rev bras reumatol.2016;56(3):240–251
ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Myelopathy
in
systemic
lupus
erythematosus:
clinical,
laboratory,
radiological
and
progression
findings
in
a
cohort
of
1,193
patients
Beatriz
Lavras
Costallat
a,
Daniel
Miranda
Ferreira
b,
Lilian
Tereza
Lavras
Costallat
a,
Simone
Appenzeller
a,∗aFaculdadedeCiênciasMédicas(FCM),UniversidadeEstadualdeCampinas(UNICAMP),Campinas,SP,Brazil
bHospitaldasClínicas,FaculdadedeCiênciasMédicas(FCM),UniversidadeEstadualdeCampinas(UNICAMP),Campinas,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received14September2015
Accepted8December2015
Availableonline14April2016
Keywords:
Systemiclupuserythematosus
Myelopathy
Transversemyelitis
Magneticresonance
a
b
s
t
r
a
c
t
Objective:To describeclinical,laboratory, radiological andprogression characteristicsof
myelopathyinsystemiclupuserythematosus(SLE).
Patientsandmethods:Aretrospectiveanalysiswasperformedonacohortof1193patients
withSLE(ACRcriteria)inordertoidentifypatientswithmyelopathy(neuropsychiatricACR).
DiseaseactivitywasassessedbytheSLEactivityindex(SLEDAI)onthedateoftheeventand
functionalcapacitywasassessedbytheExpandedDisabilityStatusScale(EDSS)atthelast
visit.
Results:Weidentified14(1.2%)patientswithmyelopathy.Allwerewomenwithamean
ageof30±11.5years.MyelopathyoccurredatthediagnosisofSLEinfour(28%)patients;
andnine(64%)patientshadanothertypeofneuropsychiatricmanifestationassociated.
Neurologicalrecurrencewasobservedinone(7%)patient.Diseaseactivitywasobservedin
2(14%)patients.Cerebrospinalfluidpresentedpleocytosison7(53%)patients;
antiphos-pholipidantibodieswerepositivein5(45%).Magneticresonanceimaging(MRI)showedT2
hyperintensitywithapredominanceoflongitudinalinvolvementin6(86%)patients.Most
weretreatedwithintravenouscorticosteroidsandcyclophosphamide.Nopatienthadfull
recoveryandfour(36%)hadhighEDSSscores.Three(21%)patientsdiedfromsepsisearly
inthecourseoftheirmyelopathy,duringorafterimmunosuppressivetherapy.
Conclusions:Myelopathyoccurredin14(1.2%)ofthepatientsinourcohortandthismaybe
thefirstmanifestationofthediseaseoccurringindependentlyofsystemicdiseaseactivity.
Althoughrare,myelopathyshowsgreatmorbidityandmortality,canberecurrentandMRI
iscriticalfordiagnosis.
©2016PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗ Correspondingauthor.
E-mail:appenzellersimone@yahoo.com(S.Appenzeller).
http://dx.doi.org/10.1016/j.rbre.2016.03.006
2255-5021/© 2016 Published by Elsevier Editora Ltda. This is an open access article under the CC BY-NC-ND license
rev bras reumatol.2016;56(3):240–251
241
Mielopatia
no
lúpus
eritematoso
sistêmico:
achados
clínicos,
laboratoriais,
radiológicos
e
evolutivos
em
uma
coorte
de
1.193
pacientes
Palavras-chave:
Lúpuseritematososistêmico
Mielopatia
Mielitetransversa
Ressonânciamagnética
r
e
s
u
m
o
Objetivo: Descrever características clínicas, laboratoriais, radiológicas e evolutivas de
mielopatianolúpuseritematososistêmico(LES).
Pacientesemétodos:Foirealizadaanáliseretrospectivadeumacoortede1193pacientescom
LES(critériosACR),paraidentificarospacientescommielopatia(ACRneuropsiquiátrico).
Aatividadededoenc¸afoianalisadapeloÍndicedeAtividadedoLES(SLEDAI)nadatado
eventoeacapacidadefuncionalpelaEscalaExpandidadoEstadodeIncapacidade(EDSS)
naúltimaconsulta.
Resultados: Foramidentificados14(1,2%)pacientescommielopatia.Todaserammulheres
commédiadeidadede30anos(DP±11,5anos).AmielopatiaocorreunodiagnósticodoLES
emquatro(28%)eemnove(64%)haviaoutrotipodemanifestac¸ãoneuropsiquiátrica
asso-ciada.Recorrênciadoquadroneurológicofoiobservadoemuma(7%)paciente.Atividade
dedoenc¸afoiobservadaem2(14%)pacientes.Olíquidocefalorraquidianoapresentava
pleocitoseem7(53%)pacientesanticorposantifosfolípideserampositivosem5(45%).A
ressonânciamagnética(RM)demonstrouhipersinalemT2compredomíniodo
comprome-timentolongitudinalem6(86%)pacientes.Amaioriafoitratadacomcorticosteroidese
ciclofosfamidaendovenosos.Nenhumapacientetevecompletarecuperac¸ãoequatro(36%)
tinhamescoresaltosdaEDSS.Óbitofoiobservadoem3(21%)duranteepisódiodemielopatia,
porsepticemiaduranteouapósterapiaimunossupressora.
Conclusões: Amielopatiaocorreuem14(1,2%)dospacientesdanossacoorteepodesera
primeiramanifestac¸ãodadoenc¸aocorrendoindependentementedeatividadesistêmicada
doenc¸a.Emborarara,édegrandemorbimortalidade,podeserrecorrenteeaRMé
funda-mentalparaodiagnóstico.
©2016PublicadoporElsevierEditoraLtda.EsteéumartigoOpenAccesssobalicença
deCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Neuropsychiatricmanifestations in systemic lupus
erythe-matosus(SLE)haveanimportantimpactontheprognosisof
thediseasebytheirfrequencyandseverity.1Myelopathyisa
manifestationofthecentralnervoussystem(CNS)thatoccurs
onlyrarelyinSLE,affectingabout1–2%ofpatients.1–3
In 1999, the American College of Rheumatology (ACR)
establishedthecriteriaofneuropsychiatricmanifestationsin
SLE,includingmyelopathy.Thispossibilityshouldbe
consid-eredifthepatientshowsarapidprogression(hoursordays)of
oneormoreofthefollowingsigns/symptoms:bilateral
mus-cleweakness in lower limbs,with or without involvement
upperlimbs;asensorydisorder withsimilarlevelofmotor
impairment,withorwithoutbowelorbladderinvolvement.
Expansiveinjurycausingspinalcordcompressionandcauda
equinainjuryshouldberuledout.4
In2002,theTransverseMyelitisConsortiumWorkingGroup
proposeddiagnosticcriteriaforidiopathictransverse
myeli-tis,definedwiththeclinicalmanifestationsdescribedabove,
associatedwithinflammationwithinthespinalcord
demon-strated bycerebrospinal (CSF) pleocytosis or increasedIgG
index or gadolinium enhancement in magnetic resonance
imaging(MRI).5
Myelopathymaypresentasatransversemyelopathywith
sectionalinvolvementofonelevelofthespinalcord,orasa
longitudinalmyelopathyinwhichmorethanthreesegments
areaffected,continuouslyornot.6
The term myelitis is still used by many authors;
how-ever,myelopathyismoresuitabletocharacterizespinalcord
changesassociatedwithinflammatorydiseasessuchasSLE,
thisbeingthenomenclaturerecommendedbyACR.4
Thecause of myelopathy inSLEisnot well understood
and the participation of both thrombosis and vasculitis
have been implicatedin this process.3 Some authors
sug-gest that there is a relationshipbetween antiphospholipid
antibodiesand myelopathy,whichwouldaugmentthe
pos-sibilityofthrombosis;butotherstudiesdonotconfirmthis
association.7–10
Although rare, thanks to its importance this condition
wasrecentlyincludedinthenewclassificationcriteriaofthe
disease.11Theliteratureonlypresentscasereports,withthe
publicationofcaseseriesonlybyafewauthors.8,10,12–19
Theaimofthisstudyistodescribecasesofmyelopathyin
SLE,fromacohortofasingleuniversityhospital,describing
theirclinicalpicture,laboratoryresults,imagingfindingson
MRIofthespinalcord,treatmentandoutcome.
Patients
and
methods
Medicalrecordsofacohortof1193patientswithSLE,20
fol-lowedattheRheumatologyoutpatientclinicoftheHospital
dasClínicas,UniversidadeEstadualdeCampinas(UNICAMP)
wereanalyzedretrospectively.
Patientswithmyelopathywereidentifiedbythepresence
242
rev bras reumatol.2016;56(3):240–251injury,andofsensoryandmotorchanges,sphincter
dysfunc-tion,or acombination ofthese,and changes consistentat
theneurologicalexamination.4,5Patientswithothercausesof
myelopathysuchascompression,trauma,malignanciesand
infectionswereexcluded.Informationondemographics,
clin-icaldataofSLEdiseasedurationofthemyelopathyepisode,
adjuvant tests, including imaging studies, auto-antibodies
and cerebrospinal fluid screening were collected. Disease
activitywasanalyzedbytheSystemicLupusErythematosus
DiseaseActivity Index –SLEDAI21 on the dayofthe event,
whendataforapplicationwereavailable,consideringdisease
activityifSLEDAI≥6,discreteactivitywhenSLEDAI<6,and
inactivitywhenSLEDAI=zero.
Informationaboutprescribedtreatmentandprogressionof
thesepatientswerealsocollected.Toevaluatethefunctional
capacity after myelopathy, the Expanded Disability Status
Scale(EDSS)ofKurtzke,appliedinthelastfollow-upvisit,was
used.22Thisisamethodusedtoquantifydisabilityoccurring
duringprogressionandovertime.
Ethicalaspects
AuthorizationoftheResearchEthicsCommittee–FCM
UNI-CAMPwasobtainedforuse ofdatafrom patients’ medical
records(OpinionoftheEthicsCommitteeofFCM-UNICAMP:
NO920/2007).
Results
Fourteen of 1193 (1.2%) SLE patients with myelopathy, all
femalesandCaucasian,withameanageattheonsetof
myelo-pathyof30±11.5yearsandmeandiseasedurationatthetime
ofmyelopathyof4±5.2years(Table1)wereidentified.
Table1showsthecumulativeclinicalmanifestationsofSLE
untilthetimeofthestudy.Infourof14(28%)patients,
myelo-pathywastheinitialmanifestation.Inone(7%)patient,the
diagnosisofSLEwasconfirmedonlytwoyearsand3months
afterthespinalcordmanifestation.
Theinitialsymptomsof these14 patientsincluded
uri-nary retention in 10 (71%), paraplegia in 7 (50%), fever in
6(42%), paraparesis in3 (21%)and paresthesiain 2(14%).
Nine(64%)patientshadalreadyhadotherneuropsychiatric
symptomsbeforethemyelopathy,three(21%)patientswith
aclinical picture ofpsychosis, two(14%) withseizure, one
(7%)withheadache,andone(7%)withcerebrovascular
dis-ease(stroke).Two(14%)patientsalsohadopticneuritis(ON).
One(7%)ofthesepatientshadsevere bilateraloptic
neuri-tismanyyearsafterherclinicalpictureofmyelopathy,which
wasconfirmedbyvisualevoked potentialchanges,without
evidenceofdemyelinatingdiseaseonbrainMRI,witha
neg-ativeresultforanti-aquaporin4antibody.Theotherpatient
hadrecurrentneuromyelitis optica(NMO)andwaspositive
foranti-aquaporin4antibody;andSLEwasconfirmed3years
andtwomonthslater,whennephritis,lymphopenia,and
pos-itivityforantinuclearantibodyandanti-DNA werenoticed.
Inthesepatientswecouldnotperformotherautoantibodies
suchasanti-MOG and anti-aquaporinI, but demyelinating
causeswereruledout,andtheclinicalpictureofbothofthem
wasattributedtoSLE.
Onlytwo(14%)patientshadnephritis,oneofthem
con-currently with myelopathy. Six patients had some typeof
hematologicalabnormalityduringthecourseofSLE.
Two(14%)patientshaddiseaseactivityduringtheepisode
ofmyelopathy,thatis,SLEDAI≥6;inone(7%)patientSLEDAI
wasnotappliedonthisoccasion,sincethediagnosisofSLE
hadnotbeenconfirmed;inthree(21%)patientstherewasno
dataavailableforthecalculationofSLEDAI.Inanother8(57%)
patientsSLEDAIwas<6,thuswithmilddiseaseactivity.Only
one(7%)patienthadnoactivedisease(Table1).Inthese10
patientsinwhomitwaspossibletoapplytheactivityindex,
aSLEDAIscorewasobtainedbecauseoffeverin3(30%),low
complementlevelsin9(90%),anti-DNApositivityin5(50%),
psychosisin1(10%),nephritisin1(10%),thrombocytopeniain
1(10%)andleukopeniain1(10%).
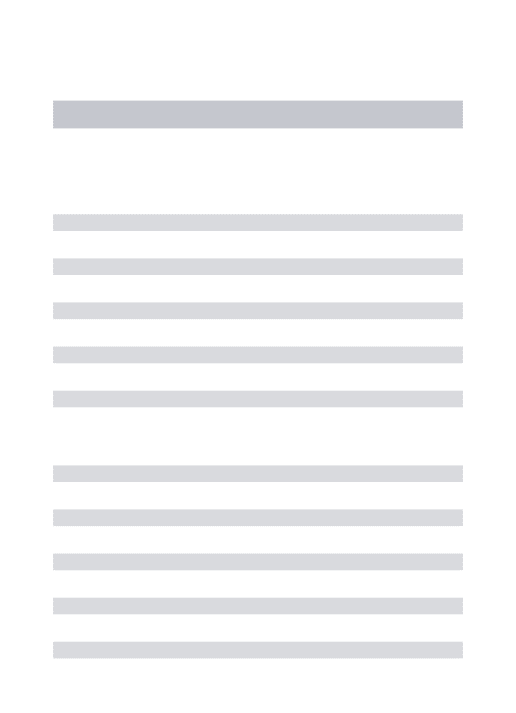
Table2showstheadditionaltestsperformedduringthe
episode of myelopathy. All patients had positive tests for
antinuclearantibodies(ANA).Anti-DNAandanti-Sm
antibod-ies were positive in 6of 13 (46%) patients who were thus
examined,andantiphospholipidantibodieswerepositivein5
of11(45%)patientssubmittedtothistest.Tenineleven(90%)
patientswhowereexaminedatthetimeofthemyelopathy
haddecreasedcomplementlevels.
Acerebrospinalfluid(CSF)testwasperformedinall(100%)
patients with normal results in seven (53%). In six (46%)
patients, pleocytosis with lymphocyte predominance was
noted. Thecultureswerenegativeinall14(100%) patients.
FulldetailsofCSFofonepatientwerenotavailable,although
thistesthadbeenconducted.
Seven(50%)patientswereexaminedbyMRI.Theother7
patients did notperform the test, and in four (28.5%)MRI
was notconductedduetolackofthis resourceinourUnit
at the time of myelopathy. In these latter patients,
myel-ography was performed in order to rule out other causes,
with normal results in all these women. The other three
(21.5%) patients died without having been able toperform
MRI,becausetherewasnoclinicalstabilityforperformingthis
test.
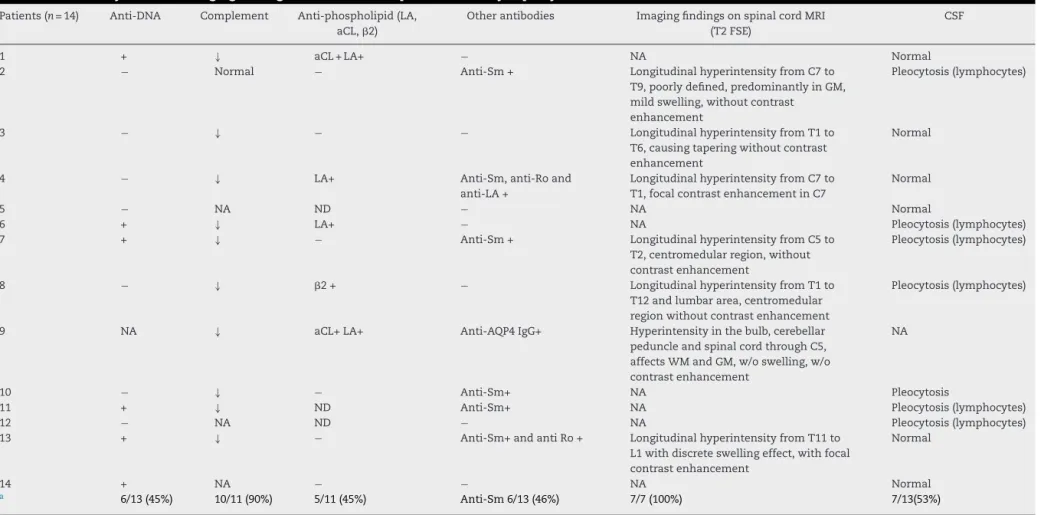
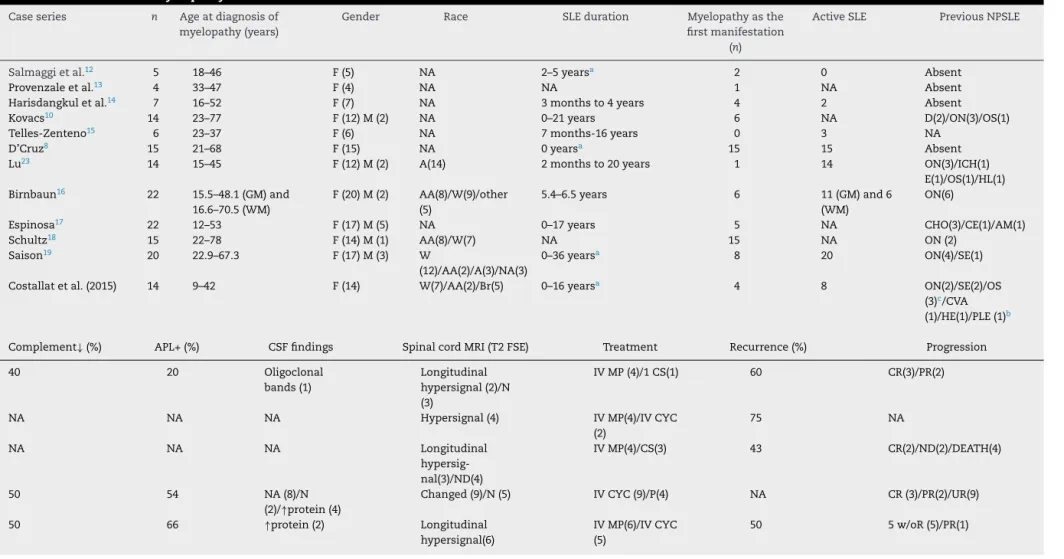
Uponthe clinicalepisode, allpatientsunderwent spinal
cordMRIinaclosed-fielddevice.In6(86%)cases,patients
hadlongitudinallesionswithhyperintensityinT2fast
spin-echosequences,withextensionto4ormorevertebrallevels
(Fig. 1)and inonlyone (14%) ofthese patients the
exam-ination was performed at 3 levels (Table 2). There was
predominantly thoracic involvement in 6 (85%) of these
cases, in 4 (57%) of them with high thoracic levels. A
spinalcordswelling effectwasnoted in2(28%)cases, and
one(14%)ofthesepatients alsoshowedcontrast
enhance-ment.Asforcontrastuptake,only2(28%)patientsshowed
enhancement at the same level of signal exchange in
pre-contrast sequences (Fig. 2). In our cases, it was not
possible to differentiate between white versus gray matter
involvement.
Withregardtotreatment,eight(57%)patientsweretreated
withacombinationofpulsetherapywithmethylprednisolone
(MP) followed by intravenous (IV) cyclophosphamide; four
(28%) patients used onlyMP pulse therapy; and two (14%)
receivedoralcorticosteroidsathighdoses,togetherwith
aza-thioprine.Allpatientsweretreatedwithinthefirsthours,or
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(3)
:240–251
243
Table1–SLE:demographic,clinical,anddiseaseactivitydataof14patientswithmyelopathy.
Patients(n=14) Race Age(years) Symptoms SLEduration
(years)
PreviousNPSLE Cumulativeclinicalmanifestationsa SLEDAI
1 Br 31 Urinaryretention/paraparesis 8 Absent Arthritis/photo/leukopenia/APS 4
2 Bl 40 Urinaryretention/paraplegia 2 Absent Arthritis/leukopenia/thrombocytopenia 0
3 W 29 Difficultyinwalking/tactilehypoesthesia 3 Psychosis Arthritis/malarrash/photo 2
4 W 42 Urinaryretention/flaccidtetraparesis 0 Seizure Malarrash/photo/oralulcers 2
5 Br 42 Fever/urinaryretention/paraplegia 2 Psychosis Arthritis/malarrash/photo/leucopenia NA
6 W 19 Urinaryretention/paresthesia 6 Stroke Arthritis/malar
rash/photo/thrombocytopenia
3
7 Br 20 Fever/urinaryretention/paraplegia 9 Absent Arthritis/malarrash/photo/nephritis 17
8 W 18 Paraparesis 1 Absent Arthritis/malar
rash/photo/serositis/lymphopenia
3
9 NA 16 Paresthesia/difficultyinwalking NAp Opticneuritis Nephritis/lymphopenia b
10 W 9 Fever/urinaryretention/paraplegia 1 Opticneuritis Arthritis/malar
rash/photo/pericarditis
3
11 Br 45 Fever/urinaryretention/paraplegia 0 Psychosis,stroke Arthritis/discoid/photo/leucopenia 13
12 W 31 Fever/urinaryretention/paraplegia 0 Headache Arthritis/alopecia NA
13 Br 41 Paraparesis 16 Seizureandplexopathy Arthritis 4
14 W 30 Fever/urinaryretention/paraplegia 13 Absent Malarrash/photo/hemolyticanemia NA
SLE,systemiclupuserythematosus;NPSLE,neuropsychiatricsystemiclupuserythematosus;SLEDAI,SystemicLupusErythematosusDiseaseActivityIndex;APS,antiphospholipidsyndrome;Br, brown;W,white;Bl,black;photo,photosensitivity;NA,notavailable;NAp,notapplicable.
a Cumulativeuntilthedateofthestudy.
244
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(3)
:240–251
Table2–LaboratorytestsandimagingfindingsonMRIof14SLEpatientswithmyelopathy.
Patients(n=14) Anti-DNA Complement Anti-phospholipid(LA, aCL,2)
Otherantibodies ImagingfindingsonspinalcordMRI (T2FSE)
CSF
1 + ↓ aCL+LA+ − NA Normal
2 − Normal − Anti-Sm+ LongitudinalhyperintensityfromC7to
T9,poorlydefined,predominantlyinGM, mildswelling,withoutcontrast
enhancement
Pleocytosis(lymphocytes)
3 − ↓ − − LongitudinalhyperintensityfromT1to
T6,causingtaperingwithoutcontrast enhancement
Normal
4 − ↓ LA+ Anti-Sm,anti-Roand
anti-LA+
LongitudinalhyperintensityfromC7to T1,focalcontrastenhancementinC7
Normal
5 − NA ND − NA Normal
6 + ↓ LA+ − NA Pleocytosis(lymphocytes)
7 + ↓ − Anti-Sm+ LongitudinalhyperintensityfromC5to
T2,centromedularregion,without contrastenhancement
Pleocytosis(lymphocytes)
8 − ↓ 2+ − LongitudinalhyperintensityfromT1to
T12andlumbararea,centromedular regionwithoutcontrastenhancement
Pleocytosis(lymphocytes)
9 NA ↓ aCL+LA+ Anti-AQP4IgG+ Hyperintensityinthebulb,cerebellar
peduncleandspinalcordthroughC5, affectsWMandGM,w/oswelling,w/o contrastenhancement
NA
10 − ↓ − Anti-Sm+ NA Pleocytosis
11 + ↓ ND Anti-Sm+ NA Pleocytosis(lymphocytes)
12 − NA ND − NA Pleocytosis(lymphocytes)
13 + ↓ − Anti-Sm+andantiRo+ LongitudinalhyperintensityfromT11to
L1withdiscreteswellingeffect,withfocal contrastenhancement
Normal
14 + NA − − NA Normal
a 6/13(45%) 10/11(90%) 5/11(45%) Anti-Sm6/13(46%) 7/7(100%) 7/13(53%)
SLE,systemiclupuserythematosus;CSF,cerebrospinalfluid;NA,notavailable;ND,notdone;aCL,anticardiolipinantibody;LAlupusanticoagulant;2,anti-beta2glycoproteinIantibody,anti-AQP4 IgG,anti-aquaporin4;WM,whitematter;GM,graymatter;MRI,magneticresonanceimaging,T2FSE,T2fastspin-echosequence
rev bras reumatol.2016;56(3):240–251
245
Fig.1–SagittalT2-weightedimagesshowinghyperintensityinspinalcord,extendingfromthebulbtoC3inthefirst episode(A)andhyperintensityandincreasedspinalcordvolumeextendingtoC5inthesecondepisode,sevenmonths afterthefirstone(B).
Uponthe applicationofEDSSafterameanfollow-up of
11.5±10.4years,itwasobservedthatall11(78%)patientsin
whichitwaspossibletoapplythisscalehadsomedegreeof
disability,whosescorerangedfrom3to8,i.e.frompatients
abletowalkbutwithsomedegreeofdisability, topatients
withneurogenicbladderrequiringwheelchairuse.Nopatient
obtainedafullrecovery.
Three(21%)deathsoccurredduringthemyelopathy
man-ifestation, caused bya widespread infection that occurred
duringorshortlyaftertheimmunosuppressivetherapy
pre-scribedfortreatmentofmyelopathyinallthreecases.
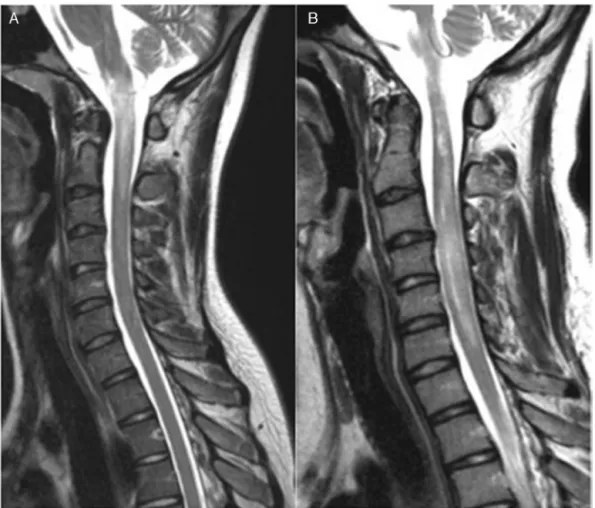
Table3liststreatment,monitoringandprogressiondata. Table4showstherelevantseriesofcasesofmyelopathyin
SLEwhichhavebeenpublishedinEnglishlanguage,
includ-ing the present series, with information on MRI findings.
Twelvecaseseriesarepresented,withresultsshowing4–22
patientsandtheirdemographic,respectiveclinicaland
labo-ratorycharacteristicsandMRI,treatmentandoutcomedata.
Diseaseactivity,recurrenceofepisodesandthepresenceof
otherneuropsychiatricsymptoms,inadditiontothe
occur-renceofmyelopathyasthefirstmanifestationofthedisease,
arealsohighlightedinthistable,whenevermentionedbytheir
authors.
Table3–Treatment,monitoringandprogressionof14 patientswithSLEandmyelopathy.
Patients Treatment Follow-up EDSS
1 IVMPandIVCYC 6years 5.5
2 IVMPandIVCYC 14years 3
3 CSandAZA 15years 6
4 IVMPandIVCYC 22years 7.5
5 IVMP 3years 6
6 IVMPandIVCYC 2months Death
7 IVMPEIVCYC 4months 3.5
8 IVMPandIVCYC 12months 6
9 IVMP,IVCYC,IVIG andMMF
3years 3
10 IVMP 24years 8
11 IVMP 2months Death
12 CSandAZA 1year 8
13 IVMPandIVCYC 2years 8
14 IVMP 8years Death
246
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(3)
:240–251
Table4–CaseseriesofmyelopathyinSLE.
Caseseries n Ageatdiagnosisof myelopathy(years)
Gender Race SLEduration Myelopathyasthe
firstmanifestation (n)
ActiveSLE PreviousNPSLE
Salmaggietal.12 5 18–46 F(5) NA 2–5yearsa 2 0 Absent
Provenzaleetal.13 4 33–47 F(4) NA NA 1 NA Absent
Harisdangkuletal.14 7 16–52 F(7) NA 3monthsto4years 4 2 Absent
Kovacs10 14 23–77 F(12)M(2) NA 0–21years 6 NA D(2)/ON(3)/OS(1)
Telles-Zenteno15 6 23–37 F(6) NA 7months-16years 0 3 NA
D’Cruz8 15 21–68 F(15) NA 0yearsa 15 15 Absent
Lu23 14 15–45 F(12)M(2) A(14) 2monthsto20years 1 14 ON(3)/ICH(1)
E(1)/OS(1)/HL(1)
Birnbaun16 22 15.5–48.1(GM)and
16.6–70.5(WM)
F(20)M(2) AA(8)/W(9)/other (5)
5.4–6.5years 6 11(GM)and6
(WM)
ON(6)
Espinosa17 22 12–53 F(17)M(5) NA 0–17years 5 NA CHO(3)/CE(1)/AM(1)
Schultz18 15 22–78 F(14)M(1) AA(8)/W(7) NA 15 NA ON(2)
Saison19 20 22.9–67.3 F(17)M(3) W
(12)/AA(2)/A(3)/NA(3)
0–36yearsa 8 20 ON(4)/SE(1)
Costallatetal.(2015) 14 9–42 F(14) W(7)/AA(2)/Br(5) 0–16yearsa 4 8 ON(2)/SE(2)/OS
(3)c/CVA
(1)/HE(1)/PLE(1)b
Complement↓(%) APL+(%) CSFfindings SpinalcordMRI(T2FSE) Treatment Recurrence(%) Progression
40 20 Oligoclonal
bands(1)
Longitudinal hypersignal(2)/N (3)
IVMP(4)/1CS(1) 60 CR(3)/PR(2)
NA NA NA Hypersignal(4) IVMP(4)/IVCYC
(2)
75 NA
NA NA NA Longitudinal
hypersig-nal(3)/ND(4)
IVMP(4)/CS(3) 43 CR(2)/ND(2)/DEATH(4)
50 54 NA(8)/N
(2)/↑protein(4)
Changed(9)/N(5) IVCYC(9)/P(4) NA CR(3)/PR(2)/UR(9)
50 66 ↑protein(2) Longitudinal
hypersignal(6)
IVMP(6)/IVCYC (5)
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(3)
:240–251
247
Table4–(Continued)
Complement↓(%) APL+(%) CSFfindings SpinalcordMRI(T2FSE) Treatment Recurrence(%) Progression
NA 73 Pleocytosis(2)/N
(13)
Changed(11)/N (2)/ND(1)
IVMP(7)/CS (6)/AZA(6)
6 CR(6)/PR(9)
28 11 Pleocytosis(6) Longitudinal
hypersignal(6) focal(5)/N(1)/ND(2)
CS(14)/IVCYC (2)/P(1)
7 R(4)
NA 54 Pleocytosis(GM) Longitudinal
hypersignal92% (GM)and74% (WM)
GMgroup,more aggressive therapy
9(GM)and 73(WM)
GMgroup,moredisability (meanofEDSS>inGM group)
74 50 Predominanceof
pleocytosis
Longitudinal hypersignal(22)
IVMP(22)/IVCYC (13)/IV
IG(4)/P(4)/RTX(2)
18 CR(3)/PR(13)/w/oR(6)
87 11 ↑protein Predominanceof
focallesion
IVMP(14)/IVCYC (2)/P(1)
NA NA
87 45 Pleocytosis(5) Longitudinal
hypersignal(9)/N (3)
IVMP(18)/IV CYC(11)/IV IG(2)/P(3)/RTX(3)
50 CR(5)/PR(12)/w/oR(1)/O(1)
90 45 Pleocytosis(7)/N
(6)
Longitudinal hypersignal(7)
IVMP(12)/CS (2)/IVCYC (10)/AZA(1)
7 CR(0)/PR(7)/w/oR(4)/DEATH(3)
SLE,systemiclupuserythematosus;NPSLE,neuropsychiatricsystemiclupuserythematosus;APL,antiphospholipidantibody;CSF,cerebrospinalfluid;FSET2,T2fastspin-echosequence;F,female;M, male;AA,AfricanAmerican;Br,brown,;A,Asian;W,white;NA,notavailable;ND,notdone;N,Normal;GM,graymatter;WM,whitematter;CHO,chorea;CE,cerebritis;HE,headache;SE,seizure;AM, asepticmeningitis;ICH,intracranialhemorrhage;HL,hearingloss;PSpsychosis;PLE,plexopathy;E,epilepsy;ON,opticneuritis;D,depression;CVA,stroke;IVMP,intravenousmethylprednisolone; IVCYC,intravenouscyclophosphamide;AZA,azathioprine;IVIG,intravenousimmunoglobulin;CS,corticosteroids;P,plasmapheresis;RTX,Rituximab;CR,completeremission;PR,partialremission; R,remission;w/oRwithoutremission.
a WithcasesofmyelopathyprecedingSLE.
b Withseizure.
248
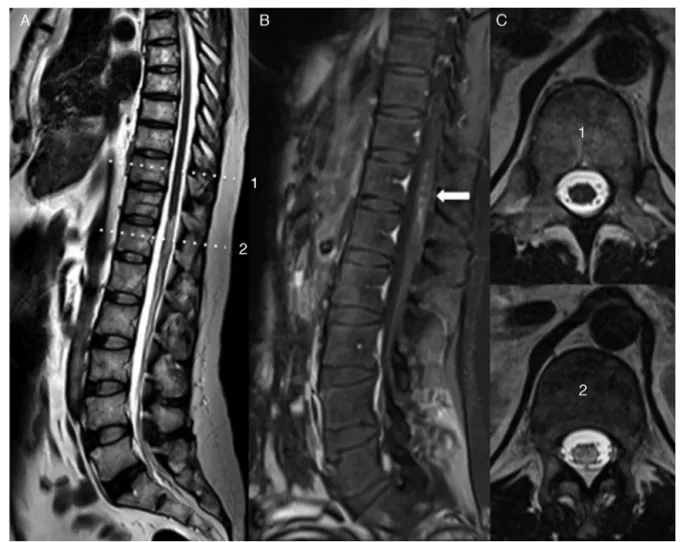
rev bras reumatol.2016;56(3):240–251Fig.2–SagittalT2-weightedimage,showinghyperintensityandmildenlargementofspinalcordvolume,extendingfrom T11tothemedullarycone.B,T1-weightedsagittalimageaftercontrastinjection,withfociofmedullaryenhancement (arrow)extendingfromT11toL1.C,AxialT2-weightedimagesdemonstratingthespinalcordwithanormalsignal obtainedattheT10level(1)andspinalcordwithhyperintensityobtainedatthelevelofT12(2).
Discussion
Myelopathyisoneofthemostrareneuropsychiatric
mani-festationsinSLE,affectingabout1–2%ofpatients,but this
conditionisveryrelevant,thankstoitshighmorbidityand
mortalityandhasbeenincludedinthenewSLEcriteria.11
Our 14 patients represented 1.2%of the cohort of 1193
patientswithSLE,apercentagesimilartothat observedin
previousstudies.1,2
All patients were female, as noted by all authors and
in line with the gender profile of this disease.8,10,12–19,23
Myelopathycan affect individuals ofall ages; ourpatients
had a mean age of 30 years – a lower mean than that
observed by other authors,8,10,12,13,15,17–19,23 and similar to
those described in two series.14,15 As for the race, there
is no reference to a higher prevalence of this
mani-festation in any ethnic group, and many authors have
not highlighted this demographic characteristic. However,
Schutz et al., in a comparison of myelopathy in SLE
ver-susidiopathic myelopathy,commentthe highestfrequency
ofAfrican–AmericanwomenwithSLE, butthis factcan be
attributed to the prevalence of the disease itself in that
area.18
Initialsymptomsarenonspecificandmayincludeashort
viralprodrome:fever,photophobia,nausea,vomiting,
dizzi-ness and nuchal pain. Subsequently, sensory and motor
changesandsphincterdysfunctioncanoccur,anditsonset
cantakehours,daysorevenweeks.Ourmyelopathypatients
presentedwithurinary retentionand fever,whichwas
ini-tially confused,insomecases,withurinarytractinfection.
Thespinalcordinjuryclueswereparesthesia,walking
difficul-ties,paraplegiaandsphincterdysfunction,withsuddenonset
withinhoursordays.
Inasystematicreviewof22casesreportedinthe
litera-turebyEspinosaetal.,theauthorsobservedin23%ofcases
a prodromal picture offever, cough,flu and constitutional
symptomsafewdaysbeforetheonsetofmyelopathy,17which
wasobservedalsobyHarisdangkuletal.11Thepresenceof
feverandurinaryretentionwasassociatedwithanirreversible
paraplegia,accordingtoBirnbaumetal.16
MyelopathymaybetheinitialmanifestationofSLE,as
hap-penedwithfourofourpatients;andthisfactwasnotedbyall
rev bras reumatol.2016;56(3):240–251
249
etal.15 Someauthorsconsiderthatwhenmyelopathyoccur
inSLE,this canbeaninitialmanifestationinup to39%of
patientswithinthefirstfiveyears.10Byanalyzingtheseries
ofreportedcases(Table4),andtakingintoaccountthetime
pointwherethemyelopathymayariseduringtheprogression
ofSLE,wecanobservetheoccurrenceofavariable
percent-age forthe duration of SLE,and there are cases inwhich
thepatientalreadyhadSLEfor36yearsbeforetheonsetof
myelopathy.19Itisalsopossiblethatmyelopathyarisesbefore
SLE;this happenedinonecaseinourseries, inwhichthe
patientpresentedwithspinalcordmanifestations2yearsand
3monthsbeforeherdiagnosisofSLE.All15casesdescribed
byD’Cruzetal.8 wereaffectedbymyelopathyastheinitial
manifestationofSLE,and only4(26%)met ACRcriteriafor
SLEattheonsetofmyelopathy.OfthefivecasesofSalmaggi
etal.,12 intwopatients myelopathy precededSLE,and the
sameoccurredwith4(20%)of20casesofaFrench
multicen-terstudy.InthisFrenchstudy,twocaseshadmyelopathyfor
morethan10yearsbeforetheestablishmentofadiagnosisof
SLE.19Salmaggietal.12concludedthatinwomenwith
myelo-pathyofunknownetiology,exhaustiveclinicalandlaboratory
assessmentsarecriticaltotrytodefineSLE.
AlthoughmyelopathyinSLEcanberecurrent,6,10 inour
series13(93%)patientshadasingleepisodeofthiscondition;
andonlyone(7%)patientexperiencedrecurrence.Recurrence
wasobservedinmanycaseseries,insomeofthemwithhigh
frequency(50–75%)asemphasizedinTable4.8,10,12–19,23This
significantpossibilityofrecurrenceimposestheneedforthe
implementationofamaintenanceimmunosuppressive
treat-ment for these patients, in an attempt to prevent further
crises.
Other neuropsychiatric manifestationshavebeen
corre-latedtothepresenceofmyelopathyinSLE10;inourseriessuch
eventsoccurredinnine(64%)patients. Inmostcases,
neu-ropsychiatricinvolvementwasanintegralpartoftheclinical
historyofthedisease,butwithoutasimultaneousoccurrence,
with the exception of one ofthe patients who had major
manifestationofpsychosis concomitantly withspinal cord
symptoms, and this patientdied after immunosuppressive
therapy.Two (14%)patientshadoptic neuritis.Optic
neuri-tisisaneuropsychiatricmanifestationoftenassociatedwith
myelopathy,also known as Devic disease or neuromyelitis
optica(NMO),andthisconditionwasreportedinsomeofthe
seriesofcasespresentedinTable4. Forsomeauthors,the
associationwithopticneuritismaybepresentin21–48%of
casesofmyelitisinSLE.10,16,23Neuromyelitisopticarecurrence
hasbeen describedinpatients positivefor
anti-aquaporin-4 antibody (anti-AQP4 IgG).24 One of our patients showed
NMOassociatedwithpositivityforanti-aquaporin4antibody,
beingtheonlycasewitharecurrentpictureofmyelopathy.
Another patientwithNMO developedbilateral optic
neuri-tismanyyearsaftermyelitis,whichwasconfirmedbyvisual
evokedpotentialtest,althoughantiaquaporin-4antibodywas
negative,whichcanoccurinNMOcases.Inbothcases,the
possibilityofdemyelinatingdiseasewasruledout,andthese
manifestationshavebeenattributedtoSLE.
Theoccurrenceofmyelopathymaybeassociatedwith
dis-easeactivity.Inourseries,twopatientshadactivedisease(one
withnephritisandtheotherwithpsychosis)andonepatient
showedinactivedisease;theremainingcasesexhibitedmild
diseaseactivity.Somepatientshadnoclinicalandlaboratory
datatoallowcalculationofthisindex;andSLEDAIwasnot
appliedinonepatientbecauseatthetimeofemergenceof
myelopathythediagnosisofSLEhadnotyetbeenconfirmed.
Some authors highlight thefact that inone thirdofcases
myelopathycanoccurinascenarioofinactivedisease.25That
isimportant,becauseinthefaceofarelevantclinicalpicture,
one should always consider myelopathy, regardless ofSLE
activity.Asfortheotherauthorsofthecaseseriespresented
inTable4,noteveryonerecordeddataondiseaseactivity.
Withrespecttoothertests,complementwasreducedin
10(90%)patientsofourcases,insomecasesaccompaniedby
otherlaboratorychanges,andinthreecasesthiswastheonly
punctuationonSLEDAIscore.
Antiphospholipid antibodies have been associated with
myelopathyinSLE7,10;inourseries,wefoundthese
antibod-iesin5(45%)ofcases,justasobservedbySaisonetal.17But
onlyone(7%) ofour patientsfulfilled theantiphospholipid
syndrome(APS) criteria.Other authors havefoundvariable
percentages, between 11% and 73% of cases, as shown in
Table4.AccordingtoBirnbaumetal.,16antiphospholipid
anti-bodiescanbeimportantinthepathogenesisofneuromyelitis
optica. In anextensive systematicreviewbyKatsiari et al.
ontheoccurrenceoftheseantibodiesincasesoftransverse
myelitis and the use ofanticoagulation inthe presenceof
myelopathy,these authorsconcludedthat, while
antiphos-pholipidantibodies mayhavearoleinthe pathogenesisof
myelopathy,themerepresenceoftheseantibodiesisnot
suf-ficienttoindicatetheanticoagulationtherapy.26
Thefindingsofthecerebrospinalfluidanalysisare
non-specific. Someauthorsfoundincreasedcellularity andalso
proteinorrhachia,18,23butoftentheCSFisnormalinpatients
withmyelopathy.7,10,27Inourseries,CSFwascollectedinall
(100%)patients,andthemostfrequentchangewaspleocytosis
(53%),withlymphocytepredominance.
Magneticresonanceimagingisthemostsensitive
imag-ingtoolintheevaluationofspinalcordinjuries,includingin
myelopathyassociatedwithSLE.Theexaminationprotocolfor
MRIimagesshouldcoverthelevelcorrespondingto
neurologi-caldamageobservedonclinicalexamination,butitisstrongly
recommendedtostudytheentirecord.Theimagingfindings
mayvary,withanemphasisontheT2hyperintensesignalon
spinalcord,theeffectofswellingincasesofspinalcordedema,
andalsothecontrastuptake.Amongthesefindings,themost
common isthesignal change,aswas alsoobservedinour
study.Wemustbearinmindthatinsomecases,MRImaybe
normal,especiallyintheearlystages.8,10,12Incaseswherethe
MRIimagingwithcontrastisnormal,itisrecommendedthat
thetestberepeated2–7daysaftertheinitialmanifestation.5
It is importantto note that CT should not beused for
diagnosis ofmyelopathybecause ofitslowsensitivity.This
technologyshouldbeusedincaseswheretheMRIis
unavail-able, andonlytoexcludecompressivecauses ofthespinal
cord.5
The thoracic region is the most frequently affected
part, which alsooccurred inourpatients.10,23 Thismay be
attributed to the type of blood supply that nourishes the
region, withemphasisforthe branches ofthelongitudinal
arteriesthatarelesslargeinthethoracicregionwhen
250
rev bras reumatol.2016;56(3):240–251in the vascular supply, as concluded by Kovacset al.10 In
recentyears,withtheimprovementinthequalityofimages
andequipment,anincreaseintheidentificationof
longitu-dinalspinalcordinjurieswasnotedincasesofmyelopathy
inSLEexaminedbyMRI–afactalsoobservedinmostofour
patients.15,18
Birnbaum et al. compared patients with lesions in
spinalcordwhitematter(spasticityandhyperreflexia)versus
patientswithlesionsinthegraymatter(flaccidityand
hypore-flexia).Theseauthorsconcludedthatthelesionsinthegray
matterareassociatedwithirreversibleparaplegiaandgreater
diseaseactivity.16Wecouldnotmakethisdistinctioninour
patients.
While being very important for the diagnosis of these
patients,MRIdoesnotseemtohavemuchusefortheir
follow-up,becausethereisnoclinicalcorrelationaftertreatmentin
theinitialstages.18Asfortheprognosis,thereseemstobea
worseprognosisinpatientswithchangesinMRIinthe
begin-ningoftheprocess,whencomparedtopatientswithnormal
MRI,10 especiallyinthosecaseswithpresenceofextensive
lesions.15
Thetreatmentofmyelopathyshouldbeinstituted
imme-diatelyafterthediagnosis,asthismanifestationhasapoor
prognosis,withhighmorbidityinupto50%ofcases10,23and
with high mortality. Delayed institution of an appropriate
treatmentwastheunfavorable outcomefactor notedbyall
authorsselected.Thecombinationofintravenouspulsesof
methylprednisoloneandcyclophosphamideisconsideredthe
treatmentofchoiceforsuchpatients.6,27AccordingtoSaison
et al.,19 the use ofhydroxychloroquine decreasedthe
neu-rologicalflaresincasesofmyelopathyinSLE,althoughthis
findingwasnotstatisticallysignificant.Insomecasesitis
nec-essarytouse intravenousimmunoglobulin,plasmapheresis
andrituximab,28especiallyinunresponsiveorrecurrentcases;
buttheresponsevary.Twelve(85%)ofourpatientsreceived
pulseMPand10(71%)receivedIVcyclophosphamidewithin
onemonth ofthe onset ofsymptoms. Ourunique caseof
recurrencewastreated,alongthediseaseprogression,with
IVimmunoglobulinandmycophenolatemofetil(MMF).None
ofourpatientsachievedfullrecovery.Theevaluationofthese
patientsbyEDSSresultedinscoresof7.5–8infourofthem,
thatis, patientswithwalking difficultiesand requiringthe
use ofa wheelchair,besidesaneurogenicbladder.All four
(28%)patientsusedMP pulseathigh doses,andtwo (14%)
ofthemwerealsomedicatedwithIVcyclophosphamide;but
eventhentheoutcome wasnotfavorable,perhapsbecause
notallofthemhaveusedbothmedicationswithintwoweeks
aftertheonsetofthemanifestation.Inourgroup,three(21%)
deathsoccurred,allcausedbyaninfectionduringorshortly
after immunosuppressive therapy for treatment of
myelo-pathy.Thisreinforcestheseriousnessofthismanifestation.
Theprognosticfactorsofmyelopathyarenotfullyknown,
butsphincterdysfunction,16,23MRIchanges,10,16involvement
ofgraymatter(flaccidityandhyporeflexia),16andinitial
sever-ity with paraplegia19 are cited as poor prognostic factors.
Musclestrength≥grade3atthetimeofhospitalizationand
anaggressivetherapyinstitutednolaterthantwoweeksafter
theepisodeofmyelopathyarebetterprognosticfactors.23In
summary,myelopathyinSLEisveryrare,butalsovery
seri-ous.Itoccurredin14(1.2%)ofourpatients.Myelopathymay
bethefirstmanifestationofthedisease,canoccuraftermany
years ofaninstalledSLE,ormay evenprecedethe disease.
Althoughrare,myelopathyhashighmorbidityandmortality
andmaybepresent,regardlessofdiseaseactivity.Moreover,
itcanberecurrentandthereforeitisrecommendeda
mainte-nanceimmunosuppressivetherapysothatnewepisodesare
prevented.MRIisessentialfordiagnosis,butthisexamination
maybenormalinveryearlystages.
Funding
Capes (Master’s scholarship) and CNPq (302205/2012-8,
466715/2014-5).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.WestSG.Neuropsychiatriclupus.RheumDisClinNAm. 1994;20:129–58.
2.TheodoridouA,SettasL.Demyelinationinrheumatic diseases.JNeurolNeurosurgPsychiatry.2006;77:290–5. 3.AllenIV,MillarJH,KirkJ,ShillingtonRK.Systemiclupus
erythematosusclinicallyresemblingmultiplesclerosisand withunusualpathologicalandultrastructuralfeatures.J NeurolNeurosurgPsychiatry.1979;42:392–401.
4.TheAmericanCollegeofRheumatologynomenclatureand casedefinitionsforneuropsychiatriclupussyndromes. ArthritisRheum.1999;42:599–608.
5.GroupTMCW.Proposeddiagnosticcriteriaandnosologyof acutetransversemyelitis.Neurology.2002;59:499–505. 6.BertsiasGK,IoannidisJP,AringerM,BollenE,BombardieriS,
BruceIN,etal.EULARrecommendationsforthemanagement ofsystemiclupuserythematosuswithneuropsychiatric manifestations:reportofataskforceoftheEULARstanding committeeforclinicalaffairs.AnnRheumDis.
2010;69:2074–82.
7.LavalleC,PizarroS,DrenkardC,Sánchez-GuerreroJ, Alarcón-SegoviaD.Transversemyelitis:amanifestationof systemiclupuserythematosusstronglyassociatedwith antiphospholipidantibodies.JRheumatol.1990;17:34–7. 8.D’CruzDP,Mellor-PitaS,JovenB,SannaG,AllansonJ,TaylorJ,
etal.Transversemyelitisasthefirstmanifestationof systemiclupuserythematosusorlupus-likedisease:good functionaloutcomeandrelevanceofantiphospholipid antibodies.JRheumatol.2004;31:280–5.
9.MokCC,LauCS,ChanEY,WongRW.Acutetransverse myelopathyinsystemiclupuserythematosus:clinical presentation,treatment,andoutcome.JRheumatol. 1998;25:467–73.
10.KovacsB,LaffertyTL,BrentLH,DeHoratiusRJ.Transverse myelopathyinsystemiclupuserythematosus:ananalysisof 14casesandreviewoftheliterature.AnnRheumDis. 2000;59:120–4.
11.PetriM,OrbaiAM,AlarcónGS,GordonC,MerrillJT,FortinPR, etal.DerivationandvalidationoftheSystemicLupus InternationalCollaboratingClinicsclassificationcriteriafor systemiclupuserythematosus.ArthritisRheum.
2012;64:2677–86.
rev bras reumatol.2016;56(3):240–251
251
erythematosus:clinicalandmagneticresonancefindingsin5 patients.ClinExpRheumatol.1994;12:389–94.
13.ProvenzaleJM,BarboriakDP,GaenslerEH,RobertsonRL, MercerB.Lupus-relatedmyelitis:serialMRfindings.AJNRAm JNeuroradiol.1994;15:1911–7.
14.HarisdangkulV,DoorenbosD,SubramonySH.Lupus transversemyelopathy:betteroutcomewithearly recognitionandaggressivehigh-doseintravenous corticosteroidpulsetreatment.JNeurol.1995;242: 326–31.
15.Téllez-ZentenoJF,Remes-TrocheJM,Negrete-PulidoRO, Dávila-MaldonadoL.Longitudinalmyelitisassociatedwith systemiclupuserythematosus:clinicalfeaturesandmagnetic resonanceimagingofsixcases.Lupus.2001;10:851–6. 16.BirnbaumJ,PetriM,ThompsonR,IzbudakI,KerrD.Distinct
subtypesofmyelitisinsystemiclupuserythematosus. ArthritisRheum.2009;60:3378–87.
17.EspinosaG,MendizábalA,MínguezS,Ramo-TelloC,
CapelladesJ,OlivéA,etal.Transversemyelitisaffectingmore than4spinalsegmentsassociatedwithsystemiclupus erythematosus:clinical,immunological,andradiological characteristicsof22patients.SeminArthritisRheum. 2010;39:246–56.
18.SchulzSW,SheninM,MehtaA,KebedeA,FluerantM,Derk CT.Initialpresentationofacutetransversemyelitisin systemiclupuserythematosus:demographics,diagnosis, managementandcomparisontoidiopathiccases.Rheumatol Int.2012;32:2623–7.
19.SaisonJ,Costedoat-ChalumeauN,Maucort-BoulchD,IwazJ, MarignierR,CacoubP,etal.Systemiclupus
erythematosus-associatedacutetransversemyelitis:
manifestations,treatments,outcomes,andprognosticfactors in20patients.Lupus.2015;24:74–81.
20.HochbergMC.UpdatingtheAmericanCollegeof Rheumatologyrevisedcriteriafortheclassificationof systemiclupuserythematosus.ArthritisRheum. 1997;40:1725.
21.BombardierC,GladmanDD,UrowitzMB,CaronD,ChangCH. DerivationoftheSLEDAI.Adiseaseactivityindexforlupus patients.TheCommitteeonPrognosisStudiesinSLE. ArthritisRheum.1992;35:630–40.
22.KurtzkeJF.Ratingneurologicimpairmentinmultiple sclerosis:anexpandeddisabilitystatusscale(EDSS). Neurology.1983;33:1444–52.
23.LuX,GuY,WangY,ChenS,YeS.Prognosticfactorsoflupus myelopathy.Lupus.2008;17:323–8.
24.DroriT,ChapmanJ.Diagnosisandclassificationof neuromyelitisoptica(Devic’ssyndrome).AutoimmunRev. 2014;13:531–3.
25.LiXY,XiaoP,XiaoHB,ZhangLJ,PaiP,ChuP,etal.Myelitisin systemiclupuserythematosusfrequentlymanifestsas longitudinalandsometimesoccursatlowdiseaseactivity. Lupus.2014;23:1178–86.
26.KatsiariCG,GiavriI,MitsikostasDD,YiannopoulouKG, SfikakisPP.Acutetransversemyelitisandantiphospholipid antibodiesinlupus.Noevidenceforanticoagulation.EurJ Neurol.2011;18:556–63.
27.BarileL,LavalleC.Transversemyelitisinsystemiclupus erythematosus–theeffectofIVpulsemethylprednisolone andcyclophosphamide.JRheumatol.1992;19:370–2. 28.ScottTF,FrohmanEM,DeSezeJ,GronsethGS,Weinshenker
BG.NeurologyTaTASoAAo.Evidence-basedguideline:clinical evaluationandtreatmentoftransversemyelitis:reportofthe TherapeuticsandTechnologyAssessmentSubcommitteeof theAmericanAcademyofNeurology.Neurology.