RESUMEN
Estudio descripivo, transversal y retros -pecivo de abordaje cuanitaivo, cuyo objeivo fue relacionar el Índice de Masa Corporal (IMC) a los eventos ocurridos en el postoperatorio de la cirugía de revas -cularización miocárdica. La recolección de datos se realizó entre abril y junio del 2012. Los paricipantes fueron divididos según su IMC en tres grupos: aquellos con estado nutricional normal, con sobrepeso y obesos. El análisis de datos se basó en la estadísica descripiva. Se encontró que los paricipantes eutróicos tuvieron más complicaciones, especialmente pulmona -res. Ente los individuos con sobrepeso y obesidad destacaron las complicaciones cardiovasculares, teniendo los sujetos con obesidad peor pronósico. Se concluyó que no existe asociación estadísicamente sig -niicaiva entre la obesidad y el sobrepeso con la mayor frecuencia de complicaciones postoperatorias a pesar de la ocurrencia de complicaciones cardiovasculares en esos grupos. El conocimiento de esas posibles complicaciones posibilita la planiicación adecuada de los cuidados de enfermería a parir de la prácica basada en la evidencia.
DESCRIPTORES Obesidad
Índice de masa de corporal Revascularización miocárdica Complicaciones postoperatorias Enfermería perioperatoria RESUMO
Estudo descriivo, transversal e retrospec -ivo, com abordagem quanitaiva, cujo ob -jeivo foi relacionar o índice de massa cor -poral (IMC) a eventos do pós-operatório da cirurgia de revascularização miocárdica. A coleta de dados ocorreu entre abril e junho de 2012. Os paricipantes foram divididos de acordo com o índice de massa corporal em três grupos: não obesos, com sobrepe -so e obe-sos. A análise de dados baseou-se na estaísica descriiva. Veriicou-se que os paricipantes não obesos iveram mais complicações, notadamente as pulmona -res. Dentre os indivíduos com sobrepeso e obesidade sobressaíram-se as complica -ções cardiovasculares. Os obesos iveram pior prognósico. Concluiu-se que a obesi -dade e o sobrepeso não iveram associação estaisicamente signiicaiva com maior frequência de complicações pós-operató -rias, apesar da ocorrência de complicações cardiovasculares nesses grupos. O conheci -mento dessas possíveis complicações pos -sibilita o planejamento adequado da assis -tência de enfermagem, a parir da práica baseada em evidências.
DESCRITORES Obesidade
Índice de massa corporal Revascularização miocárdica Complicações pós-operatórias Enfermagem perioperatória ABSTRACT
This is a descripive, retrospecive study with cross-secional quanitaive approach, which aimed to relate the body mass index with events in the postoperaive period of the myocardial revascularizaion surgery with use of extracorporeal circulaion. The data collecion period was between April and June/2012. Paients were divided ac -cording to the body mass index and clas -siied as without excess of weight, over -weight or obese. The data analysis was based on the descripive staisics. The pa -ients without excess of weight had more complicaions, especially those related to the lungs. Among overweight and obese individuals, the cardiovascular complica -ions stood out. The obese subjects had the worse prognosic. Obesity and over -weight did not have staisically signiicant associaion with a higher frequency of postoperaive complicaions, in spite of the occurrence of cardiovascular complicaions in this group. The paients without excess of weight had higher risks of developing neurological events.
DESCRIPTORS Obesity
Body mass index
Myocardial revascularizaion Postoperaive complicaions Perioperaive nursing
Overweight and obesity repercussion
in the postoperative of myocardial
revascularization surgery
O
riginal
a
rticle
Nyagra Ribeiro de Araujo1, Raul Amaral de Araújo2, Simone Maria Muniz da Silva Bezerra3
REPERCUSSÃO DO SOBREPESO E DA OBESIDADE NO PÓS-OPERATÓRIO DA CIRURGIA DE REVASCULARIZAÇÃO MIOCÁRDICA
REPERCUSIÓN DEL SOBREPESO Y DE LA OBESIDAD EN EL POSTOPERATORIO DE LA CIRUGÍA DE REVASCULARIZACIÓN MIOCÁRDICA
1 Master student of the Post-graduation Associate Program in Nursing, Universidade de Pernambuco, Universidade Estadual da Paraíba, Recife, PE, Brazil.
INTRODUCTION
In the last few decades people are consuming more high energy density foods with high levels of sugar and saturated fats. These nutriional habits combined with increased physical inacivity are expanding very rapidly in developing countries(1).
In Brazil, the analysis of secular trends indicates that obesity among adults is expanding, reaching at least 10% of the populaion in all regions of the country between 2008 and 2009(2). Projecions based on naional surveys conducted in recent decades esimate that in 2015 obe-sity will reach 40% of the U.S. populaion, 30% of the Eng-lish and 20% of the Brazilian(3).
Obesity generates a signiicant state of personal and collecive sufering, given the impact of its numerous co-morbidiies, including metabolic disorders such as meta-bolic syndrome and diabetes, gallbladder diseases, hy-pertension, orthopedic problems, cardiovascular disease (CVD), cancer and sleep apnea(4).
The nutritional status affects how individuals tol-erate the fact of undergoing heart surgery. The clini-cal condition of patients, length of hospital stay and treatment response are directly influenced by obesity, which is associated with elevated morbidity, mortality and hospital costs(5-6).
Coronary heart diseases (CHD) paricularly stand out because of their associaion with overweight and obe-sity in afected individuals. In many paients, the impair-ment becomes so extensive that drug or percutaneous therapies are insuicient to maintain a good quality of life. Therefore, more invasive procedures such as coronary ar-tery bypass grating (CABG) are required(7).
In the literature are observed contradicions regard-ing the inluence of body mass index (BMI) in the CABG postoperaive phase. In some studies, a high BMI - indicat-ing overweight or obesity - was not associated with post-operaive complicaions, while other studies have shown a posiive associaion between overweight, obesity and CABG postoperaive complicaions(8-11).
There is a lack of knowledge about the inluence of overweight and obesity in postoperaive adversiies in cardiac surgery, which requires studies addressing this is-sue. Thus, the development of this study is jusiied, aim-ing at relaaim-ing the body mass index with events of the CABG postoperaive period.
METHOD
This is a descripive and retrospecive study with cross-secional quanitaive approach(11) carried out by analy-sis of medical records of paients undergoing CABG in a 12 month period (March/2011 to February/2012) at the
Professor Luiz Tavares Cardiology Emergency Hospital of Pernambuco located in the Universidade de Pernambuco (PROCAPE/UPE). This is a reference insituion in cardiol-ogy for the North and Northeast regions of Brazil.
The study included paients of both sexes who under-went CABG with median sternotomy and cardiopulmo-nary bypass (CPB). Were excluded those with valvular dis-ease who underwent valvuloplasty or valve replacement, those who underwent CABG without CPB, those who had previously undergone CABG and individuals whose medi-cal records had missing or insuicient informaion. The applicaion of inclusion and exclusion criteria resulted in a sample of 124 individuals.
The data collecion period was between April and June 2012. Informaion from admission unil discharge was extracted from medical records of individuals, compris-ing the followcompris-ing independent variables: data from case histories and physical examinaions, comorbidiies and life habits present in the preoperaive phase, clinical presen-taion of coronary artery disease (CAD) on admission, data of the intraoperaive phase, postoperaive complicaions and length of stay.
The outcome variable was the BMI, according to the World Health Organizaion (WHO)(12) cutofs, namely: no excess of weight for BMI < 25 kg/m2, overweight for BMI ≥ 30 kg/m2 and obesity for BMI ≥ 30 kg/m2. Hence, three BMI groups were analyzed in this study.
The variables were tabulated and analyzed using de-scripive staisics with the STATA/SE 9.0 sotware. The Kolmogorov-Smirnov test was used to determine the use of parametric and nonparametric tests. The chi-squared test and the Fisher’s exact test were used for categori-cal variables(13). The groups were compared by analysis of variance (ANOVA), when the Kolmogorov-Smirnov test showed normal distribuion. In opposite cases, the Krus-kal-Wallis test was applied. All tests were applied with a 95% conidence interval and only values of p <0.05 were expressed in the tables(13).
The study was approved by the Ethics Commitee in Research of the Complexo Hospitalar Hospital Universi-tário Oswaldo Cruz/Pronto-Socorro Cardiológico de Per-nambuco (HUOC/PROCAPE) and by the CAAE number 0169.0.106.000-11.
RESULTS
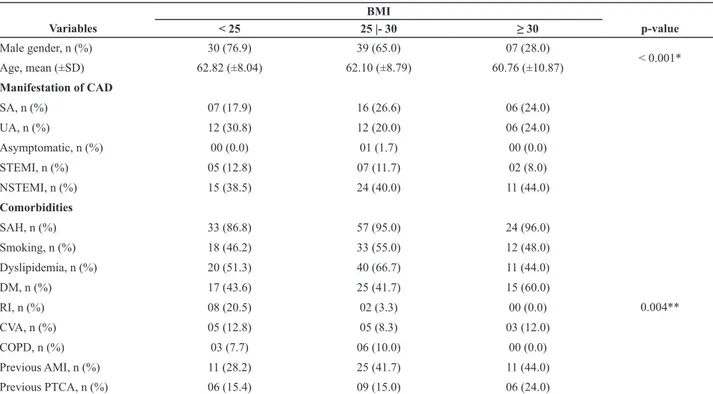
Regarding the manifestaion of CHD at hospital admis-sion, in all three groups it was observed an increased preva-lence of non-ST-elevaion myocardial infarcion (NSTEMI). However, all forms of manifestaion had similar distribuion frequencies. The systemic arterial hypertension (SAH) and diabetes mellitus (DM) were more prevalent among the obese. Smoking, dyslipidemia, alcoholism and chronic
ob-strucive pulmonary disease (COPD) were more frequent among overweight paients. The incidence of renal insuf-iciency (RI) stood out in subjects without excess of weight. The history of smoking was common in all three categories. A higher frequency of previous acute myocardial infarcion (AMI) and percutaneous transluminal coronary angioplasty (PTCA) was observed among obese individuals.
Table 1 - Characteristics of patients who underwent CABG between March/2011 and February/2012 – Recife, PE
BMI
Variables < 25 25 |- 30 ≥ 30 p-value
Male gender, n (%) 30 (76.9) 39 (65.0) 07 (28.0)
< 0.001*
Age, mean (±SD) 62.82 (±8.04) 62.10 (±8.79) 60.76 (±10.87)
Manifestation of CAD
SA, n (%) 07 (17.9) 16 (26.6) 06 (24.0)
UA, n (%) 12 (30.8) 12 (20.0) 06 (24.0)
Asymptomatic, n (%) 00 (0.0) 01 (1.7) 00 (0.0)
STEMI, n (%) 05 (12.8) 07 (11.7) 02 (8.0)
NSTEMI, n (%) 15 (38.5) 24 (40.0) 11 (44.0)
Comorbidities
SAH, n (%) 33 (86.8) 57 (95.0) 24 (96.0)
0.004**
Smoking, n (%) 18 (46.2) 33 (55.0) 12 (48.0)
Dyslipidemia, n (%) 20 (51.3) 40 (66.7) 11 (44.0)
DM, n (%) 17 (43.6) 25 (41.7) 15 (60.0)
RI, n (%) 08 (20.5) 02 (3.3) 00 (0.0)
CVA, n (%) 05 (12.8) 05 (8.3) 03 (12.0)
COPD, n (%) 03 (7.7) 06 (10.0) 00 (0.0)
Previous AMI, n (%) 11 (28.2) 25 (41.7) 11 (44.0)
Previous PTCA, n (%) 06 (15.4) 09 (15.0) 06 (24.0)
SD – Standard deviation; CAD – coronary artery disease; SA – stable angina; UA – unstable angina; STEMI – ST-elevation myocardial infarction; NSTEMI
– non-ST-elevation myocardial infarction; SAH – systemic arterial hypertension; DM – diabetes mellitus; RI – renal insuficiency; CVA – cerebrovascular
accident; COPD – chronic obstructive pulmonary disease; AMI – acute myocardial infarction; PTCA – percutaneous transluminal coronary angioplasty. *Chi-squared test. **Fisher’s exact test.
Table 2 - Perioperative variables of patients who underwent CABG between March/2011 and February/2012 - Recife-PE*
BMI
Variables < 25 25 |- 30 ≥ 30
Mean (±SD) Mean (±SD) Mean (±SD)
Age 62.82 (±8.04) 62.10 (±8.79) 60.76 (±10.87)
Number of grafts 2.49 (±0.79) 2.67 (±0.80) 2.72 (±0.74)
Surgery time 255.26 (±78.99) 273.41 (±65.09) 262.69 (±58.55)
CPB time 87.89 (±31.55) 97.89 (±32.97) 94.29 (±38.42)
Time of pre-surgical hospitalization 16.90 (±11.17) 15.83 (±12.08) 13.76 (±8.94)
Time of post-surgical hospitalization 16.15 (±16.39) 13.13 (±11.51) 10.72 (±6.25)
Total hospitalization time 33.05 (±21.80) 29.00 (±17.52) 24.48 (±9.17)
The mean duraion of surgery and of the cardiopulmo-nary bypass (CPB) was higher among overweight individu-als: 273.41 (± 65.09) minutes and 97.89 (± 32.97) minutes, respecively. Among the obese, the average ime of sur-gery was 262.69 (± 58.55) minutes and the mean CPB ime was 94.29 (± 38.42) minutes. Obese paients were those who required higher number of grats, with an average of 2.72 (± 0.74), as shown in Table 2.
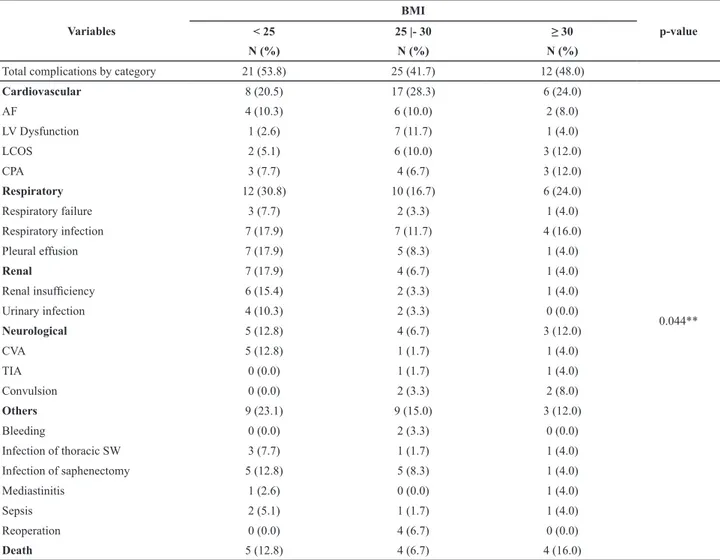
The relaive frequency of postoperaive complicaions among individuals without excess of weight was 53.8%, in obese it was 48% and 41.7% in overweight individuals. The most common complicaions among those without
Table 3 - Major postoperative complications in patients who underwent CABG between March/2011 and February/2012 – Recife, PE
BMI
Variables < 25 25 |- 30 ≥ 30 p-value
N (%) N (%) N (%)
Total complications by category 21 (53.8) 25 (41.7) 12 (48.0)
Cardiovascular 8 (20.5) 17 (28.3) 6 (24.0)
0.044**
AF 4 (10.3) 6 (10.0) 2 (8.0)
LV Dysfunction 1 (2.6) 7 (11.7) 1 (4.0)
LCOS 2 (5.1) 6 (10.0) 3 (12.0)
CPA 3 (7.7) 4 (6.7) 3 (12.0)
Respiratory 12 (30.8) 10 (16.7) 6 (24.0)
Respiratory failure 3 (7.7) 2 (3.3) 1 (4.0)
Respiratory infection 7 (17.9) 7 (11.7) 4 (16.0)
Pleural effusion 7 (17.9) 5 (8.3) 1 (4.0)
Renal 7 (17.9) 4 (6.7) 1 (4.0)
Renal insuficiency 6 (15.4) 2 (3.3) 1 (4.0)
Urinary infection 4 (10.3) 2 (3.3) 0 (0.0)
Neurological 5 (12.8) 4 (6.7) 3 (12.0)
CVA 5 (12.8) 1 (1.7) 1 (4.0)
TIA 0 (0.0) 1 (1.7) 1 (4.0)
Convulsion 0 (0.0) 2 (3.3) 2 (8.0)
Others 9 (23.1) 9 (15.0) 3 (12.0)
Bleeding 0 (0.0) 2 (3.3) 0 (0.0)
Infection of thoracic SW 3 (7.7) 1 (1.7) 1 (4.0)
Infection of saphenectomy 5 (12.8) 5 (8.3) 1 (4.0)
Mediastinitis 1 (2.6) 0 (0.0) 1 (4.0)
Sepsis 2 (5.1) 1 (1.7) 1 (4.0)
Reoperation 0 (0.0) 4 (6.7) 0 (0.0)
Death 5 (12.8) 4 (6.7) 4 (16.0)
AF – atrial ibrilation; LV – left ventricle; LCOS – low cardiac output syndrome; CPA – cardiopulmonary arrest; CVA – cerebrovascular accident; TIA – transient
ischemic attack; SW – surgical wound. **Fisher’s exact test.
excess of weight were pulmonary, whereas in overweight paients cardiovascular predominated, and in obese, cardiovascular and lung complicaions predominated in equal numbers (Table 3).
In paricipants without excess of weight, the most com-mon complicaions were respiratory infecion (17.9%), pleural efusion (17.9%), renal failure (15.4%), stroke (12.8%), infecion of saphenectomy (12.8%) and death (12.8%). In overweight individuals the following occurred: let ventricular dysfuncion (11.7%), respiratory infecion (11.7%), atrial ibrillaion (10%) and low cardiac output syn-drome (10%). In obese individuals were observed respira-tory infecion (16%), LCOS (10%), cardiopulmonary arrest (10%) and death (16%).
DISCUSSION
It was signiicantly found (p<0,001) that even though
women underwent CABG less, they were obese when doing it, predicing a worse prognosis(14-15). However, in
another study(16), the number of men was more prevalent, even in the group of obese paients.
The prevalent form of manifestaion of CAD in hos-pital admission, regardless of BMI, was the NSTEMI, a more serious medical condiion than that found in a study comparing subjects with BMI < 30 and > 30 kg/m2, and inding a higher prevalence of UA in paients admit-ted to hospital(17).
A higher occurrence of CVA was identified in pa-tients with BMI < 25 kg/m2 in the postoperative CABG period. However, a similar study found a higher prev-alence of CVA in obese people(9), while another study showed that the prevalence of CVA in the CABG postop-erative period was similar among obese and non-obese subjects(10). In the preoperative period, the category of BMI < 25 kg/m2 was also associated with greater posi-tive history for CVA.
In the postoperaive period of cardiac surgery, neuro-logic complicaions are mulifactorial, including pre, intra and postoperaive risk factors such as age, gender, previ-ous neurological disease, caroid artery disease, micro-embolisms, perfusion disorders, metabolic disorders and inlammatory responses(10).
In this study, the CPB ime was lower among paients without excess of weight and higher in overweight pa-ients. In general, it is known that the ime of surgery is di-rectly related to CPB ime(19). In some studies(17,20) in which there was staisically signiicant diference, the CPB ime was lower in paients without excess of weight and over-weight and higher in obese paients.
Individuals without excess of weight had higher to-tal hospito-talizaion ime, but in another study, the obese had longer hospital stays(16). The overweight and obese individuals were probably treated more aggressively with more precocious surgical procedure, while paients with a BMI <25 kg/m2 had longer postoperaive hospital stay and presented major complicaions.
The higher prevalence of cardiovascular complicaions in the categories of overweight and obesity was because obesity is an indirect cause of heart diseases, and related to hemodynamic changes (high blood pressure, elevated heart rate), metabolic (dyslipidemia) and ventricular hy-pertrophy, with consequent progressive atrial dilataion. All this can contribute to the occurrence of AF and LCOS(21).
A study that classiied its sample in non-obese and obese found that obese individuals had higher number of deaths, mediasiniis, CVA, respiratory failure and infec-ion, sepsis and AF and the non-obese had more myocar-dial infarcion and CPA (16). In another study, obese paients had more respiratory failure, surgical wound infecion (chest and saphenous), sepsis, heart atack and kidney insuiciency. The non-obese had more AF, CPA, bleeding and reoperaion(17).
In the present study, the higher morbidity and mortal-ity among obese paients may be related to the fact that this group was composed predominantly of females. The literature reveals higher rates of morbidity and mortality in women than in men undergoing CABG(22).
The results of this study also showed that the group with BMI <25 kg/m2 was comprised of seniors with the highest average age among the BMI categories and a greater number of postoperative complications.
Although the findings do not have statistical signifi-cance, malnutrition in the elderly is known to be re-lated to adverse surgical outcomes as it affects the immune competence and the ability to manage stress. This was evidenced by a study in which the nutritional impairment was related to longer hospital stays and re-habilitation, increased risk of infection and poor heal-ing of surgical wounds(23).
Another study(9) showed that a BMI < 22 kg/m2 may increase the incidence of postoperaive complicaions in elderly paients undergoing CABG and that obesity (con-sidered with a BMI> 27 kg / m²), in contrast, may have a protecive efect, except for cases of renal dysfuncion. The term ‘obesity paradox’ has been used to express this protecive relaion that increasing weight seems to exert on the various cardiovascular events. In myocardial re-vascularizaion, either percutaneous or surgical, the ex-tremes of a nutriional status, ie, low weight and severe obesity, have been linked to unfavorable outcomes when compared to overweight or obese paients(24-25).
CONCLUSION
Although it has not been observed a staisically sig-niicant associaion between overweight and obesity and a higher frequency of complicaions ater CABG in this study, we found that obese paients were younger and predominantly female, had more grats in the CABG pro-cedure and showed higher mortality. Overweight individ-uals had longer ime of surgery, CPB and a higher preva-lence of cardiovascular complicaions.
Regarding those individuals with BMI <25 kg/m2, it was found that they had worse renal funcion, higher mean age, greater frequency of complicaions and pro-longed hospital stay. Furthermore, these paients had a higher risk of developing neurological events.
The limitaions of this study are mainly due to its de-scripive and retrospecive aspects, which limit the pro-vision of models for predicion. Nevertheless, the results help to indicate which comorbidiies deserve atenion in future research and in the evaluaion of surgical risks re-lated to BMI.
This study is paricularly relevant for the nursing ield because the knowledge of possible complicaions that oc-cur in a paricular subgroup of paients in the postopera-ive period of cardiac surgery allows the appropriate care planning, from evidence-based pracices.
REFERENCES
1. Chaves VLV, Freese E, Lapa TM, Cesse EAP, Vasconcelos ALR. Evolução espaço-temporal do sobrepeso e da obesidade em adolescentes masculinos Brasileiros, 1980 a 2005. Cad Saúde Pública. 2010;26(7):1303-13.
2. Insituto Brasileiro de Geograia e Estaísica (IBGE). Pesquisa de Orçamentos Familiares 2008-2009. Antropometria e estado
nutricional de crianças, adolescentes e adultos no Brasil. [Inter
-net]. Rio de Janeiro; 2010 [citado 2012 set. 29]. Disponível em:
htp://www.ibge.com.br/home/estaisica/populacao/condi
-caodevida/pof/2008_2009_encaa/default.shtm
3. Hu F. Measurements of adiposity and body composiion. In:
Hu F, editor. Obesity epidemiology. New York: Oxford Univer
-sity Press; 2008. p. 53-83.
4. Rossei MB, Brito RR, Norton RC. Prevenção primária de doenças cardiovasculares na obesidade infantojuvenil: efeito ani-inlamatório do exercício ísico. Rev Bras Med Esporte. 2009;15(6):472-5.
5. Crestani1 N, Bieger P, Kik RME, Dias RL, Alscher S, Lienert RSC. Peril nutricional de pacientes adultos e idosos admiidos em um hospital universitário. Ciênc Saúde. 2011;4(2):45-9. 6. Magalhães MGPA, Alves LMO, Alcântara LFM, Bezerra SMMS.
Post-operaive mediasiniis in a heart hospital of Recife:
contribuions for nursing care. Rev Esc Enferm USP [Inter
-net]. 2012 [cited 2013 Aug 10];46(4):865-71. Available from: htp://www.scielo.br/pdf/reeusp/v46n4/en_12.pdf.
7. Gomes F, Telo DF, Souza HP, Nicolau JC, Halpern A, Serrano Junior CV. Obesidade e doença arterial coronariana: papel da inlamação vascular. Arq Bras Cardiol. 2010;94(2):273-9. 8. King-Shier KM, Leblanc P, Mather C, Sandham S, Seneviratne
C, Maitland A. Weight and Paients’ decision to undergo car
-diac surgery. Clin Nurs Res. 2013;22(2):228-49.
9. Reis C, Barbiero SM, Ribas L. O efeito do índice de massa cor
-poral sobre as complicações no pós-operatório de cirurgia de
revascularização do miocárdio em idosos. Rev Bras Cir Cardio
-vasc. 2008;23(4):524-9.
10. Nina VJS, Rocha MIA, Rodrigues RF, Oliveira VC, Teixeira JLL, Figueredo ED, et al. Avaliação do escore CABDEAL como preditor de disfunção neurológica no pós-operatório de revascularização miocárdica com circulação extracorpórea. Rev Bras Cir Cardiovasc. 2012;27(3):429-35.
11. Polit DF, Beck CT. Fundamentos de pesquisa em enferma
-gem: avaliação de evidências para a práica da enfermagem. 7a ed. Porto Alegre: Artmed; 2011.
12. World Health Organizaion (WHO). Child Growth Standards.
Physical status: the use and interpretaion of anthropom
-etry. Report of a WHO Expert Commitee. Geneva; 2013.
13. Agresi A, Finlay B. Métodos estaísicos para as ciências so
-ciais. 4a ed. Porto Alegre: Penso; 2012.
14. Godoy PH, Oliveira GMM, Silva NAS, Klein CH. Diferença nas taxas de letalidade e nas principais causas de óbito, entre
homens e mulheres, por revascularização miocárdica cirúr
-gica. Rev SOCERJ. 2008;21(3):148-53.
15. Santos FCP, Gazzi LAP, Libardi MC, Santos DFP, Silva DVB, Fichinno MZS, et al. Epidemiologia e manejo dos fatores de risco na síndrome coronariana aguda na mulher. Rev Fac Ciênc Méd Sorocaba. 2009;11(2):6-11.
16. Guaragna LP, Dall’Alba DP, Goulart PR, Guaragna JCVC, Bo
-danese LC, Magedanz EH, et al. O impacto da obesidade na morbi-mortalidade de pacientes submeidos à cirurgia de revascularização miocárdica. Sci Med. 2008;18(2):75-80. 17. Alan M, Siddiqui S, Lee V, Elayda MA, Nambi V, Yang EY, et al.
Isolated coronary artery bypass grating in obese individu
-als. Circ J. 2011;75(6):1378-85.
18. Oliveira CMC, Kubrusly M, Mota RS, Silva CAB, Oliveira
VN. Desnutrição na insuiciência renal crônica: qual o mel
-hor método diagnósico na práica clínica? J Bras Nefrol. 2010;32(1):57-70.
19. Kaya K, Cavolli R, Telli A, Soyal MF, Aslan A, Gokaslan G, et al. Of-pump versus on-pump coronary artery bypass grating
in acute coronary syndrome: a clinical analysis. J Cardiotho
-rac Surg [Internet]. 2010 [cited 2012 Sept 29];5(31):[about
8p]. Available from: htp://www.ncbi.nlm.nih.gov/pmc/ar
-icles/PMC2873363/pdf/1749-8090-5-31.pdf
20. Le-Berta G, Santana O, Pineda AM, Zamora C, Lamasa GA, Lamelas J. The obesity paradox in elderly obese paients
undergoing coronary artery bypass surgery. Interact Cardio
-vasc Thorac Surg. 2011;13(2):124-7.
21. Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS, et al. Atrial ibrillaion and obesity: results of a meta-analysis. Am Heart J. 2008;155(2):310-5.
22. Oliveira EL, Westphal GA, Mastroeni MF. Caracterísicas clínico-demográicas de pacientes submeidos à cirurgia de
revascularização do miocárdio e sua relação com a mortali
-dade. Rev Bras Cir Cardiovasc. 2012;27(1):52-60.
23. Vendites S, Almada-Filho CM, Minossi JG. Aspectos gerais da avaliação pré-operatória do paciente idoso cirúrgico. ABCD Arq Bras Cir Dig. 2010;23(3):173-82.
24. Ho K, Bertenshaw C, Same S, Schneider M, Williams K, Godsell T, et al. Diferenial associaions between body
mass index and outcomes ater elecive adult cardiac sur
-gery: a linked data cohort study. Anaesth Intensive Care. 2013;41(5):573-83.
25. De Schuter A, Lavie CJ, Patel DA, Milani RV. Obesity para