Review
The
impact
of
antioxidant
agents
complimentary
to
periodontal
therapy
on
oxidative
stress
and
periodontal
outcomes:
A
systematic
review
Francisco
Wilker
Mustafa
Gomes
Muniz
a,*
,
Sergiana
Barbosa
Nogueira
b,
Francisco
Lucas
Vasconcelos
Mendes
b,
Cassiano
Kuchenbecker
Ro¨sing
a,
Maria
Moˆnica
Studart
Mendes
Moreira
c,
Geanne
Matos
de
Andrade
d,
Rosimary
de
Sousa
Carvalho
ca
Post-GraduatePrograminDentistry,FederalUniversityRioGrandedoSul,RuaRamiroBarcelos,2492,PortoAlegre, RioGrandedoSul90035-003,Brazil
bSchoolofDentistry,FacultyofPharmacy,DenstistryandNursing,FederalUniversityofCeara´,
RuaAlexandreBarau´na,949,Fortaleza,Ceara´ 60430-160,Brazil
cDisciplineofPeriodontology,SchoolofPharmacy,DentistryandNursing,FederalUniversityCeara´,
RuaAlexandreBarau´na,949,Fortaleza,Ceara´ 60430-160,Brazil d
DepartmentofPhysiologyandPharmacology,FacultyofMedicine,FederalUniversityCeara´, RuaAlexandreBarau´na,949,Fortaleza,Ceara´ 60430-160,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Accepted19May2015
Keywords:
Chronicperiodontitis Periodontaldiseases Vitamins
Respiratoryburst Reactiveoxygenspecies Superoxidedismutase
a
b
s
t
r
a
c
t
Thereissignificantevidencelinkingchronicperiodontitis(CP)andoxidativestress(OS). CPisamultifactorialinfecto-inflammatorydiseasecausedbytheinteractionofmicrobial agents present in the biofilm associated with hostsusceptibility and environmental factors.OSisaconditionthatariseswhenthereisanimbalancebetweenthelevelsof freeradicals(FR)anditsantioxidantdefences.Antioxidants,definedassubstancesthat areabletodelayorpreventtheoxidationofasubstrate,existinallbodilytissuesand fluids,andtheirfunctionistoprotectagainstFR.Thissystematicreviewassessedthe effectsofthecomplimentaryuseofantioxidantagentstoperiodontaltherapyintermsof oxidativestress/antioxidants.Onlyrandomised,controlled,double-blindorblindstudies wereincluded.Themajorityoftheincludedstudieswereperformedinchronic periodon-titispatients.Lycopene,vitaminC,vitaminE,capsuleswithfruits/vegetables/berryand dietaryinterventionsweretheantioxidantapproachesemployed.Onlythestudiesthat usedlycopeneandvitaminEdemonstratedstatisticallysignificantimprovementwhen compared toa controlgroupintermsof periodontalparameters.However,oxidative
*Correspondingauthor.Tel.:+558596520187/5195715453.
E-mailaddresses:wilkermustafa@gmail.com(F.W.M.G.Muniz),sergianab@gmail.com(S.B.Nogueira),lucas_v_mendes@hotmail.com
(F.L.V.Mendes),ckrosing@hotmail.com(C.K.Ro¨sing),monicastudartmoreira@gmail.com(M.M.S.M.Moreira),
gmatos@ufc.br(G.M.deAndrade),roseperio@yahoo.com.br(R.d.S.Carvalho).
Abbreviations: CP, chronic periodontitis; OS, oxidative stress; FR,free radicals; ROS, reactive oxygen species; SOD, superoxide dismutase;CAT,catalase;GPx,glutathioneperoxidase;SRP,scalingandrootplanning;8-OHdG,8-hydroxydeoxyguanosine;TAOC,total antioxidantcapacity;ELISA,enzymelinkedimmunosorbentassay.
Available
online
at
www.sciencedirect.com
ScienceDirect
journalhomepage:http://www.elsevier.com/locate/aob
http://dx.doi.org/10.1016/j.archoralbio.2015.05.007
Contents
1. Introduction ... 1204
2. Methodology ... 1204
3. Results... 1205
4. Discussion... 1210
5. Conclusions... 1212
References... 1212
1.
Introduction
Periodontitisisachronicinfecto-inflammatorydisease pre-senting inflammation ofthe periodontal tissues that cause alveolarbonelossand,insomeseverecases,toothexfoliation.1 Progressionofperiodontaldiseaseisdependentonthehost immuneresponseandsusceptibility.2,3Recently,studieshave pointedtooxidativestressasbeingpartofthepathogenesisof periodontaldiseases.4Oxidativestressisaconditioncausedby aharmfulincreaseintheproductionofreactiveoxygenspecies (ROS),5 which are important signalling molecules in the regulationofseveralcellularprocesses,6emergingwhenthere isanimbalancebetweenROSlevelsandthehostantioxidant defences.Consequencesoftheoxidativestressinclude adap-tation,damageorcelldeath7throughavarietyofmechanisms, suchasDNA,lipidandproteindamage.8
RegardingthepreventionofROSformation,enzymaticand non-enzymaticantioxidantmechanismshavebeenstudiedand reportedintheliterature.Enzymaticmechanismsare responsi-blefordirectROSneutralisation,4,9,10andthesemechanismsare constitutedbyprimaryenzymesinvolvedinhumanorganism protectioninattempttomaintaintheROSlevelsinanormal range.Examplesoftheseenzymesaresuperoxidedismutase (SOD),catalase(CAT)andglutathioneperoxidase(GPx).
Superoxidedismutase(SOD)isoneofthemostabundant antioxidant enzymes in the human body.11,12 One of its mechanismsofactionistheconversionofsuperoxideanions intohydrogenperoxide(H2O2),whichoperatesasapreventive antioxidantbecauseit avoidstheformation ofthehydroxyl radical (OH ).13 The SOD levels are reduced in chronic periodontitispatientswhencomparedwithcontrols,12andit hasbeenshownthat,afterscalingandrootplaning(SRP),its serumandsalivarylevelswereincreasedsignificantly.14CATis mainlylocatedintheperoxisomes,anditiscapableofremoving intracellularH2O2and superoxideradicalswithgreat effica-cy.4,10,15 Salivary levels of CAT were reduced in chronic periodontitispatientswhencomparedtoperiodontallyhealthy subjects.16GPxisaselenium-containingperoxidaseresponsible for the protection of mammalian cells against oxidative
damages byreducting a variety ofhydroperoxides,suchas ROOH and H2O2extracellularly and inthemitochondria.4,17 Additionally,one studyshowedthatgingivalcrevicularfluid from periodontitis patients contained significantly lower amountsofreducedandoxidisedglutathionethanmatched periodontallyhealthysubjects.17
Furthermore, non-enzymaticantioxidantsaresecondary mechanismstoneutraliseROS.4,9,18,19Generally,thesetypes ofantioxidantsareobtainedexogenously,mainlythrougha balanced diet, which included a variety of fruits and vegetables,suchasblueberries,strawberries,grapes,20 avoca-do,21tomatoes,22spinach,23andcarrots.19Thenon-enzymatic antioxidantsarerepresentedbyfat-solublevitamins(vitamin A,vitaminE-tocoferolandb-carotene),water-solublevitamins (vitaminCandvitaminBcomplex),traceelements(zincand magnesium),andbioflavonoids(plantderived).
Studies have demonstrated that, in patients with peri-odontitis,oxidative levelsareincreasedwhencomparedto periodontallyhealthysubjects.24,25However,theantioxidant levelsaresignificantlylowerinchronicperiodontitispatients whencomparedtoperiodontallyhealthyindividuals.17,26–28
Itiswellestablishedthatmosttypesofperiodontitiscanbe successfullytreatedbyremovingthesupra-andsubgingival biofilmbyscalingandrootplaningcombinedwithadequate periodontalsupportmaintenance.29Scalingandrootplaning isalsocapableofdecreasingthe totaloxidantstatusinthe gingivalcrevicularfluidandimprovingtheantioxidantlevels inpatientswithchronicperiodontitis.26,30
Therefore,periodontaldiseasesand reducedantioxidant levels seem to be associated with one another,leading to increasedoxidativedamages intheoral environment.This systematicreviewassessedtheeffectofantioxidantagentsas complimentarytoperiodontaltherapyintermsofoxidative stress/antioxidants.
2.
Methodology
Thefocusedquestionforthissystematicreviewwas:istherea benefitofantioxidantagentscomplimentarilytoperiodontal stressoutcomes didnot follow the same pattern throughoutthe studies. It may be concludedthattheuseofsomeantioxidantshasthepotentialtoimproveperiodontal clinicalparameters.Theroleofantioxidant/oxidativestressparametersneedsfurther investigations.
therapyintermsofperiodontalandoxidative stress/antioxi-dantparameters?
Thesearchforthis systematicreview wasconducted in MEDLINE-Pubmed,Lilacs, and Scielo databases. Thesearch strategy included the following terms: ‘‘periodontitis’’ OR ‘‘chronicperiodontitis’’AND‘‘oxidativestress’’OR ‘‘antioxi-dant’’OR‘‘antioxidant effect’’OR‘‘vitamin’’. Theliterature wassearcheduptoSeptember2014.
Titlesandabstractsresultingfromthesearchasdescribed above were screened. Retrieval of studies was performed whenthetitlesorabstractsfulfilledthefollowingcriteria:
Randomisedclinicaltrial Double-blindorblind
Interventiongroup:studiesthattreated gingivitis/periodon-titis with supragingival plaque control/nonsurgical peri-odontal therapy and administered, complimentarily, antioxidantagentsinoneofthefollowingmanners: Systemically.
Locally.
Throughanytypeofdietintervention.
Controlgroup:studiesthatusedoneofthefollowingcontrol groupswereaccepted:
Aplaceboagentwithnonsurgicalperiodontaltherapy. Nonsurgicalperiodontaltherapyonly.
Absenceofperiodontaltherapy. Healthyperiodontalsubjects.
Nolanguageorpublicationdaterestrictionswereapplied. However,thestudieswereexcludediftheypresentedoneof thefollowingcriteria:
Observationalandexperimentalanimalstudies. Casereports,lettersandreviews.
Includedonlysubjectsyoungerthan18yearsold. Usedexperimentalgingivitisintheirstudydesign. Didnotassessanykindofoxidativestressoutcome.
Studieswithoutabstractsbutwhosetitlessuggestedthat theycouldberelatedtotheobjectiveofthissystematicreview were also selected so the full text could be screened for eligibility. All the references of every selected study were screenedforpossibleeligiblestudiesaswell.
Toreducethepotentialbiasinthereview,screeningwas performed independently by two reviewers (SBN and FWMGM). Any discrepancies with regard to the exclusion and inclusion of the studies were resolved by extensive discussionbetweenthetworeviewers.Ifanydoubtremained, anotherinvestigator(RSC)becameinvolvedintheprocess.
3.
Results
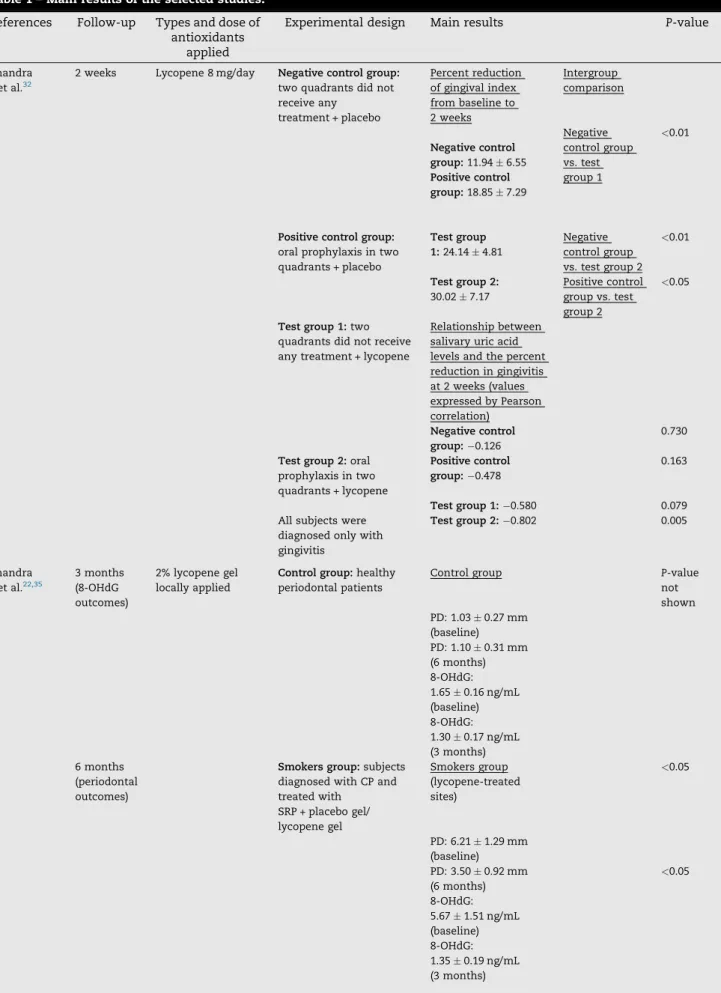
One-thousand one-hundred and fifty-three (1153) titles/ abstracts were retrieved from the search, of which seven were selected based on the criteria previously described (Fig.1).AlloftheselectedstudieswerewritteninEnglish,and themainresultsofthesestudiesareshowninTable1.
Moststudies focused on the use of antioxidants inthe treatmentofchronicperiodontitisinnonsmokers26,31–34and
onlyonestudyinthetreatmentofgingivitis.32Theantioxidant agentsusedwerevitaminE,34vitaminC26andconcentrated capsules of fruits/vegetables/berry,31 and lycopene both locally33,35 and systemically.32 One study also performed dietary intervention on anindividual basis toimprove the amountofantioxidantintake.36Additionally,twostudiesused thesplit-mouthintheirexperimentaldesign.32,33Thisdesign ischaracterisedbyatrialinwhicheachindividualistreatedby atleasttwodifferenttreatmentsinaseparateportionofthe mouth.37Therefore,inthisdesign,eachindividualis consid-ered their own control, as these different therapies may resultsindifferentoutcomes.
Split-mouthdesignisatrialinwhicheachsubjectreceives at leasttwo different treatments ina separate part ofthe mouth.
Thestudythatusedsystemicallyadministeredlycopene wasdevelopedbyChandraetal.,32andtheyanalyseditseffect inthetreatmentofgingivitis.Asplit-mouthdesignwasused with20patientsdiagnosedonlywithgingivitis;10individuals received 8mg lycopene/day systemically for 2 weeks (test group),andtheremaining10subjectsreceivedaplaceboagent (controlgroup).Bothgroupsreceivedoralprophylaxisintwo contralateraloralquadrants,andtheotherquadrantsdidnot receiveanytreatmentatbaseline.After2weeks,allgroups demonstratedstatisticallysignificantreductionsingingivitis, bleeding index and plaque index compared to baseline. Furthermore,sitestreatedwithlycopeneandoralprophylaxis significantly reduced more gingivitis when compared with bothcontrolgroups.Additionally,gingivitispatientswhowere treated onlywithlycopeneshowedagreater improvement comparedwiththegroupthatwastreatedwiththeplacebo only. That study also evaluated the relationship between salivary uric acid levels and the percentage reduction of gingivitis,showingthat,after2weeks,onlythegrouptreated withlycopeneandoralprophylaxisdemonstratedasignificant strongnegativecorrelation.
Lycopenewasalsousedlocallyintwostudies complimen-tarilyforSRP.33,35Oneofthesestudiesshowedthat lycopene-treatedsitespresentedsignificantlyhigherlevelsofprobing depth reduction and more clinical attachment gain when comparedtositestreatedwithplacebogel,despitesmoking habits.35Thestudyalsoshowedthatperiodontaltreatment wascapableofreducingtheserumlevelsof 8-hydroxydeox-yguanosine (8-OHdG), a biomarker of oxidative damage. Additionally,thelycopene-treatedsitesinnonsmokers,when compared tosmokers, benefited morefromthis reduction, achievinglevelsquitesimilartothoseofperiodontalhealthy individuals. Theotherstudy,developedbyChandraetal.,33 used asplit-mouthdesign.Three sitesofall patientswere randomlytreatedwithSRP,placebogelapplicationafterSRP and 2% lycopene gel application after SRP. In that study, lycopene-treated sitespresented significantlymoreprobing depthreductionandclinicalattachmentgainaftersixmonths. Additionally,thelevelsof8-OHdG1weekaftertherapywere statisticallyreducedatlycopene-treatedsiteswhencompared withtheothertwogroups.However,thosedifferenceswereno longerpresentafterthreemonths.
Table1–Mainresultsoftheselectedstudies.
References Follow-up Typesanddoseof antioxidants
applied
Experimentaldesign Mainresults P-value
Chandra etal.32
2weeks Lycopene8mg/day Negativecontrolgroup:
twoquadrantsdidnot receiveany
treatment+placebo
Percentreduction ofgingivalindex frombaselineto 2weeks
Intergroup comparison
Negativecontrol group:11.946.55
Positivecontrol group:18.857.29
Negative controlgroup vs.test group1
<0.01
Positivecontrolgroup:
oralprophylaxisintwo quadrants+placebo
Testgroup 1:24.144.81
Negative controlgroup vs.testgroup2
<0.01
Testgroup2:
30.027.17
Positivecontrol groupvs.test group2
<0.05
Testgroup1:two quadrantsdidnotreceive anytreatment+lycopene
Relationshipbetween salivaryuricacid levelsandthepercent reductioningingivitis at2weeks(values expressedbyPearson correlation)
Negativecontrol group: 0.126
0.730
Testgroup2:oral prophylaxisintwo quadrants+lycopene
Positivecontrol group: 0.478
0.163
Testgroup1: 0.580 0.079 Allsubjectswere
diagnosedonlywith gingivitis
Testgroup2: 0.802 0.005
Chandra etal.22,35
3months (8-OHdG outcomes)
2%lycopenegel locallyapplied
Controlgroup:healthy periodontalpatients
Controlgroup P-value
not shown PD:1.030.27mm
(baseline) PD:1.100.31mm (6months) 8-OHdG: 1.650.16ng/mL (baseline) 8-OHdG: 1.300.17ng/mL (3months) 6months
(periodontal outcomes)
Smokersgroup:subjects diagnosedwithCPand treatedwith
SRP+placebogel/ lycopenegel
Smokersgroup (lycopene-treated sites)
<0.05
PD:6.211.29mm (baseline) PD:3.500.92mm (6months)
<0.05
Table1 (Continued)
References Follow-up Typesanddoseof antioxidants
applied
Experimentaldesign Mainresults P-value
Smokersgroup (placebo-treated sites)
<0.05
PD:6.021.49mm (baseline) PD:5.161.52mm (6months)
<0.05
8-OHdG: 5.661.52ng/mL (baseline) 8-OHdG: 1.460.26ng/mL (3months)
Nonsmokersgroup:
subjectsdiagnosedwith CPandtreatedwith SRP+placebogel/ lycopenegel
Nonsmokersgroup (lycopene-treated sites)
<0.05
PD:6.040.87mm (baseline) PD:3.951.21mm (6months)
<0.05
8-OHdG: 5.341.14ng/mL (baseline) 8-OHdG: 1.110.28ng/mL (3months) Nonsmokersgroup (placebo-treated sites)
PD:6.311.27mm (baseline) PD:4.811.34mm (6months) 8-OHdG: 5.431.14ng/mL (baseline) 8-OHdG: 1.490.25ng/mL (3months)
Thelevelsof8-OHdG werereducedin everygroupthat receivedSRP
<0.001
Lycopene-treated sitesreducedeven more8-OHdGlevels, especiallyin nonsmokers
Chandra etal.33
3months (8-OHdG outcomes)
2%lycopenegel locallyapplied
Shamgroup:treatedonly withSRP
PDSDmeansat 6months
Intergroup comparison
6months (periodontal outcomes)
Placebogroup:treated withSRP+placebogel
Shamgroup:
4.921.35mm
Placebogroup:
4.511.22mm
Lycopenegroup:
3.621.04mm
Placebovs. sham Lycopenevs. sham Lycopenevs. placebo
0.430 0.001 0.020
Lycopenegroup:treated with+lycopenegel
8-OHdGlevels at3months
Table1 (Continued)
References Follow-up Typesanddoseof antioxidants
applied
Experimentaldesign Mainresults P-value
Shamgroup:
1.42ng/mL
Placebogroup:
1.52ng/mL
Lycopenegroup:
1.39ng/mL
Placebovs. sham Lycopenevs. sham Lycopenevs. placebo
0.460 0.930 0.277
Abou Sulaiman and Shehadeh26
1month (TAOC outcomes)
VitaminC2000mg/ day
Controlgroup:healthy periodontalsubjects
TAOClevels1 monthafter periodontaltherapy:
3months (periodontal outcomes)
Testgroup1:subjects diagnosedwithCPand treatedwith
SRP+vitaminC
Controlgroup:
62588.7mm Teq(baseline)
Testgroup1:
655.843.2mm Teq
Testgroup2:
651.463.3mm Teq
>0.05
(between all groups)
MeanofPD3 monthsafter periodontaltherapy
Testgroup2:subjects diagnosedwithCPand treatedonlywithSRP
Controlgroup:
notshown
Testgroup1:
2.880.48mm
Testgroup2:
3.070.61mm
0.329 (between testgroup 1and2)
ZareJavid etal.36
6months Customiseddietary intervention
Controlgroup:treated onlywithSRP
TAOCmeanand 95%CIat6months
Controlgroup:
1.23(1.18;1.26)
0.02
Testgroup:treatedwith SRP+dietaryintervention
Testgroup:1.31 (1.23;1.39) Nostatistical differencewas foundinthe periodontal outcomes(data notshown)
Chapple etal.31
8months CapsulesFV(4 fruits/vegetables capsules+2placebo capsulesfor9 months)
Controlgroup:onlySRP ThetestgroupFV showedstatistically significantgreater reductioninPD whencomparedto thecontrolgroup2 monthsafter therapy
<0.03
CapsulesofFVB(6 fruits/vegetables/ berrycapsulesfor9 months)
TestgroupFV:
SRP+capsulesFV
At5-and8-months evaluation,that differencewasno longerstatistically significant
>0.05
TestgroupFVB:
SRP+capsulesFVB
Additionally,thePD reduction,intest groupFVB,wasnot statisticallydifferent fromcontrolgroup atanytime
only in half of this sample was vitamin C systemically administered in a 2000mg dose per day for 4 weeks. The totalantioxidantcapacity(TAOC)ofplasmawasevaluatedat baselineand1monthafterSRP.Complimentaryuseofvitamin CdidnotpromoteanyadditionalimprovementintheTAOC levelsandinperiodontalparameters3monthsaftertherapy. However,periodontaltherapyitselfwassufficienttoimprove theTAOClevels.
The impact of customised dietary intervention was verified by Zare Javid et al.36 in 51 chronic periodontitis patients.Thecustomiseddietaryinterventionwasperformed toincreasethehabitofeatingfruits,vegetablesandwhole grainsinanattempttoimprovetheantioxidantstatus.Inthat study,onegroupreceivedonlySRPandgeneralnutritional considerations (control group), while the other group re-ceivedSRP,aone-to-onesessionwithacommunitynutrition assistantandapersonalisedpackagewithdietary interven-tions(testgroup).Thelevels oftotalapparentantioxidant capacityinplasma,assessed byTroloxequivalent antioxi-dantcapacity,showedthatthetestgrouppresented signifi-cantlyhigherlevelsofantioxidantcapacitythanthecontrol group.However,thedifferentperiodontaloutcomesdidnot demonstrate statistically significant differences in both
groups. Furthermore, it is important tohighlight that the periodontalparameters(bleedingindex)remainedunaltered inbothgroupsduringtheentirestudy.
Chappleetal.31investigatedtheadjunctiveeffectofdaily supplementationwithencapsulatedfruit,vegetableandberry juicepowderconcentratedinclinicalperiodontalparameters. Sixty chronic periodontitispatients weredivided into three groups,withonereceivingonlySRP (controlgroup),andthe other receiving SRP, four fruit/vegetable capsules and two placebocapsulesfor9months(FVgroup),andanothergroup receivedSRPandsixcapsules,containingfruit/vegetable/berry juicepowderconcentrationsfor9months(FVBgroup). Two months after periodontal therapy, the FV group showed significantlygreaterprobingdepthreductionwhencompared tothecontrolgroup.Thisdifferencewasnolongerstatistically significantafter5months.RegardingtheFVBgroup,theresults werestatisticallyequaltothoseofthecontrolgroupandFV group at all experimental times. Despite the absence of differences intheperiodontaloutcomeswithlonger follow-up,theserumb-carotenelevelswereincreasedsignificantlyin boththeFVandFVBgroupsincomparisonwiththeplacebo group.Surprisingly, thehighestlevelswerefoundintheFV group,even8monthsaftertherapy.
Table1 (Continued)
References Follow-up Typesanddoseof antioxidants
applied
Experimentaldesign Mainresults P-value
Singh etal.34
3months VitaminE200mg everyotherday
Controlgroup:healthy periodontalsubjects
Median(minimum; maximum)PDvalues
<0.05
(between test group1 andtest group2)
Controlgroup:1.19 (0.17;2.18)mmat baseline
Testgroup1:2.06 (1.12;3.03)mmat 3months
Testgroup2:1.85 (1.14;2.98)mmat 3months
Testgroup1:subjects diagnosedwithCPand treatedonlywithSRP
Median(minimum; maximum)of serumSODactivity
<0.05
(between test group1 andtest group2)
Testgroup2:subjects diagnosedwithCPand treatedwith
SRP+vitaminE
Controlgroup:69.36 (53.85;91.31)%
Testgroup1:62.06 (55.19;90.92)%
Testgroup2:85.90 (49.06;95.63)%
Singhetal.34evaluatedtheeffectofvitaminE, complimen-tarilytoSRP,inperiodontalandSOD outcomes.Thisstudy used38patientsdividedintotwogroups:onegroupreceived onlySRP,andtheotherwastreatedwithSRPandvitaminE 200mg(300IU)everyotherday.Itwasfoundthatthegroup that receivedSRP and vitaminEdemonstrated statistically significant improvements in all periodontal parameters analyzed, which included plaque index, probing depth, clinicalattachmentlevel,and bleedingonprobing. Further-more,the serum SOD activitywas significantlyelevated in bothSRP-treated groups. However, inthe vitaminEgroup, when compared with the control group, the increase was statisticallysignificant,achievinglevelssimilartoperiodontal healthysubjects.
4.
Discussion
Thepresentsystematicreviewwasaimedatunderstanding the optimal use ofantioxidants asadjuncts toperiodontal therapy.Theresultsofthereviewmayhaverelevanceforthe developmentoftreatmentprotocols.
Theselectedstudiesforthissystemicreviewhaddiverse study designs with follow-ups ranging from 2 weeks to 8 months; those studies were mainly focused on treating chronicperiodontitis.Theantioxidantusedandthe antioxi-dant/oxidativestressoutcomemeasuredalsovariedineach study.Thishighdegreeofvariationinmethods,aswellasthe heterogeneity in results, prevented using a meta-analytic approach. Therefore, direct extrapolations of the results shouldbemadewithextremecaution.
Oxidativestressisaphysiologicalconditionthat,inlow levels, can somehow be beneficial for the host, as it can
stimulatethegrowthofepithelialcellsandfibroblastsandkill some bacteria. However, oxidative stress can cause tissue damageasaconsequenceoftheabnormalincreaseinreactive oxygen species(ROS).10,38Neurodegenerative, inflammatory diseases, cancer, nutritional deficiency, diabetes and some psychiatricdisordersmaybeinvolvedwithabnormal produc-tion of ROS.39,40 Additionally, the mechanisms of tissue damage caused by ROS have been used to explain the relationshipbetweenperiodontitisandavarietyofsystemic diseases,suchasdiabetes,41mitochondrialdysfunction,42and metabolicsyndrome.43Intheperiodontium,different biologi-calmechanismsareresponsiblefortheincreaseinROSlevels, such as neutrophil infiltration, fibroblasts, osteoclasts and endothelialcells,whichresultsinbreakdownoftheepithelial structureanddamagetotheconnectivetissuesintheadjacent areas.25,44,45 Additionally, an in vitro study showed that
Fusobacteriumnucleatum,aperiodontopathogenicgram nega-tive bacterium, was able to stimulate ROSproduction and inducelipidperoxidation.46
AbnormalROSproduction can leadtophysiologicaland pathologicalconsequencesofhypoxia,impairmentofaerobic function, lysis of the cell membrane, DNA fragmentation, ischaemicinjury, inactivationofcertainproteolyticenzyme inhibitors, activation of proteolytic enzymes and, more drastically, cell death.42,47 These events might result in collagenolysisanddegradationofspecificextracellularmatrix components, such as hyaluronic acid and proteoglycans,47 whichcanpartiallyexplaintheetiopathogenesisof periodon-titis.
Antioxidantsexistineverybodyfluidandtissue,protecting against the damages of ROS.48 Antioxidants act against oxidative damagebydirectlyscavenging ROSandrepairing the damage caused by these harmful agents. In addition,
antioxidants act through down-regulation of some redox-sensitivepro-inflammatorygenetranscriptionfactorsand,at the same time, they regulate the anti-inflammatory gene transcription factors.4,48 Uricacid isthe mostpredominant antioxidantinsaliva,49anditslevelswillvaryaccordingtothe degree of saliva stimulation.17 The uric acid antioxidant activityincludesscavengingofsingletoxygenandhydroxyl radicals.4Thesecharacteristicsmayexplainwhyuricacidwas negativelycorrelatedwithreductionofgingivitisinoneofthe selected studies that used lycopene complimentarily to gingivitistreatment.32
Accordingtotheliterature,oneofthemostcommonlyused assaysformeasuringoxidativestressdamageis8-hydroxy-20 -deoxyguanosine(8-OHdG),whichisamarkerofDNAdamage derived from conversion of guanine to 8-hydroxyguanine, assessed by an enzyme linked immunosorbent assay (ELISA).25,50The levelsof8-OHdG insaliva wasfound tobe higherinsubjectswithchronicperiodontitiscomparedwith periodontallyhealthycontrols,24showingthat8-OHdG corre-lates reliably with the increase of ROS production during periodontalinflammation.Therefore,thisbiomarkerisreliable for evaluatingtheefficacy ofantioxidantson oxidantstress studies.51Twooftheselectedstudiesevaluatedtheeffectof complimentaryuseoflocallydeliveredlycopeneinperiodontal outcomes and also in the 8-OHdG levels.33,35 Both studies showedthatthreemonthsafterSRP,thelevelsof8-OHdGwere reduced in all sites. That decrease was significantly more pronounced in the sites that were treated with SRP and lycopene. However, in one ofthese studies, that difference wasobservedonlyoneweekaftertherapy,anditdisappeared afterthreemonths.33LocallydeliveredlycopeneandSRPwere alsorelatedtosignificantimprovementsinprobingdepthand clinical attachment levels in both studies. Lycopene, the carotenoidthatgives ripetomatoesabrightredcolour,isa naturalnon-enzymatic antioxidant thatexhibitsthehighest physicalquenchingratewith singlet oxygen.52Furthermore, lycopenealsoprotectsagainstDNAdamageinducedbyH2O2,53 decreasesthelevelsofgingivitis32andmayexertinhibitionon bacterial colonisation.54,55 All of these characteristics may explain the promising results from the studies that used lycopenecomplimentarily toSRP.However, theeffect ofan antioxidantagentin8-OHdGlevelsremainsunclear,andfurther studieswithdifferentantioxidantsshouldbeperformed.
Analysisoftotalantioxidantcapacity(TAOC)isthemost reliableoxidativestressoutcometoassesstheincapacityof antioxidantstoneutraliseROSandotherfreeradicals.56Two ofthe selected studies assessed TAOC using vitamin C or customiseddietaryinterventioncomplimentarilyto periodon-taltreatment.26,36ThestudythatusedvitaminCshowedthat SRP was capable of increasing TAOC levels, which was accompaniedbyimprovementinperiodontalindices,despite theappliedcomplimentarytherapy.However,thestudythat intended to increase the intake of antioxidants through customised dietary intervention showed that TAOC levels weresignificantlyincreasedafterthecomplimentarytherapy. Ontheotherhand,theimprovementsinperiodontalindices didnotreachstatisticallysignificantdifferencesamongthe testgroupandthegroupthatreceivedonlySRP.
Vitamin C(ascorbic acid) is anessential component of everylivingcell,anditsreducedusageisassociatedwithpoor
immunefunction.57Incontrast,higherintakeofvitaminCis associated with antiviral resistance and anti-carcinogenic effects and several other immune function improve-ments.58,59TheuseofvitaminCisassociatedwith stimula-tion of collagen fibre production andimmunomodulation functions, suchassignificant decreasesinserumlevelsof lipid peroxides andenhanced phagocytosis functions.59–61 Despite the benefits associated with vitamin C intake, significant improvements in periodontal indices were not demonstrated.Thisoutcomemightbebecauseascorbicacid actions in periodontal tissues are limited or because the optimal levelsofintakerequiredtomaintainanimproved immuneresponsetotreatorpreventinfectiousdiseaseshave notbeenassessed.59
Theingestionoffruits,vegetables,wholegrainproducts andalsolowerintakeoffoodwithsaturatedfatsandsugars arethefoundationofahealthyandbalanceddiet.62Intwoof the selected studies, the increased intake of fruits and vegetables, otherwise known as antioxidants agents, was obtained through individualised dietary intervention36 or through administration of capsules containing b-carotene, vitamin E, vitamin C and folic acid.31 It is known that b -carotene isefficientatscavenging singletoxygen,63and its levels aresignificantlylowerinperiodontitispatientswhen comparedtocontrolsubjects.64However,theanalysesfrom the selected studies showed that both types of dietary interventiondidnotpromoteadditionalperiodontal improve-mentslong-term,despiteitsbeneficialeffectsonantioxidant biomarkers(i.e.,b-caroteneandTAOC).
VitaminEisthemajorfat-solubleantioxidantpresentinall cellmembranes,anditreducesthelevelsoffreeradicalsand alsoexertssomeanti-inflammatorypropertieswith improve-mentsinthehumoralimmuneresponse.65–67Thisvitaminis essentialfornormalreproductioninhumans,developmentof muscles and a variety of physiological and biochemical functions.Inoneoftheselectedstudies,vitaminEwasused complimentarily to SRP. The group that received both therapiesshowedsignificantimprovementsinallperiodontal parameterswhencomparedtothegroupthatreceivedonly SRP.34Thedifferenceswerealsofollowedbyimprovementsin theSODactivityinseruminthetestgroup.Thepotential anti-inflammatoryeffectofvitaminEmaybeduetoitsinhibitionof prostaglandinbiosynthesis,68suppressionoftheproductionof proinflammatorycytokines,69adecreaseinC-reactiveprotein levels69andpreventionofactivationofnuclearfactor
kBby free radicals.69,70 Despite the significantly different results obtainedbySinghetal.,34itisimportanttohighlightthatthe meandifferencesbetweencontrolandtestgroupsweresmall andmightnothaveanyclinicalimpact.Additionally,vitamin E isknowntoinduceanxietyinratswithligature-induced periodontitis.71Therefore,theseconditionsshouldbe consid-eredbeforethecomplimentaryuseofvitaminEinperiodontal treatment.
5.
Conclusions
Thissystematicreviewsuggestedthatuseofanantioxidant, complimentary treatment for periodontal disease has the potentialtoimproveperiodontalclinicalparameters. Howev-er,theimpactofthecombinationofperiodontaltherapywith antioxidantsintermsofantioxidant/oxidativestress param-etersrequiresfurtherinvestigation.
Authors’
contribution
F.W.M.G. Muniz selected the studies, extracted the data, analyzedthedataandwrotethemanuscript.S.B.Nogueira selectedthestudies,extractedthe data,analyzedthedata and wrote the manuscript. F.L.V. Mendes reviewed the manuscriptandhelpedwiththeliteraturereviewanddata analysis. C.K.Ro¨singreviewedthe manuscriptandhelped with the literature review and data analysis. M.M.S.M. Moreira reviewed the manuscript and helped with the literature review, data analysis and search strategy. G.M. de Andrade reviewed the manuscript and helped data analysis. R.D.S. Carvalho developed the review protocol, reviewed the manuscript and helped with the literature review,dataanalysisandsearchstrategy.Shealsohelpedin theselectionofthestudies.
Funding
None.
Competing
interests
Nonedeclared.
Ethical
approval
Notrequired.
r
e
f
e
r
e
n
c
e
s
1. AmericanAcademyofPeriodontology.Parameteron chronicperiodontitiswithslighttomoderatelossof periodontalsupport.JPeriodontol2000;71(5Suppl.):853–5.
2. EbersoleJL,TaubmanMA.Theprotectivenatureofhost responsesinperiodontaldiseases.Periodontology
2000;1994(5):112–41.
3. KornmanKS.Mappingthepathogenesisofperiodontitis:a newlook.JPeriodontol2008;79(8Suppl.):1560–8.
4. ChappleIL,MatthewsJB.Theroleofreactiveoxygenand antioxidantspeciesinperiodontaltissuedestruction.
Periodontol2000;43:160–232.
5.KiyoshimaT,EnokiN,KobayashiI,SakaiT,NagataK,Wada H,etal.Oxidativestresscausedbyalowconcentrationof hydrogenperoxideinducessenescence-likechangesin
mousegingivalfibroblasts.IntJMolMed2012;30(5): 1007–12.
6. ChappleIL.Reactiveoxygenspeciesandantioxidantsin inflammatorydiseases.JClinPeriodontol1997;24(5):287–96.
7. HalliwellB,WhitemanM.Measuringreactivespeciesand oxidativedamageinvivoandincellculture:howshould youdoitandwhatdotheresultsmean?BrJPharmacol
2004;142:231–55.
8. BartoldPM,WiebkinOW,ThonardJC.Theeffectof oxygen-derivedfreeradicalsongingivalproteoglycansand hyaluronicacid.JPeriodontalRes1984;19(4):390–400.
9. KaklamanosEG,TsalikisL.Areviewonperi-implant crevicularfluidassayspotentialinmonitoringand predictingperi-implanttissueresponses.JIntAcad Periodontol2002;4(2):49–59.
10.BattinoM,BullonP,WilsonM,NewmanH.Oxidativeinjury andinflammatoryperiodontaldiseases:thechallengeof anti-oxidantstofreeradicalsandreactiveoxygenspecies.
CritRevOralBiolMed1999;10(4):458–76.
11.AkalinFA,TokluE,RendaN.Analysisofsuperoxide dismutaseactivitylevelsingingivaandgingivalcrevicular fluidinpatientswithchronicperiodontitisand
periodontallyhealthycontrols.JClinPeriodontol2005;32: 238–43.
12.KimSC,KimOS,KimOJ,KimYJ,ChungHJ.Antioxidant profileofwholesalivaafterscalingandrootplaningin periodontaldisease.JPeriodontalImplantSci2010;40(4): 164–71.
13.ScandaliosJG.Oxidativestress:molecularperceptionand transductionofsignalstriggeringantioxidantgene defenses.BrazJMedBiolRes2005;38:995–1014.
14.DaiyaS,SharmaRK,TewariS,NarulaSC,KumarSehgalP. Micronutrientsandsuperoxidedismutasein
postmenopausalwomenwithchronicperiodontitis:apilot interventionalstudy.JPeriodontalImplantSci2014;44(4): 207–13.
15.IbrahimW,LeeUS,YenHC,StClairDK,ChowCK. Antioxidantandoxidativestatusintissuesofmanganese superoxidedismutasetransgenicmice.FreeRadicBiolMed
2000;28(3):397–402.
16.TrivediS,LalN,MahdiAA,SinghB,PandeyS.Associationof salivarylipidperoxidationlevels,antioxidantenzymes,and chronicperiodontitis.IntJPeriodonticsRestorDent
2015;35(2):e14–9.
17.ChappleIL,BrockG,EftimiadiC,MatthewsJB.Glutathione ingingivalcrevicularfluidanditsrelationtolocal
antioxidantcapacityinperiodontalhealthanddisease.Mol Pathol2002;55(6):367–73.
18.PriorRL.Fruitsandvegetablesinthepreventionofcellular oxidativedamage.AmJClinNutr2003;78(3Suppl):570S–8S.
19.PlatelK,SrinivasanK.Bioavailabilityofmicronutrientsfrom plantfoods:anupdate.CritRevFoodSciNutr2015.[inpress], PMID:25748063.
20.ZhaoM,LiuX,LuoY,GuoH,HuX,ChenF.Evaluationof protectiveeffectoffreeze-driedstrawberry,grape,and blueberrypowderonacrylamidetoxicityinmice.JFoodSci
2015;80(4):H869–74.PMID:25754417.
21.KopecRE,CooperstoneJL,SchweiggertRM,YoungGS, HarrisonEH,FrancisDM,etal.Avocadoconsumption enhanceshumanpostprandialprovitaminAabsorptionand conversionfromanovelhigh-b-carotenetomatosauceand fromcarrots.JNutr2014;144(8):1158–66.
22.ChandraHM,ShanmugarajBM,SrinivasanB,Ramalingam S.Influenceofgenotypicvariationsonantioxidant propertiesindifferentfractionsoftomato.JFoodSci
2012;77(11).C1174–8.
oxidativestress.JSportsMedPhysFit2014.[inpress],PMID: 24921623.
24.SezerU,CicekY,CanakciCF.Increasedsalivarylevelsof 8-hydroxydeoxyguanosinemaybeamarkerfordisease activityforperiodontitis.DisMarkers2012;32:165–72.
25.TakaneM,SuganoN,IwasakiH,IwanoY,ShimizuN,ItoK. NewbiomarkerevidenceofoxidativeDNAdamageinwhole salivafromclinicallyhealthyandperiodontallydiseased individuals.JPeriodontol2002;73(5):551–4.
26.AbouSulaimanAE,ShehadehRM.Assessmentoftotal antioxidantcapacityandtheuseofvitaminCinthe treatmentofnon-smokerswithchronicperiodontitis.J Periodontol2010;81(11):1547–54.
27.BaltaciogluE,AkalinFA,AlverA,BalabanF,UnsalM, KarabulutE.Totalantioxidantcapacityandsuperoxide dismutaseactivitylevelsinserumandgingivalcrevicular fluidinpost-menopausalwomenwithchronic
periodontitis.JClinPeriodontol2006;33:385–92.
28.BrockGR,ButterworthCJ,MatthewsJB,ChappleIL.Local andsystemictotalantioxidantcapacityinperiodontitisand health.JClinPeriodontol2004;31:515–21.
29.RamfjordSP,KnowlesJW,NissleRR,BurgettFG,ShickRA. Resultsfollowingthreemodalitiesofperiodontaltherapy.J Periodontol1975;46(9):522–6.
30.BostanciV,TokerH,SenelS,OzdemirH,AydinH.Effectof chronicperiodontitisonserumandgingivalcrevicularfluid oxidantandantioxidantstatusinpatientswithfamilial Mediterraneanfeverbeforeandafterperiodontaltreatment.
JPeriodontol2014;85(5):706–12.
31.ChappleIL,MilwardMR,Ling-MountfordN,WestonP, CarterK,AskeyK,etal.Adjunctivedailysupplementation withencapsulatedfruit,vegetableandberryjuicepowder concentratesandclinicalperiodontaloutcomes:a double-blindRCT.JClinPeriodontol2012;39(1):62–72.
32.ChandraRV,PrabhujiML,RoopaDA,RavirajanS,Kishore HC.Efficacyoflycopeneinthetreatmentofgingivitis:a randomised,placebo-controlledclinicaltrial.OralHealth PrevDent2007;5(4):327–36.
33.ChandraRV,SrinivasG,ReddyAA,ReddyBH,ReddyC, NagarajanS,etal.Locallydeliveredantioxidantgelasan adjuncttononsurgicaltherapyimprovesmeasuresof oxidativestressandperiodontaldisease.JPeriodontalImplant Sci2013;43(3):121–9.
34.SinghN,ChanderNarulaS,KumarSharmaR,TewariS, KumarSehgalP.VitaminEsupplementation,superoxide dismutasestatus,andoutcomeofscalingandrootplaning inpatientswithchronicperiodontitis:arandomizedclinical trial.JPeriodontol2014;85(2):242–9.
35.ChandraRV,SandhyaYP,NagarajanS,ReddyBH,NaveenA, MurthyKR.Efficacyoflycopeneasalocallydeliveredgelin thetreatmentofchronicperiodontitis:smokersvs nonsmokers.QuintessenceInt2012;43:401–11.
36. ZareJavidA,SealCJ,HeasmanP,MoynihanPJ.Impact ofacustomiseddietaryinterventiononantioxidant status,dietaryintakesandperiodontalindicesinpatients withadultperiodontitis.JHumNutrDiet2014;27(6): 523–32.
37.Antczak-BouckomsAA,TullochJF,BerkeyCS.Split-mouth andcross-overdesignsindentalresearch.JClinPeriodontol
1990;17(7Pt1):446–53.
38.KlebanoffSJ.Oxygenmetabolismandthetoxicpropertiesof phagocytes.AnnInternMed1980;93(3):480–9.
39.AzziA,GysinR,KempnaP,MunteanuA,NegisY,Villacorta L,etal.VitaminEmediatescellsignalingandregulationof geneexpression.AnnNYAcadSci2004;1031:86–95.
40.ShiraiM,KawaiY,YamanishiR,TeraoJ.Approachtonovel functionalfoodsforstresscontrol5,Antioxidantactivity profilesofantidepressantherbsandtheiractive components.JMedInvest2005;52(Suppl.):249–51.
41.SugiyamaS,TakahashiSS,TokutomiFA,YoshidaA, KobayashiK,YoshinoF,etal.Gingivalvascularfunctions arealteredintype2diabetesmellitusmodeland/or periodontitismodel.JClinBiochemNutr2012;51:108–13.
42.GovindarajP,KhanNA,GopalakrishnaP,ChandraRV, VanniarajanA,ReddyAA,etal.Mitochondrialdysfunction andgeneticheterogeneityinchronicperiodontitis.
Mitochondrion2011;11:504–12.
43.MarchettiE,MonacoA,ProcacciniL,MummoloS,GattoR, TeteS,etal.Periodontaldisease:theinfluenceofmetabolic syndrome.NutrMetab(Lond)2012;9:88.
44.TakaneM,SuganoN,EzawaT,UchiyamaT,ItoK.Amarker ofoxidativestressinsaliva:associationwith periodontally-involvedteethofahopelessprognosis.JOralSci
2005;47(1):53–7.
45.AgnihotriR,PandurangP,KamathSU,GoyalR,BallalS, ShanbhogueAY,etal.Associationofcigarettesmokingwith superoxidedismutaseenzymelevelsinsubjectswith chronicperiodontitis.JPeriodontol2009;80(4):657–62.
46.SheikhiM,BouhafsRK,HammarstromKJ,JarstrandC.Lipid peroxidationcausedbyoxygenradicalsfromFusobacterium -stimulatedneutrophilsasapossiblemodelforthe emergenceofperiodontitis.OralDis2001;7(1):41–6.
47.JacobyBH,DavisWL.Theelectronmicroscopic
immunolocalizationofacopper-zincsuperoxidedismutase inassociationwithcollagenfibersofperiodontalsoft tissues.JPeriodontol1991;62(7):413–20.
48.HalliwellB.Reactiveoxygenspeciesinlivingsystems: source,biochemistry,androleinhumandisease.AmJMed
1991;91(3C):14S–22S.
49.MooreS,CalderKA,MillerNJ,Rice-EvansCA.Antioxidant activityofsalivaandperiodontaldisease.FreeRadicRes
1994;21(6):417–25.
50.SawamotoY,SuganoN,TanakaH,ItoK.Detectionof periodontopathicbacteriaandanoxidativestressmarkerin salivafromperiodontitispatients.OralMicrobiolImmunol
2005;20:216–20.
51.CanakciCF,CicekY,YildirimA,SezerU,CanakciV. Increasedlevelsof8-hydroxydeoxyguanosineand malondialdehydeanditsrelationshipwithantioxidant enzymesinsalivaofperiodontitispatients.EurJDent
2009;3(2):100–6.
52.DiMascioP,KaiserS,SiesH.Lycopeneasthemostefficient biologicalcarotenoidsingletoxygenquencher.ArchBiochem Biophys1989;274:532–8.
53.SinghM,KrishanappaR,BagewadiA,KeluskarV.Efficacyof orallycopeneinthetreatmentoforalleukoplakia.OralOncol
2004;40:591–6.
54.DarveauRP,TannerA,PageRC.Themicrobialchallengein periodontitis.Periodontology20001997;14:12–32.
55.KornmanKS,PageRC,TonettiMS.Thehostresponsetothe microbialchallengeinperiodontitis:assemblingthe players.Periodontology20001997;14:33–53.
56.WoodfordFP,WhiteheadTP.Ismeasuringserum antioxidantcapacityclinicallyuseful?AnnClinBiochem
1998;35(Pt1):48–56.
57.SchwagerJ,SchulzeJ.Modulationofinterleukinproduction byascorbicacid.VetImmunolImmunopathol1998;64:45–57.
58.CampbellJD,ColeM,BunditrutavornB,VellaAT.Ascorbic acidisapotentinhibitorofvariousformsofTcellapoptosis.
CellImmunol1999;194:1–5.
59.FieldCJ,JohnsonIR,SchleyPD.Nutrientsandtheirrolein hostresistancetoinfection.JLeukocBiol2002;71(1):16–32.
60.delaFuenteM,FerrandezMD,BurgosMS,SolerA,PrietoA, MiquelJ.Immunefunctioninagedwomenisimprovedby ingestionofvitaminsCandE.CanJPhysiolPharmacol
1998;76(4):373–80.
messengerRNAlevelsinhumanskinfibroblast.JInvest Dermatol1988;90(4):420–4.
62.CrollJK,Neumark-SztainerD,StoryM.Healthyeating:what doesitmeantoadolescents?JNutrEduc2001;33(4):193–8.
63.DeanRT,FuS,StockerR,DaviesMJ.Biochemistryand pathologyofradical-mediatedproteinoxidation.BiochemJ
1997;324(Pt1):1–18.
64.LindenGJ,McCleanKM,WoodsideJV,PattersonCC,Evans A,YoungIS,etal.Antioxidantsandperiodontitisin 60–70-year-oldmen.JClinPeriodontol2009;36:843–9.
65.CohenME,MeyerDM.EffectofdietaryvitaminE
supplementationandrotationalstressonalveolarboneloss inricerats.ArchOralBiol1993;38:601–6.
66.BeckMA,KolbeckPC,RohrLH,ShiQ,MorrisVC,Levander OA.VitaminEdeficiencyintensifiesthemyocardialinjuryof coxsackievirusB3infectionofmice.JNutr1994;124(3): 345–58.
67.EhrlichHP,TarverH,HuntTK.Inhibitoryeffectsofvitamin Eoncollagensynthesisandwoundrepair.AnnSurg
1972;175(2):235–40.
68.LikoffRO,GuptillDR,LawrenceLM,McKayCC,MathiasMM, NockelsCF,etal.VitaminEandaspirindepress
prostaglandinsinprotectionofchickensagainst
Escherichiacoliinfection.AmJClinNutr1981;34(2):245–51.
69.NazrunAS,NorazlinaM,NorlizaM,NirwanaSI.The anti-inflammatoryroleofvitaminEinpreventionof
osteoporosis.AdvPharmacolSci2012;2012:142702.
70.ManiamS,MohamedN,ShuidAN,SoelaimanIN.Palm tocotrienolexertedbetterantioxidantactivitiesinbonethan alpha-tocopherol.BasicClinPharmacolToxicol2008;103:55–60.