www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
ORIGINAL
ARTICLE
Influence
of
body
position
on
the
displacement
of
nasal
prongs
in
preterm
newborns
receiving
continuous
positive
airway
pressure
Marisa
Afonso
Andrade
Brunherotti
a,∗,
Francisco
Eulógio
Martinez
baHealthPromotionProgram,UniversidadedeFranca(Unifran),Franca,SP,Brazil
bFaculdadedeMedicinaRibeirãoPreto,UniversidadedeSãoPaulo(USP),RibeirãoPreto,SP,Brazil
Received21September2014;accepted18January2015 Availableonline27June2015
KEYWORDS
Prematureinfant; Continuouspositive airwaypressure; Supineposition; Proneposition
Abstract
Objective: Toevaluatetheinfluenceofbodypositiononthedisplacementofnasalprongsin
preterminfants.
Methods: Thisprospective,randomized,crossoverstudyenrolledinfantsbornatamean
ges-tationalageof29.7±2weeks,birthweightof1353±280gand2.9±2.2daysoflife,submitted
tocontinuouspositiveairwaypressurebynasalprongs.Themainoutcomewasthenumberof
timesthatthenasalprongsweredisplacedfollowinginfantpositioninginthefollowingbody
positions:prone,rightlateral,leftlateral,andsupine,accordingtoapre-establishedrandom
order.Moreover,cardiorespiratoryvariables(respiratoryrate,heartrate,andoxygen
satura-tion)wereevaluatedforeachbodyposition.Dataforeachpositionwerecollectedevery10min,
overaperiodof60min.Anoccurrencewasdefinedwhenthenasalprongsweredisplacedfrom
thenostrilsafter3mininthedesiredposition,requiringinterventionoftheexaminer.
Results: Amongthe16studiedinfants,theoccurrenceofnasalprongdisplacementwasonly
observedintheproneposition(9infants---56.2%)andintheleftlateralposition(2infants
---12.5%).Thenumberoftimesthattheprongsweredisplacedwas11intheproneposition(7
withinthefirst10min)and2intheleftlateralposition(1withinthefirst10min).Noclinically
significantchangeswereobservedinthecardiorespiratoryvariables.
Conclusions: Maintenance of the nasal prongs to provide adequate noninvasive respiratory
supportwasharderintheproneposition.
© 2015Sociedadede Pediatria de SãoPaulo. Published by Elsevier Editora Ltda.All rights
reserved.
DOIoforiginalarticle:http://dx.doi.org/10.1016/j.rpped.2015.01.005
∗Correspondingauthor.
E-mail:brunherotti@uol.com.br(M.A.A.Brunherotti).
PALAVRAS-CHAVE
Recém-nascido prematuro; Pressãopositiva contínuanasvias aéreas;
Decúbitodorsal; Decúbitoventral
Influênciadaposic¸ãocorporalnodeslocamentodapronganasalemrecém-nascido
pré-termoempressãopositivacontínuaemviasaéreas
Resumo
Objetivo: Analisarainfluênciadaposic¸ãocorporalnodeslocamentodapronganasalem
recém-nascidospré-termos.
Métodos: Estudoprospectivo,randomizadoetipocrossover.Foramestudadosrecém-nascidos
com média de idade gestacional de 29,7±2semanas, peso de nascimento de 1.353±280g,
2,9±2,2diasdevidaeemusodapressãopositivacontínuadeviasaéreas.Avaliou-seonúmero
devezesemqueodispositivonasalsofreudeslocamento,alémdevariáveiscardiorrespiratórias,
comofrequênciarespiratória,cardíacaesaturac¸ãodeoxigênio,conformeacrianc¸afoi
colo-cadanasposic¸õescorporaisprona,lateraldireita,lateralesquerdaesupina,segundoordem
aleatóriapreviamenteestabelecida.Asinformac¸õesemcadaposic¸ãoforamcoletadasacada
10minutos,por60minutos.Foiconsideradaocorrênciaquandoodispositivonasalsedeslocou
doorifíciodasnarinas,apósoperíododetrêsminutosnaposic¸ãodesejada,ehouvenecessidade
deintervenc¸ãodoexaminador.
Resultados: Nas16crianc¸asestudadas,odeslocamentododispositivonasalocorreusomente
nasposic¸õesprona(novecrianc¸as---56,2%)elateralesquerda(duascrianc¸as---12,5%).Apronga
se deslocou11vezes naposic¸ãoprona, setedelasnosprimeirosdezminutos,eduasvezes
naposic¸ãolateralesquerda,uma nosprimeirosdezminutos.Nãosedetectaramalterac¸ões
clinicamentesignificativasnasvariáveiscardiorrespiratórias.
Conclusões: Aposic¸ãopronamostroumaiordificuldadeparasemanterodispositivonasalde
suportepressóriconãoinvasivonaformaadequada.
© 2015Sociedadede Pediatriade SãoPaulo. Publicado porElsevier Editora Ltda.Todosos
direitosreservados.
Introduction
Nasal prongs area type of device usedin infants receiv-ingnoninvasivepressuresupportthroughcontinuouspositive airway pressure (CPAP). Nasal CPAP is frequently used in preterminfantsatbirthoraftermechanicalventilation dis-continuation.
Some advantages of using nasal CPAP as first choice ofventilatory supporthave been demonstrated,suchasa decreaseintheneedforinvasiveventilatorysupport,better pulmonarymechanicsresultsandreducedrespiratorywork.1
Thissupport,whenusedaftertrachealextubation,is indi-catedbytheBrazilianConsensusonMechanicalVentilation as level ‘‘A’’ of evidence.2 Therefore,the neonatalcare
teamshouldbeencouragedtousethesystem.
Theprofessionalteaminvolvedinneonatalcareiscritical tothesuccessofthenasalCPAPtechnique.Adequate knowl-edgeofthetechniquebytheteamandcaredirectedtothe nasaldevicehandlingallowthedecreaseincomplications, suchasnasalseptallesions,nasalbleedingsandinadequate prongpositioning.3
Proper positioning of the nasal prongs is the one that does not deform the face, does not compress the nasal septumanddoes notallowthe displacementofthe inter-faceinsidethenostrils.4Inadequatepositioningofthenasal
devicegeneratesincreasingpressureinthecolumella, caus-ingreducedbloodflowandaconsequentrisk forischemia andtissuedamage.5Thus,itisimportanttopayattentionto
thepositioningofthenasalprongsinapreventivemanner, inordertoreducetheincidenceofnasallesionsinducedby thedevice.6
Inordertoattainbetterdevicefixationandstabilityon thefaceand in anattempt tokeepthe nasalCPAP inter-faceproperlyandcomfortablypositioned, severalfixation models have been developed. However, scientific studies havenot describedwhether acertainbodypositioncould facilitateorhinderthepermanenceofnasalprongsinthe correct place. The body positioning could influence the correctpermanence of the prongs, asthe adequate body positionhasshowntobeimportantincertainclinical situa-tions,suchasincreasedgastricvolume,7incasesofapnea8
orforthesleeprhythm9oftheinfant.
Therefore,thisstudyaimedtoanalyzetheinfluenceof bodypositioningonthenasalprongdisplacementinpreterm infantsduringnasalCPAPuse.
Method
Thestudydesignwasanalytical,prospective,crossoverand observational, carried out between January and Decem-ber 2009. The assessed preterm infants were followed at the Pediatric Intensive Care sector of a tertiary pub-lic hospital. The study was approved by the Institutional Review Board,protocol #024/2008. The informedconsent formswereshowntoandsignedbytheinfants’parentsor guardians.
neonatesthat showedagitatedbodymovements, continu-ouscryingandcontractedfacialexpressiondemonstrating painwereexcluded.
NasalCPAPwasappliedusingHudson®(HudsonRCIinfant
nasalCPAPcannulasystem,TeleflexIncorporated,USA) sili-conizednasalprongs.Allnewbornsreceivedhydrocolloidin thenostrils,keepingtheorificesopenfortheintroduction ofthenasalprongs.Thesizeoftheprongswaschosenbased onthereferencetableprovidedbythemanufacturer,which associatesthechild’sweightwiththerecommended diame-terofthedevice,withalloftheprongsbeingwelladapted tothenostrils.
FornasalCPAP,thegases werehumidifiedandwarmed andthefractionof inspiredoxygen wascontrolledbythe oxygenblender.Theprematureinfantswerestable, requir-ingamaximumof 30%oxygenandpositive-endexpiratory pressure (PEEP) no higher than 6cmH2O, with little
con-tinuousflowvariationfrom7to8L/min.Themeanairway pressuremeasuredattheventilatordidnotexceed7cmH2O.
Theinfantswereplacedinthefollowingpositions:supine (A), right lateral (B), prone (C) and left lateral (D) posi-tion,evaluatedaccordingtothecriteriaofcrossovertrials.10
Eachchildwasrandomlyplacedintheabovementionedbody positions,beginning withthe sequence position.The pos-sible sequences of body positions were organized aiming nottorepeattheorderofdecubitus,thus beingselected: Sequence1(A,D,C,B);Sequence2(C,A,B,D);Sequence 3(B,C,D,A),Sequence4(D,B,A,C).
The foursequenceswere randomizedinto fourgroups, so that each selected child was allocated toa sequence of positions according to the previous drawing of lots. Theinfantremainedfor 60minineach bodyposition.The studybegan 1h after feeding, whichwas offeredthrough an orogastric tube. When the child wasfed between the positioningmaneuvers,a1-hintervalwasallowedfor place-ment in the study position. All infants were followed by thesameexaminerinordertomaintainthesamepositions
forallinfants.Thebodypositionsthatneededcushion sup-port were the leftand right lateral positions. During the observationperiod,theinfantswerenotsubmittedtoany manipulation.
An occurrence was considered when the nasal device wasdisplacedfromtheorificeofthenostrilsafter3minin the desiredposition,requiring repositioning bythe exam-iner. We analyzed the number of occurrences within 1h ofobservationof eachbodypositionperinfant.Moreover, cardiorespiratoryvariableswereobserved:respiratoryrate, measuredbyobservingthechestforafullminute,heartrate andoxygensaturation, bothusingtheDixtal-DX2010 mon-itor with neonatalsensor located at the foot. Data were collectedevery10minduring60min,withatotalofseven collectionsforeveryposition.
The sample was selected by convenience, as it is a homogeneous group. However, sample calculation was subsequently employed to estimate the proportion, with permissibleestimationerrorof5%.Thecharacteristicsofthe studygroupweredescriptivelyshownasmeanandstandard deviation.To comparetheoccurrenceof nasaldevice dis-placement,accordingtobodyposition,thechi-squaretest wasappliedtothecontingencytablerelatedtothe occur-rence,withp<0.05beingconsidered significant.Todetect possible differences in cardiorespiratoryindicators among thefourgroups,analysisofvariancewasusedforrepeated measures,usingthesoftwareStatistica7.0.
Results
Atotalof19infantsbornduringthestudy periodmetthe inclusion criteriaand were eligible for the study; 3 were excluded. Twonewborns wereagitatedandcried continu-ouslybeforedatacollectionstartedandone,aftercollection ofdataonthefirstbodypositionofthesequence,required venipuncture,becomingagitated.Therefore,westudied16 preterm infants, whowere randomly assignedto each of
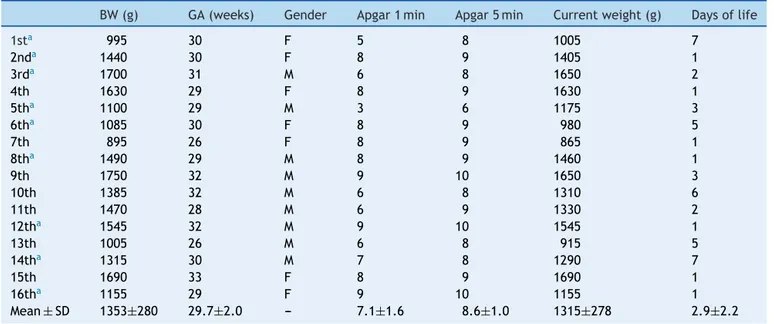
Table1 Generalcharacteristicsofpreterminfantsstudied.
BW(g) GA(weeks) Gender Apgar1min Apgar5min Currentweight(g) Daysoflife
1sta 995 30 F 5 8 1005 7
2nda 1440 30 F 8 9 1405 1
3rda 1700 31 M 6 8 1650 2
4th 1630 29 F 8 9 1630 1
5tha 1100 29 M 3 6 1175 3
6tha 1085 30 F 8 9 980 5
7th 895 26 F 8 9 865 1
8tha 1490 29 M 8 9 1460 1
9th 1750 32 M 9 10 1650 3
10th 1385 32 M 6 8 1310 6
11th 1470 28 M 6 9 1330 2
12tha 1545 32 M 9 10 1545 1
13th 1005 26 M 6 8 915 5
14tha 1315 30 M 7 8 1290 7
15th 1690 33 F 8 9 1690 1
16tha 1155 29 F 9 10 1155 1
Mean±SD 1353±280 29.7±2.0 --- 7.1±1.6 8.6±1.0 1315±278 2.9±2.2
Table2 Number ofnewborns requiring re-position ofthe nasal device duringthe seven observations for each evaluated decubitus.
Supine Prone Rightlateral Leftlateral p
Correctionofdevice 0 09(56.2%)a 0(0.0%) 2(12.5%) 0.001
pvalueaccordingtochi-squaretest.
a Thepronepositionwasassociatedwithahigherfrequencyofdisplacementofthenasaldevice(p=0.001)whencomparedtoother evaluateddecubitus.
1 0 1 2 3 4 5 6
60 50 40 30 20 10
Minutes in the body position
Number of occurrences
Left lateral Prone
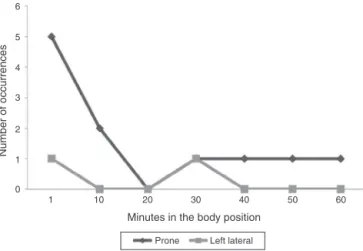
Figure1 Periodofoccurrenceofnasaldisplacementinthe
bodypositionsofthe11infants.
thefourpreviouslyestablishedsequences.Allinfantswere appropriateforgestationalageandtheirmain characteris-ticsareshowninTable1.
Foreach evaluation period,we verifiedthe numberof correctionsofthedoublenasalprongininfantsindifferent bodypositions.Table2showsthenumberofinfantsinwhom displacementofthedoublenasalprongoccurredindifferent bodypositions,inallassessed periods.Theproneposition showedahigherincidenceofnasaldevicedisplacement.In thisgroup,ninechildren(56.2%)requiredtheinterventionof theexaminerforthedevicerepositioning.Whencomparing theoccurrenceof nasaldevice displacementbetween the fourposturalpositions,thepronepositionshowedagreater numberofdisplacements,whichwasstatisticallysignificant (p=0.001)whencomparedtotheotherpositions.Inthefirst
10min of observation,therewere seven displacementsin thepronepositioninseveninfantsandoneintheleftlateral position.Intotal,therewere11devicedisplacementsinthe pronepositionand2intheleftlateralposition(Fig.1).
Themeanvaluesfoundforthecardiorespiratory indica-tors in the four body positions were withinthe expected normal range.The difference between the minimum and maximumvaluesofrespiratoryratewas30---47inspirations; forheartrate,38---50beatsperminuteandforoxygen satu-ration,of4---6%.Thelowestvariationswereobservedinthe leftlateralposition.Therewerenodifferencesbetweenthe cardiorespiratoryresultsattheseventimes observedwith thedifferentgroups(Table3).
Discussion
ThenasalCPAPtechniquesuccessisdirectlyassociatedwith theadequateuseofthenasaldevice.Whenthenasaldevice is displaced from the nostrils, there is need for correc-tionbythehealthteam.Therefore,theteammustbevery attentive and available for these corrections. The risk of nasalcomplicationsincreaseswhenthedeviceisnot main-tainedintheadequate positionandmaycausehyperemia and/ornasalbleeding.11Abodypositionthatresultsin
bet-ter adaptation and fewer correctionsof the nasal device could improve the technique success and give the team peaceofmind.
Inthepresentstudy,weanalyzedtheinfluenceofbody positionon the nasaldevice adequacy in preterm infants using nasal CPAP. The two body positions that required device correction in the nostrils were the prone (56.2%) andtheleftlateralpositions(12.5%).Regardingtheprone position,the CPAP circuit was in direct contactwith the
Table3 Cardiorespiratoryvariablesandinteractionbetweenbodypositionsandtimefrom11preterminfantsthatrequired
correctionofthenasaldevice,inmean±standarddeviation(minimumandmaximumvalues).
Supine(S) Prone(P) Rightlateral(RL) Leftlateral(LL) p-valuea
Respiratoryrate(ipm) 0.805
Mean±SD 39.7±10.6 38.1±8.3 39.0±9.7 37.7±6.6
Minimum---maximum 22---69 23---64 17---60 27---57
Heartrate(bpm) 0.970
Mean±SD 134.2±10.4 138.1±11.9 137.9±8.8 138.0±9.9
Minimum---maximum 110---159 110---160 110---155 120---158
Oxygensaturation(%) 0.976
Mean±SD 134.2±10.4 97.6±1.0 97.1±1.4 97.3±1.0
Minimum---maximum 93---99 95---100 94---100 95---99
bed,asnewbornsinthepronepositionremainedwith cervi-calrotationtotheleftside,withthefacebeingsupported by the bed. This factor could bring some disadvantages. When the infant moved the cervical spine joint, the bed itselffunctioned asan obstacleto thedevice, prompting itsdisplacement.Themomentofdevicedisplacementwas verified, with greater need for correction of the double nasal prong in the first 10min. It is possible that, in the proneposition,thecompressionofthenasaldeviceonthe face worked asa stimulus, triggering automatic response movementsofthecervicalspineandcausingdisplacement
of the double nasal prong. After some time, sensory
accommodationmay haveoccurred. However,despitethe reductionin dislocations,thesecontinued tooccur inthe pronepositionduring theentire 60min of observation.In the left lateral position, the displacement of the nasal deviceoccurredonlyintwoinfantsandatdifferenttimes; thus,thereisnojustificationtoassociatethispositionwith theoccurrenceofCPAPdisplacement.
Nostudy describedin theliterature hasassessednasal devicedisplacement indifferentbodypositions. Regoand Martinez11 evaluatedthe permanence of thenasal device
according to the model used and the child’s weight. Newbornsweighingbetween1500and2500gweremore dif-ficulttomaintainadequatelyconnectedtothenasalCPAP (p=0.04), when compared with those whose weight was
≤1000g.Thenumberoftimesthedevicewasdisplacedfrom thenostrilpertimeunitwasnotassociatedwiththelength ofstayinnasalCPAP.
Well-positionednasal prongs without displacement can resultinlowerriskofnasalinjuryandensurelesslossof con-tinuouspositiveairwaypressure.Therefore,bodyposition isdirectlyrelatedtofactorsthatinterferewithnasalCPAP response.The bodypositionthatreceivesgreater empha-sisinprematureinfantsistheproneposition,whichseems toyieldbestoxygensaturationresults.Studieshaveshown thatnewborns inthelateweaningprocessrespondedwith increasedoxygensaturationwhenmaintainedintheprone position.12,13
Heimann et al.8 evaluated episodes of desaturation in
18preterm infantsbreathing spontaneously. Inthesupine position,whencomparedwiththeprone,thereweremore episodesof moderate(between85%and80%, p=0.04)and severedesaturation(<80%;p=0.03).The proneandsupine positions were also object of study in infants with and without use of supplemental oxygen at postnatal age of 2---10weeks.Thefollowedgroupwasdividedinto10infants usingoxygentherapy(30weeks;1.175g)and10 non-oxygen-dependent infants (31 weeks and 1.589g). The oxygen saturationvaluesinthepronepositionwerehigherthanin thesupineposition(p=0.01)in theoxygen-therapy group. The oxygen saturation values remained between 94% and 97%inthepronepositionandbetween94%and95%inthe supineposition.Amongthenon-oxygen-dependentinfants, therewasnostatisticaldifference(p=0.25).14
Inapreviousstudy,weobservedthatthesupineposition couldbe thebest choice for prematurenewborns receiv-ingnasalCPAP.Oxygensaturationandrespiratoryandheart rate indicators were assessed in the four body positions (prone,supine,rightandleftlateralpositions)inpremature newborns usingnasal CPAP. The indicators showed similar behavior, not demonstrating a position of preference for
preterminfantsinstableconditionandwelladaptedtothe continuous positive airway pressure system; however, the leftandrightlateralpositionswereless beneficialfor the oxygensaturationindicator.15Thepresentstudyalsoshowed
nodifferencesbetweenbodypositioningand cardiorespira-toryindicators assessedininfants thatunderwentposition correctionofthenasaldevice.
Itwasnotpossibletoidentifyintheliteratureother stud-iesthat evaluatedthe occurrence of displacement of the nasalCPAP deviceinchildren.The studysample consisted of16infantsandweconsideritslowsamplepowerasone of the main study limitations. Additionally, the profile of the selected infants, which were clinicallystable and,at thetimeofobservation,werecalmandnotundergoingany manipulation,mayhavefavoredthelowerdisplacementof thenasaldevice.
Thisstudy demonstratedthat thepronepositionis the most difficult one to maintain the noninvasive device of nasalpressuresupportadequatelypositionedinpremature infants in stable clinical condition. Displacement occurs especiallyinthefirst10minafterbodypositioning.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.RoehrCC,ProquittéH,Hammer H,et al. Positiveeffects of earlycontinuouspositiveairwaypressureonpulmonary func-tion in extremely premature infants: results of a subgroup analysisoftheCOIN trial.Arch DisChildFetal NeonatalEd. 2011;96:F371---3.
2.MorettiC,GianniniL, FassiC,etal.Nasalflow-synchronized intermittentpositivepressureventilationtofacilitateweaning in very low-birthweight infants: unmasked randomized con-trolledtrial.PediatrInt.2008;50:85---91.
3.DavisPG,MorleyCJ,OwenLS.Non-invasiverespiratorysupport ofpretermneonateswithrespiratorydistress:continuous pos-itiveairwaypressureandnasalintermittentpositivepressure ventilation.SeminFetalNeonatalMed.2009;14:14---20. 4.NascimentoRM,FerreiraAL,CoutinhoAC,etal.Thefrequency
ofnasalinjuryinnewbornsduetotheuseofcontinuous pos-itiveairway pressure withprongs. Rev Lat AmEnfermagem. 2009;17:489---94.
5.GünlemezA,IskenT,GökalpAS,etal.Effectofsilicongel sheet-inginnasalinjuryassociatedwithnasalCPAPinpreterminfants. IndianPediatr.2010;47:265---7.
6.Alves AM,Santos ER, SouzaTG. Prevenc¸ão de lesões nasais secundáriasaousodepressãopositivacontínuanasviasaéreas (CPAP)emrecém-nascidosprematurosdeextremobaixopeso. RevUnivValeRioVerde.2013;11:209---17.
7.Pádua G, Martinez EZ, Brunherotti MA. Efeitos cardiorrespi-ratóriosfrenteàposic¸ãodocorpoemrecém-nascidospré-termo submetidosaoaumentodovolumegástrico.ArqGastroenterol. 2009;46:321---7.
parameters and thermoregulation in premature infants. Neonatology.2010;97:311---7.
9.AmmariA,SchulzeKF,Ohira-kistK,etal.Effectsofbody posi-tiononthermal,cardiorespiratoryandmetabolicactivityinlow birthweightinfants.EarlyHumDev.2009;85:497---501. 10.PocockSJ.Clinicaltrials:apracticalapproach.Chichester:John
Wiley;1983.
11.RegoMA,MartinezFE.Clinicaland laboratorialrepercussions ofnasal CPAP in pretermnewborns. JPed (Rio J). 2000;76: 339---48.
12.AbdeyazdanZ,NematollahiM,MohhamadizadehM.Theeffects of supine and prone positions on oxygenation in premature
infants undergoing mechanical ventilation. Iran J Nurs Mid-wiferyRes.2010;15:229---33.
13.MalagoliRC,SantosFF,OliveiraEA,etal. Influenceofprone positiononoxigenation,respiratoryrateand musclestrength inpreterminfantsbeingweanedfrommechanicalventilation. RevPaulPediatr.2012;30:251---6.
14.BhatRY,LeipäläJA,SinghNRP,etal.Effectofpostureon oxy-genation,lungvolume,andrespiratorymechanicsinpremature infantsstudiedbeforedischarge.Pediatrics.2003;112:29---32. 15.BrunherottiMA,MartinezEZ,MartinezFE.Effectofbody