportedgenitourinaryinfections.
Methods: thiswasapopulation-basedcross-sectionalstudy,whichincludedallmothersof new-bornsofsingletondeliveriesthatoccurredin2010,withbirthweight≥500grams,whoresided inthecityofRioGrande.Womenwereinterviewedinthetwomaternityhospitals.Caseswere womenwhohadlostamnioticfluidbeforehospitalizationandwhosegestationalagewasless than37weeks.Statisticalanalysiswasperformedbylevelstocontrolforconfoundingfactors usingPoissonregression.
Results: ofthe2,244womeneligibleforthestudy,3.1%hadpreterm prematureruptureof fetalmembranes,whichwasmorefrequent,afteradjustment,inwomenoflower socioeco-nomicstatus,(prevalenceratio[PR]=1.94),withlowerlevelofschooling(PR=2.43),age>29 years(PR=2.49),andsmokers(PR=2.04).Itwasalsoassociatedwiththreatenedmiscarriage (PR=1.68)andpretermlabor,(PR=3.40).Therewasnoassociationwithmaternalurinarytract infectionorpresenceofgenitaldischarge.
Conclusions: theoutcomewasmorecommoninpuerperalwomenwithlowerlevelofschooling, lower socioeconomic status,older, and smokers,aswell as thosewith ahistory of threat-enedmiscarriageandprematurelabor.Thesefactorsshouldbeconsideredintheprevention, diagnosis,andtherapyapproach.
©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:HackenhaarAA,AlbernazEP,FonsecaTM.Pretermprematureruptureofthefetalmembranes:association
withsociodemographicfactorsandmaternalgenitourinaryinfections.JPediatr(RioJ).2014;90:197---202.
夽夽StudyconductedatFaculdadedeMedicinaoftheUniversidadeFederaldoRioGrande
∗Correspondingauthor.
E-mail:arnildo@vetorial.net(A.A.Hackenhaar).
0021-7557/$–seefrontmatter©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Rupturaprematurade
membranasfetais;
Prematuro;
Condic¸õessociais;
Idadematerna;
Doenc¸asurogenitais
femininas
Rupturaprematuradasmembranasfetaispré-termo:associac¸ãocomfatores sociodemográficoseinfecc¸õesgeniturináriasmaternas
Resumo
Objetivo: oobjetivodesteestudofoiverificaraocorrênciadarupturaprematuradas mem-branasfetaispré-termoemgestac¸õesúnicasesuaassociac¸ãocomfatoressociodemográficos maternoseinfecc¸õesgeniturináriasautorreferidas.
Métodos: estudo transversal de base populacional onde foram incluídastodas as mães dos recém-nascidosdospartosúnicosocorridosnoanode2010,compesoaonascerigualousuperior a500gramas,residentesnomunicípio.Aspuérperasforamentrevistadasnasduasmaternidades dacidade.Foramconsiderados casosasgestantesqueperderamlíquidoamnióticoantesda internac¸ão hospitalare cujotempo de gestac¸ão fosseinferior a37 semanas. Foi realizada análiseestatísticaporníveis,paracontroledefatoresdeconfusãopormeiodaregressãode Poisson.
Resultados: das2.244mulhereselegíveisparaoestudo,3,1%apresentaramrupturaprematura dasmembranasfetaispré-termo,aqualfoimaisfrequente,apósajuste,nasmulheresdemenor níveleconômico,razãodeprevalência(RP)de1,94,menorescolaridade,RPde2,43,comidade superiora29anos,RPde2,49etabagistas,RPde2,04.Tambémesteverelacionadacomameac¸a deaborto,RP de1,68,edetrabalhodepartopré-termo,RPde3,40.Nãohouveassociac¸ão cominfecc¸ãourináriamaternaoupresenc¸adecorrimentogenital.
Conclusões: odesfechofoimaisfrequentenaspuérperascommenorescolaridade,maispobres, maisvelhasetabagistas,assimcomonaquelascomhistóricodeameac¸adeabortamentoe tra-balhodepartoprematuro.Estesfatoresdevemserconsideradosnasuaabordagempreventiva, diagnósticaeterapêutica.
©2013SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Pretermprematureruptureoffetalmembranes(PPROM)is
definedaslossofamnioticfluidbeforetheonsetoflaborin
pregnanciesoflessthan37weeks.1Thisconditionoccursin
approximately3%ofpregnancies.2
PPROMisassociatedwithmaternalandfetalpathologies, contributingtothebirthofprematureinfants.3Thelonger
thetimeelapsedbetweenruptureanddelivery,thegreater thechanceofinfectionforbothmotherandfetus.4
ThemostcommoncauseofPPROMisspontaneous,which hasa multifactorialetiology.Itmayberelatedtoa struc-turaldefect inthe membranesduetocollagen deficiency ormalformation,totheweakeningofthemembranesdue to enzymatic destruction in inflammatory or infectious processes,andtosacexposureduetoisthmus-cervix incom-petence. PPROM risk is increased if the mother has had previous occurrenceof PPROMand lowbody massindex.5
Itsoccurrenceisalsorelatedtomechanicalfactors,suchas twinpregnancies,duetodistendeduterinevolume.6There
isahypothesisoftheassociationbetweenPPROMand geni-tourinaryinfections,butthereisnoconsensusinthisregard. The availablestudiesonPPROM indeveloped countries arecase-control,anddonotconsiderfactorssuchaslevelof schoolingandmaternalage.7---9Thesefactorsareimportant
whenobservingtheincreaseinthenumberofinfantsborn prematurely.10
The association between prematurity and PPROM indi-cates the need to investigate its occurrence in singleton pregnanciesanditsassociation withmaternal socioecono-micfactorsandself-reportedgenitourinaryinfections,and
thus, todevelop hypotheses for itsoccurrenceand direct measuresofdiseaseprevention.
Methods
Thiswasapopulation-basedcross-sectionalstudy.The
sam-pleincludedallmothersofnewbornsofsingletondeliveries
in2010,withbirthweight≥500g,whosemothersresidedin
RioGrande,Brazil,andsignedaninformedconsent.
Moth-ers who did not live in Rio Grande, multiparous women,
and those who refused to participate in the study were
excluded.
Datawerecollectedthroughasingle,pre-coded,
semi-open questionnaire by interviewers in the two maternity
hospitals of the city during hospitalization in the first
72hours after birth. The signs and symptoms present
prior to hospitalization, such as loss of fluid, blood,
or uterine contractions, were retrospectively evaluated.
The occurrence of all maternal diseases that occurred
during pregnancy and those prior to pregnancy, as
well as data on sociodemographic status, were
investi-gated.
PPROM was considered when the women had shown
loss of amniotic fluid before hospitalizationand had
ges-tationalage <37weeks.The gestationalage variablewas
assessed based on the last menstrual period. When the
date of last menstrual period was not be recalled, the
gestational age estimated by ultrasonography performed
between the fifth and 20thweek of pregnancy wasused,
Table1 Sociodemographicfactorsrelatedtotheoccurrenceofpretermprematureruptureoffetalmembranes.RioGrande, Brazil,2010.
Level1variables n PPROM(%) CrudePR(95%CI) p-value AdjustedPRa(95%CI) p-value
Socioeconomic
classificationperscore intertiles
0.001b 0.010b
First(poorest) 504 4.2 1.82(1.26---2.61) 1.94(1.27---2.97) Second 840 3.2 1.40(0.99---1.98) 1.49(1.03---2.17)
Third(richest) 785 2.3 1.00 1.00
Mother’sage(years) <0.001c <0.001c
Lessthan20 422 3.6 1.67(1.15---2.41) 1.43(0.96---2.14)
20to29 1,172 2.1 1.00 1.00
30orolder 650 4.6 2.16(1.59---2.94) 2.49(1.81---3.44)
Mother’sschooling (years)
0.005b 0.035b
Zerotoeight 1.004 3.6 2.73(1.41---5.50) 2.43(1.20---4.89) Nineto11 1.007 3.1 2.39(1.21---4.74) 2.30(1.11---4.77)
12ormore 233 1.3 1.00 1.00
Ethnicity 0.169c 0.171c
White 1,569 3.3 1.24(0.91---1.69) 1.26(0.92---1.73)
Non-white 675 2.7 1.00 1.00
CI,confidenceinterval;n,numberofwomen;PR,prevalenceratio.
a Level1variableswereadjustedtoeachother.
b Chi-squaredtestforlineartrend.
c Chi-squaredtestforheterogeneityofproportions.
pediatrician. Socioeconomic classification was performed
using the Brazilian economic classification criteria of the
Brazilian Association of Research Companies, based on
possession of items and the head of the family’s level
of schooling.12 Skin color was observed by the
inter-viewer.
Cases of self-reported urinary tract infection were considered incasesof symptomaticinfections and asymp-tomatic bacteriuria, the latter detected during routine prenatal care.13 Cases of self-reported genital discharge
were considered, in which the women had a non-white vaginal discharge, associated with bad odor, itching, or dyspareunia.14
Themissingvalueswerenotanalyzed;4.7%ofthedataon gestationalagewereunknown.Thevariablewiththe great-est amountof missinginformationwasthe socioeconomic level,duetotherateof5.2%lack ofdataontheyearsof schoolingof the child’sfather. The analyses hada signifi-cancelevelof95%.Gestationalagewasusedasreference tocalculatesamplesize,obtainingaprevalenceratioof1.6, consideringthe10% occurrencerateofprematurerupture ofmembranesintermpregnancies(85%inthestudy popu-lation),and15% wereaddedtothesamplesizetocontrol forconfounders.Thus,2,231interviewswererequired.
Multivariateanalysiswasbasedontheconceptualmodel for hierarchicallevels,15 andwasperformed usingPoisson
regression,controllingforconfoundingfactors.Those varia-bles that maintained a p-value ≤ 0.20 in the univariate
analysis were included in the multivariable analysis. The studywasapprovedbytheEthicsCommitteeofUniversidade FederaldoRioGrande(FURG).
Results
A total of 2,355 women with singleton pregnancies were
interviewed,ofwhom18refusedtoparticipateinthestudy;
therewere51lossesbyhospitaldischargebefore72hours
afterbirth.PPROMratewas3.1%.Thisproportionwas23.6%
inpretermpregnancies.
Itwasobservedthat18.8%ofthemotherswere
adoles-cents,44.7%hadeightyearsorlessofschooling,69.9%were
white,and20.1%weresmokers.TheoccurrenceofPPROM
washigherinwomenoflowersocioeconomicstatus,lower
educationallevel,andthoseolderthan29years(Table1).
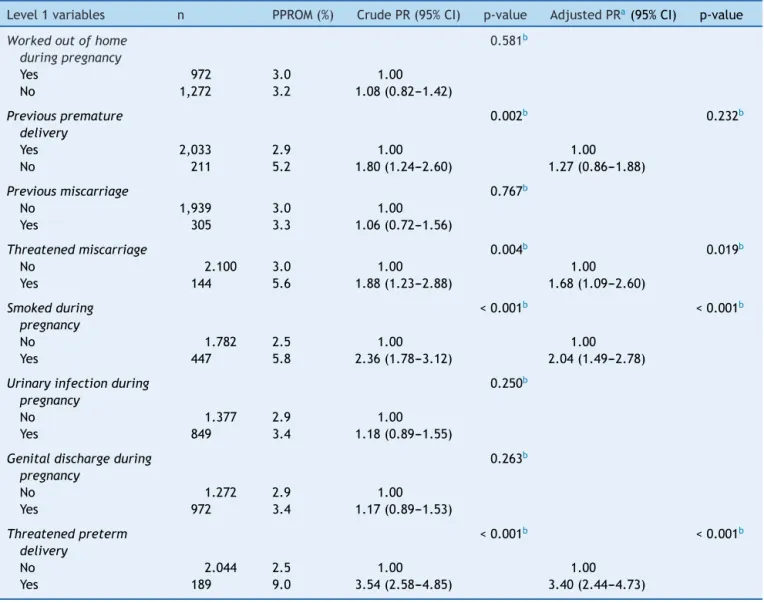
Regarding maternal habits and diseases, after adjust-ment, the occurrence of PPROM was higher in women whohadundergone treatment for threatened miscarriage and preterm labor during pregnancy, and among smokers (Table2).
Discussion
Infantmortality,especiallywhenassociatedwiththe
neona-tal component16 and the impactof prematurity oninfant
morbimortality,indicates aneed for knowledge regarding themechanismsrelatedtoPPROM,ariskfactorforpreterm birth.
Inthestudiedpopulation,3.1%hadPPROM.This propor-tionis consistentwiththatfound intheliterature.1,2 This
Table2 Maternaldiseasesrelatedtotheoccurrenceofpretermprematureruptureoffetalmembranes.RioGrande,Brazil, 2010.
Level1variables n PPROM(%) CrudePR(95%CI) p-value AdjustedPRa(95%CI) p-value
Workedoutofhome duringpregnancy
0.581b
Yes 972 3.0 1.00
No 1,272 3.2 1.08(0.82---1.42)
Previouspremature delivery
0.002b 0.232b
Yes 2,033 2.9 1.00 1.00
No 211 5.2 1.80(1.24---2.60) 1.27(0.86---1.88)
Previousmiscarriage 0.767b
No 1,939 3.0 1.00
Yes 305 3.3 1.06(0.72---1.56)
Threatenedmiscarriage 0.004b 0.019b
No 2.100 3.0 1.00 1.00
Yes 144 5.6 1.88(1.23---2.88) 1.68(1.09---2.60)
Smokedduring pregnancy
<0.001b <0.001b
No 1.782 2.5 1.00 1.00
Yes 447 5.8 2.36(1.78---3.12) 2.04(1.49---2.78)
Urinaryinfectionduring pregnancy
0.250b
No 1.377 2.9 1.00
Yes 849 3.4 1.18(0.89---1.55)
Genitaldischargeduring pregnancy
0.263b
No 1.272 2.9 1.00
Yes 972 3.4 1.17(0.89---1.53)
Threatenedpreterm delivery
<0.001b <0.001b
No 2.044 2.5 1.00 1.00
Yes 189 9.0 3.54(2.58---4.85) 3.40(2.44---4.73)
CI,confidenceinterval;n,numberofwomen;PR,prevalenceratio.
aAdjustedforfirst-levelandsecond-levelvariableswithp≤ 0.20.
b Chi-squaredtestforheterogeneityofproportions.
oflowersocioeconomiclevel,theprenatalassistanceisof
poorerquality,asthesewomenundergoasmallernumberof
consultationsandhavefewerlaboratorytests,17whichmay
contributetotheoccurrenceofthisdisease.
TheassociationofPPROMinpregnantwomenaged>29 yearscanbeexplainedbyendogenouschangesinthefetus anditsannexes,asfetalaneuploidyrates arehigherwith increasingmaternalage.18Studiesretrievedintheliterature
didnotidentifyageasrisk factorforthisdisease,asthey pairedPPROMcaseswithage-matchedcontrols.7---9
Threatened miscarriage during pregnancy was associ-ated withPPROM, which has alsobeen observed in other studies.19,20Theremaybepoorembryonicdevelopmentin
casesofPPROM. This studyalsodemonstratedan associa-tionbetweenmaternalsmokingandPPROM,similarlytothe reviewstudybyCastlesetal.21
The lack of association between PPROM and genitouri-nary infections during pregnancy in this study may be attributedtothetreatmentcompletionfortheseinfections
by mostwomen. Otherstudies have alsoidentifiedhigher valuesofmediatorsofinfectiousprocessesorbacteriaafter PPROM.22---24
There is an association between PPROM and previous treatment for threatened pretermlabor. The presence of uterine contractionsduring threatenedpreterm labor can weaken the amniotic membrane. Another study has also found an association between the presence of early con-tractionsduringpregnancyandPPROM.25
Themainlimitationofthisstudywasitscross-sectional design,whichdetectsonlyanassociationanddoesnotinfer causality.Thus,theintentionofthestudywastoraisenew hypotheses about theoccurrence ofPPROM. The use of a recall questionnaire withself-reported informationis the method of choice for cross-sectional studies that seekan association.Otherstudiesonprematureruptureofthefetal membranes26andurinaryandgenitaltractinfections27also
infection.However,thistypeofinfectionappears tohave no association with prematurity or PPROM. For instance, screeningforStreptococcusgroupBisrecommendedafter the35thweekofgestation.28
Maternalandfetalinfectiondoesnotappeartobeprior tothe occurrence of PPROM, but ratheritsconsequence. The risk of PPROM maternal and fetal infection could be increasedbyalongertimeofrupturepriortobirthinlate pretermgestations(34to37weeks)whencomparedtoterm pregnancies.29
The associations observed indicate the importance of prenatal care quality, especially for pregnant women of lower socioeconomic status. The fight against maternal smoking, aknownriskfactor for manyhealth problemsin childhood,shouldbeoneofthegoals inhealth promotion during pregnancy. It is recommended that studies on PPROM stratify the data by maternal age. The evidence of increasedrisk of PPROM in pregnantwomen aged> 29 yearsdemonstratetheimportanceofidentifyingriskfactors andtheirinclusioninprenatalcareandchildbirthprotocols.
Funding
Health Secretariatof the city of Rio Grande- CNPq2009
UniversalEdict.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.ModenaAB,KaihuraC,FieniS.Prelabourruptureofthe mem-branes:recentevidence.ActaBiomed.2004;75:5---10.
2.WatersTP, MercerB.Preterm PROM:prediction,prevention, principles.ClinObstetGynecol.2011;54:307---12.
3.Smith G, RafuseC, Anand N, Brennan B, Connors G, Crane J,etal.Prevalence,management,and outcomesofpreterm prelabourruptureofthemembranesofwomeninCanada.J ObstetGynaecolCan.2005;27:547---53.
4.RoveranV,Tedesco JJ,ForteWC, YamanoLM, Rodrigues LP, VazquezML,etal.Valoresséricosdeimunoglobulinasedos com-ponentesdocomplementoemgestantescomrupturaprematura demembranas.RevBrasGinecolObstet.2007;29:175---80.
5.CaugheyAB,RobinsonJN,NorwitzER.Contemporarydiagnosis andmanagementofpretermprematureruptureofmembranes. RevObstetGynecol.2008;1:11---22.
6.Belfort P. Amniorrexe prematura. In: Rezende J, editor. Obstetrícia.10th ed.GuanabaraKoogan:RiodeJaneiro;2007. p.918---28.
7.HargerJH,HsingAW,TuomalaRE,GibbsRS,MeadPB, Eschen-bachDA,etal.Riskfactorsforpretermprematureruptureof fetalmembranes:amulticentercase-controlstudy.AmJObstet Gynecol.1990;163:130---7.
8.Ekwo EE, Gosselink CA, Woolson R, Moawad A. Risks for premature ruptureof amnioticmembranes. IntJEpidemiol. 1993;22:495---503.
9.Hadley CB, Main DM, Gabbe SG. Risk factors for preterm premature ruptureof thefetal membranes. Am JPerinatol. 1990;7:374---9.
10.Barros FC, Victora CG, Matijasevich A, Santos IS, Horta BL, Silveira MF, et al. Preterm births, low birth weight,
and intrauterine growth restriction in threebirth cohortsin Southern Brazil: 1982, 1993 and 2004. Cad Saude Publica. 2008;24:390---8.
11.CapurroH,KonichezkyS,FonsecaD,Caldeyro-BarciaR.A sim-plifiedmethodfordiagnosisofgestationalageinthenewborn infant.JPediatr.1978;93:120---2.
12.Associac¸ãoBrasileiradeEmpresasdePesquisa(ABEP).Critério
de Classificac¸ão Econômica Brasil. 2008. [cited 25 Oct
2009]. Available from: http://www.abep.org/novo/Content.
aspx?ContentID=301
13.Brasil, Ministério da Saúde. Secretaria de Atenc¸ão à Saúde. DepartamentodeAc¸õesProgramáticasEstratégicas.Área Téc-nica de Saúde da Mulher. Pré-natal e puerpério: atenc¸ão qualificadaehumanizada---manualtécnico.Brasília:Ministério daSaúde;2005(SérieA.NormaseManuaisTécnicos).
14.CesarJA,Mendoza-SassiRA,González-ChicaDA,MenezesEH, BrinkG,PohlmannM,etal.Prevalênciaefatoresassociadosà percepc¸ãodeocorrênciadecorrimentovaginalpatológicoentre gestantes.CadSaúdePública.2009;25:2705---14.
15.VictoraCG,HutllySR, FuchsSC, OlintoMT.The roleof con-ceptualframeworksinepidemiologicalanalysis:Ahierarchical approach.IntJEpidemiol.1997;26:224---7.
16.deAlmeidaMF,GuinsburgR,MartinezFE,ProcianoyRS,Leone CR, Marba ST, et al. Perinatal factors associated withearly deathsofpreterminfantsborninBraziliannetworkonneonatal researchcenters.JPediatr(RioJ).2008;84:300---7.
17.Gonc¸alves CV, Cesar JA, Mendoza-Sassi RA. Qualidade e equidadenaassistênciaàgestante:umestudodebase popula-cionalnoSuldoBrasil.CadSaudePublica.2009;25:2507---16.
18.Forabosco A, Percesepe A, Santucci S. Incidence of non-age-dependent chromosomal abnormalities: a population-based study on 88965 amniocenteses. Eur J Hum Genet. 2009;17:897---903.
19.DadkhahF,KashanianM,EliasiG.Acomparisonbetweenthe pregnancyoutcomeinwomenbothwithorwithoutthreatened abortion.EarlyHumDev.2010;86:193---6.
20.Weiss JL, Malone FD, Vidaver J, Ball RH, Nyberg DA, Com-stock CH, etal. Threatened abortion: arisk factor for poor pregnancyoutcome,apopulation-basedscreeningstudy.AmJ ObstetGynecol.2004;190:745---50.
21.CastlesA,AdamsK,MelvinCL,KelshC,BoultonML.Effectsof smokingduringpregnancyFivemeta-analyses.AmJPrevMed. 1999;16:208---15.
22.PolettiniJ,VieiraEP,SantosMP,Perac¸oliJC,WitkinSS,SilvaMG. Interleukin18messengerRNAandproIL-18proteinexpressionin chorioamnioticmembranesfrompregnantwomenwithpreterm prelaborruptureofmembranes.EurJObstetGynecolReprod Biol.2012;161:134---9.
23.Roveran V, Silva MA, Yamano L, Rodrigues LP, Vasquez ML, PiatoS. Expressãolocaldo fatorde necrosetumoral alfana ruptura prematura de membranas.Rev BrasGinecol Obstet. 2009;31:249---53.
24.WittA,BergerA,GruberCJ,PetricevicL,WordaAP,HussleinP. IncreasedintrauterinefrequencyofUreaplasmaurealyticumin womenwithpretermlaborandpretermprematureruptureof themembranesandsubsequentcesareandelivery.AmJObstet Gynecol.2005;193:1663---9.
25.MercerBM,GoldenbergRL, MeisPJ,et al.ThePreterm Pre-diction Study: prediction of preterm premature rupture of membranesthroughclinicalfindingsandancillarytesting:the National Institute of Child Health and Human Development Maternal-FetalMedicineUnitsNetwork.AmJObstetGynecol. 2000;183:738---45.
26.WhiteheaNS,CallaghanW,JohnsonC,WilliamsL.Racial, eth-nic,andeconomicdisparitiesintheprevalenceofpregnancy complications.MaternChildHealthJ.2009;13:198---205.
infections and risk of gastroschisis: findings from the National Birth Defects Prevention Study, 1997-2003. BMJ. 2008;336:1420---3.
28.CagnoKC,PettitJM,WeissBD.PreventionofperinatalgroupB streptococcaldisease:updatedCDCguideline.AmFam Physi-cian.2012;86:59---65.