Early diagnosis of lip cancer preceded
by a persistent actinic lesion in a kidney
transplant patient: a case report
Francisco Artur Forte Oliveira, DDS, MSc QClarissa Pessoa Fernandes, DDS, MSc QAna Paula Negreiros Nunes Alves, DDS, MSc, PhD Mario Rogerio Lima Mota, DDS, MSc, PhD QPaula Frassinetti Castelo Branco Camurca Fernandes, MD, MSc, PhD
Fabricio Bitu Sousa, DDS, PhD
Lip cancer is 65 times more likely to occur in kidney transplant patients than in members of the general population. Immunosuppression drugs taken by the transplant patients have been associated with this increased occurrence. This case report shows the progression from actinic cheilosis to squamous cell carcinoma (SCC) in the lower lip of a 58-year-old man receiving immunosuppressive therapy 9 years after undergoing a kidney transplant. Earlier incisional biopsies had resulted in a histological
diagnosis of actinic cheilosis. However, the last incisional biopsy showed histological results compatible with SCC, and oncological surgery was performed. Eight months post-surgery, the patient was free of cancer and metastasis. Frequent dental follow-up visits allowed for the early diagno-sis, proper treatment, and an improved prognosis for this patient.
Received: December 2, 2012 Accepted: April 8, 2013
O
ne well-established complication of organ transplantation is an increased risk for various types of cancer.1Kidney transplant patients have a greater risk of developing lip cancer, nonmela-noma skin cancer (NMSC), anogenital neoplasias, and non-Hodgkin lymphoma compared to the general population. Immunosuppressive therapy—administered to prevent rejection of the transplanted organ—has been cited as a factor in the increased incidence of these diseases.1-3
Squamous cell carcinoma (SCC) is a malignancy that is most commonly found in the head and neck region.
The incidence of SCC in the lower lip is up to 65 times higher in kidney transplant patients compared to the general population.1 The transitional
epithelium between the lip mucosa and the skin makes this area vulnerable to carcinogenic factors such as ultraviolet (UV) radiation, either UVA (longwave) or UVB (shortwave). Actinic cheilosis presents as a scaly lesion on the lip vermilion and is caused by damage from UV radiation. The progression of an actinic lesion to SCC has been shown to be potentiated by certain immunosuppressive drugs.4,5
The progression from actinic lesions to SCC involves a number of risk factors. Major risk factors include the intensity of sun exposure (influenced by geographic latitude, occupational habits, and skin color), age, and genetic predisposition; minor risk factors include immunosup-pression (as occurs in organ transplanta-tion), tobacco, alcohol, and human papilloma viruses (HPVs).6
Long-term administration of immu-nosuppressive drugs, combined with exposure to carcinogenic factors, result in immune deregulation and DNA damage.7 The type, dose, and duration of
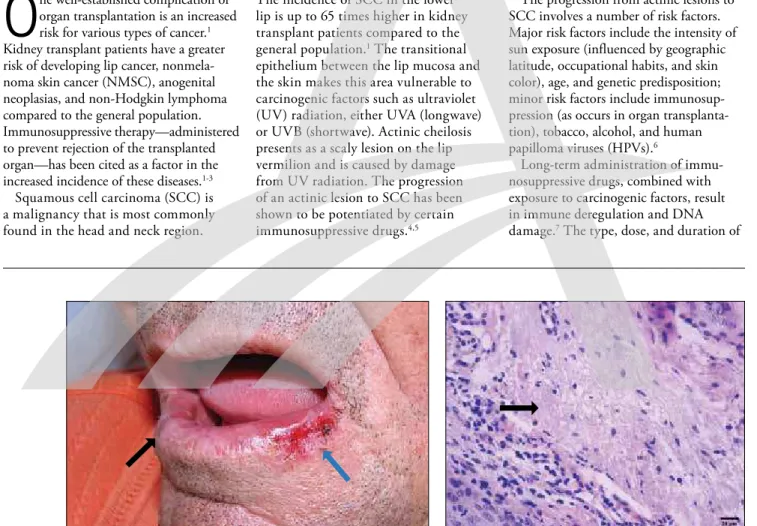
Fig. 1. Clinical aspect of an ulcerative irregular lesion on the patient’s lower lip (blue arrow) and leukoplakic areas throughout the lip (black arrow).
Fig. 2. Photomicrograph of the ulcerative lesion, showing the underlying connective tissue with basophilic alteration of collagen (arrow) (H&E, magnification 200X).
Cancer Screening
the administration of immunosuppres-sive drugs can affect the risk of cancer. One group of immunosuppressors are calcineurin inhibitors, such as tacrolimus and cyclosporine; they elevate the risk of cancer considerably (especially cyclospo-rine) compared to other classes of drugs.8,9
This article presents a case involving a kidney transplant patient who received an early diagnosis of lower lip SCC. Frequent follow-up visits enabled the dentist to employ proper treatment for the lesion, thus providing an improved prognosis.
Case report
A 58-year-old man who had received a kidney transplant 9 years earlier due to lupus nephritis was referred from the Nephrology Service of the Federal University of Ceara Hospital, Brazil,
to the university’s School of Dentistry for treatment. The patient had received immunosuppressive therapy since the transplant, taking cyclosporine (originally 300 mg, now 75 mg), mycophenolate mofetil, and prednisone (originally 20 mg, now 5 mg). The patient stated at anamne-sis that he was an agriculturist and a non-smoker who used to work under intense exposure to the sun. During clinical evaluation, an ulcerative recurrent lesion (approximately 2 cm in diameter) exhibit-ing some healexhibit-ing areas was observed on the lower lip. In addition, leukoplakic lesions were seen throughout the lower lip, as was blurring of the margin between the vermilion zone and the cutaneous portion of the lip (Fig. 1). After hema-tological evaluation, an incisional biopsy was performed, leading to a histological
diagnosis of actinic cheilosis (Fig. 2). An excisional biopsy confirmed the histologi-cal diagnosis. The patient was encouraged to use lip balm with sunscreen, and to decrease his exposure to the sun, thus preventing further damage; at that time, a follow-up regimen was established. In the 20 months postbiopsy, the patient had 2 recurrences (followed by healing) over a period of 4 months, which were associ-ated with unprotected exposure to the sun (Fig. 3). A third recurrence (6 months after the first) persisted for more than 15 days (Fig. 4). An incisional biopsy led to a histological diagnosis of well-differentiated, superficially invasive SCC (Fig. 5 and 6). Using a wide “V” excision, the tumor was removed from the lip. The resection margins were histologically tumor-free. After SCC was diagnosed, the Fig. 3. The patient 20 months after excisional biopsy. Fig. 4. An indurated chronic focal ulceration that appeared after
the first recurrence.
Fig. 5. Photomicrograph of the lip mucosa, showing moderately differentiated squamous cell carcinoma (SCC) with invasive islands and cords within the connective tissue (H&E, magnification 40X).
Fig. 6. Photomicrograph of SCC in the lower lip, showing cellular and nuclear pleomorphism, as well as hyperchromatic nuclei (H&E, magnification 400X).
patient’s immunosuppressive therapy was modified, and the cyclosporine regimen was replaced with everolimus (1 mg QD). Six months after oncological surgery, the patient remained lesion- and metastasis-free, and was monitored through frequent follow-up visits (Fig. 7).
Discussion
The overall incidence of cancer is 2-4 times greater in transplanted patients compared to the general population, and the inci-dence increases in the years following trans-plantation.10 Immunosuppressive therapy
has been cited in connection with this inci-dence; other risk factors that can increase the incidence include antigenic stimulation from the graft, donor-derived transmission of cancer, and donor-derived transmission of an oncogenic virus.1,2,11
Kidney transplant recipients are at an increased risk for tumors (with or without infectious etiology), and the spectrum of cancer is similar to that seen in human immunodeficiency virus infection, which suggests a healthy immune system is essential for the prevention of cancer.1-3,12
The literature has reported a decreased risk of malignancy prior to transplantation, during dialysis, and in situations where the immunosuppression was interrupted.5,13
In addition to deregulating the immune system, calcineurin inhibitors have direct and indirect carcinogenic actions that contribute considerably to elevate malig-nancy risk. Calcineurin inhibitors inhibit
DNA repair pathways—such as nucleotide excision repair—and have a direct effect on tumor growth and metastasis.8 Another
immunosuppressive drug, azathioprine, has a byproduct (6-thioguanine) that accumulates in the DNA material of the cells, which in turn increases the cells’ photosensitivity to UVA radiation. This increased sensitivity can result in oxidative stress, thus a higher probability of normal cells becoming carcinogenic.14
Immunosuppressive regimens that include mycophenolate mofetil (a guano-sine synthesis inhibitor) and a new class of inhibitors, known as mammalian targets of rapamycin (mTORs)—that include everolimus and sirolimus—actually reduce the risk of cancer compared to calcineurin inhibitors.2,5,8 Limited clinical data are
available concerning these new immuno-suppressive agents; however, in vitro studies have reported the antitumor properties of mTOR inhibitors, which make them useful as anticancer agents for existing tumors (most likely because of their potent anti-angiogenic effect).8,15 Modifying therapeutic
regimens to include these new immunosup-pressive drugs can potentially reduce the risk of new tumors and recurrence.
Studies comparing double- and triple-agent immunosuppressive regimens have found that the level of immunosuppression confers a proportional risk for skin cancer development. Triple-agent immunosup-pressive regimens possess an increased risk compared with double-agent therapy.7
Long-term use of immunosuppres-sive regimens is also associated with an increased risk for cancer; Moloney et al found a peak incidence of skin cancer 8 years after kidney transplantation.16 In
the present case, lip cancer was the first malignant lesion to appear. The patient’s triple-agent immunosuppressive regimen (the same since transplantation) included cyclosporine, which is strongly related to tumor development. Despite reducing the patient’s dosage regimen of immunosup-pressive drugs, lip cancer appeared after 9 years of treatment.
As stated before, the incidence of SCC of the lower lip in kidney transplant patients varies, but can be 65 times greater than the risk among the general population.1,5,9,17-21 It is probable that lip
cancer has similar risk factors to those of skin cancer. The anatomical position of the vermilion of the lower lip—in addition to the transitional epithelium that exists between the lip mucosa and the skin—makes this area vulnerable to a distinct combination of exposures with well-known carcinogenic potential.5
Important etiological factors (such as tobacco and alcohol use, HPVs, and UV radiation) can damage epithelial DNA. In addition, both UVA and UVB are responsible for the breakdown of vitamin A, local immunosuppression, mutagenic changes to the DNA, and mutations in the epithelial p53 tumor-suppressor gene that inhibits apoptosis. Immunosuppressive drugs intensify these effects and jeopardize important DNA repair pathways.8,22
The clinical and histological aspects of SCC of the lower lip are not limited to kidney transplant patients. Nevertheless, patients with NMSC show an increased number of immunohistochemical markers for tumor angiogenesis (that is, microves-sel density and capillary proliferation index) compared to immunocompetent individuals.2,4,7-9 Lip cancer associated
with kidney transplantation occurs at an earlier age compared to the general popu-lation. Lip cancer in the general popula-tion is more prevalent in male Caucasians, and individuals exposed to high doses of solar radiation. The gender difference may be due to the fact that many women wear lipstick, offering them some protec-tion from UV radiaprotec-tion.2,5,11,23
Fig. 7. The patient 6 months after the tumor was removed.
Cancer Screening Early diagnosis of lip cancer preceded by a persistent actinic lesion in a kidney transplant patient
Since the patient in the present case was at high risk for developing lip cancer, he underwent follow-up appointments every 3 months after actinic cheilosis was first diagnosed. At every appointment, the need for sun protection was reinforced. The recurrences were related to the patient’s return to work, which required intense solar exposure, even though the patient was aware that such exposure was contraindicated. The recurrent lip lesions were monitored weekly and an early sign of malignancy—the lesion’s failure to heal—led to an incisional biopsy during the last recurrence.
Conclusion
Due to the high risk of malignancies, kidney transplant patients must undergo routine examinations and long-term fre-quent follow-ups by medical and dental teams. The follow-up in the present case— involving careful examination of the skin and oral regions—made early diagnosis of potentially malignant and malignant lesions possible. Modifying the immuno-suppressive regimen after cancer is diag-nosed (by utilizing sirolimus or everolimus instead of cyclosporine or tacrolimus) may be a safe alternative to reduce the risk of de novo cancer or tumor recurrence.
Author information
Drs. Oliveira and C. Fernandes are doctoral students, Department of Stomatology and Oral Pathology, School of Dentistry, Federal University of Ceara, Fortaleza, Brazil, where
Drs. Alves, Mota, and Sousa are associate professors, and Dr. P. Fernandes is chief of the renal transplant unit.
References
1. Collett D, Mumford L, Banner NR, Neuberger J, Watson C. Comparison of the incidence of malignancy in recip-ients of different types of organ: a UK Registry audit. Am J Transplant. 2010;10(8):1889-1896.
2. Lopez-Pintor RM, Hernandez G, de Arriba L, de Andres A. Lip cancer in renal transplant patients. Oral Oncol. 2011;47(1):68-71.
3. Wisgerhof HC, van der Geest LG, de Fijter JW, et al. Incidence of cancer in kidney-transplant recipients: a long-term cohort study in a single center. Cancer Epi-demiol. 2011;5(2):105-111.
4. Geraud C, Koenen W, Neumayr L, et al. Lip cancer: retrospective analysis of 181 cases. J Dtsch Dermatol Ges. 2012;10(2):121-127.
5. van Leeuwen MT, Grulich AE, McDonald SP, et al. Im-munosuppression and other risk factors for lip cancer after kidney transplantation. Cancer Epidemiol Bio-markers Prev. 2009;18(2):561-569.
6. Jadotte YT, Schwartz RA. Solar cheilosis: an ominous precursor: part I. Diagnostic insights. J Am Acad Der-matol. 2012;66(2):173-184.
7. Zavos G, Karidis NP, Tsourouflis G, et al. Nonmelano-ma skin cancer after renal transplantation: a single-center experience in 1736 transplantations. Int J Dermatol. 2011;50(12):1496-1500.
8. Kuschal C, Thoms KM, Schubert S, et al. Skin cancer in organ transplant recipients: effects of immunosuppres-sive medications on DNA repair. Exp Dermatol. 2012; 21(1):2-6.
9. Basic-Jukic N, Bubic-Filipi L, Prgomet D, et al. Head and neck malignancies in Croatian renal transplant recipients. Bosn J Basic Med Sci. 2010;10(Suppl 1): S37-S39.
10. Engels EA, Pfeiffer RM, Fraumeni JF Jr, et al. Spectrum of cancer risk among US solid organ transplant recipi-ents. JAMA. 2011;306(17):1891-901.
11. Vajdic CM, van Leeuwen MT. Cancer incidence and risk factors after solid organ transplantation. Int J Can-cer. 2009;125(8):1747-1754.
12. Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS com-pared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370(9581):59-67. 13. Vajdic CM, McDonald SP, McCredie MR, et al. Cancer
incidence before and after kidney transplantation. JAMA. 2006;296(23):2823-2831.
14. Hofbauer GF, Attard NR, Harwood CA, et al. Reversal of UVA skin photosensitivity and DNA damage in kid-ney transplant recipients by replacing azathioprine. Am J Transplant. 2012;12(1):218-225.
15. Campistol JM. Minimizing the risk of posttransplant malignancy. Transplant Proc. 2008;40(10 Suppl):S40-S43.
16. Moloney FJ, Comber H, O’Lorcain P, O’Kelly P, Conlon PJ, Murphy GM. A population-based study of skin can-cer incidence and prevalence in renal transplant recipi-ents. Br J Dermatol. 2006;154(3):498-504. 17. Makitie AA, Lundber M, Salmela K, Kyllonen L,
Pukkala E. Head and neck cancer in renal transplant patients in Finland. Acta Otolaringol. 2008;128(11): 1255-1258.
18. Villeneuve PJ, Schaubel DE, Fenton SS, Shepherd FA, Ji-ang Y, Mao Y. Cancer incidence among Canadian kid-ney transplant recipients. Am J Transplant. 2007;7(4): 941-948.
19. Adami J, Gabel H, Lindelof B, et al. Cancer risk follow-ing organ transplantation: a nationwide cohort study in Sweden. Br J Cancer. 2003;89(7):1221-1227. 20. Kyllonen L, Salmela K, Pukkala E. Cancer incidence in
a kidney-transplanted population. Transpl Int. 2000; 13(Suppl 1):394-398.
21. Birkeland SA, Lokkegaard H, Storm HH. Cancer risk in patients on dialysis and after renal transplantation. Lancet. 2000;355(9218):1886-1887.
22. Wood NH, Khammissa R, Meyerov R, Lemmer J, Feller L. Actinic cheilitis: a case report and a review of the literature. Eur J Dent. 2011;5(1):101-106. 23. King GN, Healy CM, Glover MT, et al. Increased
preva-lence of dysplastic and malignant lip lesions in renal-transplant recipients. N Engl J Med. 1995;332(16): 1052-1057.
www.agd.org General Dentistry July/August 2014 e29