www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
REVIEW
ARTICLE
Feeding
methods
for
children
with
cleft
lip
and/or
palate:
a
systematic
review
夽
Giesse
Albeche
Duarte
a,∗,
Ramon
Bossardi
Ramos
b,
Maria
Cristina
de
Almeida
Freitas
Cardoso
aaUniversidadeFederaldeCiênciasdaSaúdedePortoAlegre,ProgramadePós-graduac¸ãoemCiênciasdaReabilitac¸ão---Linha
Musculoesquelética,PortoAlegre,RS,Brazil
bHospitaldeClínicasdePortoAlegre,PortoAlegre,RS,Brazil
Received6July2015;accepted8October2015 Availableonline2March2016
KEYWORDS Cleftlip; Cleftpalate; Feedingmethods; Breastfeeding; Swallowingdisorders
Abstract
Introduction:Feedingdifficultiesinchildrenwithcleftlipandpalate(CLP)arefrequentand appearatbirthduetoimpairmentofsuckingandswallowingfunctions.Theuseofappropriate feedingmethodsforthedifferenttypesofcleftandtheperiodofthechild’slifeisofutmost importancefortheirfulldevelopment.
Objective:ReviewstudiescomparingfeedingmethodsforchildrenwithCLP,pre-and postop-eratively.
Methods:ThesearchcoveredtheperiodbetweenJanuary1990andAugust2015inthePubMed, LILACS, SciELO,andGoogle Scholardatabasesusing theterms:cleftlip orcleftpalateand feedingmethodsorbreastfeedingorswallowingdisordersandtheirsynonyms.Thissystematic reviewwasrecordedinPROSPEROundernumberCRD42014015011.Publicationsthatcompared feedingmethodsandpublishedinPortuguese,English,andSpanishwereincludedinthereview. Studieswithassociatedsyndromes,orthopedicmethods,orcomparingsurgicaltechniqueswere notincluded.
Results:Thethreereviewedstudiesontheperiodpriortosurgicalrepairshowedbetter feed-ingperformancewiththreedifferentmethods:squeezablebottle,syringe,andpaladaibottle. Onlyonestudyaddressedthepostoperativeperiodofcleftlipand/orpalaterepair,with pos-itiveresultsforthefeedingmethodwithsuction.Likewise,thepost-liprepairstudiesshowed betterresultswithsuctionmethods.Afterpalatoplasty,twostudiesshowedbetterperformance withalternativefeedingroutes,onestudywithsuctionmethod,andonestudythatcompared methodswithnosuctionshowedbetterresultswithspoon.
夽 Pleasecitethisarticleas:DuarteGA,RamosRB,CardosoMC.Feedingmethodsforchildrenwithcleftlipand/orpalate:asystematic
review.BrazJOtorhinolaryngol.2016;82:602---9.
∗Correspondingauthor.
E-mail:duarte.giesse@gmail.com(G.A.Duarte).
http://dx.doi.org/10.1016/j.bjorl.2015.10.020
Conclusion: Thestudiesshowthatpriortosurgicalrepair,theuseofalternativemethodscanbe beneficial.Inthepostoperativeperiodfollowingliprepair,methodswithsuctionaremore ben-eficial.However,inthepostoperativeperiodofpalatoplasty,therearedivergencesofopinion regardingthemostappropriatefeedingmethods.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE Fendalabial; Fissurapalatina; Métodosde alimentac¸ão; Aleitamento materno; Transtornos dedeglutic¸ão
Métodosdealimentac¸ãoparacrianc¸ascomfissuradelábioe/oupalato:umarevisão sistemática
Resumo
Introduc¸ão: Asdificuldades dealimentac¸ão em crianc¸as comfissura labiopalatina (FLP)são frequentesesurgemlogoaonascimento,devidoaocomprometimentodasfunc¸õesdesucc¸ãoe deglutic¸ão.Autilizac¸ãodemétodosdealimentac¸ãoadequadosaosdiferentestiposdefissura eaomomentodavidadacrianc¸aéprimordialparaseuplenodesenvolvimento.
Objetivo: Revisar estudosque compararammétodos de alimentac¸ãopara crianc¸as comFLP antesdacorrec¸ãocirúrgicaenopós-operatório.
Método: Abuscacompreendeuoperíodoentrejaneirode1990eagostode2015,nasbases dedadosPubMed,LILACS,ScieloeGoogleAcadêmicoseutilizando ostermos:FendaLabial ou Fissura Palatina e Métodos de Alimentac¸ão ou Aleitamento Materno ou Transtornos de deglutic¸ão e seus sinônimos. Esta revisão sistemática foi registrada no PROSPERO sob o númeroCRD42014015011.Foramincluídaspublicac¸õescomparandométodosdealimentac¸ão nos idiomas português, inglês e espanhol. Pesquisas com síndromes associadas, métodos ortopédicosoucomparandotécnicascirúrgicasnãoforamincluídas.
Resultados: Os três estudos revisados sobre o período que antecede a correc¸ão cirúrgica apresentaram melhordesempenhonaalimentac¸ãocomtrêsdiferentesmétodos:mamadeira compressível,seringaepaladai.Umúnicoestudoabordouopós-operatóriodefissuradelábio e/oupalato,apresentandoresultadospositivosparaaalimentac¸ãocommétodocomsucc¸ão. Damesmaforma,nopós-queiloplastiaosestudosmostrarammelhoresresultadoscom méto-doscomsucc¸ão.Apósapalatoplastia,doisestudosapresentarammelhordesempenhocomvia alternativadealimentac¸ão;umestudocommétodocomsucc¸ão;eoutroquecomparoumétodos semsucc¸ãoapresentoumelhoresresultadoscomcolher.
Conclusão:Osestudosmostramque,antesdacorrec¸ãocirúrgica,autilizac¸ãodemétodos alter-nativospodeapresentarbenefícios.Nopós-operatóriodequeiloplastia,osmétodoscomsucc¸ão sãomaisbenéficos.Porém,noperíodopós-operatóriodepalatoplastiahádivergênciasquanto aosmétodosmaisindicados.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Cleftlipandpalate(CLP)arecongenitalmalformationsthat
canaffectthelip,thepalate,orboth,1resultingfromerrors
intheembryonicfacialfusionprocess2duetoalterationsin
thenormal developmentoftheprimaryand/or secondary
palate.3
Withthediagnosisofcleftpalate/lip,feedingisamajor
concernfor parents.4 Feeding difficultiesappear atbirth,
due to impairment of the suction and swallowing
mech-anisms resulting from the alteration in the anatomical
structures. At this early stage, the priority is monitoring
infantnutritionandweightgain.5
SurgeryistheinitialtreatmentforCLP.Liprepairsurgery
isrecommendedby3monthsoflifeandforthepalate,up
to9or12months,asthechronologyofproceduresadmits
somevariationdependingonthespecializedcenter.6,7
Ade-quatenutritionisalsoimportantforthechildtobeableto
undergothecleftrepairsurgery,i.e.,stableweightgainwith
nohealth alterations and the capability to safely receive
anesthetics.8
Afterthesurgicalprocedure,itisestimatedthatthechild
willabletofeedwithlessdifficulty,astheoralstructures
willberepaired.However,intheimmediatepostoperative
period,theconductregardingfeeding alsovaries,
accord-ingtotheprotocolsusedbythedifferentdepartmentsand
accordingtothetypeofcleft.
Postcleft-liprepairfeedingtechniquescanvary
consid-erably.Therecommendationsusuallyrangefromimmediate
uptosixweeks.9Afterpalatoplasty(palatereconstructive
surgery),thisdivergenceisevengreaterandthereare
cen-tersthatadoptprotocolsin whichbottlesand nipplesare
prohibitedforaperiodof30days.10
Basedontheliterature,thissystematic reviewaimsto
describe studies comparing feeding methods for children
withdifferenttypesofcleftlip/palateinthepre-and
post-operativeperiods,aimingtotrainparentsandprofessionals
fortheoftendifficulttaskoffeedingchildrenwithCLP.
Methods
Searchstrategy
The literature search was carried out from January 1,
1990 to August 31, 2015. The search was performed
in the PubMed, LILACS, SciELO and Google Scholar
databases, as they include most of the publications in
thisarea.This systematicreviewwasconductedaccording
tothePRISMA Statement11,12 and registered at PROSPERO
(http://www.crd.york.ac.uk/PROSPERO/) under number CRD42014015011.
The search strategy consisted in the following terms
(Mesh):(‘‘Cleft Lip’’[Mesh]OR‘‘CleftPalate’’ [Mesh]OR
‘‘EctodermalDysplasia’’OR‘‘CleftLips’’ OR‘‘Lip,Cleft’’
OR‘‘Lips,Cleft’’ORHarelipORHarelipsOR‘‘CleftPalates’’
OR‘‘Palate,Cleft’’OR‘‘Palates,Cleft’’OR‘‘CleftPalate,
Isolated’’) AND (‘‘Feeding Methods’’ [Mesh]OR ‘‘Feeding
Method’’ OR ‘‘Method, Feeding’’ OR ‘‘Methods,
Feed-ing’’ OR ‘‘Breast Feeding’’ [Mesh]OR ‘‘Feeding, Breast’’
OR Breastfeeding OR ‘‘Breast Feeding, Exclusive’’ OR
‘‘ExclusiveBreastFeeding’’OR‘‘Breastfeeding,Exclusive’’
OR‘‘ExclusiveBreastfeeding’’OR‘‘Deglutition Disorders’’
[Mesh] OR ‘‘Deglutition Disorder’’ OR ‘‘Disorders,
Deg-lutition’’ OR ‘‘Swallowing Disorders’’ OR ‘‘Swallowing
Disorder’’OR‘‘Dysphagia’’OR‘‘OropharyngealDysphagia’’
OR‘‘Dysphagia,Oropharyngeal’’).
Selectioncriteria
Studies that comparedfeeding methods for children with
cleftlipand/orpalateandpublishedinEnglish,Portuguese,
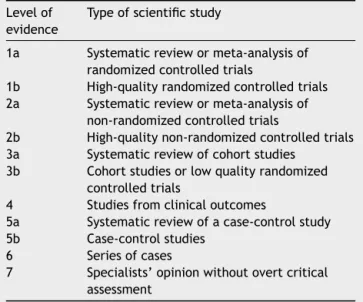
or Spanish, with level of evidence 1b to 4 according to
the criteria proposed by the American
Speech-Language-Hearing Association (ASHA)13 were included in the review
(Table1). Studies of syndromes associated withthe
pres-enceofCLPwereexcluded,aswerestudiesthataddressed
theuseofspecificorthopedicmethodsor thoserelatedto
surgicaltechniques.Amanualsearchwasperformedinthe
referencesoftheselectedarticlestoidentifyotherpossible
studiestointegrateintothereview.
Dataanalysis
Tworesearchers(GADandRBR)independentlyreviewedthe
titlesandabstractsofallselectedarticlestoassesswhether
the studies would be eligible for inclusion in the review.
Theselectedarticleswerereadinfulltoconfirmeligibility
andtoextractdata.Disagreementswereresolvedby
discus-sionbetweenthetworesearchers.Whennecessary,athird
Table 1 Levels of scientific evidence according to the criteriaproposedbytheAmericanSpeech-Language-Hearing Association.13
Levelof evidence
Typeofscientificstudy
1a Systematicreviewormeta-analysisof randomizedcontrolledtrials
1b High-qualityrandomizedcontrolledtrials 2a Systematicreviewormeta-analysisof
non-randomizedcontrolledtrials
2b High-qualitynon-randomizedcontrolledtrials 3a Systematicreviewofcohortstudies
3b Cohortstudiesorlowqualityrandomized controlledtrials
4 Studiesfromclinicaloutcomes
5a Systematicreviewofacase-controlstudy 5b Case-controlstudies
6 Seriesofcases
7 Specialists’opinionwithoutovertcritical assessment
reviewer (MCAFC) wasconsulted. When abstracts did not
provide sufficient information, the fulltext of thearticle
wasreadfortheassessment.
The following information was extracted from each
study:yearofpublication,firstauthor’sname,typeofstudy,
population,comparedfeedingmethods,numberofsubjects
pergroup,andassessedparameters.
Results
and
discussion
Thesearchstrategyperformedtoselectthestudiesincluded
inthisreviewisshowninFig.1.Theinitialsearchidentified
382articlesaspotentiallyeligible.Afterevaluatingthetitle
and abstract 348 articles were excluded, asthey did not
comparefeedingmethodsforchildrenwithCLP.Fullreading
ofthe34remainingstudieswasperformedandofthese,11
studies were selected tointegrate the systematic review
(seven withlevel ofevidence 1b, threewith3b, and one
level413).
The age range of the studied population was between
0and 18monthsat thestartof thestudies; however,the
follow-up duration was variable. The sample size of the
assessedgroupsrangedfrom18to96subjects/observations
pergroup.
382 potentially relevant references identified
Abstract analysis 348 studies excluded after title or abstract analysis
34 references selected for full-text analysis
Full text analysis
11 studies included in the systematic review
23 excluded after full-text analysis. Reason for exclusion: 11 did not compare methods
5 orthopedic methods 4 other languages 1 inadequate methodology
2 letters to the editor
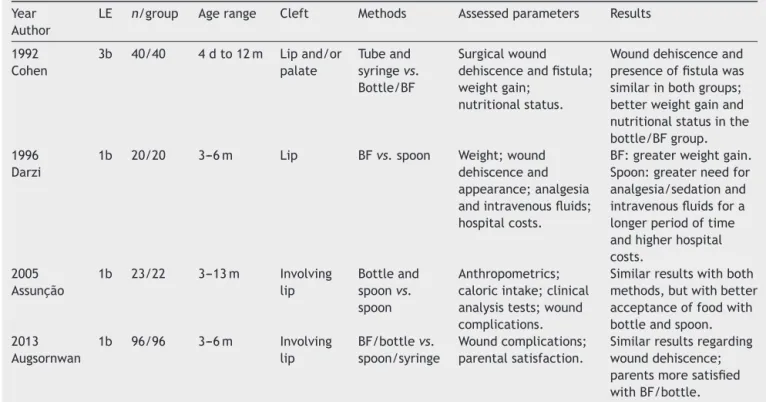
Table2 Characterizationofstudiescomparingfeedingmethodsinthepreoperativeperiodofsurgicalrepair.
Year Author
LE n/group Agerange Clefttype Methods Assessedparameters Results
1999 Shaw
1b 52/49 NB Lipand/or
palate
Rigidbottlevs. squeezable bottle
Weight;length;head circumference.
Squeezablebottle: beneficialeffecton weightgainandhead circumference. 2011
Ize-Iyamu
1b 38/19 0---14w Involving thepalate
Syringevs.cup andspoon
Timeoffeeding; efficiency(presence offoodescapeand/or regurgitation);weight gain.
Syringe:highervolume offoodandshorter feedingtime,lessescape andregurgitationand increaseinweightgain. 2015
Ravi
3b 50/50/50 2---12m Lipand palate
Paladaivs. bottlevs. spoon
Anthropometrics; weightgainpattern.
Meanweightandmean weightgainvelocity: paladai>bottle>spoon; paladai:highernumber ofwell-nourished childrenuntilthepalate repairsurgery;however, aftersurgeryandthe startofcomplementary feeding,thenutritional statusofthethree groupsimproved.
n,numberofsubjectsorobservations;m,months;w,weeks;NB,newborn;LE,AmericanSpeech-Language-HearingAssociationlevelof evidence.13
Thestudiesaddressed16differentsituationsoffeeding
methodsormethodassociations.Themaincharacteristicsof
thefeedingmethodsoftheincludedstudieswere:
alterna-tivefeedingroute---nasogastrictube;feedingmethodsthat
requiredsuction---bottleandBF;feedingmethodswithout
suction ---cup, spoon,syringe,and paladai(a shallowcup
withaspoutpopularlyusedinIndia).
Theparametersevaluatedinthestudieswere:ingested
food acceptance and volume;feeding performance; time
and complications during feeding; growth and nutritional
gain; clinical analysis exams; pain; need for sedation
and/oranalgesia;dehiscence,presenceoffistulaandother
complicationsinthesurgicalwound;hospitallengthofstay
andcosts.
Table 2 depicts the characteristics of twostudies that
comparedfeedingmethodsinthepreoperativeperiodand
onethatintegratedthepre-andpostoperativeperiods.
Regardingtheperiodpriortothesurgicalrepairofcleft
lip and/or palate, two dietary methods were compared:
rigidandsqueezablebottles.Thestudyevaluated
anthropo-metricdata(weight,length,andheadcircumference)and
feedingmethodreliability(assessedbytheneedfor
adjust-ments tothe nipple or change of the feeding methodby
a health professional). The results showedno differences
regardingtheanthropometricvariables,althoughanupward
trendwasobservedinweightgainandheadcircumference
in the group fedwith squeezable bottle,in addition, the
children inthis grouprequired fewernipple modifications
andrequiredlessprofessionalsupportandinterventions.14
Thedifferencebetweentheassistedmethod(squeezable
bottle)andtherigidbottlemaybeassociatedwithhigher
volumeoffoodintakeand/orlowerenergyexpenditureto
extractfood fromthe squeezable bottle,asless effort is
requiredwiththeassistedmethod.However,anotherstudy
evaluatedchildrenwithcleftpalatecomparingfeedingwith
rigidandsqueezablebottles,withorwithouttheuseof
shut-ter,showingnosignificantdifferencesbetweenthemethods
regardingcaloricintakeandgrowth.15
EventhoughBFisverymuchencouraged,especiallyfor
childrenwithCLP,many ofthosewithcleft palatedonot
performwellwhenBFand/orfeedingfromabottlebefore
surgicalrepair. Therefore, Ize-Iyamu etal.compared two
alternativemethods:syringevs.cupandspoon.Thechildren
werefollowedupweeklyaimingtoidentifythefeedingtype
anddifficulties, assessthe feeding, evaluatefeeding
effi-ciencyinrelationtofoodescapeandreflow/regurgitation,
andassessweightgainbetween0and14weeks.
The results showed that the group fed with a syringe
hadlowerfeedingtimeatthe6-weekassessment;100%of
the group of infants fed with a cup and spoon had food
escape and regurgitation compared with 79% escape and
74%ofregurgitationwiththesyringeat6weeks.Moreover,
thosefedacombinationofbreastmilkandformulausinga
syringeshowedasignificantincreaseinweightgainbetween
the 10th and the 14th week. Thus, the authors reported
thatfeedingwithasyringewasapractical,easy-to-perform
method,withgreateradministeredvolume,lesstimespent
withfeeding,andlessfoodescapeandregurgitationaswell
assignificantweightgain.16
An alternative method,although less well known, was
studiedbyRavietal.,whocomparedtheimpactoffeeding
withapaladai,abottle,andaspoonontheweightgain
pat-ternofchildrenaged2monthsto1year.Betterresultswere
Table3 Characterizationofstudiescomparingmethodsoffeedinginthepostoperativeperiodofsurgicalrepairofcleftlip and/orpalate,isolatedliprepair,orlipassociatedornotassociatedwithpalate.
Year Author
LE n/group Agerange Cleft Methods Assessedparameters Results
1992 Cohen
3b 40/40 4dto12m Lipand/or palate
Tubeand syringevs. Bottle/BF
Surgicalwound dehiscenceandfistula; weightgain;
nutritionalstatus.
Wounddehiscenceand presenceoffistulawas similarinbothgroups; betterweightgainand nutritionalstatusinthe bottle/BFgroup. 1996
Darzi
1b 20/20 3---6m Lip BFvs.spoon Weight;wound dehiscenceand appearance;analgesia andintravenousfluids; hospitalcosts.
BF:greaterweightgain. Spoon:greaterneedfor analgesia/sedationand intravenousfluidsfora longerperiodoftime andhigherhospital costs.
2005 Assunc¸ão
1b 23/22 3---13m Involving lip
Bottleand spoonvs. spoon
Anthropometrics; caloricintake;clinical analysistests;wound complications.
Similarresultswithboth methods,butwithbetter acceptanceoffoodwith bottleandspoon. 2013
Augsornwan
1b 96/96 3---6m Involving lip
BF/bottlevs. spoon/syringe
Woundcomplications; parentalsatisfaction.
Similarresultsregarding wounddehiscence; parentsmoresatisfied withBF/bottle.
n,numberofsubjectsorobservations;d,days;m,months;BF,breastfeeding;tube,feedingtube;LE,AmericanSpeech-Language-Hearing Associationlevelofevidence.13
weight, mean weight gain velocity, and number of
well-nourishedchildrenuntilthepalatesurgicalrepair;however,
aftersurgeryandthestartofcomplementaryfeeding,the
nutritionalstatusofthethreegroupsimproved.17
Althoughtheuseofthepaladaiisnotcommonworldwide,
studiesassessinglesswidespreadmethodsareimportant,as
thesedevicesmay,aloneor togetherwithother methods,
facilitate foodintakeand promotelower energy
expendi-tureforsomechildrenwithcleftlipand/orpalate,thereby
contributingtogreaterweightgain.18
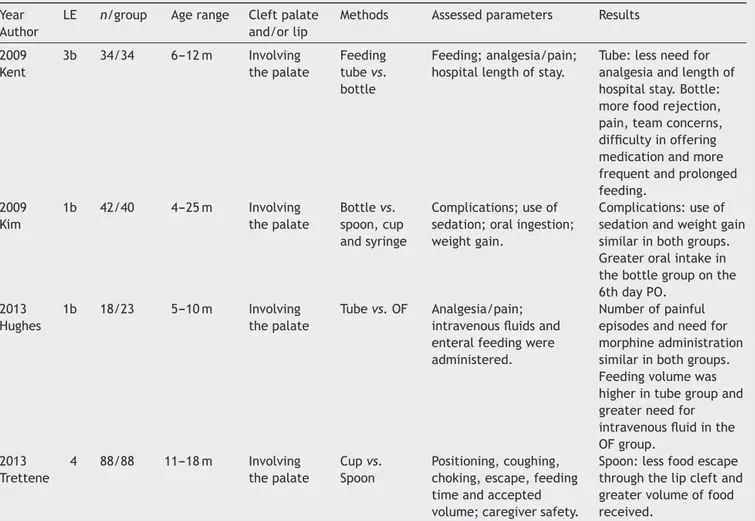
Table3 showsthe characterizationof fourstudiesthat
comparedfeedingmethods inthe postoperativeperiodof
surgicalrepairofcleftlipand/orpalate,isolatedliprepair,
orliprepairassociatedornotassociatedwithpalatoplasty.
The use of methods with suction in the postoperative
periodisacontroversialissue.Therefore,Cohenetal.
com-paredtheuseoffeedingtubeorsyringevs.BForbottleafter
lipand/orpalaterepairsurgery.Thestudyevaluatedwound
dehiscence,presence oforonasalfistula,weightgain,and
nutritionalstatus.Theresultsregardingwounddehiscence
and the presence of fistula were similar in both groups.
However,attheanthropometricandnutritionalassessment,
betterweightgainandnutritionalstatuswasobservedinthe
bottleandBFgroup.19
Nonetheless, this study did not perform statistical
comparisonsofthesevariables,astheywereassessed
sub-jectivelybythegeneralimpressionofobserversandnursing
staff.Duetomethodologicalandethicalissues,suchstudies
areusuallyimpossibletoperformblinded,andobservations
ofthestaffwerepotentiallybiased.
WhencomparingBFwithspoonfeedingregardingweight
and surgical wound appearance and dehiscence after lip
repair,theresultsshowedthatbreastfedchildrenhad
sig-nificantly greater weight gain and slightly shorter length
of hospital stay. Children fed with a spoon were more
irritable,requiredmoreanalgesicdrugsorsedation,andhad
higher hospitalcosts. Additionally, therewasone case of
wounddehiscenceandoneofscarhypertrophyinspoon-fed
group.20
Asimilarstudyassessingbottleandspoonvs.spoon
feed-ingafterliprepairshowedverysimilarresultsbetweenthe
groups; however,therewasgreateracceptanceoffeeding
in thegroupusing thebottleandthe spoon.Also,infants
fedonlywithaspoonshowedirritabilityanddiscomfortdue
totheabruptchange inthetypeoffeeding,whichbefore
surgerywasperformedwiththebottle.21
Whencomparing BF/bottle vs.spoon/syringe regarding
wound dehiscence and parental satisfaction in the
post-operative lip repair surgery, this review observed similar
resultsforwounddehiscence;however,parentsweremore
satisfied andrelaxed when feeding theirchildren through
BF/bottle.22
Thesestudiesshowingfavorableresultsfor thefeeding
methodwithsuctioncorroborateanotherstudythatfound
thatinfantssubmittedtoliprepairsurgeryandfedbybottle
showednoadverseeffectstothesurgery.9Theunfavorable
resultsforthemethodswithoutsuction(spoonandsyringe)
maybeassociatedwithsuckingdeprivationininfants,which
makes them more irritated and, consequently, more
Table4 Characterizationofstudiescomparingfeedingmethodsinthepostoperativeperiodofsurgicalrepairofcleftpalate associatedornotassociatedwithliprepair.
Year Author
LE n/group Agerange Cleftpalate and/orlip
Methods Assessedparameters Results
2009 Kent
3b 34/34 6---12m Involving thepalate
Feeding tubevs. bottle
Feeding;analgesia/pain; hospitallengthofstay.
Tube:lessneedfor analgesiaandlengthof hospitalstay.Bottle: morefoodrejection, pain,teamconcerns, difficultyinoffering medicationandmore frequentandprolonged feeding.
2009 Kim
1b 42/40 4---25m Involving thepalate
Bottlevs. spoon,cup andsyringe
Complications;useof sedation;oralingestion; weightgain.
Complications:useof sedationandweightgain similarinbothgroups. Greateroralintakein thebottlegrouponthe 6thdayPO.
2013 Hughes
1b 18/23 5---10m Involving thepalate
Tubevs.OF Analgesia/pain; intravenousfluidsand enteralfeedingwere administered.
Numberofpainful episodesandneedfor morphineadministration similarinbothgroups. Feedingvolumewas higherintubegroupand greaterneedfor intravenousfluidinthe OFgroup.
2013 Trettene
4 88/88 11---18m Involving thepalate
Cupvs. Spoon
Positioning,coughing, choking,escape,feeding timeandaccepted volume;caregiversafety.
Spoon:lessfoodescape throughthelipcleftand greatervolumeoffood received.
n, numberofsubjects orobservations;m, months;PO, postoperative;tube,feedingtube;OF,oralfeeding;LE,American Speech-Language-HearingAssociationlevelofevidence.13
inadditiontothefactthatlipmovementwhilecryingcould
damagethesurgicalwound.
Suction is essential to infants, because in addition to
beingasourceoffood,itisacomfortingfactor23 and
pro-motes bonding between motherand child, aswell as the
developmentoforalmotorskills.24Therefore,feeding
with-out restrictions after surgical lip repair is becoming the
standard care,25 as it hasshown better results and lower
complicationrates.20---22
However, among the primary surgeries, palate repair
is the most invasive and is associated with greater
dif-ficulty in accepting oral feeding adequately, which can
interfere withthe child’s weightgain.19,26 Additionally, it
is traditionally suggested that the bottle should not be
usedsoon afterpalatoplasty, becauseinappropriate
nega-tive pressureon thesuture line may adversely affect the
results.27
Table 4 summarizes fourstudies that compare feeding
methodsinthepostoperativeperiodofpalaterepairsurgery,
associatedornotassociatedwithliprepair.
Two studies compare an alternative feeding route or
oral/suctionmethod in the first24hours of postoperative
palate repair surgery. The first study assessed feeding,
analgesia,and timeof hospitalstay of infants fed witha
bottleand througha nasogastric tube. The study showed
that those fed through the nasogastric tube were more
stable,requiredlessanalgesia,andweredischargedearlier
fromthehospital.Theparentsoftheseinfantsweremore
relaxed,knowingthattheirchildwasfedandhadadequate
analgesia,whereasthenurses believed theywereable to
providebetterqualityofcare.Conversely,thegroupfedby
bottleshowedhigherfeedingrejection,pain,concernfrom
the care team, difficulty receiving medication, and more
frequentandprolongedfeeding.28
Thesecondstudyevaluatedtheuseofmorphine,number
ofpainfulepisodes,administeredintravenousfluidvolume,
andenteralfeeding.Theresultsshowedthatboththe
num-berofpainfulepisodesandtheuseofmorphineweresimilar
inthefeedingtubegroupandtheoralgroup;however,the
receivedfoodvolumewashigherinfeedingtubegroupand
therewasa greaterneed for intravenous fluidinthe oral
feedinggroup.29
Bothstudies by Kentet al.and Hugheset al.assessed
painparametersbasedontheFace,Legs,Activity,Cry,
Con-solability(FLACC)scoringsystem,measuredbyobservations
surgery.30 One of the possible limitations of both studies
wasthelackofblinding.Tocorrectthis,theuseof
alterna-tivefeedingrouteswouldberequiredforallthechildren,
tomaintaintheevaluatorsblindedtothefeedingmethod;
however,thefeedingtubemaydamagethepalaterepairand
causepainandthiscouldbeonemoreconfoundingfactor
totheresults.29
Ontheotherhand,differentresultswereobtainedwhen
comparing infants fed with a bottle vs. those fed with
a spoon, cup and syringe for six days post-palatoplasty.
The parameters analyzed were: complications (bleeding,
breathing problems, wound dehiscence, and oronasal
fis-tula),frequency of sedation use, oral intake, and weight
gain. The rate of overall complications, use of sedation,
andweightgainwere similarinboth groups; however, on
the sixth post-operative day, oral intake was greater in
the bottlegroup. According tothe authors, these results
suggestthatthebottlecanbeintroducedduringthe
imme-diatepostoperativeperiod,asthefeedingmethoddidnot
affecttheimmediatepostoperativecourseofpalaterepair
surgery.31
TheresultsofthestudybyKimetal.regardingthe
sur-gicalprocedurearedifferentfromthestudiesofKentetal.
and Hughes et al. This might have occurred because the
studybyKimetal.hadarelativelyhomogeneoussampleof
patientsregardingtheextentofthecleft,usedastandard
technique for the closing of the palate, and the surgery
wasperformedbyasinglesurgeon.Forexample,the
occur-renceoffistulasseemstoberelatedtocleftseverity32,33and
rarelywiththetechniqueemployedforthepalateclosure.32
Additionally, thestudies by Kent et al.and Hughes etal.
evaluatedonly the first 24hours, while the study by Kim
etal.followsthefirstsixpostoperativedays.Therefore,it
canbeassumedthattube feedingwouldbeamore
effec-tivemethodduringthefirsthoursandthebottlecouldbe
includedinthedietonthefollowingdays.
Another important factor to be addressed is that
dif-ferent protocols are used in different hospitals, as some
institutionsprohibittheuseofbottlesandnipplesfora
cer-tainperiodafterpalaterepairsurgery.Therefore,thestudy
byTretteneetal.comparesfeedingwithacupandaspoon
intheimmediatepostoperativeperiodofpalatoplasty.This
studyassessed44binomials bycaregiversfor four
consec-utivetimes,intercalatingthefeedingmethod.Positioning,
coughing,choking,foodescapethroughthelipcommissure,
feedingtime,acceptedvolume,andsafetyreportedbythe
caregiverwereanalyzed.
Theresultsdemonstratethatthetechniquethatusesthe
spoonshowedlessfoodescapethroughthelipcommissure,
higherfoodvolumeacceptance,andchildrensubmittedto
full palatoplasty had less frequent cough episodesduring
feeding.10Anotherpositivefactorregardingtheuseofthe
spoonisthehigherdegreeoforalstimulationandthe
pro-motionofmusclecontractionandnerveendingstimulation
whencomparedtothecup.34,35
Although there are studies comparing similar feeding
methods,itwasnotpossibletoperformameta-analysisof
theresultsshowninthissystematicreview.Studies
demon-strated verydifferent methodologiesand,above all,very
heterogeneousparameterswereevaluated,whichprevents
theequivalenceofstudies,afundamentalcharacteristicfor
theviabilityofthemeta-analysis.
Conclusion
Feedingthroughmethodswithsuctionispossibleand
appro-priate for children with CLP before the surgical repair,
particularlythosewithisolatedpre-foramenclefts,asthey
arethecaseswiththegreatestchancesofsuccess.However,
accordingtotheresultsofthestudies,theuseof
alterna-tivemethodssuchassqueezablebottle,syringe,andpaladai
maybebeneficialincertaincases.
Inthe postoperativeperiodof lip repair surgery,
feed-ing methodswithsuction seem tobemore beneficialand
do not show major complications after surgery. However,
regardingthepostoperativeperiodofpalaterepairsurgery,
therearedivergencesonthemostsuitablefeedingmethod,
rangingfromtotalinterruptionoforalfeedingforat least
24hours,suctionmethoddeprivation,andfeedingmethod
with unrestricted suction. More studies on feeding
meth-ods,particularlyinthepostoperativeperiodofpalaterepair
surgery,arerequired.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Jesus MSV,PenidoFA, Valente P.Avaliac¸õesfonoaudiológicas clínicaeinstrumentalemindivíduoscomfissuralabiopalatina. In:JesusM,DiNinnoC,editors.Fissuralabiopalatina.SãoPaulo: Roca;2009.p.57---75.
2.CardimVL.Crescimentocraniofacial.In:AltmannE,editor. Fis-suraslabiopalatinas.Barueri:Pró-Fono;2005.p.31---8. 3.MarquesRMF,LopesLD,KhouryRBF.Embriologia.In:Altmann
E,editor.Fissuraslabiopalatinas. Barueri:Pró-Fono;2005. p. 3---23.
4.ArarunaRdC,VendruscoloDM.Nutritionofchildrenwithcleftlip andcleftpalate,abibliographicstudy.RevLatAmEnfermagem. 2000;8:99---105.
5.Amstalden-MendesLG,MagnaLA,Gil-da-Silva-LopesVL. Neona-tal care of infants with cleft lip and/or palate: feeding orientationand evolutionofweight gain ina nonspecialized Brazilianhospital.CleftPalateCraniofacJ.2007;44:329---34. 6.BertierCE,TrindadeIEK,SilvaFilhoOG.Cirurgiasprimáriasde
lábioepalato.In:TrindadeIEK,SilvaFilhoOG,editors.Fissuras labiopalatinas:umaabordageminterdisciplinar.SãoPaulo: San-tos;2007.p.73---85.
7.MartinsDMFS.Fissuraslabiaisepalatinas.In:FerreiraLM, edi-tor.Manualdecirurgiaplástica.SãoPaulo:Atheneu;1995.p. 165---73.
8.WyszynskiDF.Cleftlipand palate:fromorigin totreatment. NewYork:OxfordUniversityPress;2002.
9.SkinnerJ,ArvedsonJC,JonesG,SpinnerC,RockwoodJ. Post-operative feeding strategiesfor infants withcleft lip. Int J PediatrOtorhinolaryngol.1997;42:169---78.
10.TretteneAdosS,MondiniCC,MarquesIL.Feedingchildrenin theimmediateperioperativeperiodafterpalatoplasty:a com-parisonbetweentechniquesusingacupandaspoon.RevEsc EnfermUSP.2013;47:1298---304.
12.StroupDF,BerlinJA,MortonSC,OlkinI,WilliamsonGD,Rennie D,etal.Meta-analysisofobservationalstudiesinepidemiology: aproposalforreporting.Meta-analysisofObservationalStudies inEpidemiology(MOOSE)group.JAMA.2000;283:2008---12. 13.MullenR.Thestateoftheevidence:ASHAdevelopslevelsof
evi-denceforcommunicationsciencesanddisorders.March2007. [cited15Sept2015].Availablefrom:http://www.asha.org. 14.ShawWC,BannisterRP,Roberts CT.Assistedfeeding ismore
reliableforinfantswithclefts---arandomizedtrial.CleftPalate CraniofacJ.1999;36:262---8.
15.Brine EA, Rickard KA, Brady MS, Liechty EA, Manatunga A, Sadove M, et al. Effectiveness of two feeding methods in improvingenergyintakeandgrowthofinfantswithcleftpalate: arandomizedstudy.JAmDietAssoc.1994;94:732---8. 16.Ize-IyamuIN,SaheebBD.Feedinginterventionincleftlipand
palatebabies:apracticalapproachtofeedingefficiencyand weightgain.IntJOralMaxillofacSurg.2011;40:916---9. 17.RaviBK,PadmasaniLN,HemamaliniAJ,MurthyJ.Weightgain
patternofinfantswithorofacialcleftonthreetypesoffeeding techniques.IndianJPediatr.2015;82:581---5.
18.DiNinnoCQMS, MouraD,Raciff R, MachadoSV, RochaCMG, Norton RC, et al. Aleitamentomaterno exclusivo em bebês com fissura de lábio e/ou palato. Rev Soc Bras Fonoaudiol. 2011;16:417---21.
19.CohenM, MarschallMA, SchaferME. Immediate unrestricted feedingofinfantsfollowingcleftlipandpalaterepair.J Cran-iofacSurg.1992;3:30---2.
20.DarziMA,ChowdriNA,BhatAN.Breastfeedingorspoonfeeding aftercleftliprepair:aprospective,randomisedstudy.BrJPlast Surg.1996;49:24---6.
21.Assuncao AG, Pinto MA, Peres SP, Tristao MT. Immediate postoperative evaluation of the surgical wound and nutri-tionalevolution after cheiloplasty. Cleft Palate CraniofacJ. 2005;42:434---8.
22.AugsornwanD,SurakunpraphaP,PattangtanangP,Pongpagatip S,JenwitheesukK,ChowchuenB.Comparisonofwound dehis-cenceandparent’ssatisfactionbetweenspoon/syringefeeding andbreast/bottlefeedinginpatientswithcleftliprepair.JMed AssocThai.2013;96Suppl.4:S61---70.
23.InternationalLLL.Breastfeedingababywithcleftliporcleft palate.In:InternationalLLL,editor.Schaumburg,IL,2004. 24.KummerAW.Cleftpalateandcraniofacialanomalies:effectson
speechandresonance.NewYork:CengageLearning;2008. 25.NoordhoffMS,ChenPK.Unilateralcheiloplasty.In:MathesSJ,
editor.Plasticsurgery,vol.4.Philadelphia,PA:Saunders;2006. p.165.
26.MartinV.Atendimentodeenfermagempréepós-operatório.In: WatsonACH,SellDA,GrunwellP,editors.Tratamentodefissura labialefendapalatina.SãoPaulo:Santos;2005.p.184---90. 27.RandallP,LaRossaD.Cleftpalate.In:McCarthyJG,editor.
Plas-ticsurgery,vol.4.Philadelphia,PA:Saunders;1990.p.2723. 28.Kent R, Martin V. Nasogastric feeding for infants who have
undergone palatoplasty for a cleft palate. Paediatr Nurs. 2009;21:24---9.
29.Hughes J, LindupM, Wright S, Naik M, Dhesi R, Howard R, etal.Doesnasogastricfeedingreducedistressaftercleftpalate repairininfants?NursChildYoungPeople.2013;25:26---30. 30.MerkelS,Voepel-LewisT,MalviyaS.Painassessmentininfants
and young children: the FLACCscale. AmJ Nurs. 2002;102: 55---8.
31.KimEK,LeeTJ,ChaeSW.Effectofunrestrictedbottle-feeding onearlypostoperativecourseaftercleftpalaterepair.J Cran-iofacSurg.2009;20Suppl.2:1886---8.
32.Cohen SR, Kalinowski J, LaRossa D, Randall P. Cleft palate fistulas:a multivariatestatisticalanalysisofprevalence, eti-ology,andsurgicalmanagement.PlastReconstrSurg.1991;87: 1041---7.
33.Phua YS, de Chalain T. Incidence of oronasal fistulae and velopharyngealinsufficiencyaftercleftpalaterepair:anaudit of211childrenbornbetween1990and2004.CleftPalate Cran-iofacJ.2008;45:172---8.
34.AltmannEBC,Vaz ACN, PaulaMBSF,Khoury RBF.Tratamento Precoce.In:AltmannE,editor.Fissuraslábiopalatinas.4thed. Carapicuiba:Pró-Fono;1997.p.291---324.