r e v b r a s o r t o p . 2016;51(3):319–328
SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
Obstetric
paralysis:
anterior
arthroscopic
release
of
the
shoulder
and
transfer
of
the
latissimus
dorsi
using
a
homologous
graft
夽
Alberto
Naoki
Miyazaki,
Caio
Santos
Checchia
∗,
Sergio
Luiz
Checchia,
Marcelo
Fregoneze,
Pedro
Doneux
Santos,
Guilherme
do
Val
Sella
FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received19May2015 Accepted18August2015 Availableonline3May2016
Keywords:
Paralysis,obstetric Brachialplexusneuropathy Tendontransfer
Transplantation Homologous Shoulder Arthroscopy
a
b
s
t
r
a
c
t
Objective:Descriptionofanewsurgicaltechniquefortreatingtheshouldersofpatients withsequelaeofobstetricparalysis.Preliminaryanalysisontheresultsobtainedfromthis technique.
Methods:Fiveconsecutivepatientsunderwenttheproposedsurgicalprocedure,consisting ofarthroscopicanteriorjointreleasefollowedbytransferofthelatissimusdorsitendon (elongatedandreinforcedwithahomologoustendongraft)totheposterosuperiorportion ofthegreatertubercle,usingasingledeltopectoralapproach.Allthepatientswere reeval-uatedafteraminimumpostoperativeperiodoftwelvemonths.Thefunctionalassessment wasbasedontherangeofmotionandthemodifiedMalletclassificationsystem.Statistical analyseswerenotpossiblebecauseofthesmallsample.
Results:Overall, passive and active lateral rotations increased, while medial rotation decreased.Theothermovements(elevation,capacitytoplaceahandinthemouthand capacitytoplaceahandbehindtheneck)hadlessconsistentevolution.Themeanmodified Malletscoreimprovedby4.2points(from11.4to15.6).
Conclusion: Thelatissimusdorsitendoncanbetransferredtotheposterosuperiorportionof thegreatertuberclethroughasingledeltopectoralapproachwhenelongatedandreinforced withahomologoustendinousgraft.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
StudyconductedattheDepartmentofOrthopedyandTraumatology,FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo (DOT-FCMSCSP),SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:caio.checchia@gmail.com(C.S.Checchia).
http://dx.doi.org/10.1016/j.rboe.2016.04.004
Paralisia
obstétrica:
liberac¸ão
artroscópica
anterior
do
ombro
e
transferência
do
grande
dorsal
com
enxerto
homólogo
Palavras-chave:
Paralisiaobstétrica
Neuropatiasdoplexobraquial Transferênciatendinosa Transplante
Homólogo Ombro Artroscopia
r
e
s
u
m
o
Objetivos:Descric¸ãodeumanovatécnicacirúrgicaparaotratamentodeombrodepacientes comsequeladeparalisiaobstétrica.Análisepreliminardosresultadosobtidoscomessa técnica.
Métodos:Cincopacientesconsecutivosforamsubmetidosaotratamentocirúrgicoproposto, queenvolvealiberac¸ãoarticularanteriorporviaartroscópica,seguidadatransferênciado tendãodomúsculograndedorsal(alongadoereforc¸adocomenxertotendíneohomólogo) paraaporc¸ãopóstero-superiordotubérculo maior,comousodeumaúnicavia delto-peitoral.Todosforamreavaliadosapósumperíodopós-operatóriomínimode12meses.A avaliac¸ãodafunc¸ãobaseou-senaamplitudedemovimentoenaclassificac¸ãomodificada deMallet.Apequenacasuísticanãopermitiuanálisesestatísticas.
Resultados: Deformageral,asrotac¸õeslateraispassivaeativamelhoraram,enquantoa rotac¸ãomedialpiorou.Osoutrosmovimentos(elevac¸ão,capacidadedecolocac¸ãodamão nabocaecapacidadedecolocac¸ãodamãonanuca)tiveramevoluc¸ãomenosconsistente. AmédiadoescoredeMalletmodificadomelhorou4,2pontos(de11,4para15,6).
Conclusão: Otendãodomúsculograndedorsalpodesertransferidoparaaporc¸ão póstero-superiordotubérculomaiorpormeiodeumaúnicaviadelto-peitoral,quandoalongadoe reforc¸adocomenxertotendíneohomólogo.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Mostpatients withobstetricalbrachial plexuspalsy (OBPP) sequelaedevelopspontaneous,completeornearlycomplete improvementofshoulderfunction.1–5However,inthosewith incompleterecovery,medialrotationshouldercontractureis oneofthemostcommonsequelae,4,6–9duetomuscle imbal-ance secondary to plexus injury (with a predominance of medialrotatorsoverlateralrotators).Thissequelaoccursearly andcanbefoundinadvancedstagesinpatientsasyoungas2 years.1,3–6,8–13Ifleftuntreated,itcanleadtoaverydebilitating jointdeformitytotheshoulderfunction.6,11
In 1918, Sever14 proposed and described the release of the pectoralis majorand subscapularis.L’Episcopo, in1934 andagainin1939,15,16observingthetendencyofrecurrence ofmedialrotation contractureafterSever procedure, asso-ciatedthis surgeryto the transferof the insertions ofthe latissimus dorsi and teres major muscles from the ante-riormedialportiontotheposterolateralhumerus.Currently, surgicalprocedurescanbedividedintothreegroups:(1) ten-dontransferswithoutanteriorshoulderrelease;(2)anterior releaseoftheshoulder,usuallyaccompaniedbytendon trans-fer;and(3)rescueprocedures,suchashumeralosteotomyor shoulderarthrodesis,typicallyforpatientswithseverejoint deformity.12,17
Thesecondgroupofproceduresiscurrentlyrecommended by most authors for the treatment patients that present withpre-existing medialrotation shouldercontracture,but stillhaveacongruentjoint.2–9,11,18–20 Theanterior shoulder releasemaybeachievedbyopen3,5–7,20–26orarthroscopic sur-gicaltechniques.3,4,8–10Thetendontransfermostcitedinthe
literatureisthatofthelatissimusdorsi(whetherornot accom-panied bythe teres major), so that it will act as a lateral shoulderrotator.2–5,7–9,12,18,19,27 Theattachmentpointofthe transferredtendonwasinitiallydescribedasthelateral cor-texofthehumerus,justbelowthegreatertuberosity,usingthe deltopectoralapproach.15,16Later,inordertopromote abduc-tionimprovement,thetransferwasmodifiedtothe posterosu-periorportionofthegreatertuberosity.18However,toachieve this,itwasnecessarytouseaposteriorapproachormultiple accessroutes.Nostudiesusingonlyananteriorapproachto thisnewtopographywereretrievedintheliterature.
Thisstudyaimedtodescribeanddiscussthesurgical tech-niquedevelopedandusedbyourgroupinfivepatientswith OBPP, whichinvolves:(1)arthroscopic releaseofthe shoul-dertogainpassivelateralrotationand(2)thetransferofthe latissimusdorsi,whereitstendoninsertionislengthenedand reinforced with a tendonallograft so that it can be trans-ferredtotheposterosuperiorportionofthegreatertuberosity throughasingleanteriorsurgicalapproach.
Materials
and
methods
From May2011toJuly2013,fivepatientswithmedial rota-tionshouldercontractureunderwentarthroscopicreleaseand latissimusdorsitendontransferperformedbytheShoulder and Elbow Surgical Group of our institution. The research projectwasapprovedbytheHumanResearchEthics Commit-teeofthesameinstitution.
rev bras ortop.2016;51(3):319–328
321
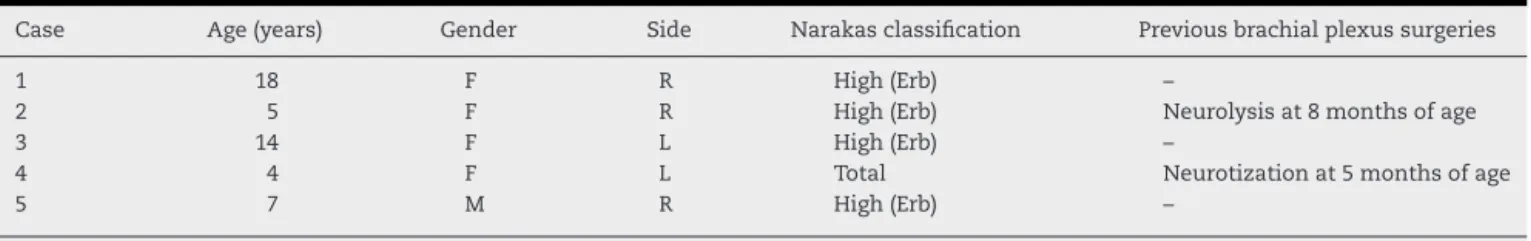
Table1–Patientclinicaldata.
Case Age(years) Gender Side Narakasclassification Previousbrachialplexussurgeries
1 18 F R High(Erb) –
2 5 F R High(Erb) Neurolysisat8monthsofage
3 14 F L High(Erb) –
4 4 F L Total Neurotizationat5monthsofage
5 7 M R High(Erb) –
Source:Servicerecords(same).
deformities(i.e.,classifiedasmaximumofgrade3,according totheWaters1classification).
Ofthefivepatients,fourwerefemaleandone(case5)male. Themean age atsurgery was9 years (4–18). According to theWaters1classification,theshouldersofallpatientswere classifiedasgrade1(nojointdeformity).Asforthemodified Narakasclassification,apudSawyer,12fourpatientshadupper brachialplexusinjury(typeI,involvingC5–C6)andonlycase 4hadtotalplexusinjury(typeIII).Cases2and4hadalready
undergonepriorbrachialplexussurgery.Case2underwent aneurolysisateightmonthsoflife;case4,atfivemonths, underwentC5rootneurotizationtotheposteriorcord,C6 neu-rotizationtotheanteriordivisionofthelateralcord,accessory nerveneurotizationtothesuprascapularnerve,andC7root neurotizationtothemiddlestem(Table1).
Forthefunctionalassessment,activeandpassiverangeof motion(ROM)measurementsweremadebyphysicians,with theuseofagoniometer.ShoulderROMsincludedpassive lat-eralrotation(withtheshoulderadducted)andthefollowing activemovements:elevationinthescapularplane,lateraland medialrotation(withtheshoulderadducted),hand-to-mouth, and hand-to-neck. Patients were assessed and classified accordingtothemodifiedMalletscale,apudBaeetal.,28for globalshoulderfunctioninpatientswithOBPP(Fig.1).
All patients underwent pre- and post-operative radio-graphicassessmentinthe trueAP,axillary,and scapularY views.Intwocases(2and3),computedtomographieswere performed.
Themeanpostoperativeoutpatientfollow-uptimewas23 monthsand 15 days (range: 12–49months). Functional re-evaluationof the operatedshoulder was conducted inthe samemannerasthepre-operativeevaluation(Table2).
Duetothesmallnumberofcasesoperatedsofarwiththis technique,theresultswerenotstatisticallyanalyzed.
Surgical
technique
Thefirststepofthesurgery,whichaimstogainpassivelateral rotation(Fig.2),isthearthroscopicrelease,performedwiththe patientundergeneralanesthesiaandinthebeach-chair posi-tion.Withthearthroscope(4-mmdiameter,30-degreeangle) positionedintheposteriorportalandanarthroscopicscissor intheanterior,ananteriorcapsulotomyuntilthefiveo’clock positionisperformed,aswellasatenotomyoftheproximal portionofthesubscapularistendon,whennecessary(Fig.3).
Then,the openmuscletransferismade.Througha del-topectoral approach, the proximal third of the pectoralis majortendonisdetachedandthelatissimusdorsiandteres
majortendonsinsertionsare identified(Fig. 4).Thetendon ofthelatissimusdorsiisrepaired,totallydetachedfromthe humerus,anditsmusclebellyispartiallydissected.Itisthen stretchedandreinforcedwithahomologoustendonfroma tissuebank(Fig.5),whichistrimmedtohavethesamewidth asthepatient’stendonandsufficientlengthtoreachthe pos-terosuperior portionofthegreatertuberosity.Incases1,2, and3,Achillestendonswereused.Incases4and5,patellar tendons.
Thetendon(alreadystretched)ispassedinferiorlytothe teresminorandthelateralheadofthetricepstothe poste-riorportion ofthehumerus. Thisisdonewiththeaid ofa longcurvedclamp,whichispassedbetweenthedeltoidand humeralheadinordertoreachthetendon(Fig.5).Finally,with theshoulderplacedat15◦ ofabductionand60◦ofrotation,
thetransferissutured(withnonabsorbableNo.5wire)tothe posterosuperiorportionofthegreatertuberosity(Fig.6).
Attheendofsurgery,thepatientisimmobilizedinneutral rotationwithanabductionsling,whichiskeptfull-timefor sixtoeightweeks.Inthisperiod,theslingisremovedonlyfor bathingand fordailyphysicaltherapy,whichinvolvesonly passivelateralrotationshoulderexercises.Afterthisperiod, shoulderROMgain andmaintenanceareinitiated,but still withoutstrengthening.Thelatterisstartedonlyfourmonths aftersurgery.
Results
TheresultsareshowninTable2indetail,whichcomparesthe pre-andpostoperativeROMs(andtheirscoresinthemodified Mallet28 classification) ofeach evaluatedmotion,separated bypatient. Thisallowsforaclearpictureofthefunctional evolutionofeachoperatedshoulder(Table2).
Ingeneral,passiveandactivelateralrotationsimproved, whilemedialrotationgotworse.Othermovements(elevation, hand-to-mouth,andhand-to-neck)presentedlessconsistent evolution.ThemeanmodifiedMalletscore28improvedby4.2 points(11.4–15.6;Table2).
Discussion
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
6;
5
1(3)
:319–328
Table2–Comparisonofpreoperativevs.postoperativefunction,stratifiedbypatientandmotion.
Case Follow-up (months)
Passivelateralrotation Activelateralrotation Elevation Medialrotation Handtomouth Handtoneck MALLETSCORE
Pre-op Post-op Pre-op Post-op Pre-op Post-op Pre-op Post-op Pre-op Post-op Pre-op Post-op Pre-op Post-op
1 49 30◦ 45◦ −10◦(2) −10◦(2) 75◦(3) 80◦(3) Sacrum(3) Sacrum(3) Marked
trumpet sign(2)
Partial trumpet sign(3)
Not possible (2)
Not possible (2)
13 13
2 26 20◦ 70◦
−45◦(1) 0◦(2) 90◦(3) 130◦(4) T12(4) Not
possible(2) Marked trumpet sign(2)
<40◦abd
(4)
Not possible (2)
Easy(4) 9 16
3 20 10◦ 80
−5◦(2) 30◦(4) 150◦(4) 140◦(4) T7(5) T7(5) Marked
trumpet sign(2)
Partial trumpet sign(3)
Hard(3) Easy(4) 12 20
4 14 45◦ 90 0◦(2) 70◦(4) 90◦(3) 80◦(3) Trochanter
(2)
Not possible(2)
Marked trumpet sign(2)
Partial trumpet sign(3)
Not possible (2)
Not possible (2)
8 14
5 12 45◦ 80◦ 10◦(3) 15◦(4) 80◦(3) 80◦(3) T12(4) Gluteus(2) Partial
trumpet sign(3)
Partial trumpet sign(3)
Not possible (2)
Hard(3) 15 15
MEAN 24 30◦ 73◦ −10◦(2) 21◦(3.2) 97◦(3.2) 102◦(3.4) (3.6) (2.8) (2.2) (3.2) (2.2) (3) 11.4 15.6
Source:Servicerecords(same).
rev bras ortop.2016;51(3):319–328
323
Abduction
Lateral rotation
Medial rotation
Hand-to-neck
Hand-to-mouth
<30º 30º to 90º >90º
<0º 0º to 20º >20º
Not possible
Not possible
Marked trumped sign Partial trumpet sign <40º abduction
T12 S1
Easy Hard
Grade III
Grade IV
Grade II
Fig.1–SchematicrepresentationofthemodifiedMalletclassification28toassessshoulderfunctioninpatientswithOBPP.
GradeI,nofunction;gradeV,functionequaltothecontralateralshoulder.GradesII,III,andIVarerepresentedforeach motion.S1,firstsacralvertebra;T12,12ththoracicvertebra.
developingjointdeformity andthereforewould notbenefit fromthisprocedure.19
Inordertoprovidethemostappropriatetherapeutic indi-cation in each case, radiological assessment is necessary. Inaddition to assessingjoint congruity and deformitiesof the glenoid and humeral head, rated according to Waters classification,1X-raysandcomputedtomographyallowforthe assessmentandmeasurementoftheshapeandversionofthe glenoidjointsurfaceandtheamountofposteriorsubluxation ofthehumeralhead.1,4,9,22 Pedowitzetal.4andKozinetal.9 demonstratedthatmagneticresonanceimagingcanalsobe usedforthis purpose,and isindicated incaseswherethe humeralepiphysisandglenoidarestillcartilaginous.
Regardingthesurgicaltechnique,thearthroscopicrelease usedinthepresentstudyisnotunusual;itwasfirstdescribed byPearl10in2003.Theuseofthearthroscopicapproach(rather
than open) isjustifiedbythe fact that subscapularis teno-tomy isnotalways necessarytoobtainthedesired passive lateralrotation.Bynotperformingatenotomy,intheory,the riskofiatrogeniclateralrotationcontractureisreduced;itcan occurwithotheropensubscapularisstretchingtechniques.10 AsadvocatedbyPearlet al.,8,10 Pedowitzet al.,4 and Kozin etal.,9itisnoteworthythatthereleaseisconsidered incom-plete whenthepassiveexternalrotationachievedwiththe shoulderabductedat90◦islowerthan45◦(Fig.2).Ifthatisthe
Fig.2–Case3.Passivelateralrotationoftheleftshoulderbefore(a)andafter(b)thearthroscopicprocedure.
Fig.3–Case2.Viewoftheintra-articularspaceoftherightshoulder,withthearthroscopeintheposteriorportal.
x=humeralhead;y=subscapularistendon.(A)Tenotomyoftheproximalportionofthesubscapularismusclewithapunch. (B)Aftersubscapularistenotomyandanteriorcapsulotomy(arrow).
Regardingthetendontransfer,thefirstaspectconsidered initsdevelopmentwasrelatedtothesurgicalapproach.To makeatendontransferspecificallytotheposteriorsuperior portionofthegreater tuberosity,somesurgeonsuse a sin-gleposteriorapproach,2,3,9,18asingleaxillaryapproach,20an anteriorapproach(deltopectoral)associatedwithaposterior approach,26orasaber-cutapproachassociatedtoaposterior approach.29,30Noarticlesdescribingthetendontransfertothe describedsiteusingthetechniquedescribedinthepresent study (asingleanterior accessroute)were retrieved inthe literature.
Thedeltopectoralapproachwaschosenforitsadvantages when compared to other approaches, which are: orthope-dicsurgeonsfamiliarity;noviolationofthedeltoidmuscle; allows, when necessary, the osteotomy of the dysplastic
coracoidprocess12,20andelongationofthetendonsofthe pec-toralismajor,shortheadofthebiceps,andcoracobrachialis7; andallowsthedetachmentofthetendonsofthelatissimus dorsi and teres majorundergood viewing,31 which,in the authors’opinion,reducestheriskofiatrogenicinjurytothe axillary nerve.However,the anterior approachhasthe fol-lowing disadvantages:in the authors’opinion, greater risk ofiatrogenic injurytothe radialnerve (it cannotbeeasily identified, despitebeing verynearthe surgicalsite[Fig. 4]); and theimpossibilityofawidedissectionofthelatissimus dorsi and teres major muscles, which does not allow for their traction tothe posterosuperior portionof the greater tuberosity.
rev bras ortop.2016;51(3):319–328
325
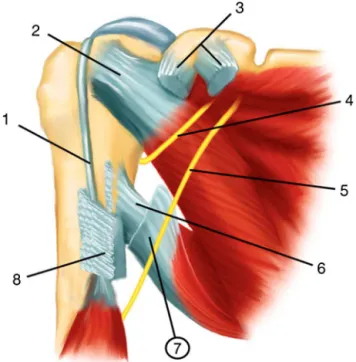
Fig.4–Schematicrepresentationoftherightshoulder. Anteriorview.Thedeltoidmuscleisnotshown.(1)Long headofthebiceps;(2)subscapularistendon;(3)insertionof theconjointtendonandthepectoralisminortendoninto thecoracoidprocess(musclesarenotshown);(4)axillary nerve;(5)radialnerve;(6)teresmajortendon;(7)latissimus dorsitendon(sectioned);and(8)humeralinsertionofthe pectoralismajormuscle(muscleisnotshown).
wereaddedtothetechnique:(1)arthroscopicaljointrelease (whichhas already been described and discussed); and (2) tendonlengtheningandstrengtheningwithagraft,toallow thefixationofthelatissimusdorsitotheposteriorsuperior
aspect ofthe greater tuberosity,which intheory would be biomechanically morefavorable.In thepresent cases, allo-graftsofcalcanealorpatellartendonswereused,astheywere consideredtobesufficientlystrongandwide.Allograftscould also beusedin order tostrengthen tendontransfer. Thus, theauthorsbelievethatitispossibletomaintainthepatient withonlyafunctionalslingandwithoutrigidthoracobrachial immobilization(plasterororthosis).
Another important aspect taken into consideration in the development ofthe techniquewas whatwould be the biomechanically best anatomicalsite forthetendon trans-fer attachment. Reviewing the literature, two trends were identified:(1)someauthors5–8,19usethelateralcortexofthe humerus, justbelowthegreater tuberosity,thesame place suggestedbytheL’Episcopotechnique16;(2)others2–4,9,18,20,26 usetheposterosuperiorportionofthegreatertuberosity(oron therotatorcuffitself),accordingtothetechniquedescribed byHofferetal.18 Thedifferenceintheprinciplebehindthe twotechniquesliesinthevectorsoftheforcesgeneratedby thetransferredmusculotendinousunits.Inthefirstgroup,the transferactsonlyasalateralrotatoroftheshoulder,whilein the secondgroup, inadditiontoactingasalateral rotator, ittheoreticallyallowsforgainsinshoulderabduction,which isoneofthecompromisedmovementsinpatientswithOBPP sequelae.AccordingtoHofferetal.,18thisisbecauseatransfer madetotheposterosuperiorportionofthegreater tuberos-ityincreasesthestabilizingeffectoftherotatorcuffandthus enablesthedeltoidtobemoreeffectiveasashoulder abduc-tor.However,itisworthdiscussingwhetherthistheoretical differenceisabletopromoteachangeinclinicaloutcomes.
Intheanalysisofresultsobtainedintheliterature,itwas observedthatseveralstudies(regardlessoflocationoftendon transfer)reportedimprovedlateralshoulderrotationformost patients.2,3,5,6,8,9,18–20,26However,thesamecouldnotbesaid forabductiongains.Ofthestudiesthatusedtransfertothe
Fig.6–Schematicrepresentation(a)andintraoperativephotograph(case1)(b)rightshoulder.Anteriorview.Arrows:siteof transfersutureattheposteriorsuperioraspectofthegreatertuberosity.
Pre-operative
a
b
c
d
Pre-operative
Post-operative
Post-operative
rev bras ortop.2016;51(3):319–328
327
lateralcortexofthe humerus,improvedamplitude ofsuch motionformostpatientswasonlyobservedinthestudiesby Coveyetal.19and byWickstrometal.6 However,abduction improvedinallstudiesinwhichthetransferwasmadetothe posterosuperiorportionofthegreatertuberosity.2,3,9,18,20,26
Specificallyinrelationtotheimprovementofshoulder ele-vationinthescapularplane,presentedresultsarelesserthan expected(Table 2). Although bothtendon transferand the useofagraftdecreasethestrengthofthetransferredmuscle group,theauthorsbelievethattheincreaseineffectivenessof thedeltoidasanabductorafterthetransferofthelatissimus dorsitotheposterosuperiorportionofthegreatertuberosity18 occursmoreduetothetenodesiseffectofthetransferthanto activemusclecontraction,asproposedGerberetal.29,30and byNové-Josserandetal.32Therefore,theadditionofatendon graftwouldnotaffectthefunctionaloutcome.However,only case2presentedimprovementsofsuchmotion(Table2),while intheotherfouritwasvirtuallyunchanged(Table2). Consid-ering this fact, the authors believe that the lifting motion canbefurtherimprovedinfuturecasesifthesutureofthe bonetransferismadewiththeshoulderatagreaterdegree of abduction, which would provide higher tension to the transfer.
Improvementinlateralrotationwasexpected,asthe find-ingswere similartothosefoundinotherseries.5 Thiswas observed withthe improvementin active and passive lat-eralrotation,whichwasachievedinfouroutoffivepatients (Table2).Otherfindingsthatcorroboratethistheorywerethe improvement(also inalmostevery case)ofhand-to-mouth andhand-to-neckmovements(Table2),becausethe move-ment of bringing the hand to the face without the need ofshoulderabductionrequiresactivelateralrotationofthe shoulder.11,33Inclinicalpractice,alesspronouncedtrumpet signtranslatesintoanimprovementoftheactivelateral rota-tionability(Fig.7).
Fullopensubscapularistenotomy,intheory,leadsto reduc-tion inactivemedialrotationability. Theproximalportion ofthe subscapularis tendon can be accessed and undergo intra-articulartenotomythrougharthroscopy.4,8–10This ten-donportionispreciselytheonethatZancolliandZancolli7 believe to be the most shortened. Therefore, arthroscopic surgerytheoreticallyprovidesalateralrotationgain(through thereleaseoftheshortenedportionofthetendon)without causingthelossofactivemedialrotation,asitwould main-tainthedistalportionofthesubscapularisintact.Thestudy byKozinetal.9reinforcesthisthesisbyreportingnochanges inmedialrotationabilityafterarthroscopicpartial subscapu-larisrelease.However,Pearletal.,8 inastudy publishedin 2006,demonstrated that their patients had significant loss ofthismotionafterundergoingthesamearthroscopic surgi-caltechnique.Ourexperienceyieldedmixedresults.Intwo cases, the medialrotation was unchanged.In three, it got worse.
Despitethesmallnumberofpatientsinthepresent stud-ies,and in lightof the results, the authors believe that it ispossibletoimprove upperlimbfunctioninthis groupof patientsusingthesurgicaltechniquedescribed.Itis impor-tanttomentionthatthe limbfunctioninthesepatients is extremely precarious, and any percentageof improvement cangreatlybenefittheirdailyactivities.
Conclusion
Thelatissimusdorsimuscletendoncanbetransferredtothe posterosuperiorportion ofthegreater tuberosity througha singledeltopectoralaccesswhenlengthened withatendon allograft.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.WatersPM,SmithGR,JaramilloD.Glenohumeraldeformity secondarytobrachialplexusbirthpalsy.JBoneJointSurgAm. 1998;80(5):668–77.
2.PagnottaA,HaerleM,GilbertA.Long-termresultson abductionandexternalrotationoftheshoulderafter latissimusdorsitransferforsequelaeofobstetricpalsy.Clin OrthopRelatRes.2004;426:199–205.
3.WatersPM,BaeDS.Effectoftendontransfersand extra-articularsoft-tissuebalancingonglenohumeral developmentinbrachialplexusbirthpalsy.JBoneJointSurg Am.2005;87(2):320–5.
4.PedowitzDI,GibsonB,WilliamsGR,KozinSH.Arthroscopic treatmentofposteriorglenohumeraljointsubluxation resultingfrombrachialplexusbirthpalsy.JShoulderElbow Surg.2007;16(1):6–13.
5.CabralJRD,CrepaldiBE,SambuyMTC,CostaACD,Abdouni YA,ChakkourI.Avaliac¸ãodafunc¸ãodomembrosuperiornos pacientescomparalisiaobstétricaapóscirurgiade
Sever-L’piscopomodificada.RevBrasOrtop.2012;47(4):451–4.
6.WickstromJ,HaslamEtHutchinsonRH.Thesurgical managementofresidualdeformitiesoftheshoulder followingbirthinjuriesofthebrachialplexus.JBoneJoint SurgAm.1955;37(1):27–36.
7.ZancolliEA,ZancolliERJr.Palliativesurgicalproceduresin sequelaeofobstetricpalsy.HandClin.1988;4(4):643–69.
8.PearlML,EdgertonBW,KazimiroffPA,BurchetteRJ,WongK. Arthroscopicreleaseandlatissimusdorsitransferfor shoulderinternalrotationcontracturesandglenohumeral deformitysecondarytobrachialplexusbirthpalsy.JBone JointSurgAm.2006;88(3):564–74.
9.KozinSH,BoardmanMJ,ChafetzRS,WilliamsGR,HanlonA. Arthroscopictreatmentofinternalrotationcontractureand glenohumeraldysplasiainchildrenwithbrachialplexusbirth palsy.JShoulderElbowSurg.2010;19(1):102–10.
10.PearlML.Arthroscopicreleaseofshouldercontracture secondarytobirthpalsy:anearlyreportonfindingsand surgicaltechnique.Arthroscopy.2003;19(6):577–82.
11.WatersPM.Updateonmanagementofpediatricbrachial plexuspalsy.JPediatrOrthopB.2005;14(4):233–44.
12.SawyerJR.Paralyticd.In:CanaleST,BeatyJH,editors. Campbell’soperativeorthopaedics.12ed.Philadelphia: MosbyElsevier;2013.p.1255–333.
13.VieiraLAG,PoderosoMA,Gonc¸alvesMCK,HissadomiMI, BenegasE,FerreiraNetoAA,etal.Aosteotomiade centralizac¸ãodacabec¸aumeral,naluxac¸ãoposteriordo ombro,seqüeladeparalisiaobstétrica.RevBrasOrtop. 2004;39(11/12):661–9.
14.SeverJW.Theresultsofanewoperationforobstetrical paralysis.AmJOrthopSurg.1918;16:248–57.
16.L’EpiscopoJB.Restorationofmusclebalanceinthetreatment ofobstetricalparalysis.NYStateJMed.1939;39:357.
17.LopesEI,ChakkourI,GomesMD,CauchiolliCA,RamirezJFG, LopesFilhoJD.Osteotomiaderotac¸ãoexternadoúmerono tratamentodasdeformidadesemrotac¸ãointernadoombro nasseqüelasdeparalisiaobstétrica.RevBrasOrtop. 1996;31(4):322–6.
18.HofferMM,WickendenR,RoperB.Brachialplexusbirth palsies:resultsoftendontransferstotherotatorcuff.JBone JointSurgAm.1978;60(5):691–5.
19.CoveyDC,RiordanDC,MilsteadME,AlbrightJA.Modification oftheL’Episcopoprocedureforbrachialplexusbirthpalsies.J BoneJointSurgBr.1992;74(6):897–901.
20.PhippsGJ,HofferMM.Latissimusdorsiandteresmajor transfertorotatorcuffforErb’palsy.JShoulderElbowSurg. 1995;4(2):124–9.
21.GilbertA,BrockmanR,CarliozH.Surgicaltreatmentof brachialplexusbirthpalsy.ClinOrthopRelatRes. 1991;264:39–47.
22.PearlML,EdgertonBW.Glenoiddeformitysecondaryto brachialplexusbirthpalsy.JBoneJointSurgAm. 1998;80(5):659–67.
23.GiostriGS,MacheziniEJ,PasinAP.Rotac¸ãointernana paralisiaobstétrica:comparac¸ãodosresultadosdos
procedimentosdeSever-L’Episcopoeosteotomiaderrotadora doúmero.RevBrasOrtop.1996;31(1):33–5.
24.ChuangDC,MaHS,WeiFC.Anewstrategyofmuscle transpositionfortreatmentofshoulderdeformitycausedby obstetricbrachialplexuspalsy.PlastReconstrSurg. 1998;101(3):686–94.
25.WatersPM,PeljovichAE.Shoulderreconstructioninpatients withchronicbrachialplexusbirthpalsy:acase–controlstudy. ClinOrthopRelatRes.1999;(364):144–52.
26.OzbenH,AtalarAC,BilselK,DemirhanM.Transferof latissmusdorsiandteresmajortendonswithout
subscapularisreleaseforthetreatmentofobstetricalbrachial plexuspalsysequela.JShoulderElbowSurg.
2011;20(8):1265–74.
27.SantosC,PereiraA,PintoRR,TrigueirosM,LemosR,SilvaC. Cirurgiapaliativadoombroemparalisiaobstétricadoplexo braquial.RevIberamCirMano.2010;38(1):25–30.
28.BaeDS,WatersPM,ZurakowskiD.Reliabilityofthree classificationsystemsmeasuringactivemotioninbrachial plexusbirthpalsy.JBoneJointSurgAm.2003;85A(9): 1733–8.
29.GerberC,VinhTS,HertelR,HessCW.Latissimusdorsi transferforthetreatmentofmassivetearsoftherotatorcuff: apreliminaryreport.ClinOrthopRelatRes.1988;(232): 51–61.
30.GerberC.Latissimusdorsitransferforthetreatmentof irreparabletearsoftherotatorcuff.ClinOrthopRelatRes. 1992;(275):152–60.
31.BoileauP,ChuinardC,RoussanneY,NeytonL,TrojaniC. Modifiedlatissimusdorsiandteresmajortransferthrougha singledelto-pectoralapproachforexternalrotationdeficitof theshoulder:asanisolatedprocedureorwithareverse arthroplasty.JShoulderElbowSurg.2007;16(6):671–82.
32.Nové-JosserandL,CostaP,LiotardJP,SafarJF,WalchG,Zilber S.Resultsoflatissimusdorsitendontransferforirreparable cufftears.OrthopTraumatolSurgRes.2009;95(2):
108–13.