Surgical approach of hypertelorbitism in craniofrontonasal
dysplasia
Abordagem cirúrgica do hiperteleorbitismo na displasia craniofrontonasal
Rafael DenaDai, asCBC-sP1; Wellington Matheus RoBeRto1; Celso luiz Buzzo1; enRiCo ghizoni1; CésaR augusto RaPoso-aMaRal1;
Cassio eDuaRDo RaPoso-aMaRal1.
INTRODUCTION
T
he principles of craniofacial surgery established by the French plastic surgeon Dr. Paul Louis Tessier in the 1960s are among the most relevant milestones of medicine in the 20th century1. Among Tessier’sremarkable contributions, the art of moving the orbits deserves special attention1,2. In his seminal articles,
Tessier3-6 presented the surgical principles for the
treatment of orbital hypertelorism (hyperteleorbitism) and demonstrated that it was possible to approach the cranial, nasal and oral cavities in the same surgical intervention, while the orbits and their contents simultaneously moving in all directions.
Hyperteleorbitism is characterized by true lateralization of the entire orbital complex (medial and lateral walls) and is a clinical finding of numerous craniofacial anomalies7, especially craniofrontonasal
dysplasia, also called craniofrontonasal syndrome (OMIM # 304110), identified in 1979 by Cohen8 as a
subgroup of frontonasal dysplasias (OMIM # 136760). Craniofrontonasal dysplasia is a rare X-linked syndrome, associated with mutations in the EFNB1 gene, which provides instructions for the production of ephrin-B1, a protein important for the normal development of the
frontonasal neural crest that originates the face and skull. It displays hyperteleorbitism, often asymmetric, unilateral or bilateral coronal craniosynostosis, among other craniofacial and extracranial deformities. Although its genetics and phenotypes have been addressed in numerous studies8-11, guidelines on the specific treatment
of hyperteleorbitism are scarce and have been reported almost exclusively in the international context12-17.
In previous works, our group18,19 studied the
recurrence of the orbital position after the correction of hyperteleorbitism in different craniofacial deformities. However, to the best of our knowledge, there are no national studies on the intracranial and extracranial surgical approach for the treatment of hyperteleorbitism specifically in patients with craniofrontonasal dysplasia. Therefore, the objective of the present study was to present our experience in the surgical treatment of hyperteleorbitism in craniofrontonasal dysplasia.
METHODS
This is a retrospective, observational study of patients with craniofrontonasal dysplasia surgically treated at the Institute of Craniofacial Plastic Surgery
1 - SOBRAPAR Hospital, Institute of Craniofacial Plastic Surgery, Campinas, SP, Brazil.
A B S T R A C T
Objective: to present our experience in the hypertelorbitism surgical treatment in craniofrontonasal dysplasia. Methods: retrospective analysis of craniofrontonasal dysplasia patients operated through orbital box osteotomy or facial bipartition between 1997 and 2015. Surgical data was obtained from medical records, complementary tests, photographs, and clinical interviews. Surgical results were classi-fied based on the need for additional surgery and orbital relapse was calculated. Results: seven female patients were included, of whom three (42.86%) underwent orbital box osteotomy and four (57.14%) underwent facial bipartition. There was orbital relapse in average of 3.71±3,73mm. Surgical result according to the need for further surgery was 2.43±0.53. Conclusion: surgical approach to hypertelorbitism in craniofrontonasal dysplasia should be individualized, respecting the age at surgery and preferences of patients, parents, and surgeons.
of the SOBRAPAR Hospital between 1997 and 2015. The study was approved by the Ethics in Research Committee of the SOBRAPAR Hospital (002/16) and is in agreement with The Helsinki Declaration of 1975, perfected in 1983.
We included only patients with diagnostic confirmation of craniofrontonasal dysplasia10,11,17
submitted to craniofacial surgical interventions by the same group of plastic surgeons and with adequate postoperative follow-up. We excluded patients with uncertain diagnosis and/or submitted to major craniofacial surgeries in other services. We obtained demographic and clinical data and information related to surgical interventions through reviews of medical records, photographs, frontal cephalograms, and clinical interviews.
Surgical approach
We submitted all patients to facial bipartition or to orbital box osteotomy under general anesthesia with the objective of correcting the hyperteleorbitism. In general, we employed facial bipartition in patients with immature craniofacial skeleton, and orbital box osteotomy, in adults with adequate occlusion. Decisions among surgical approaches were based on the age of the patients, whether or not they had complete dentition, the occlusion aspect and the preferences of patients (or parents) and plastic surgeons.
Orbital box osteotomy
We used intra and extracranial approaches to make quadrangular orbital osteotomies. We applied a Coronal and gingivobucal sulcus incision to obtain the subperiosteal exposure of the frontal bones, orbits and the middle third of the face. Next, we performed a frontal craniotomy, followed by circumferential orbital osteotomies, taking care to preserve the tendons of the medial cantus. We also osteotomized the zygomatic-maxillary and naso-zygomatic-maxillary pilars. The planned osteotomy of the medial fronto-ethmoidal segment was marked and performed with a reciprocating saw following adequate intracranial midline dissection and frontal lobe retraction. After removal of the median segment, we translocated the orbits medially. We then fixed the nasophrontal processes of the
maxilla with steel wires, and the vertical pillars, with titanium plates and screws. Before closure, we raised a pericranial flap and advanced it till the base of the skull on the midline19.
Facial bipartition
For facial bipartition, in addition to the osteotomies described for the orbital box osteotomy, we performed osteotomies of the pterygomaxillary, septal and palatal regions to allow full mobilization of the middle third of the face. After the osteotomies, was proceeded to the craniofacial disjunction with the Rowe de-impacting forceps. In the sequence, was performed a inverted “V” osteotomy in the medial region towards the galli crest, being careful not to to damage the olfactory nerves next to the cribriform plate. This osteotomy was symmetric, for patients with bilateral fusion of the coronal suture, or asymmetric, for individuals with unilateral fusion. We removed the frontal bone, ethmoid bone and nasal septum via intracranial access. Subsequently, we rotated the segments of the hemifaces medially. We then fixed the nasofrontal processes and the lateral portions of the hemifaces to the zygomatic processes with steel wires. We fixed the inferomedial portions of the hemifaces to each other with plates and screws. We placed Autologous bone grafts form the skull cap on the lateral portions of the orbital edges and on the zygomatic arches that were medialized and eventually advanced19.
Complementary surgical procedures
In both techniques, we used different types of locoregional flaps for simultaneous correction of soft tissue deformities. We reconstructed the nose, lips and eyelids as needed. We treated the excess medial skin with Kawamoto (“K”) sub-dermal points or resection of the excess frontal skin. All patients underwent transnasal medial cantopexy.
Bone measurements
preparation of the present study). In the recent and late preoperative and postoperative periods, we performed bone measurements on frontal cephalograms12,18,19.
In the intraoperative period, we measured the IOD with a pachymeter, before and after the inverted “V” osteotomy12,18,19. We classified all patients according
to the IOD measured intraoperatively6: first degree
(mild), IOD > 30 mm and ≤ 34mm; Second degree (moderate), IOD>34mm and ≤40mm; and third degree (severe), IOD>40mm.
Evaluation of surgical results
We used the measurements of the recent and late postoperative periods together to define
the recurrence of the orbital position after surgery. We defined orbital recurrence as the difference between the measurements of the internal IOD at the postoperative periods19. We graded all results
of large craniofacial surgical interventions (facial bipartition and orbital box osteotomy) according to the classification system on the need for additional surgery described by Whitaker20: category I, does not
require surgical revision; category II, requires minor surgical revisions of the craniofacial contour; Category III, requires extensive additional osteotomies (surgical intervention less than the initial/main surgery); and category IV, requires a complete new craniofacial surgical intervention, similar to the initial/main surgery.
Statistical analyzes
We compiled all information in Excel for Windows (Microsoft Corporation, USA). We used the mean for metric variables and the percentages for categorical variables. We carried out the intragroup and intergroup comparative analyzes (IOD and Whitaker classification) with the Mann-Whitney test and test of equality between two proportions. We performed all analyzes with the Statistical Package for Social Sciences version 20 for Windows (SPSS, Chicago, IL, USA). We considered as significant the values for a 95% confidence interval (p<0.05).
RESULTS
We included seven female patients diagnosed with craniofrontonasal dysplasia. The mean patients’ age at the time of the craniofacial interventions was 11.86 ± 8.05 years (4-29), being 14.67 ± 12.90 years (4-29) And 10 ± 2 years (7-12) for orbital box osteotomy and facial bipartition procedures, respectively. Three (42.86%) and four (57.14%) patients were classified with mild and moderate hyperteleorbitism, respectively.
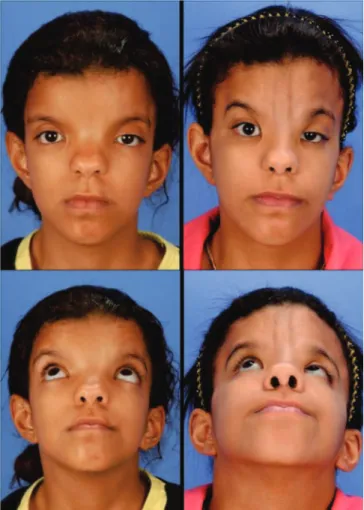
Three (42.86%) patients underwent orbital box osteotomy and four (57.14%) underwent facial bipartition (Figures 1 and 2). Patients received a mean of 3.33 ± 2.07 units (1-6) of packed red blood cells during surgery and remained hospitalized for an average of 7.71 ± 3.86 days (6-16). There were two (28.57%) complications related to procedures, infections of
surgical sites treated with intravenous antibiotic therapy. There were no deaths or complications such as visual deficit or permanent neurological damage.
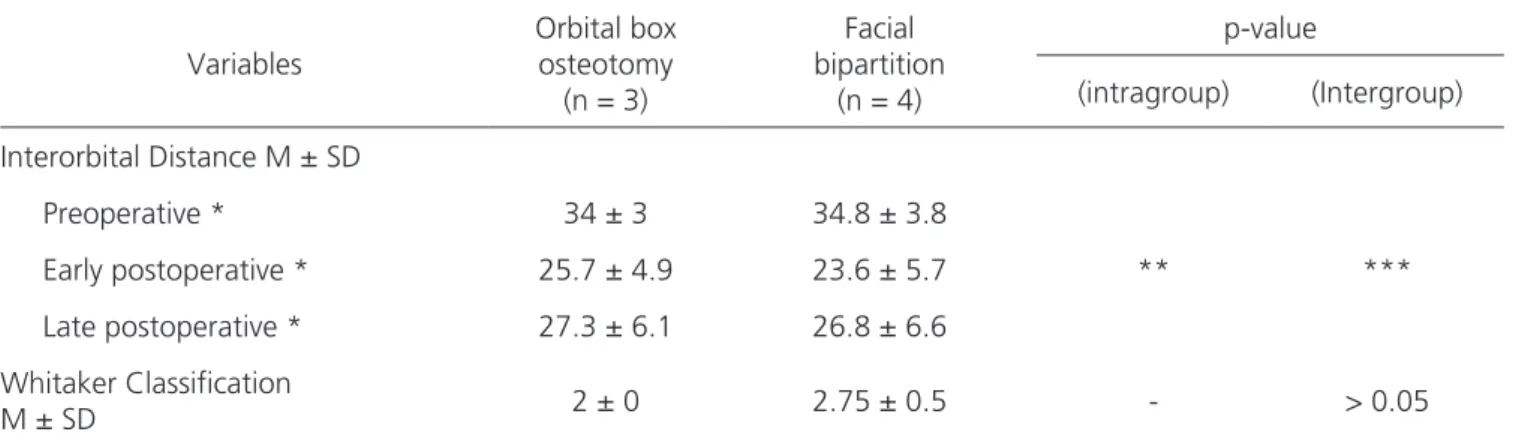
Before the interventions, the mean IOD was 34.43 ± 3.21 mm (30-39) as measured with the cephalograms, and 35.43 ± 2.7 mm (31-39) when measured intraoperatively with the pachymeter, just before the osteotomies. The mean reduction in IOD in the recent postoperative period was 11.14 ± 4.53 mm, corresponding to a reduction of 31.58 ± 13.14% (19.44-51.61). The mean reduction in IOD in the late postoperative period was 8.43 ± 6.80 mm, which corresponds to a reduction of 23.29 ± 17.99% (5.56-43.59) of the IOD initial mean. The mean orbital recurrence was 3.71 ± 3.73 mm (0-10) (Table 1).
The overall mean of the surgical results classified according to the Whitaker need for surgical revision20 was 2.43 ± 0.53 (between categories II and III)
(Table 1). Four (57.14%) and three (42.86%) patients were classified as categories II and III, respectively. All patients have had normal intellectual development and are still in follow up on our service.
DISCUSSION
The correction of hyperteleorbitism has been a challenge for plastic surgeons dealing with craniofrontonasal dysplasia17, since such patients often
have severe and asymmetric hyperteleorbitism17,21,
therefore requiring a great mobilization of the orbits in three dimensions18. Since the first description of
craniofrontonasal dysplasia8, the surgical treatment
of hyperteleorbitism in these patients has been restricted only to reports of isolated cases and to retrospective series in the international context12-17.
Although there are national publications18,19,22,23 that
address the surgical correction of hyperteleorbitism of several craniofacial deformities together, this is the first Brazilian study that brings the peculiarities of the intracranial and extracranial interventions performed for the treatment of hyperteleorbitism in patients with craniofrontonasal dysplasia .
In the literature, after Tessier3-6 described
the surgical principles of the intra and extracranial approach for the correction of hyperteleorbitism,
many adaptations and technical innovations have been published, especially those described by Van der Muelen24,25, who modified the box osteomy and
created the facial bipartition. The latter comprises the medial rotation of the two hemifaces by means of the intracranial access, associated with successive osteotomies at the pterygomaxillary junction and palatine plates, simultaneously correcting the orbits and the inverted “V” occlusion reported in patients with hyperteleorbitism. In addition, Converse et al.26,27
described the one-stage orbitotomy for the correction of hyperteleorbitism in adult patients, avoiding osteotomies in the palate.
Although there are national reports on the treatment of hyperteleorbitism by extracranial osteotomies22,23, the procedures of choice have been
the orbital box osteotomy and facial bipartition17-19,21,
as both techniques allow the three-dimensional mobilization of the target structures and, therefore, the approach of a broad spectrum of clinical presentation of hyperteleorbitism. In the particular scope of craniofrontonasal dysplasia, Kawamoto et al.17 considered
that facial bipartition enabled a better correction of craniofacial deformity when compared with orbital box osteotomy. It has also been argued that facial bipartition is simpler to perform and does not require osteotomies in the interorbital region that may compromise dental buds and lacrimal pathways15,17. It is important that
these aspects15,17 be considered; However, significant
rotation of the hemifaces during facial bipartition in adult patients with severe hyperteleorbitism produces a diastema of the central maxillary incisors which may be very difficult to correct orthodontically and potentially require a LeFort I osteotomy19. Moreover, in these
patients, dental buds are at potential risk during the rigid fixation of the osteotomy segments in the nasomaxillary and zygomaticomaxillary pillars19. Based on this, we
prefer the orbital box osteotomy for the correction of hyperteleorbitism in adult patients with normal maxillary morphology and acceptable occlusion, while reserving facial bipartition to treat patients with mixed or deciduous dentition19. With this surgical approach, we obtained
a significant improvement in the craniofacial symmetry of all patients evaluated, there being need of additional surgeries of the craniofacial contour (categories II and III of Whitaker20).
The coronal suture fusion pattern (unilateral versus bilateral) determines the clinical characteristics of patients with craniofrontonasal dysplasia10,11,17. In
addition to hyperteleorbitism, patients with unilateral fusion of the coronal suture also present vertical orbital dystopia, so that the orbit ipsilateral to the fusion is displaced cranially compared with the contralateral orbit10,11,17. Therefore, in these situations, the inverted
“V” resection should be asymmetrical, the “leg” of the “V” ipsilateral to the coronal suture fusion being vertically planned, and the contralateral leg, horizontally. Total (bilateral) fusions of the coronal suture lead to a facial pattern with greater symmetry, although brachycephalic10,11,17, so that the inverted “V”
resection can be symmetrical. One can apply this same reasoning to the frontal bone. Patients with unilateral coronal fusion present an asymmetric frontal region (the frontal bone ipsilateral to the fusion is laterally located on the contralateral side, which usually presents with a bone hump or bulging). Thus, we perform the inversion of the bone plate in these situations, so that the bone hump is rotated 180 degrees to be fixed in the depressed frontal region. Such a surgical maneuver allows obtaining of facial symmetry. However, this maneuver is unnecessary in those patients with bilateral fusion of the coronal suture.
Another relevant aspect in the surgical treatment of hyperteleorbitism in craniofrontonasal dysplasia is the manipulation of soft tissues17. The
medialization of the orbits determines a tissue excess
Table 1. Intra and intergroup (orbital box osteotomy versus facial bipartition) comparative analyses.
Variables
Orbital box osteotomy
(n = 3)
Facial bipartition
(n = 4)
p-value
(intragroup) (Intergroup)
Interorbital Distance M ± SD
Preoperative * 34 ± 3 34.8 ± 3.8
** ***
Early postoperative * 25.7 ± 4.9 23.6 ± 5.7 Late postoperative * 27.3 ± 6.1 26.8 ± 6.6 Whitaker Classification
M ± SD 2 ± 0 2.75 ± 0.5 - > 0.05
in the median region, which can be resected in the form of “Z”, obeying the principles of Tessier6, by
means of direct resection without the Z-plasty, or by using the “K” stitches17,28. The “K” stitches are
named after their creator, Dr. Henry K. Kawamoto, who described the technique to reduce the excess of soft tissues without the need for scars on the frontal region17,28. The technique consists in decreasing the
thickness of all planes from the forehead to the dermis, but without incision in the epidermis17,28. This surgical
maneuver, eventually followed by mattress suturing, leads to soft tissue contraction without the need for direct excision, as recommended by the authors17,28.
Another important clinical feature is poor positioning of the medial corner, which determines a small skin fold characteristic of craniofrontonasal dysplasia and more easily identified in patients who present unilateral fusion of the coronal suture compared with those with bilateral one. The treatment of this particular deformity is fundamental, since it alleviates the stigma of craniofrontonasal dysplasia. The surgical approach can be performed by means of Z-plasty or by the technique described by Fuente del Campo29, which has been routinely used by the UCLA
Craniofacial Clinic group17.
The literature has reported that self-perception of a deformed face may be present in children less than four years of age15. Such children
begin to feel different from their peers and lose the motivation to attend environments with other children18. As orbital repositioning improves overall
facial harmony and allows the acquisition of binocular vision (usually impaired due to hyperteleorbitism)18, and
early surgery has the potential to attenuate the stigmas and stereotypes faced by children with craniofacial deformities mainly in the school environment18,
many parents seek specialized centers to resolve the anxiety related to the appearance of their children18,19.
However, it is important to mention that surgical intervention for the correction of hyperteleorbitism may display recurrence of orbital position and also compromise facial growth, especially when performed in children with an immature craniofacial skeleton19,21.
In the literature, analyzes of the 1980s and 1990s12, 30 presented mixed results regarding the
relationship between the patients’ age and the orbit position recurrence rate. Two recent longitudinal studies19,21 have evaluated numerous patients
with hyperteleorbitism (including patients with craniofrontonasal dysplasia) treated surgically and have shown that age is a determining factor in the rate of orbital position recurrence. In addition, the surgical technique (orbital box osteotomy versus facial bipartition) was not determinant in the rate of recurrence19 and
there is a divergence regarding the effect of the severity of hyperteleorbitism on recurrence19,21.
There is evidence that facial growth reaches 90% of the adult size before the age of sixteen31 and
that the permanent upper incisors present eruption typically before the age of eight19. Thus, since the
presence of permanent dentition may contribute to greater bone stability in the postoperative period and this is an important factor for the choice of surgical technique, we have adopted eight years as the age limit to differentiate patients who have higher or lower potential for continuous growth of the middle third of the face and patients whose state of dentition is less or more mature19. By applying this concept, in
this study we found rates of orbital recurrence similar to the ones reported in previous studies18,19,21.
In this context, while waiting for skeletal maturity to operate hyperteleorbitism is associated with lower relapse rates19, other aspects can often
determine that interventions be performed in younger patients19,21. In fact, multiple factors contribute to
the decision on when surgical correction should be performed19,21. Among the most relevant are
the emotional and psychological responses of both parents and children with hyperteleorbitism19. The
physical appearance of these children can be shocking, and parents are often anxious to have the surgery performed as early as possible, or before their children reach school age, to try to mitigate the challenges that children may face as they become self-critical and begin to have contact with their peers19,21.
(intervention age versus outcomes versus potential risks in the short and long terms). If even with this multidisciplinary support the child and parents demonstrate the desire for surgery, it cannot be denied that, in this particular situation, the possibility of recurrence is certainly no more relevant than the desire for positive image and recovery of
self-esteem, that allow the confrontation of prejudice derived from peers18,19.
According to the presented and discussed surgical results, the approach of these patients should be individualized, respecting, whenever possible, the age and preferences of patients and their parents, as well as the experience of surgeons.
REFERENCES
1. Hallock GG. The plastic surgeon of the 20th centu-ry. Plast Reconstr Surg. 2001;107(4):1014-24. 2. Monasterio FO. The art of moving the orbits. Plast
Reconstr Surg. 2007;119(1):316-22.
3. Tessier P, Guiot G, Rougerie J, Delbet JP, Pastor-iza P. Hypertelorism: cranio-naso-orbito-facial and subethmoid osteotomy. Panminerva Med. 1969;11(3):102-16.
4. Tessier P. Orbital hypertelorism. I. Successive sur-gical attempts. Material and methods. Causes and mechanisms. Scand J Plast Reconstr Surg. 1972;6(2):135-55.
5. Tessier P, Guiot G, Derome P. Orbital hypertelorism. II. Definite treatment of orbital hypertelorism (OR.H.) by craniofacial or by extracranial osteoto-mies. Scand J Plast Reconstr Surg. 1973;7(1):39-58. 6. Tessier P. Experiences in the treatment of orbital
hypertelorism. Plast Reconstr Surg. 1974;53(1):1-18.
7. Cohen MM Jr, Richieri-Costa A, Guion-Almeida ML, Saavedra D. Hypertelorism: interorbital growth, measurements, and pathogenetic considerations. Int J Oral Maxillofac Surg. 1995;24(6):387-95. 8. Cohen MM Jr. Craniofrontonasal dysplasia. Birth
Defects Orig Artic Ser. 1979;15(5B):85-9.
9. Forrest CR, Hopper RA. Craniofacial syn-dromes and surgery. Plast Reconstr Surg. 2013;131(1):86e-109e.
10. van den Elzen ME, Twigg SR, Goos JA, Hooge-boom AJ, van den Ouweland AM, et al. Pheno-types of craniofrontonasal syndrome in patients with a pathogenic mutation in EFNB1. Eur J Hum Genet. 2014;22(8):995-1001.
11. Tan ST, Mulliken JB. Hypertelorism: nosolog-ic analysis of 90 patients. Plast Reconstr Surg. 1997;99(2):317-27.
12. McCarthy JG, La Trenta GS, Breitbart AS, Zide BM, Cutting CB. Hypertelorism correction in the young child. Plast Reconstr Surg. 1990;86(2):214-25; discussion 226-8.
13. Suzuki H, Nara T, Minato S, Kamiishi H. Experi-ence of surgical treatment for craniofrontonasal dysplasia. Tohoku J Exp Med. 1991;164(4):251-7. 14. Wolfswinkel EM, Weathers WM, Correa B, Bu-chanan EP, Hollier LH Jr. Craniofrontonasal dys-plasia: variability of the frontonasal suture and implications for treatment. J Craniofac Surg. 2013;24(4):1303-6.
15. Orr DJ, Slaney S, Ashworth GJ, Poole MD. Craniofrontonasal dysplasia. Br J Plast Surg. 1997;50(3):153-61.
16. Moreira Gonzalez A, Elahi M, Barakat K, Yavuzer
Objetivo: apresentar nossa experiência no tratamento cirúrgico do hiperteleorbitismo na displasia craniofrontonasal. Métodos: análise retrospectiva dos pacientes com displasia craniofrontonasal operados por orbital box osteotomy ou por bipartição facial entre os anos de 1997 e 2015. Informações sobre as intervenções cirúrgicas foram obtidas dos prontuários médicos, exames complementares, fotografias e entrevistas clínicas. Os resultados cirúrgicos foram classificados com base na necessidade de cirurgia adicional, e a recidiva orbital foi calcu-lada. Resultados: sete pacientes do sexo feminino foram incluídas, três submetidas à orbitalbox osteotomy (42,86%) e quatro (57,14%) à bipartição facial. Houve uma recidiva orbital média de 3,71±3,73mm. A média global dos resultados cirúrgicos de acordo com a necessi-dade de novas cirurgias foi de 2,43±0,53. Conclusão: a abordagem cirúrgica do hiperteleorbitismo na displasia craniofrontonasal deve ser individualizada, respeitando, sempre que possível, a idade e as preferências dos pacientes, seus familiares e cirurgiões.
Descritores: Anormalidades Craniofaciais. Cirurgia Plástica. Olho. Osteotomia.
R, Brinkmann B, Jackson IT. Hypertelorism: the importance of three-dimensional imaging and trends in the surgical correction by facial biparti-tion. Plast Reconstr Surg. 2005;115(6):1537-46. 17. Kawamoto HK, Heller JB, Heller MM, Urrego A,
Gabbay JS, Wasson KL, et al. Craniofrontonasal dysplasia: a surgical treatment algorithm. Plast Reconstr Surg. 2007;120(7):1943-56.
18. Raposo-Amaral CE, Raposo-Amaral CA, Bradley JP, Guidi MC, Buzzo CL. Estudo da recidiva após a correção do hiperteleorbitismo. Rev Bras Cir Plast. 2009;24(4):425-31.
19. Raposo-Amaral CE, Raposo-Amaral CM, Rapo-so-Amaral CA, Chahal H, Bradley JP, Jarrahy R. Age at surgery significantly impacts the amount of orbital relapse following hypertelorbitism cor-rection: a 30-year longitudinal study. Plast Re-constr Surg. 2011;127(4):1620-30.
20. Whitaker LA, Bartlett SP, Schut L, Bruce D. Cra-niosynostosis: an analysis of the timing, treat-ment, and complications in 164 consecutive pa-tients. Plast Reconstr Surg. 1987;80(2):195-212. 21. Wan DC, Levi B, Kawamoto H, Tanna N, Tabit C,
do Amaral CR, Bradley JP. Correction of hyper-telorbitism: evaluation of relapse on long-term follow-up. J Craniofac Surg. 2012;23(1):113-7. 22. Psillakis JM, Zanini SA, Godoy R, Cardim VL.
Orbit-al hypertelorism: modification of the craniofaciOrbit-al osteotomy line. J Maxillofac Surg. 1981;9(1):10-4. 23. Cardim VL, Salomon RL, Dornelles RF, Silva AS,
Silva AL, Blom JO. Hiperteleorbitismo: uma pro-posta de tratamento. Rev Bras Cir Craniomaxilo-fac. 2008;11(4):156-62.
24. Van der Muelen JC. Medial faciotomy. Br J Plast Surg. 1979;32(4):339-42.
25. Van der Muelen JC, Vaandrager JM. Surgery re-lated to the correction of hypertelorism. Plast Re-constr Surg. 1983;71(1):6-19.
26. Converse JM, Ransohoff J, Mathews ES, Smith B, Molenaar A. Ocular hypertelorism and pseu-dohypertelorism. Advances in surgical treatment. Plast Reconstr Surg. 1970;45(1):1-13.
27. Converse JM, Smith B, Wood-Smith D. Deformi-ties of the midface resulting from malunited or-bital and naso-oror-bital fractures. Clin Plast Surg. 1975;2(1):107-30.
28. Urrego AF, Garri JI, O’Hara CM, Kawamoto HK Jr, Bradley JP. The K stitch for hypertelorbitism: im-proved soft tissue correction with glabellar width reduction. J Craniofac Surg. 2005;16(5):855-9. 29. Fuente del Campo A. A simple procedure for
aes-thetic correction of the medial epicanthal fold. Aesthetic Plast Surg. 1997;21(6):381-4.
30. Mulliken JB, Kaban LB, Evans CA, Strand RD, Murray JE. Facial skeletal changes following hypertelorbitism correction. Plast Reconstr Surg. 1986;77(1):7-16. 31. Sarnat BG, Bradley JP. The upper face and orbit:
Clinical considerations. In: Sarnat BG, Bradley JP. Craniofacial biology and craniofacial surgery. London: World Scientific; 2010. p.335-53.
Received in: 02/03/2017
Accepted for publication: 11/05/2017 Conflict of interest: none.
Source of funding: none.
Mailing address:
Cassio Eduardo Raposo-Amaral E-mail: cassioraposo@hotmail.com