EFFECT OF ACUPUNCTURE ON HEART RATE
VARIABILITY AND OTHER NON-INVASIVE
HEMODYNAMIC PARAMETERS IN PATIENTS WITH
HEART FAILURE
A CLINICAL RESEARCH PROTOCOL
Nuno Cândido Maia Correia
Dissertação de Mestrado em Medicina Tradicional Chinesa
I
Nuno Cândido Maia Correia
EFFECT OF ACUPUNCTURE ON HEART RATE VARIABILITY AND
OTHER NON-INVASIVE HEMODYNAMIC PARAMETERS IN HEART
FAILURE
A CLINICAL RESEARCH PROTOCOL
Dissertação de Candidatura ao grau de Mestre
em Medicina Tradicional Chinesa submetida ao
Instituto de Ciências Biomédicas de Abel
Salazar da Universidade do Porto.
Orientador
– Prof. Doutor Henry Johannes Greten
Categoria – Professor Associado
Afiliação
– Instituto de Ciências Biomédicas
Abel Salazar da Universidade do Porto.
Co-orientador
– Prof. Doutor Paulo Bettencourt
Categoria – Professor Associado
Afiliação
– Faculdade de Medicina da
Universidade do Porto.
III
DEDICATION
To my beautiful Wife Vânia for all her love and support.
V
Scientific Chinese medicine, since its inception approximately 2100 years ago, is based upon the consistent application solely of inductive synthesis. (..) all its statements refer to the direct perception of dynamic and present effects. Prof. Manfred B. Porkert [1]
Acupunctural neuroreflexotherapy is useful and is clearly therapeutic, it works out of necessity through the channels of positive biology, without the interference of energetic conceptions that are foreign to experimental deductive thought. Francisco Abad-Alegría and Carlos Pomarón [2]
Traditional Chinese Medicine is a system of sensations and findings designed to establish a functional vegetative state. Prof. Henry Johannes Greten [3]
VII
ACNKOWLEDGMENTS
I would like to thank my closest family for all their background support that has enabled me to develop my own education.
To Maria das Dores Pombinho, a personal reference to me in life and Medicine, and the “yin-yang” we have shared.
To my dear Professors Jorge Machado, Manuel Laranjeira, and Johannes Greten, for their friendship, collegiality, and contagious braveness in the gracious quest of helping patients.
To Professor Andrew Remmpis for his accurate guidance and scientific expertise. To Professor Gerhard Litscher for sharing his experience and knowledge.
To Petra for her support in general management.
To my Biology teacher and dear friend Carlos Alberto, for his wisdom, excellence and friendship.
To Professor Paulo Bettencourt for his open mind and scientific culture that enables an internal medicine junior doctor to explore other “non-conventional” fields of health science and knowledge, while training in this magnificent and holistic medical specialty.
To my research colleague and friend Eduardo Capitão, an outstanding Nurse professional.
To some Humanity references whose historical legacy stands has an inspiration to me: the unrepeatable Leonardo da Vinci; Siddharta Gautama; Abel Salazar, William Osler, Mother Theresa of Calcutta; Albert Einstein; Nuno Grande, and Maria de Sousa.
To my few Friends for all their trust and tolerance.
Finally, to Medicine the mission I have struggled for as a way of helping my fellow human beings and making some useful sense out of this ridiculous life-time.
IX
RESUMO
Introdução: a insuficiência cardíaca (IC) é um problema de saúde à escala mundial com
um prognóstico sombrio. Resulta principalmente de mecanismos complexos de activação neuro-humoral que conduzem a uma desregulação autonómica. Investigação animal parece suportar o conceito de que a acupunctura poderá desencadear reflexos vegetativos que produzem substâncias endógenas inibitórias do efluxo simpático. Até ao presente, a escassa investigação em pacientes com IC sugere que a acupunctura poderá prolongar a distância de marcha bem como promover a variabilidade de frequência cardíaca (VFC).
Objectivo: estudar o efeito da acupunctura em pacientes com IC através da avaliação da
VFC e de outros parâmetros hemodinâmicos não invasivos (PHNIs).
Métodos: apresenta-se um protocolo clínico de um estudo clínico preliminar, prospectivo,
aleatorizado, controlado, duplamente cego, e com um desenho do tipo cruzado. Uma amostra de 20 doentes, do sexo masculino (idades entre 40 e 90 anos), com IC classe II (classificação da New York Heart Association) e fracção de ejecção do ventrículo esquerdo ≤40%, é seleccionada da consulta de IC de um hospital central. Cada paciente é submetido a uma avaliação basal da distância de marcha, aferida pelo teste de marcha gradual vaivém (TMGV), seguida de medição do grau de dispneia e fadiga através da escala de Borg. Durante a fase de intervenção os doentes são expostos, numa sequência aleatorizada, a uma sessão de electro-acupuntura “verdadeira” (EAv) e uma sessão de eletro-acupuntura “falsa” (EAf), separadas por uma semana de washout. A EAv consiste na estimulação bilateral de acupontos segundo o modelo de Heidelberg da Medicina Tradicional Chinesa; a EAf é definida como EA bilateral em acupontos considerados inactivos. Em ambas as intervenções, os parâmetros da VFC e PHNI são avaliados enquanto a EA de baixa frequência (2Hz), seguida de um teste tilt, é aplicada durante 15 minutos. O TMGV e a escala de Borg são reavaliados após cada intervenção de EA,. Outcomes principais: VFC, ratio baixa frequência/alta frequência (BF/AF; índice de equilíbrio simpático) e alta frequência (AF; índice de modulação vagal), e vários PHNIs. Parâmetros secundários: a distância de marcha e grau de dispneia e fadiga. Os dados serão analisados utilizando o software PASW® e um p <0,05 será aceite como estatisticamente significativo. O protocolo de investigação clínica foi aprovado pela Comissão de Ética de uma instituição hospitalar.
X
Resultados: a revisão da literatura indica que a acupunctura exerce efeitos
simpaticolíticos, pro-vagotónicos, e anti-inflamatórios. Foi descoberta uma via neurológica específica que participa na inibição, provocada pela EA, de reflexos cardiovasculares excitatórios ao nível centro cárdio-regulador no núcleo ventro-lateral rostral bulbar. Igual número de acupontos, verdadeiros e falsos, será submetido a estimulação com a mesma frequência de EA. Espera-se que o estudo possa revelar um aumento significativo da VFC, do ratio BF/AF e do poder de AF associado à intervenção com EAv versus EAf. Uma correlação entre os outcomes principais e secundários poderá ser encontrada com diferenças significativas entre EAv versus EAf.
Discussão: os resultados deste estudo preliminar poderão sugerir efeitos específicos dos
acupontos na fisiopatologia da IC associados a um possível benefício terapêutico. Os dados obtidos podem vir a suportar um ensaio clínico de maior escala e com parâmetros adicionais. No futuro, se a sua eficácia clínica for comprovada, a acupunctura poderá constituir uma estratégia adjuvante no tratamento convencional da IC.
Palavras-chave: Insuficiência cardíaca; variabilidade da frequência cardíaca; teste de
marcha; sistema nervoso autónomo; acupunctura; electro-acupunctura; medicina Chinesa tradicional.
XI
ABSTRACT
Introduction: Heart failure (HF) is a worldwide health problem with a dismal prognosis
mainly resulting from complex mechanisms of neurohumoral activation leading to system wide autonomic deregulation. Animal research data support the concept that acupuncture may elicit vegetative reflexes that release of endogenous substances which in turn inhibit sympathetic outflow. To the present date, only two preliminary clinical trials have recently suggested that acupuncture may prolong the 6-min walk distance and may increase heart rate variability (HRV) in HF patients.
Objective: To study the effect of acupuncture in HF patients as measured by HRV and
other non-invasive hemodynamic parameters (NIHP).
Methods: It is presented the clinical protocol of a preliminary, prospective, randomized,
controlled, double-blinded, clinical trial in a cross-over design. Twenty male patients (ages between 40 and 90 years old), with HF class II (New York Heart Association‟s classification) and left ventricular ejection fraction ≤ 40%, are sampled from the Outpatient HF Clinic of a central hospital. Each patient is submitted to a baseline assessment of walking distance, using the incremental shuttle walk test (ISWT), followed by evaluation of the degree of dyspnea and fatigue as measured by the Borg scale. During the intervention patients are exposed, in a randomly sequence, to one session of “verum-electroacupuncture” (vEA) and one session of “sham-“verum-electroacupuncture” (sEA), separated by a one-week washout period. Verum-EA consists of bilateral stimulation of acupoints following the Heidelberg Model of Traditional Chinese Medicine; sEA is defined as bilateral EA in acupoints considered inactive for this disease. In both interventions low-frequency EA (2Hz) is applied during 15 minutes, followed by a tilt test, while HRV and NIHP parameters are measured. ISWT and the Borg scores are reassessed after each EA intervention. Main parameters: HRV, low-frequency/high-frequency power ratio (LF/HF, an index of sympathovagal balance) and high-frequency power (HF, an index of vagal modulation), and several NIHP. Secondary parameters: walking distance and degree of dyspnea and fatigue. Data will be analyzed using PASW® software and a p<0.05 will be accepted as statistically significant. The research protocol was approved by the Ethics Committee of the respective hospital.
XII
Results: review of the recent literature indicates that acupuncture exerts sympatholytic,
pro-vagotonic, and anti-inflammatory effects. It was discovered a specific neurological pathway participating in EA inhibition of excitatory cardiovascular reflexes at the rostral ventrolateral medulla cardiovascular center. Since both verum and sham acupoints are stimulated by equal EA frequency, the study may reveal a significant increase in HRV, in LF/HF power ratio and HF power in the vEA intervention versus sEA intervention. A correlation between main and secondary outcomes may be observed with significant differences between both interventions.
Discussion. Results from the proposed preliminary trial may demonstrate specific effects
of acupoints in the pathophysiology of HF which may be associated with a therapeutic benefit. Collected data may support a full-scale clinical trial with additional parameters. In the future, if its clinical efficacy is proved, acupuncture may become an adjuvant strategy alongside the conventional treatment of HF.
Key-words: Heart failure; heart rate variability; walk test ; autonomic nervous system;
XIII
Contents
INTRODUCTION ... 21
CHAPTER ONE ... 25
Theoretical framework ... 25
1.1. Heart failure a worldwide burgeoning problem ... 27
1.2. Etiopathophysiology of heart failure – modern understanding and ground for studies in acupuncture ... 28
1.3. Conventional therapeutic approach to heart failure ... 39
1.4. Acupuncture an historical and scientific overview ... 45
1.6. Heart rate variability a tool for acupuncture studies in heart failure ... 81
1.7. Assessment of heart failure patients’ functional capacity in acupuncture trials ... 85
CHAPTER TWO ... 86
Clinical research protocol ... 86
CHAPTER THREE ... 100 Results ... 100 CHAPTER FOUR ... 102 Discussion ... 102 CHAPTER FIVE ... 108 Future perspectives ... 108 References ... 112
XV
INDEX OF FIGURES
Figure 1. Evolution of the pathogenesis of heart failure with depressed efection fraction. 33
Figure 2. The neurohormonal system in heart failure ...35
Figure 3. Stages in the evolution of HF and recommended therapy ...41
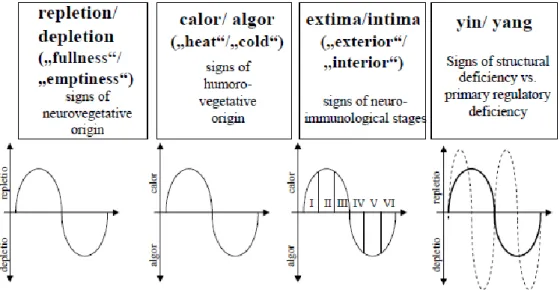
Figure 4. The Heidelberg Model of TCM ...52
Figure 5. Regulation as a technical process. ...52
Figure 6. The Fou Qi emblem: symbol for the regulatory meaning of yin, yang, and the phases. ...53
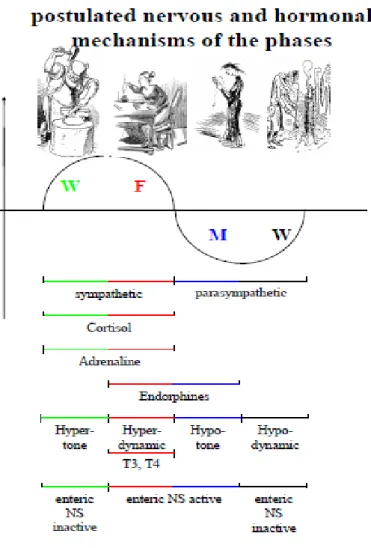
Figure 7. Phases of Chinese Medicine and physiological analogies ...54
Figure 8. Schematic representation of the TCM methodology of diagnosis. ...55
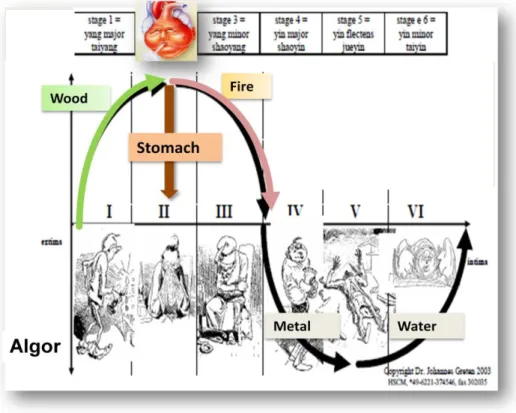
Figure 9. Chronic heart failure as a splendor yang syndrome in Algor Laedens theory. ...58
Figure 10. Acupuncture may be indicated in four areas of cardiovascular Disease. ...65
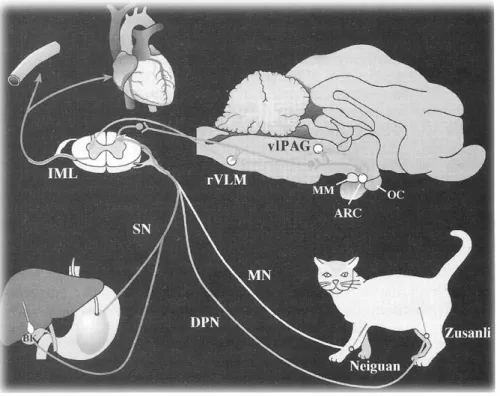
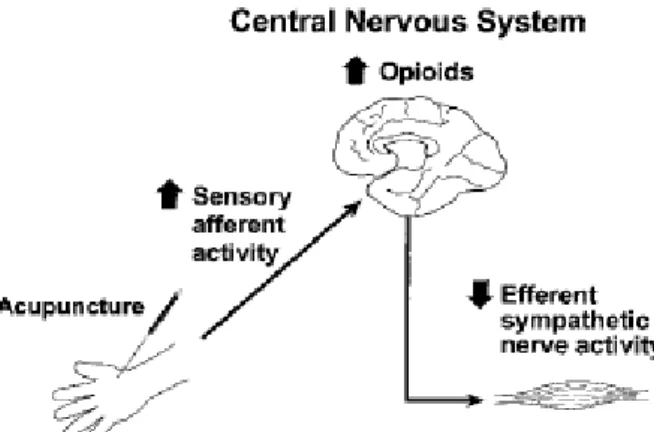
Figure 11. Proposed mechanism for acupuncture‟s modulation of sympathetic neural activity in heart failure ...65
Figure 12. Experimental evaluation of peripheral and central neural mechanisms of action of acupuncture on the cardiovascular system of anesthetized cats.. ...70
Figure 13. Neural pathway of EA effect on cardiovascular neurons in rVLM. ...71
Figure 14. Central modulation of heart rate variability. ...81
Figure 15. Study cross-over design.. ...90
XVI
INDEX OF TABLES
Table 1. Etiologies of Heart Failure ...30 Table 2. Frequency-dependent release of CNS opioid peptides by peripheral electrical
stimulation. ...67
Table 3. Summary of research on heart rate variability (HRV) and acupupuncture. LF, low
frequency band; HF, high frequency band. EA, electroacupuncture. ...84
Table 4. Eligibility criteria ...92 Table 5. Schedule of the project ...99
XVII
LIST OF ABBREVIATIONS
5-HT: 5-hydroxytriptamine 6-MWT: six-minute walk test
ACC/AHA: American College of Cardiology/American Heart Association
ACE inhibitors: Angiotensin-converting enzyme Ach: acetylcholine
AD: anno domini
ADH: antidiuretic hormone AF: alta-frequência
AICD: automatic implantable cardioverter-defibrillator
ANP: atrial natriuretic peptide ANS: autonomous nervous system ARB: angiotensin receptor blockers ATPase: adenosine triphosphatase AVP: arginine vasopressin
BaCl2: Barium chloride BB: -blocker
BC: before Christ BF: baixa-frequência
BNP: brain natriuretic peptide BP: blood pressure
CAD: Coronary artery disease
CAM: complementary and alternative medicine CCM: Cardiac contractility modulation
CR: Cardiac resynchronization therapy. DP: deep peroneal nerve
EA: electroacupuncture EAf: electro-acupunctura falsa EAv: electro-acupunctura verdadeira ECG: electrocardiogram
EF: Ejection fraction
eNOS: endothelial nitric oxide synthase EP: evolutionary/evolutive phase
fMRI: functional magnetic resonance imaging
GABA: gamma-aminobutyric acid GC: guiding-criteria
HF: (chronic) heart failure HF: High-frequency HRV: heart rate variability IML: intermedio lateral
ISWT: incremental shuttle walking test K: kidney meridian
LI: large intestine meridian
LF/HF: low-frequency/High-frequency ratio LF: low-frequency
LV: left ventricular
LVEF: left ventricular ejection fraction LU: lung meridian
MA: manual acupuncture MI: myocardial infarction
MIBG: iodine-131-meta-iodobenzylguanidine. MLWHFQ: Minnesota Living with HF Questionnaire
MMPs: metalloproteinases. MN: median nerve
MRE: magnetic resonance elastography MTPs: myofascial trigger points
MTrPs: myofascial trigger points
NIHP: non-invasive hemodynamic parameters NO: oxide
NRO: nucleus raphe obscurus NTS: nucleus tractus solitari NYHA: New York Heart Association OC: optic chiasm
PA: placebo acupuncture
PAG: periaqueductal gray substance
PENS: percutaneous electrical nerve stimulation
PC: pericardium meridian PG: prostaglandins
XVIII
LIST OF ABBREVIATIONS (cont.)
PHNI: parâmetros hemodinâmicos não invasivos
RAAS: renin-angiotensin-aldosterone system rVLM: rostral ventrolateral medulla
S: stomach meridian
SDNN: standard deviation of all normal to normal R-R intervals
sEA: sham-acupunture
SERCA2A: sarcoplasmic reticulum Ca2+ adenosine triphosphatase
SHRs: spontaneous hypertension rats SNS: sympathetic nervous system SPN: superficial peroneal nerve SPN: superficial radial nerve SR: sarcoplasmic reticulum
TCM: Traditional Chinese Medicine
TENS: transcutaneous electrical nerve stimulation
TMGV: teste de marcha gradual vaivém TNF: tumour necrosis factor alfa US: United States
VA: verum acupuncture' VAD: ventricular assist device vEA: verum-acupuncture
VFC: variabilidade da frequência cardíaca vlPAG: ventrolateral periaqueductal gray vPAG: ventral periaqueductal gray VS: vagal stimulation
21
23
Introduction
Chronic heart failure (HF) is a major health issue affecting millions of people and carrying important economic health costs. Despite optimized standard therapeutics, the prognosis remains dismal.
The majority of patients with HF are limited in daily life by dyspnea and fatigue and reduced exercise capacity. The current state-of-the art medical treatment includes mainly -blocker and angiotensin converting enzyme inhibitor in order to oppose the sympathetic nervous system over activation and its consequences. Additionally, novel approaches have been addressing the clinical benefit of selective electric vagal nerve stimulation to normalize autonomic balance.
Acupuncture has shown to induce anti-sympathotonic, pro-vagotonic, anti-inflammatory and immunomodulatory effects. Therefore, from a theoretical standpoint, acupuncture might be an attractive, beneficial, low-cost and low-risk treatment strategy in addition to standard HF medication.
The major aim of this thesis is to propose a clinical research protocol to test the effects of acupuncture in heart failure patients.
To fulfill this goal the author firstly presents the most recent theoretical and laboratorial background data based on an extensive literature research with the intention to support the following proposed clinical research protocol.
The theoretical fundamentals are presented in the first part of the thesis (theoretical framework, chapter one). A review of heart failure‟s epidemiology, etiopathophysiology and state-of-the-art treatment is presented followed by an historical and scientific overview of acupuncture. Thereafter a profound review of current data from acupuncture research in provided with special emphasis in cardiovascular disease.
The theoretical framework is expected to provide the needed support for the following detailed description of the proposed clinical research protocol (chapter two), the core of this master thesis. Noteworthy, by the time of this thesis submission, the respective research protocol has been approved by the Ethics Committee of the Hospital where the study will be undertaken.
Since the laboratorial work is yet to be undertaken, the third and forth chapters, respectively, of the thesis debate the expected results while the discussion is supported by literature findings. Finally, the thesis is enclosed with the author‟s future perspectives in regard to acupuncture research in the field of heart failure (chapter five).
25
CHAPTER ONE
27
1. Theoretical framework
1.1.
Heart failure
a worldwide burgeoning problem
Heart failure is a clinical syndrome that occurs in patients who, due to an inherited or acquired abnormality of cardiac structure and/or function, develop a constellation of clinical symptoms (dyspnea and fatigue) and signs (edema and crepitations) that lead to frequent hospitalizations, a poor quality of life, and a shortened life expectancy [4].
Worldwide more than 20 million people are affected. The overall prevalence of HF in the adult population in developed countries is 2%. HF prevalence follows an exponential pattern, rising with age, and affects 6–10% of people over the age of 65. Although the relative incidence of HF is lower in women than in men, women represent at least half of the cases of HF because of their longer life expectancy. In North America and Europe, the lifetime risk of developing HF is approximately one in five for a 40-year-old. The overall prevalence of HF is thought to be increasing in part because current therapies of cardiac disorders, such as myocardial infarction (MI), valvular heart disease, and arrhythmias, are allowing patients to survive longer [5-8].
Diseases of the circulatory system or cardiovascular diseases are the main cause of death in the European Union. They account for 42% of all deaths in the total population. Diseases of the circulatory system are more common at advanced ages: 81% of male deaths and 94% of female deaths are older than 65 years1. In Portugal, like in Europe, cardiovascular disease is the major cause of death, accounting for 40% of the total mortality2.
A 2006 Portuguese population-based study, with a representative sample of 739 non-institutionalized adults with age equal or superior to 45 years old from the city of Porto, found that the prevalence of heart failure in stage C (i.e., symptomatic heart failure according to the classification of the American College of Cardiology/American Heart Association), was 7,2%. The prevalence of HF in stage B (structural or functional heart disease but asymptomatic) was of 21.4%. On the basis of risk factors assessment, 48% were at high risk of heart failure despite the absence of structural or functional changes as evaluated by heart ultrasound studies [9].
1 http://epp.eurostat.ec.europa.eu/cache/ITY_OFFPUB/KS-30-08-357/EN/KS-30-08-357-EN.PDF 2 http://www.min-saude.pt/portal/conteudos/enciclopedia+da+saude/doencas/doencas+do+aparelho+circulatorio/doencasca rdiovasculares.htm
28
Despite many recent advances in the evaluation and management of HF, the development of symptomatic HF still carries a poor prognosis.
Community based studies indicate that 30–40% of patients die within 1 year of diagnosis and 60–70% die within 5 years, mainly from worsening HF or as a sudden event (probably because of a ventricular arrhythmia).
Although it is difficult to predict prognosis in an individual, patients with symptoms at rest have a 30–70% annual mortality rate, whereas patients with symptoms with moderate activity have an annual mortality rate of 5–10%. These figures show that functional status is an important predictor of patient outcome [10].
Although western science has developed a number of effective treatment strategies for this disease, treatment is not perfect and often is associated with side effects.
It has long been a dream to cure diseases by non-invasive measures that activate self-healing mechanisms, without using drugs or surgical operations.
In this context, there has been increasing interest from western countries in exploring so-called “complementary” or “alternative” therapies such as the role of acupuncture in cardiovascular disease.
1.2.
Etiopathophysiology of heart failure
– modern understanding and
ground for studies in acupuncture
In general, HF implies structural disease of the heart with functional consequences to the circulation, and it can theoretically occur from any form of heart disease.
The pathophysiology of heart failure (HF) is to some extent dependent on the etiology (table 1, page 30). There are many common features regardless of the underlying cause and there are always some underlying structural abnormalities. The clinical symptoms, as already mentioned, include dyspnea, fatigue, either at rest or during exertion, and in advanced cases there is usually evidence of salt and water retention.
Until recently, HF was considered to arise primarily in the setting of a depressed left ventricular ejection fraction (LVEF). However, epidemiological studies have shown that approximately one-half of patients who develop HF have a normal or preserved ejection fraction (EF) between 40–50%. Accordingly, heart failure is now broadly categorized into one of two groups: (1) HF with a depressed EF (commonly referred to as systolic failure) or (2) HF with a preserved EF (commonly referred to as diastolic failure) [10].
There is considerable overlap between the etiologies of these two conditions. Hypertension, coronary artery disease (CAD), valvular heart disease, and cardiomyopathy are leading causes of heart failure. Coronary artery disease is responsible for 60–75% of
29
cases of HF. Hypertension contribute to the development of HF in 75% of patients, including most patients with CAD. Both CAD and hypertension interact to augment the risk of HF, as does diabetes mellitus [10].
In 20–30% of the cases of HF with a depressed EF, the exact etiologic basis is not known. These patients are referred to as having nonischemic, dilated, or “idiopathic” cardiomyopathy. Prior viral infection or toxin exposure (e.g., alcoholic or chemotherapeutic) may also lead to a dilated cardiomyopathy. Moreover, a large number of the cases of dilated cardiomyopathy may be secondary to specific genetic defects, most notably those in the cytoskeleton. Most of the forms of familial dilated cardiomyopathy are inherited in an autosomal dominant fashion. Mutations of genes encoding cytoskeletal proteins (desmin, cardiac myosin, vinculin) and nuclear membrane proteins (lamin) have been identified thus far. Dilated cardiomyopathy is also associated with Duchene‟s, Becker's, and limb girdle muscular dystrophies. Conditions that lead to a high cardiac output (e.g., arteriovenous fistula, anemia) are seldom responsible for the development of HF in a normal heart. However, in the presence of underlying structural heart disease, these conditions can lead to overt HF.
Rheumatic heart disease remains a major cause of HF in Africa and Asia, especially in the young. Hypertension is an important cause of HF in the African and African-American populations. Chagas' disease is still a major cause of HF in South America. Not surprisingly, anemia is a frequent concomitant factor in HF in many developing nations. As developing nations undergo socioeconomic development, the epidemiology of HF is becoming similar to that of Western Europe and North America, with CAD emerging as the single most common cause of HF. Although the contribution of diabetes mellitus to HF is not well understood, diabetes accelerates atherosclerosis and is often associated with hypertension [10].
30
Table 1. Etiologies of Heart Failure
Depressed Ejection Fraction (<40%)
Coronary artery disease Nonischemic dilated cardiomyopathy Myocardial infarction Familial/genetic disorders
Myocardial ischemia Infiltrative disordersa
Chronic pressure overload Toxic/drug-induced damage
Hypertensiona Metabolic disordera
Obstructive valvular diseasea
Viral
Chronic volume overload Chagas' disease
Regurgitant valvular disease Disorders of rate and rhythm Intracardiac (left-to-right) shunting Chronic bradyarrhythmias Extracardiac shunting Chronic tachyarrhythmias
Preserved Ejection Fraction (>40–50%)
Pathological hypertrophy Restrictive cardiomyopathy Primary (hypertrophic
cardiomyopathies)
Infiltrative disorders (amyloidosis, sarcoidosis)
Secondary (hypertension) Storage diseases (hemochromatosis)
Aging Fibrosis
Endomyocardial disorders
Pulmonary Heart Disease
Cor pulmonale
Pulmonary vascular disorders
High-Output States
Metabolic disorders Excessive blood-flow requirements Thyrotoxicosis Systemic arteriovenous shunting Nutritional disorders (beriberi) Chronic anemia
31
1.2.1. Adaptive responses of the myocardium in heart failure
The heart is capable of short-term adaptations to off-set a perceived reduction in myocardial performance or excessive hemodynamic load.
The Frank-Starling mechanism, which states that the energy of contraction is a function of the muscle fiber length, allows increased preload or enhanced end-diastolic volume to sustain cardiac performance, both under normal conditions and during heart failure. The sympathetic nervous system (SNS) is activated, thus increasing the force of contraction of the heart and of the heart rate. It also facilitates the activation of the renin-angiotensin-aldosterone system (RAAS), which operates to restore circulating volume and protect blood pressure, maintaining perfusion of vital organs, via physiologic effects of angiotensin II.
The heart under chronic “siege” can also increase its own mass, with or without chamber dilatation, to augment the number of contractile filaments. The increase in myocardial mass and remodeling of the heart occurs over a prolonged period of time, while activation of the Frank-Starling mechanism, the sympathetic nervous system, and the RAAS occur nearly instantaneously. Together, the mechanisms converge to allow the heart to physiologically adapt to impaired function and perverse loading conditions. Circulatory homeostasis and cardiac output can be maintained despite a reduced ejection fraction. The adaptative myocardial responses allow blood pressure to be protected and allow the development of clinical overt heart failure to be forestalled. Additionally, release of counter-regulatory peptides from the heart (e.g. natriuretic peptides) promotes peripheral vasodilatation, natriuresis and diuresis, and off-sets the activation of the SNS and the RAAS.
These adaptive responses are evolutionary remnants that have provided a survival advantage long before heart failure was ever a threat.
1.2.2. Heart failure pathogenesis - how does heart failure begin?
HF may be viewed as a progressive disorder that is initiated after an index event (figure 1). This event may be clinically obvious, such as the sudden loss of large amounts of contractile tissue (e.g. acute myocardial infarction), or it might be insidious, such as the development of hypertension, aortic stenosis or insufficiency, or mitral insufficiency. The index event might go undiagnosed, such as the onset of lymphocytic infiltrative myocarditis or amyloid heart disease. It may also behave clinically silent, such as the expression of mutant gene or genes that eventually lead to hypertrophic or dilated cardiomyopathy.
32
The recognition of this primordial event and the position of the patient in the natural history of the syndrome are important in order to define an appropriate medical approach and treatment. However, in the “real world” many patients with heart failure do not have an obvious underlying cause identified, despite extensive evaluation.
The pace at which the natural history of HF unfolds is highly variable and depends on many extrinsic factors (diet, response to medications, compliance of drug therapy, etc.) as well as intrinsic factors (gene expression, age, severity of index event, etc) that often lie beyond the physician control.
Regardless of the nature of the inciting event, the feature that is common to each of these index events is that they all, in some manner, produce a decline in the pumping capacity of the heart. In most instances patients remain asymptomatic or minimally symptomatic following the initial decline in pumping capacity of the heart, or develop symptoms only after the dysfunction has been present for some time. Thus, when viewed within this conceptual framework, LV dysfunction is necessary, but not sufficient, for the development of the syndrome of HF.
1.2.3. The “muscle hypothesis” for chronic heart failure
During exercise the majority of patients with CHF are limited by dyspnea and fatigue with delayed recovery [11]. In parallel with the severity of circulatory failure, peak oxygen consumption is decreased, the ventilatory threshold appears earlier and the slope of the increase in oxygen consumption versus time is reduced [11]. Remarkably, this exercise limitation is independent of the impairment of left ventricular ejection fraction (LVEF). Therefore, the „muscle hypothesis‟ was proposed: raised levels of inflammatory cytokines are causing skeletal muscle fatigue and activation of muscle ergoreceptors, subsequently leading to an increase in ventilation, sensation of breathlessness, perception of fatigue and finally, autonomic dysbalance [12-14].
1.2.4. How adaptations in heart failure go wrong
Most of the adaptations that occur in patients with heart failure evolved for short-term benefit, such as to allow “fight or fright” (the SNS), to ward off hemodynamic compromise from blood loss (SNS and RAAS) or severe dehydration (RAAS). As rudimentary life-forms gradually moved from the salty oceans to land, those who developed mechanisms to conserve salt and water ensured themselves a survival advantage. These are very old evolutionary steps (approximately 600 million years old) and although they may still be
33
adaptive in the early stages of heart failure, ultimately become counterproductive, contributing to the pathophysiology of HF. The exact reasons why patients with left ventricular (LV) dysfunction may remain asymptomatic isn‟t yet clearly understood. One potential explanation is that a number of compensatory mechanisms become activated in the presence of cardiac injury and/or LV dysfunction, and they appear to be able to sustain and modulate LV function for a period of months to years (figure 1). Compensatory mechanisms that have been described thus far include (figure 2):
(1) Activation of the renin-angiotensin-aldosterone and adrenergic nervous systems, which are responsible for maintaining cardiac output through increased retention of salt and water
(2) Increased myocardial contractility.
(3) Activation of countervailing vasodilatory molecules that offset the excessive peripheral vascular vasoconstriction, such as the atrial and brain natriuretic peptides (ANP and BNP), prostaglandins (PGE2 and PGI2), and nitric oxide (NO).
(4) Genetic background, gender, age, or environment may influence these compensatory mechanisms, which are able to modulate LV function within a physiologic/homeostatic range, such that the functional capacity of the patient is preserved or is depressed only minimally.
Figure 1. Pathogenesis of heart failure with depressed ejection fraction. The transition
from adaptive to maladaptive activation of the SNS and RAAS, and from early structural changes in the heart and vasculature to progressive organ dysfunction, characterizes the pathophysiology of HF. The exact mechanisms that are responsible for this transition from asymptomatic to symptomatic are not known. Ultimately, there is the increased activation of potentially detrimental neurohormonal, adrenergic, and cytokines systems, more perverse loading condition, change in the size and shape of the heart, ineffective circulatory homeostasis, and multi-organ failure [10].
34
Neurohumoral activation characterizes a state in which the neural and hormonal systems designed to maintain adequate organ perfusion are turned on to excessively high levels. This activation may include the sympathetic nervous system (SNS), renin-angiotensin-aldosterone-system, vasopressin, and atrial natriuretic peptide. [15]. Although initially this is an adaptive response to cardiac injury, prolonged activation of these support systems inevitably leads to progressive heart failure symptoms and ultimately cardiac death.
In an animal model of early left ventricular dysfunction without overt heart failure, plasma norepinephrine levels are elevated, indicative of early SNS activation [16].
Power spectral analysis of heart rate variability suggests that there is sympathetic activation early in the course of left ventricular dysfunction in a canine model of heart failure [17].
In humans, it was demonstrated that sympathetic activation with ventricular dysfunction occurs even in the absence of heart failure, after the finding of high plasmatic levels of norepinephrine in this situation [18]. Using the technique of microneurography to record muscle sympathetic nerve activity directly from a peroneal nerve in humans, it was found that even in patients with mild heart failure, sympathetic nerve activity to the muscle circulation is increased. Interestingly, patients with heart failure secondary to diastolic dysfunction do not have elevated plasma norepinephrine [19]. These findings indicate that the neurohormonal excitation reflects systolic ventricular dysfunction and not simply clinical heart failure.
The heart is the first organ to be targeted by the increase in SNS activation [20]. Measurements of cardiac adrenergic activity using MIBG (iodine-131-meta-iodobenzylguanidine) scintigraphy indicate that cardiac sympathetic nerve activity is increased in patients with heart failure at a time when volume and pressure overload are not present [21, 22]. In patients with mild heart failure, cardiac sympathetic nerve activity, as reflected by norepinephrine levels, is increased threefold above control before increased sympathetic nerve activity to the kidney or muscle circulations.[20]
Sympathetic nerve activation decreases ventricular fibrillation threshold, predisposing to sudden death [23]. Heart failure patients with the greatest activation of the sympathetic nervous system are associated with poorest prognosis, progression of the disease, and higher mortality [24-30].
Possible mechanisms implicated in the sympathetic activation in heart failure include 1) attenuation of tonically inhibitory input to the central nervous system; 2) activation of excitatory input to the central nervous system; and/or 3) changes in humoral or local brain factors affecting central neural sympathetic regulation (figure 2). Attenuation of the normal inhibitory baroreflex restraint on SNS would lead to SNS activation [15].
35
Sympathetic stimulation of the kidney leads to the release of renin, with a resultant increase in the circulating levels of angiotensin II and aldosterone. The activation of the renin-angiotensin-aldosterone system promotes salt and water retention and leads to vasoconstriction of the peripheral vasculature, myocyte hypertrophy, myocyte cell death, and myocardial fibrosis.
Figure 2. Activation of the
neurohormonal system in heart failure [10].
Patients with heart failure have a blunted Starling relationship at rest and during exercise. For any degree of stretching of the myocardium due to elevated end-diastolic volume, there is less incremental change in the contractile state of the myocardium. Ventricular function curves cannot be elevated to normal ranges by the adrenergic overdrive, in part because the failing heart is relatively depleted of tissue norepinephrine and 1-receptor density. The ability of patients to respond to increased end-diastolic volume is clearly diminished, i.e., they manifest less “cardiac reserve” when called upon to increase myocardial contractility.
Heart failure is accompanied by an increased vascular tone in attempt to maintain perfusion pressure in the face of falling blood pressure. This mechanism is parallel to the setting of volume depletion, which has had millions of years to allow for favorable mutation to counteract the problem, so that species could adjust to the paucity of salt and water
36
and enhance perfusion to vital organs. This net outcome results from the activity of the SNS and RAAS, and they are activated in very early asymptomatic HF.
Distribution of blood flow is altered in HF, directing it towards vital organs (brain, heart, splanchnic beds), in spite of the reduction in cardiac output. Skeletal muscle flow in augmented at rest in HF, while renal blood flow is diminished. Structural changes in vessel walls also take place, reducing vascular compliance. Sodium content of the vascular wall is increased, contributing to arterial stiffening.
Baroreceptors are sensory receptors that sense changes in mechanical stretch and their activity may also be influenced by local ionic or humoral mechanisms. Arterial baroreceptors tonically inhibit central sympathetic neural outflow. In heart failure, baroreflex control of sympathetic nerve activity is abnormal [31, 32], leading to heightened sympathetic activity. It has been demonstrated that SNS activity is only elevated to those organs and tissues subject to baroreflex restraint in heart failure and not to all organs and tissues [33, 34]. SNS activation to muscle circulation, which is under baroreflex control, is elevated [19, 33, 35]. In contrast, sympathetic nerve activity directed to the skin, a tissue free from baroreflex control, is not elevated, even in patients with advanced heart failure [33]. Sympathetic neural responses to baroreceptor modulation are abnormal in heart failure patients, even in those with mild heart failure [36]. This blunted baroreflex restraint would lead to elevated sympathetic traffic.
Response to hyperemia is also blunted and exercise-induced vasodilatation is attenuated. This is at least in part the consequence of peripheral vascular endothelial dysfunction. Vasodilator response can be restored by administration of L-arginine, a precursor of endothelium-derived nitric oxide (NO). The NO‟s role is discordant in the peripheral vasculature and heart muscle: the expression of NO synthase in peripheral vasculature is impaired, whereas inducible NO synthase may be increased in myocardium, NO may mediate the effects of inflammatory cytokines (tumor necrosis factor-) on -adrenergic receptor function, leading to diminished myocardial responsiveness to catecholamines [37].
Redistribution of blood flow to more vital organs likely offers and additional survival advantage. Over time such adaptive responses may worsen renal function, impair exercise tolerance, favor tissue and circulatory congestion. The activation of the SNS in HF is still not clearly understood.
Changes in size, shape, geometry of the heart are likely the result of excessive SNS and RAAS activity, which act as growth factors to promote myocyte hypertrophy [38].
37
1.2.5. Ventricular remodeling
When the heart is under volume or pressure overload, the excessive loading condition leads to myocyte hipertrophy. Pressure overload causes concentric hypertrophy and volume overload tends to eccentric hypertrophy. Cellular division of cardiac myocytes is a possibility, but very unusual. The change in size and shape of the heart has been called myocardial remodeling. It seems that different gene patterns are implicated for each of the above mentioned hypertrophy phenotypes, and usually there is a hybrid of the two[39]. As the LV chamber dilates, systolic wall stress increases, impairing LV systolic function. Elongation of myocytes is associated with chamber dilation, including cell dropout (apoptosis and necrosis) and “slippage” of myocytes away from proper alignment [40]. The large, less economical, dilated heart is more prone to dysrhytmias, and dyssynchrony (electrical and mechanical). Cardiomyopathy is the byproduct of long-standing adverse loading conditions, unrelenting neurohormonal stimulation, increased production of matrix metalloproteinases (MMPs) and cell dropout (apoptosis or necrosis). Alterations in calcium excitation-contraction coupling, -adrenergic receptor coupling to downstream proteins, myosin adenosine triphosphatase (ATPase) activity, regulatory proteins, occur in HF. Their quantitative contribution has been elusive.
The decreased cardiac output in HF patients results in an "unloading" of high-pressure baroceptors in the left ventricle, carotid sinus, and aortic arch. This unloading leads to the generation of afferent signals to the central nervous system (CNS) that stimulate cardioregulatory centers in the brain which stimulate the release of arginine vasopressin (AVP) from the posterior pituitary. AVP [or antidiuretic hormone (ADH)] is a powerful vasoconstrictor that increases the permeability of the renal collecting ducts, leading to the reabsorption of free water. These afferent signals to the CNS also activate efferent sympathetic nervous system pathways that innervate the heart, kidney, peripheral vasculature, and skeletal muscles [10].
The increase in wall thinning along with the increase in afterload created by LV dilation leads to a functional afterload mismatch that may contribute further to a decrease in stroke volume. Moreover, the high end-diastolic wall stress might be expected to lead to: (1) hypoperfusion of the subendocardium, with resultant worsening of LV function; (2) increased oxidative stress, with the resultant activation of families of genes that are sensitive to free radical generation (e.g., TNF and interleukin 1); and (3) sustained expression of stretch-activated genes (angiotensin II, endothelin, and TNF) and/or stretch activation of hypertrophic signaling pathways [10].
38
Simultaneously to the increasing in myocyte size, there is augmented collagen deposition within the heart (reactive or replacement collagen). In HF, fibroblasts produce more collagen, and its deposition alters the function of the heart, since it makes the chamber stiff. Synthesis of collagen may be related to activation of fibroblasts by angiotensin II, aldosterone, and altered stress /strain forces on the heart. It has been assumed that MMP are active in HF contributing the collagen deposition. The action of tissue MMP inhibitors (TIMPs) may be decreased in myocardium, thus facilitating the degradation of collagen.
Despite the reduction or dissolution of collagen normally present to align myocytes, the increased interstitial collagen may contribute for diastolic dysfunction [41]. Muscle and chamber stiffness is overall increased which has important consequences for LV filling pressure and its relation to left ventricular end-diastolic volume.
There is a reduction in the density of -receptor, due to excessive local concentration of norepinephrine, and there appears to be an unhinging of the membrane bound -receptors from the Gs proteins and a tighter coupling to the Gi proteins, thus attenuating the response to excessive norepinephrine on the heart. This is presumably an evolutionary conserved protective effect, preventing lethal overstimulation of the heart by catecholamines. However, the net result is a likely reduction in myocardial reserve.
Coronary blood flow at rest is often normal in patients with heart failure, but has been found to be reduced in some patients with dilated cardiomyopathy and in some with ischemic cardiomyopathy. Capillary density may be reduced has LV mass increases. Patients with LVH demonstrate a reduced coronary reserve, consistent with diminished hyperemic response common to many vascular beds in the setting of heart failure. Coronary blood flow may also diminish to match reduced contractile state, a condition referred to as “hibernating myocardium”, which is viable muscle tissue, thus may improve with revascularization [42].
1.2.6. Systolic Dysfunction
In order to understand how the changes that occur in the failing cardiac myocyte contribute to depressed LV systolic function in HF, it is important to understand the biology of the cardiac muscle cell. Sustained neurohormonal activation results in transcriptional and posttranscriptional changes in the genes and proteins that regulate excitation-contraction coupling and cross-bridge interaction. Collectively, these changes impair the ability of the myocyte to contract and, therefore, contribute to the depressed LV systolic function observed in patients with HF [10].
39
1.2.7. Diastolic Dysfunction
Myocardial relaxation is an ATP-dependent process that is regulated by uptake of cytoplasmic calcium into the sarcoplasmic reticulum (SR) by sarcoplasmic reticulum Ca2+ adenosine triphosphatase (SERCA2A) and extrusion of calcium by sarcolemmal pumps.
Accordingly, reductions in ATP concentration, as occurs in ischemia, may interfere with these processes and lead to slowed myocardial relaxation. Alternatively, if LV filling is delayed because LV compliance is reduced (e.g., from hypertrophy or fibrosis), LV filling pressures will similarly remain elevated at end diastole. An increase in heart rate disproportionately shortens the time for diastolic filling, which may lead to elevated LV filling pressures, particularly in noncompliant ventricles. Elevated LV end-diastolic filling pressures result in increases in pulmonary capillary pressures, which can contribute to the dyspnea experienced by patients with diastolic dysfunction. Importantly, diastolic dysfunction can occur alone or in combination with systolic dysfunction in patients with HF.
Controversy still remains regarding the definition of “diastolic heart failure” and what the core lesion might be. Importantly, the two conditions (i.e., systolic and diastolic heart failure) often coexist and are indistinguishable at the bedside [10, 43].
1.3.
Conventional therapeutic approach to heart failure
In the past treatment of heart failure was focused on drugs to improve ventricular function directly with positive inotropic drugs. Nowadays, therapeutic modulation of neurohumoral activation is a key to successful treatment of heart failure.
Although the failing heart may include both systolic and diastolic dysfunctions, to the present body of knowledge, the initial step is to differentiate the predominant dysfunction (systolic from diastolic heart failure).
Noteworthy, the overwhelming number of studies in HF population has been performed in patients with the syndrome of systolic dysfunction.
Although there is a growing recognition that as many as 30-50% of all hospitalized patients with HF have preserved ejection fraction (EF>40-50%) there remains a paucity of evidence-based recommendations for this group of diastolic HF. Most reviews underline the importance of excluding significant coronary ischemia and that control of hypertension is critical. Control of heart rate is useful in those patients presenting with atrial arrhythmias (e.g. atrial fibrillation). A search for exacerbating drugs may be fruitful since these patients frequently have comorbid conditions (obesity, diabetes, arthritis, renal failure). It is also appropriate to screen sleep apnea [44, 45].
40
Dyspnea may be treated by reducing total blood volume (dietary sodium restriction and diuretics), decreasing central blood volume (nitrates), or blunting neurohormal activation with angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB), and/or beta-blockers. Treatment with diuretics and nitrates should be initiated at low doses to avoid hypotension and fatigue.
In patients with systolic dysfunction (EF<40%) it is mandatory to search for reversible or correctable causes of the low systolic function. In the United States (US) the most common cause of dilated cardiomyopathy is chronic ischemia related to coronary artery obstruction [46-52]. Other correctable etiologies include illicit drug use or alcohol use, thyroid disorders, uncontrolled hypertension.
It is important to exclude the role of coronary artery disease (CAD) as the cause of left ventricular dysfunction, since it has been estimated that CAD is the cause of HF in two-thirds of patients with left ventricular dysfunction [53].
In patients with HF and angina coronary revascularization was shown to improve symptoms and survival, although patients with markedly impaired ventricular function were not included in these studies.
As many as one-third of patients with nonischemic cardiomyopathy may complain of chest pain suggestive of angina and in these patients noninvasive imaging may demonstrate perfusion defects and segmental wall motion abnormalities. It is therefore reasonable to proceed directly to coronary angiography in young patients with HF, angina and left ventricular dysfunction. However, it is still a matter of debate whether or not routine coronary angiography is warranted in all patients who present with HF and left ventricular dysfunction in the absence of chest pain, because coronary revascularization has not been clearly demonstrated to improve survival in patients without angina [53]. Nonetheless, there are data to suggest that revascularization might improve ventricular function. Therefore, it is a reasonable strategy to exclude coronary artery disease in all patients with newly diagnosed HF and left ventricular systolic dysfunction even in the absence of chest pain.
The ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult has been instrumental in more clearly articulating the early stages of HF, or the preclinical phase of the disease, and the patterns of disease associated with subsequent progression to clinical symptoms. A new approach to the classification of HF was established in order to appropriately characterize HF evolution in 4 stages (figure 3) [54].
41 Figure 3. Stages in the evolution of HF and recommended therapy by stage proposed by the ACC/AHA guideline s for the evaluation and management of chronic HF in adults [54].
HF should be viewed as a continuum that is comprised of four interrelated stages.
Stage A includes patients who are at high risk for developing HF but without structural
heart disease or symptoms of HF (e.g., patients with diabetes mellitus or hypertension).
Stage B includes patients who have structural heart disease but without symptoms of HF
(e.g., patients with a previous myocardial infarction (MI) and asymptomatic LV dysfunction). Stage C includes patients who have structural heart disease and have developed symptoms of HF (e.g., patients with a previous MI with dyspnea and fatigue).
Stage D includes patients with refractory HF requiring special interventions (e.g., patients
with refractory HF who are awaiting cardiac transplantation).
In this continuum, every effort should be made to prevent HF, not only by treating the preventable causes of HF (e.g., hypertension) but by treating the patient in Stages B and C with drugs that prevent disease progression (e.g., ACE inhibitors [ACEi] and beta blockers [BB]) and by symptomatic management of patients in stage D. Once patients have developed structural heart disease, their therapy depends on their NYHA functional classification. Although this classification system is notoriously subjective and has large interobserver variability, it has withstood the test of time and continues to be widely applied to patients with HF. For patients who have developed LV systolic dysfunction but remain asymptomatic, the goal should be to slow disease progression by blocking neurohormonal systems that lead to cardiac remodeling. For patients who have developed symptoms the primary goal should be to alleviate fluid retention, lessen disability, and reduce the risk of further disease progression and death. These goals generally require a strategy that combines diuretics (to control salt and water retention) with neurohormonal interventions (to minimize cardiac remodeling).
42
1.3.1. Treating elevated cardiac filling pressures
When volume overload is identified the strategy is focused on relieving congestion. Diuretics produce symptomatic benefits more rapidly than any other drug used for HF. Although some patients with dilated cardiomyopathy who have been stabilized on a standard regimen of neurohormonal antagonists may be effectively managed without diuretics, the large majority of patients will need a regular dose of diuretics.
1.3.2. Neurohormonal antagonists
All patients with low EF, in the absence of aortic outflow obstruction, are treated with both ACE inhibitor and a -blocker. For historical reasons, clinicians commonly start an ACE inhibitor first and add a -blocker as a second agent but recent data suggest that starting a B-blocker as initial therapy has some advantages. The ultimate task is to maintain patients on both drugs and at the highest tolerated dosages. Some patients not tolerate ACE inhibitor due to dry cough, exacerbation of renal failure, and angioedema. Such patients may be treated with direct ARBs, which bind to angiontensin II receptors, and are also a proven effective treatment in HF.
Additional pharmacological agents in HF symptomatic patients despite treatment with adequate doses of -blocker and ACE inhibitor are digoxin and aldosterone antagonists.
The use of digoxin is a Class I indication in conjunction with diuretics, ACEi, and BB (3). It has been demonstrated that digoxin use conveys a significant decrease in risk of dead or hospitalizations due to worsening HF and that it is well-tolerated and associated with few adverse side effects.
Aldosterone antagonists are recommended in patients with symptoms of HF despite the use of digoxin, diuretics, ACEi, and BB. The aldosterone antagonists, spironolactone, conferred a significant reduction in the risk of death as well as a reduction in the risk of hospitalization from cardiovascular causes.
1.3.3. Conventional non-pharmacological therapies
Chronic heart failure generates many debilitating symptoms for the sufferer. Nonpharmacologic treatment modalities play an important role, alongside effective modern pharmaceutical, surgical, and device therapies. These treatments include those lifestyle measures that reduce the risk of underlying diseases (coronary artery disease, diabetes, hypertension, hyperlipidemia, and those lifestyle interventions that benefit either the symptoms or prognosis of established heart failure.
43
HF patients should be advised to stop smoking and to limit alcohol consumption to two standard drinks per day in men or one per day in women. Patients suspected of having an alcohol induced cardiomyopathy should be urged to abstain from alcohol consumption indefinitely. Extremes of temperature and heavy physical exertion should be avoided. Certain drugs are known to make HF worse and should also be avoided. For example, nonsteroidal anti inflammatory drugs, including cyclooxygenase 2 inhibitors, are not recommended in patients with chronic HF because the risk of renal failure and fluid retention is markedly increased in the presence of reduced renal function or ACE inhibitor therapy. Patients should receive immunization with influenza and pneumococcal vaccines to prevent respiratory infections. It is equally important to educate the patient and family about HF, the importance of proper diet, as well the importance of compliance with the medical regimen.
Although heavy physical labor is not recommended in HF, routine modest exercise has been shown to be beneficial in patients with NYHA class I–III HF. For euvolemic patients, regular isotonic exercise such as walking or riding a stationary bicycle ergometer, as tolerated, should be encouraged. Some trials of exercise training have led to encouraging results with reduced symptoms, increased exercise capacity, and improved quality and duration of life. One study evaluated the effects of combined endurance/resistance training on NT-proBNP levels in patients with HF. Results suggested that combined endurance/resistance training significantly reduced circulating levels of NT-proBNP in patients with HF arguing against any increase in adverse remodeling. Regarding cardiac rehabilitation, some supervised in-hospital training is necessary, and home-based training can also be recommended in well-evaluated patients.
The benefits of weight loss by restriction of caloric intake have not been clearly established. Dietary restriction of sodium (2–3 g daily) is recommended in all patients with HF and preserved or depressed EF. Further restriction (<2 g daily) may be considered in moderate to severe HF. Fluid restriction is generally unnecessary unless the patient develops hyponatremia (<130 mEq/L), which may develop because of activation of the renin-angiotensin system, excessive secretion of antidiuretic hormone, or loss of salt in excess of water from diuretic use. Fluid restriction (<2 L/day) should be considered in hyponatremic patients or for those whose fluid retention is difficult to control despite high doses of diuretics and sodium restriction. Caloric supplementation is recommended for patients with advanced HF and unintentional weight loss or muscle wasting (cardiac cachexia); however, anabolic steroids are not recommended for these patients because of the potential problems with volume retention. The use of dietary supplements ("nutraceuticals") should be avoided in the management of symptomatic HF because of the lack of proven benefit and the potential for significant (adverse) interactions with
44
proven HF therapies. Some authors have demonstrated an important role for the dietician in a multidisciplinary HF program, by showing significant improvements in quality of life scores after the dietician intervention, suggesting improved nutrition and avoidance of worsening HF due to excessive sodium intake [55].
The management of patients with systolic HF includes the evaluation for additional nonpharmacologic therapies that have been demonstrated to improve survival.
Cardiac resynchronization therapy (CRT) may reduce symptoms, improve functional capacity, and possible improve mortality in select patients with systolic HF [56, 57]. Currently patients who may benefit from CRT are those presenting with a prolonged QRS interval (>140ms). However, the surface electrocardiogram lacks sensitivity in identifying patients who have contraction dyssynchrony [58]. It is appropriate to consider CRT in patients with refractory symptoms of HF and evidence of either interventricular or intraventricular dyssynchrony.
1.3.4. Refractory heart failure
Cardiac transplantation is an option for only very select few of this group. In patients who are not candidates for cardiac transplantation, permanent ventricular assist devices (VAD) may improve survival and quality of life [59-62]. These devices may become technologically improved in the future and may become a wider available solution.
In this group of patients, repeat discussion about end-of-life decisions and wishes must be undertaken. Home inotropic therapy may increase mortality but it may improve quality of life. Recent studies demonstrated that in many patients with stage D, quality of life is more desired than length of life. Hospice is an appropriate alternative for many patients, as compared to an endless cycle of increasingly longer hospital admissions [63].
Implantable cardiac defibrillators (ICDs) in systolic HF are indicated in patients with cardiac arrest due to ventricular tachycardia or ventricular fibrillation or hemodynamically significant sustained VT. It is class IIa indication in patients with ischemic cardiomyopathy with an EF less than 30% who are at least 1 month post myocardial infarction or 3 months post coronary artery revascularization [10, 64-68].
45
1.4.
Acupuncture
an historical and scientific overview
The word "acupuncture" is derived from the Latin words "acus" (needle) and "punctura" (penetration). Acupuncture originated in China approximately 2500 years ago (one of the oldest medical procedures in the world) and is a treatment based on the ancient Chinese Medicine.
Over its long history and dissemination, acupuncture has diversified and encompasses a large array of styles and techniques. Common styles include Traditional Chinese, Japanese, Korean, Vietnamese, and French acupuncture, as well as specialized forms such as hand, auricular, and scalp acupuncture.
Acupuncture also refers to a family of procedures used to stimulate anatomical points. Aside from needles, acupuncturists can incorporate manual pressure, electrical stimulation, magnets, low-power lasers [69-71], heat, and ultrasound.
Despite this diversity, the techniques most frequently used and studied are manual manipulation and/or electrical stimulation of thin, solid, metallic needles inserted into skin. The precise origin of acupuncture is a source of debate. There is no single archaeological finding that points to a momentary emergence of acupuncture. Rather evidence exists for a variety of potential antecedent practices like bloodletting, tattoos for religious purposes, and use of bones to extract abscess [72]. Older recompilations and analyses of the system and new archaeological findings suggest that Chinese Medicine did not start with the Yellow Emperor‟s Classic on Internal Medicine 2300 years ago. It seems that Chinese Medicine may be three times older than that, leading to the fact that the origin and the bibliographic sources are within the dark of history [73].
According to other authors, texts on acupuncture date back to 206 BC, although the Yellow Emperor, Huang Di, the originator of traditional Chinese medicine lived in 2697 BC. Others mention that the first written document to record the use of acupuncture is the Nei Jing (Inner Classic of the Yellow Emperor) dated approximately 100 BC. It is a collection of 81 treatises divided into two parts [74]. By the time of its compilation, acupuncture was already a signature therapy of Chinese medicine.
The importance of acupuncture as medical therapy emerged around the same time that Confucianism and Taoism gained prominence in China. These philosophies are imprinted in the fundamental principles of acupuncture theory, and their influence is patently evident throughout the ancient texts [72, 75]. Acupuncture underwent significant development and expansion within the ensuing 1500 years and arguably climaxed in the Ming era

![Figure 2. Activation of the neurohormonal system in heart failure [10].](https://thumb-eu.123doks.com/thumbv2/123dok_br/15881197.1089289/35.892.148.724.260.700/figure-activation-neurohormonal-heart-failure.webp)


![Table 3. Effect of gallbladder bradykinin-induced blood pressure reflex response [127]](https://thumb-eu.123doks.com/thumbv2/123dok_br/15881197.1089289/69.892.130.791.930.1129/table-effect-gallbladder-bradykinin-induced-pressure-reflex-response.webp)