Case Report
Braz J Oral Sci.October | December 2012 - Volume 11, Number 4
Florid cement-osseous dysplasia of maxilla
and mandible: a rare clinical case
Chandramani B. More
1, Rajan Shirolkar
2, Chhaya Adalja
2, Mansi N Tailor
31MDS,PhD, Professor and Head, Department of Oral Medicine and Radiology, K.M.Shah Dental College and Hospital, Sumandeep Vidyapeeth, Piparia,
Vadodara, Gujarat state. India
2MDS, Professor, Department of Oral Medicine and Radiology, K.M.Shah Dental College and Hospital, Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat
state. India
3Post graduate student (Part II), Department of Oral Medicine and Radiology, K.M.Shah Dental College and Hospital, Sumandeep Vidyapeeth, Piparia,
Vadodara, Gujarat state. India
Correspondence to:
Chandramani B. More Department of Oral Medicine and Radiology, K.M.Shah Dental College and Hospital, Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat state. India. Phone: +91 9974900278 / +91 9867111478. Fax: +91 2668-245292 E-mail: drchandramanimore@rediffmail.com
Abstract
Cemento-osseous dysplasia is a group of disorders known to originate from periodontal ligament tissues. Florid cemento-osseous dysplasia clearly appears to be a form of bone and/or cementoid tissues restricted to jaw bones. This lesion is usually asymptomatic and is incidentally detected during routine radiographic examination. The diagnosis is made by clinical and radiographic examinations, and biopsy is not necessary. The patient must manifest the typical changes in at least two quadrants. An asymptomatic individual requires only a periodic follow-up to ensure that there is no change in the disease behavior. Surgical management is indicated only for a progressive lesion that produces orofacial disfigurement. This paper presents a rare case of a 60-year-old female who was clinically and radiographically diagnosed as having florid cemento-osseous dysplasia in the maxilla and mandible. Discussion is presented with emphasis on clinical and radiographic manifestations.
Keywords: fibro-osseous lesion, florid cemento-osseous dysplasia, maxilla, mandible.
Introduction
The term florid cement-osseous dysplasia (FLCOD) was first proposed by Melrose et al in 1976 to describe a condition of exuberant multi quadrant masses of cementum and/or bone in both the jaws and in some cases, simple bone cavity like lesions in affected quadrant. This condition has been interpreted as a dysplastic lesion or developmental anomaly arising in tooth bearing areas. The word ‘florid’ was introduced to describe the widespread, extensive manifestations of the disease in the jaws 1.
The World Health Organization (WHO) workshop group on head and neck tumors classified osseous dysplasia into four subtypes based upon the extent and radiographic appearances - Periapical osseous dysplasia in the anterior mandible, Focal osseous dysplasia or Focal cemento-osseous dysplasia (FCOD) in a posterior region of the jaws, Florid osseous dysplasia (FOD) involving many quadrants of the jaws, and Familial gigantiform cementoma 2.Florid-cemento-osseous dysplasia
was a term proposed in the 2nd edition of the WHO “International Histological Classification of Odontogenic Tumors’’ to replace the gigantiform cementoma of the 1st edition 3.
Received for publication: August 09, 2012
FLCOD lesions are usually asymptomatic and detected incidentally during routine radiographic examination2. The
diagnosis of this lesion is based on clinical and radiographic examination, and biopsy is not necessary 4, 5. The patient must
manifest the typical changes in at least two quadrants for the diagnosis of FLCOD. A four quadrant disease may be suggestive of a familial nature.
This article reports the case of a 60-year-old woman presenting FLCOD of the maxilla and mandible. Discussion is presented with emphasis on clinical and radiographic manifestations.
Clinical Case
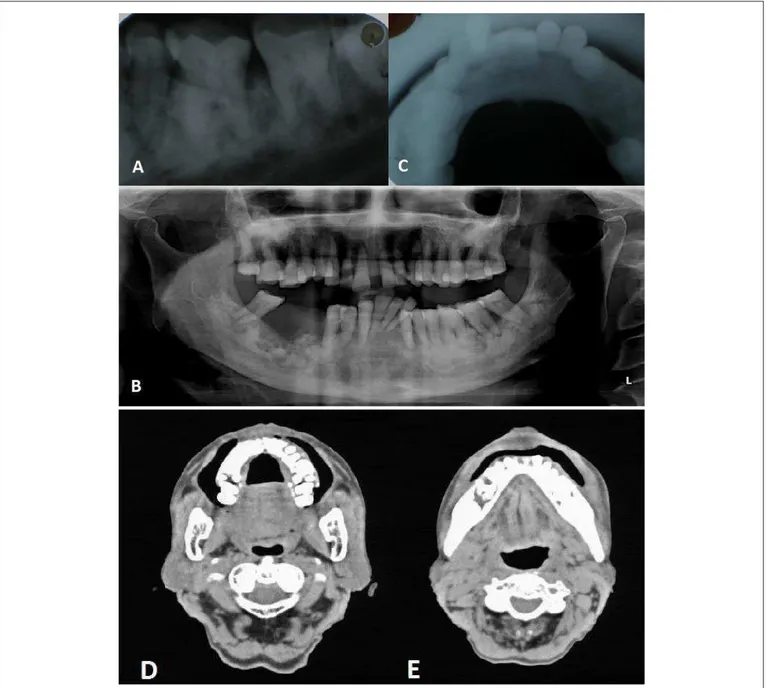
A 60-year-old female patient (Fig.1A) presented to the department of Oral Medicine and Radiology, K. M. Shah Dental College and Hospital, Vadodara, with a complaint of pain of varying intensity at different sites of upper and lower jaw with 5 to 6 months of evolution. The patient was under analgesics prescribed by the local dentist sin then. The dentist extracted the teeth 45, 46 and 47 assuming that they were the culprits for pain. As there was no relief, she was referred to our department for further evaluation. The pain was episodic and dull to severe at different sites of maxilla and mandible. Her medical history was significant only for hypertension, which, according to her, was under control with Amlodipine for the last 10 years. The family history had no significant associations to the dental case. The patient was responsive and well oriented as to time and place. Her vital signs were within normal limits. On extraoral examination, tenderness was noticed from left ramus to right ramus of the mandible and from left to right maxillary bone. The submandibular lymph nodes were enlarged, palpable and tender bilaterally. The intraoral examination revealed presence of all teeth except for 45, 46 and 47. The labial, buccal, palatal and lingual gingiva was firm, fibrotic, hyperplastic, non tender and had generalized pseudo-pockets (Fig 1B and 1C). Also, mild cortical plate expansion was noted throughout the jaws. Crowding was present in the maxillary and mandibular anterior area. Generalized attrition and grade III mobility was present in 31, 32, 33, 34, 35, 36, 37, 38 and 41. All the remaining teeth had grade I mobility. The clinical diagnosis of Drug (Amlodipine) induced gingival enlargement was considered with differential
Fig. 1- A. Extraoral view, B and C: Intraoral views showing gingival enlargement.
diagnosis of Idiopathic gingival enlargement and pseudo gingival enlargement.
On viewing the periapical Fig. 2A) and panoramic (Fig.2B) radiographs, we noted multiple ill defined, varying size radiopaque areas of calcification in the premolar and molar regions of all the four quadrants. In the maxilla, the lesion extended bilaterally, from the distal root of first premolar to the mesial root of third molar. Bilaterally, the lesion extended mesiodistally from the distal root of canine to the anterior surface of mandible ramus. The right mandibular canal appeared to be displaced inferiorly. The radiopaque calcification was more severe in the mandible. The radiopaque lesion had well-defined borders. The bone adjoining the lesion borders was sclerosed at multiple sites with a pseudo-corticated appearance. The radiopaque calcifications appeared like cotton-wool structures. Generalized bone loss was severe in 31, 32, 33, 34, 35, 36, 37, 38 and 41. The cross-sectional mandibular occlusal view (Fig.2C) showed multiple radiopaque foci with minor cortical plate expansion. The plain computed tomography scan of maxilla and mandible (Fig. 2D and 2E) showed bilateral multiple hyperdense areas in the premolar and molar regions. Multiple lobulated calcified masses were symmetrically distributed in the posterior segment of maxilla and mandible.
The routine hematological investigations along with serum calcium and serum alkaline phosphatase levels were within normal limits. In spite of explaining the complications of extraction, patient consistently insisted on the extraction of mobile 36, 37 and 38 with minimal injury to the tissues. These teeth were extracted and biopsy specimens were collected from the extraction sockets.
The histopathological analysis of the specimen showed presence of multiple structures including metaplastic osteoid and cementoid structures in a collagenous spindle-shaped background and plump fibroblasts. A granulation tissue surrounding the lesion showed hemorrhagic areas and neo-vascularization with chronic inflammatory cell infiltration suggestive of FLCOD. Based on the radiographic and histopathological findings, the final diagnosis of FLCOD was made.
Fig. 2- A. Periapical view; B: Panoramic View; C: Occlusal view showing multiple ill-defined, varying size radiopaque areas of calcification in premolar and molar region; D and E: Axial computed tomography scan showing bilateral multiple hyperdense areas in the premolar and molar region.
Discussion
FLCOD is a benign, non-neoplastic and self-limiting jaw lesion. Many authors use several synonyms, such as multiple enostoses, multiple cemento-ossifying fibromas, multiple periapical osteo-fibromatosis, florid osseous dysplasia and gigantiform cementoma. This amalgamates FLCOD with other bone diseases, thereby confounding the literature.WHO classifies FLCOD as a type of fibro-osseous lesion2.
Fibro-osseous lesions are a group of bone disorders in which the normal bone is replaced with fibrous connective tissue containing abnormal bone or cementum. The initial radiographic appearance of this group of lesions is radiolucent. Over time, the lesion evolves to a mixed radiolucent
radiopaque stage before progressing to a completely radiopaque stage. The normal trabecular pattern of bone is not seen in the lesion. Each lesion has its characteristic texture, a fact that can aid in the differential diagnosis6.
The etiology of FLCOD remains unknown. Waldron et al.10 have proposed that reactive or dysplastic changes in the
periodontal ligament might cause the disease.These lesions are characterized by replacement of bone by connective tissue matrix. The matrix displays varying degrees of mineralization in the form of woven bone or cementum-like round basophilic acellular structures. The affected area undergoes changes from vascular bone into cementum-like lesion. The term cemento-osseous dysplasia is a histopathological term, yet the diagnosis can be made by clinical and radiographic findings1. Florid cement-osseous dysplasia of maxilla and mandible: a rare clinical case
Although the disease may be totally asymptomatic, some patients present pain, swelling, purulent discharge and sequestrum formation2,7,8. It can be hypothesized that the
etiological factors such as wearing dentures, tooth extraction make the vascular tissue of the lesion exposed to the oral cavity. Traumatic episodes of this calcified tissue cause retrograde infection and subsequent cellulitis, sequestration or even osteomyelitis2.The hypovascular nature of the disease
increases in severity when infection of the lesion occurs2,8.In
severe cases, mandibular nerve paresthesia and/or jaw expansion, albeit rare, may be found2.
FLCOD is discovered most frequently in the mandible of middle aged females (the mean age being 42 years), although the age range is broad. The condition shows a marked predilection for blacks and Asians2,6-8.Often FLCOD
produces no symptoms and is found incidentally during radiographic examination. Occasionally patient complains of intermittent, poorly localized pain in the affected bone. If the lesions become secondarily infected, features of osteomyelitis may develop, including mucosal ulceration, fistulous tracts with suppuration, sequestrum formation and pain2,7,8.Clinically, it may appear as cortical expansion,
particularly of the mandible. The expansion may be sufficient pronounced to cause the professional to suspect a neoplasm of Paget’s diseases of the bone. Infection may be absent, but dull aching sensation of intermittent nature may be the fundamental feature in the mandibular molar region. Teeth in the involved bone are vital unless other dental disease coincidentally affects them. FLCOD lesions are lobulated masses of dense, lightly mineralized almost acellular cemento-osseous tissue typically occurring in several parts of the jaw
3.FLCOD may have a familial nature, hence familial FLCOD.
In 1953, Agazzi and Belloni1 described an Italian family in
which several members manifested four-quadrant disease that had begun at an early age and resulted in facial disfiguration. Radiographically, FLCOD usually presents as a diffuse distribution of lobular irregularly shaped radiopacities throughout the alveolar process 7. The epicenter is apical to
the teeth, within the alveolar process and usually posterior to the cusp. In the mandible, lesions occur above the alveolar canal. The periphery usually is well defined and has a sclerotic border. The soft tissue capsule may not be apparent in mature lesions. The internal structure can vary from an equal mixture of radiolucent and radiopaque lesions to almost completely radiopaque 8.Its mineralization increases with time and the
same lesion may appear in various stages depending upon the degree of calcification. Immature FLCOD usually presents densely sclerotic lobular or irregular-shaped radiopacities with a radiolucent halo which separates the lesion from the surrounding bone. With maturation, FLCOD involves multiple sites throughout the jaw. Occasionally, a radiopaque lesion blends with the adjacent bone 2.Some prominent
radiolucent lesions may be present, which usually represent the development of a simple bone cyst. The radiopaque lesions can vary from small oval and circular regions (cotton-wool appearance) to large, irregular, amorphous areas of calcification7,8.Large FLCOD lesions can displace the inferior
alveolar nerve canal in an inferior direction. The lesion can also displace the floor of the maxillary antrum in a superior direction and can cause enlargement of the alveolar bone by displacement of the buccal and lingual cortical plates. The roots of associated teeth may have a considerable amount of hypercementosis, which may fuse with the abnormal surrounding cemental tissue of the lesion. Extraction of these teeth may be difficult 8.These variable features of FLCOD
militate against the diagnosis of fibrous dysplasia, cemento-ossifying fibroma and to a lesser extent, Paget’s disease of the bone.
A solitary bone cyst (traumatic bone cavity) coexists in some FLCOD cases. A possible explanation for this occurrence may be that the fibro-osseous proliferation obstructs the interstitial fluid drainage, resulting in cystic degeneration within the FLCOD lesion. This collision phenomenon necessitates surgical exploration and histopathological examination to establish a definite diagnosis. In a patient without solitary bone cyst formation, the diagnosis of FLCOD is clinical or radiographic. Biopsy is not necessary. A patient must manifest the typical changes in at least two quadrants for a clinical diagnosis of FLCOD to be made. Malignant fibrous histiocytoma developing in FLCOD was also reported in one patient, but the prognosis was good 2.
Histopathologically the tissue consists of fragments of cellular mesenchymal tissue composed of spindle-shaped fibroblasts and collagen fibers with numerous small vessels. Free hemorrhage is typically noted interspersed throughout the lesion. Within this fibrous connective tissue background is a mixture of woven bone, lamellar bone and cementum-like particles. The proportion of each mineralized material varies from lesion to lesion and from area to area in the individual site of involvement. As the lesion matures and become more sclerotic, the ratio of fibrous connective tissue to mineralized material decreases. With maturation, the bone trabeculae become thick, curvilinear structures that have been said to resemble the shape of ginger roots. With progression to the final radiopaque stage, the individual trabeculae fuse and form lobular masses composed of sheets or fused globules of relatively acellular and disorganized cemento-osseous material2, 9.
When the diagnosis of FLCOD is suspected, an incisional biopsy and/or elective tooth extraction in the unaffected (asymptomatic) area of the lesion is best avoided because they may cause acute (and possibly serious) infection in that region 7. Hence, complete surgical removal of the entire
disease, which may cause discontinuity of the jaw, is absolutely unnecessary. An asymptomatic individual requires only a periodic follow-up to ensure that there is no change in the disease behavior2,4,8. Surgical management is indicated
only for a progressive lesion that produces orofacial disfigurement. It is not normally justified to surgically remove these lesions as this often requires extensive surgery. Since the tissue diffusion of the lesion is poor, antibiotic treatment may be ineffective for an infected lesion2.
The main differential diagnoses for FLCOD are chronic diffuse sclerosing osteomyelitis (CDSO), periapical cemental dysplasia, fibrous dysplasia and Paget’s disease of bone (PD)
2, 7, 8. CDSO usually produces signs and symptoms of infection
and it is usually limited in extent, whereas FLCOD is usually asymptomatic and affects at least two or more quadrants of the jaw. In Periapical cemental dysplasia lesion will always be associated with root of mandibular anterior teeth whereas in FLCOD lesions are not contacting the teeth. Fibrous dysplasia is common in children and FLCOD is more common in adults. PD is often a polyostotic lesion involving several bones of the body apart from the jaw and produces biochemical changes such as elevated alkaline phosphatase 2.
An accurate differential diagnosis is important. Notable, progressive bone atrophy under a denture can also create significant clinical problems due to exposure of the lesion. Good oral care to prevent tooth loss and denture maintenance is therefore, pivotal 2.
In conclusion, FLCOD is a benign, non-neoplastic and self-limiting jaw lesion and discovered most frequently in the mandible of middle aged females. This lesion is usually asymptomatic and detected incidentally during routine radiographic examination. It affects at least two or more quadrants of the jaws. The diagnosis is made by clinical and radiographic examination, and biopsy is not necessary. An asymptomatic individual requires only a periodic follow-up of the treatment. Surgical management is indicated only for a progressive lesion that produces orofacial disfigurement.
Acknowledgements
The authors are thankful to Dr. J. R. Patel, Faculty Dean, Sumandeep Vidyapeeth University, Pipariya, Vadodara for his constant support and encouragement for preparing this clinical case.
References
1. Mangala M., Ramesh DN, Surekha PS, Santosh P. Florid cemento-osseous dysplasia : Review and report of two cases; IJDR 2006, volume 17, issue 3, page 131-134.
2. Pitak-Arnnop P., Dhanuthai K., Chaine A., Bertrand J., Bertolus C. Florid osseous dysplasia: Report of a case presenting acute cellulitis; Med Oral Pathol Oral Cir Bucal. 2009 Sep 1;14 (9):e461-4.
3. C Ogunsalu, D Miles. Cemento-osseous Dysplasia in Jamaica. Review of Six Cases; West Indian Med J 2005; 54 (4): 264-267
4. Dagistan S., Tozoðlu U., Göregen M., Çakur B. Florid cemento-osseous dysplasia: A case report; Med Oral Pathol Oral Cir Bucal 2007;12: E348-50. 5. Mupparapu M., Singer S., Milles M., Rinaggio J. Simultaneous presentation of focal cemento-osseous dysplasia and simple bone cyst of the mandible masquerading as a multilocular radiolucency; Dentomaxillofacial Radiology. 2005; 34: 39-43.
6. Singer S., Mupparapu M., Rinaggio J. Florid cemento-osseous dysplasia and chronic diffuse osteomyelitis: report of a simultaneous presentation and review of the literature; J Am Dent Assoc 2005;136;927-931
7. Wood N., Goaz P. Differential Diagnosis of Oral and Maxillofacial Lesions. Fifth Edition; Page 509-511, 515-517.
8. White S., Pharoh M. Oral Radiology Principles of interpretation. Fifth Edition. Page 495-498.
9. Neville B., Damm D., Allen C., Bouquot J. Oral and maxillofacial pathology; 2nd Edition:558-561.
10. Waldron CA. Fibro-osseous lesions of the jaw. J Oral Maxillofac Surg 1993; 51: 828-835.
Florid cement-osseous dysplasia of maxilla and mandible: a rare clinical case