ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Use
of
pamidronate
for
osteoporosis
treatment
in
public
health
care
in
Brazil
Leila
Bianchet
Zanatta
a,
Cristina
Marcatto
a,
Cassio
Slompo
Ramos
a,
Nadila
Ma ˜nas
a,
Carolina
Moreira
a,b,
Victoria
Borba
a,b,∗aUniversidadeFederaldoParaná,HospitaldeClínicas,Servic¸odeEndocrinologiaeMetabologia,Curitiba,PR,Brazil
bUniversidadeFederaldoParaná,DepartamentodeMedicinaInterna,DivisãodeEndocrinologia,Curitiba,PR,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received26August2015 Accepted1May2016 Availableonline29July2016
Keywords: Pamidronate Bonemineraldensity Osteoporosis
a
b
s
t
r
a
c
t
Purpose:Theuseofbisphosphonatesforosteoporosisiseffectiveinreducingtheriskof fractures.However,oralformulationsaresometimesnotwelltoleratedorare contraindi-cated.DuetoitsavailabilityinBrazilianpublichealthsystem,pamidronateisfrequently prescribedforosteoporosis,despitethelackofstudiesdemonstratingitsanti-fracture effi-cacyandtheabsenceofFDAorEMEAapprovalforthispurpose.Theaimofthisstudywas toevaluatethebonemineraldensity(BMD)responsetopamidronateinagroupofwomen withosteoporosisinatertiarycarehospital.
Patients and methods:The medical records of women with osteoporosis who received pamidronateforuptotwoyearsoftreatmentwerereviewed.Patientswerestratifiedat highorintermediateriskoffracture.
Results:Atotalof70womenwereintreatmentwithpamidronate.Amongthem,74%were athighriskoffracture.AsignificantgaininspineBMDafter24monthsoftreatmentwas observed(p=0.012).Therewasnodifferencebetweenthegroupsofhighandnothighriskof fracture.Atthefemur,nosignificantincreaseinBMDwaspresent,though,astrongnegative correlationwithhighPTHlevels(r=−0.61;p=0.003)wasseen.Inthemultivariateanalysis
BMIat12monthshadimpactintheresponsetothetreatment.
Conclusion:Theintravenouspamidronateinagroupofpostmenopausalwomenwith pre-dominanthighriskoffracturepromotedanisolatedgaininthespineBMD,eventhough, clinicalrandomizedtrialsareneededtoconfirmitsanti-fractureefficacy.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗ Correspondingauthor.
E-mail:vzcborba@gmail.com(V.Borba).
http://dx.doi.org/10.1016/j.rbre.2016.07.005
Uso
de
pamidronato
para
o
tratamento
da
osteoporose
no
sistema
público
de
saúde
no
Brasil
Palavras-chave: Pamidronato
Densidademineralóssea Osteoporose
r
e
s
u
m
o
Justificativa: Ousodebisfosfonatosparaaosteoporoseéeficaznareduc¸ãodorisco de fraturas.Noentanto,asformulac¸õesoraisàsvezesnãosãobemtoleradasousão con-traindicadas.Emrazãodasuadisponibilidadenosistemapúblicodesaúdebrasileiro,o pamidronatoéfrequentementeprescritoparaaosteoporose,apesardafaltadeestudos quedemonstremasuaeficáciaantifraturaedaausênciadeaprovac¸ãodaFoodandDrug Administration(FDA)oudaEuropeanMedicineAgency(Emea)paraessafinalidade.Oobjetivo desteestudofoiavaliararespostadadensidademineralóssea(DMO)aopamidronatoem umgrupodemulherescomosteoporoseemumhospitalterciário.
Pacientesemétodos:Revisaram-seosprontuáriosmédicosdemulherescomosteoporoseque receberampamidronatoporatédoisanosdetratamento.Aspacientesforamestratificadas emriscoaltoouintermediáriodefratura.
Resultados: Estavamemtratamentocompamidronato70mulheres.Entreelas,74%tinham altoriscodefratura.Observou-seumganhosignificativonaDMOdacolunavertebralapós 24mesesdetratamento(p=0,012).Nãohouvediferenc¸aentreosgruposderiscodefratura altoenãoalto.Nofêmur,nãofoiencontradoaumentosignificativonamassaóssea;contudo, observou-seumafortecorrelac¸ãonegativacomaltosníveisdePTH(r=-0,61;p=0,003).Na análisemultivariada,oIMCaos12mesesteveimpactonarespostaaotratamento. Conclusão: Opamidronatointravenosoemumgrupodemulheresnapós-menopausa pre-dominantementecomaltoriscodefraturapromoveuumganhoisoladonaDMOdacoluna vertebral,emborasejamnecessáriosensaiosclínicosrandomizadosparaconfirmar sua eficáciaantifratura.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Bisphosphonatesrepresentthemajordrugsinthe therapeu-ticarsenalofosteoporosis.Theyarepowerfulanti-resorptive agents, deposited in mineral bone, and their diversity in actionandanti-fractureefficacymaybeclinicallywarranted dependingonthestrengthofconnectionanddetachmentto thebonetissue.1Amongthefourbisphosphonatesapproved forosteoporosistreatment,basedondouble-blind random-izedcontrolledtrials,zoledronatehasthegreatestaffinityfor bone,followedrespectivelybyalendronate,ibandronate,and risedronate.2
Pamidronateisanitrogen-containingbisphosphonatewith anintermediarypotencytoinhibitbonereabsorption,andit wasinitiallyindicatedforpreventingbonemetastasisgrowth indifferenttypesofcancer.1,3Theefficacyofpamidronatehas beendemonstratedinthetreatmentoflyticbonemetastasis; tocontrolhypercalcemiaofmalignancyinmultiplemyeloma; inthepreventionofosteoporosisinducedbyglucocorticoids orsecondarytochemotherapyorimmunosuppressivedrugs aftersolidorganandstemcelltransplantation.4–13
Thepamidronatehasbeenextensiblyusedsince1991and becamestandardizedbythepublichealthagencyfor osteo-porosis treatment. It started to be widely used due to its availabilityinthepublichealthcaresystemandthelackof otherformallyapprovedparenteralanti-resorptivedrugsfor osteoporosistreatmentatthattime.Itisimportanttonote that this is the only non-oral medication for osteoporosis treatmentavailableinourpublichealthcaresystem.However,
pamidronatehasneverbeenapprovedforosteoporosis treat-mentand,despiteitsfrequentuseindailypracticeformany patientswithintolerancetooralbisphosphonates, prospec-tivestudiesarelackinginevidencetosupportpamidronate’s anti-fractureefficacy.
Objectives
Primary
Theaimofthisstudyistoevaluatethetherapeuticresponse topamidronateintheBMDgainofspineandtotalfemur,ina groupofpostmenopausalwomenwithosteoporosis,followed inanosteoporosisoutpatientclinicforatreatmentperiodof upto36months.
Secondary
Toevaluatetheinfluenceofclinicalaspectssuchasage, frac-turerisk,anddoseofpamidronateadministeredperyearon theresponsetothetreatment.
Methods
Studydesignandpatients
A retrospective study was conducted with patients on treatment for osteoporosis with intravenous pamidronate. ThestudywasapprovedbytheEthicsCommitteeonHuman ResearchoftheHC–UFPR.
Patients
AllpatientstreatedwithpamidronatefromOctober2006to October 2010 were initially included. The vast majority of patientshadbeendiagnosedwithpostmenopausal osteoporo-sis,followedbyglucocorticoid-inducedosteoporosis.Patients withsecondaryosteoporosisduetomalabsorptivesyndromes, gastrointestinalsurgery,prolongedimmobilization,and intol-erance to oral bisphosphonates were also included. The exclusion criteria were males and patients with any dis-easethatcouldinterferewithboneorcalciumorvitaminD metabolism,aswellasthosewithmalignancies.
In Brazil, any algorithm is available to classify osteo-porosis patientsbythe severity ofriskfactors forfracture. Patientswereclassifiedashavinghighandintermediate frac-tureriskbasedonknownclinicaldata,todate,thevalueof BMDTscore,ownor familyhistory ofapastfragility frac-ture, and risk factors for osteoporosis suchas menopause orprematureovarianfailure,smoking,rheumatoidarthritis, chronicuseofglucocorticoidsorimmunosuppressivedrugs, lowweight,malabsorptivesyndromes,prolonged immobiliza-tion,andfamilyhistoryofosteoporosis.14
ConsideringthatFraxalgorithmisnotrecommendedfor patientspreviouslytreated,15 wecharacterizedpatients tak-ing into accounttraditional riskfactors. Highriskpatients were:olderthan75years;ownorfamilyhistoryofvertebralor femoralfracture;olderthan65yearswiththreeormorerisk factorsforosteoporosisorwithaTscore<−3.0SD.
Intheintermediateriskgroupwerethosepatientsyounger than75yearswithtworiskfactorsandnomajorosteoporotic fracture,orwithaTscore<−3.0SDand lessthan tworisk
factors;thoseyoungerthan65yearswithoutriskfactorswith oralintolerancetobisphosphonates,whereastheTscorewas >−3.0SDorwithosteopeniaandoneriskfactor.
Protocol
Asaretrospectivestudy,theauthorsdidnotinterferewith the decision to use the medication and were not respon-sibleforthe careofpatients. Patientsreceived intravenous pamidronateinfusion,atatotaldoseof90mgdilutedin500ml ofsalineor5%dextrosesolution,foraperiodoffourhours, everysixmonths,accordingtotheroutineprotocoloftheBone MetabolismUnit.AllpatientswerevitaminD3sufficientatthe timeofthefirstinfusionandweresupplementedwith vita-minDandwithcalcium iftheirintakewasbelowthedaily needs.
BMDassessment
BMDatthelumbarspine(L1–L4)andtotalfemurwas mea-suredat0,12,24,and36monthsoftreatmentbyDXA,GE LunarProdigyAdvancePA+302284(GEMedicalSystems, Madi-son, WI) witha coefficient of variability of0.010g/cm2 for lumbar spine and 0.012g/cm2 for proximal femur and by
Hologic QDR– 1000W (Hologic,Inc.,Waltham, MA), witha coefficientofvariabilityof0.046g/cm2forlumbarspineand 0.052g/cm2forproximalfemur.Theevaluationofeachpatient was performed, considering only the results of the same equipment.
Medicalrecordsevaluation
Themedicalrecordswerereviewedinsearchofinformation regardinggender;ownorfamilyhistoryofapastfragility frac-ture and riskfactors forosteoporosis, such as menopause or premature ovarian failure, smoking, rheumatoid arthri-tis, chronic use of glucocorticoids or immunosuppressive drugs, low weight, malabsorptive syndromes, or prolonged immobilization. The results of creatinine (Picrato Alcaline method, reference 0.57–1.11mg/dL), parathyroidhormone– PTH (Quimioluminescence method, reference 12–68pg/ml) andcalcium(ArsenazzoIIImethod,reference8.5–10.5mg/dL), both usingARCHITECT ci8200®,Abbott; 25(OH)vitaminD3 (Quimioluminescence method – LIAISON®, DiaSorin, refer-ence 30–100ng/mL) ofthe first timeofinfusionand ofthe subsequentvisits,whenavailable,werecaptured.
Statisticalanalysis
A descriptiveanalysiswas performedand the resultswere describedasmean,median,minimum,maximumvalues,and standard deviations. Student’s t test was used to evaluate thegaininBMDbetweentwoparticularmomentsforpaired samples.Tocomparethetwodifferentgroups(highand inter-mediate)betweentwoparticulartimepoints,theStudent’st testwasperformedforindependentsamples.
In order to quantify the association between two variables–gaininBMDbetweentwoparticularmomentsand thedeterminantconditionsofthisvariation,weestimatedthe Pearsoncorrelationcoefficient,havinginvestigatedthe follow-ingvariables:totalpamidronatedoseperyear,age,BMI,and PTH.TheFisherexacttestassessedtheassociationbetween twodichotomousqualitativevariables.
Topredictthevalueofmultiplevariablestotheresponsein BMDgain,ananalysisofMultipleLinearRegressionwasdone. Weappliedthelogisticregressionmodeltoassessthe asso-ciation betweentheexplanatory variablesandlikelihoodof treatmentresponse(characterizedasgainorstabilityofBMD atthetime).TheWaldtestwasusedtoevaluatethe hypoth-esisofinterestontheexplanatoryvariables.Theresultswere expressed as mean or median for parametric or nonpara-metric data respectively and p value<0.05 was considered statisticallysignificant.DatawereanalyzedwiththeStatistica v.8.0software.
Results
intolerance;thedataofthesesixpatientswerenotincluded intheanalysis.Thetotalnumberofpatientswhoshowedno exclusioncriteriaandwhocompletedthestudywas74.Ofthis total,49patientshadBMDevaluationinthefirstyearof treat-ment,21inthesecondyear,andonly18inthethirdyearof treatment.Thedataof70patientswhohadBMDinthefirst twoyearsoftreatmentwereanalyzed.
Duringthetreatment,asignificantlossoftrackingofthe patientsaswell asagreater interval betweenthedoses of medication was observed. The mean dose decreased from 213mgperyearinthefirst12monthsto167mgperyearover thenext24monthsandto150mgperyearafter36monthsof follow-up.
Clinical,laboratory,anddemographicdata
Atotalof70womenwithameanageof68yearsold,most ofwhom(93%)wereCaucasianand49(70%)athighriskof fracture,wereevaluated.ThemeanBMIwas25.9kg/m2,the meanserum PTH was50.78(18–102)pg/mL,andthe serum calcium was 9.4(8.4–10.4)mg/dL, withinthe normalrange. Amongthe group withhigh risk offracture, 40 (80%) had afractureinthepast, whileintheintermediateriskgroup only6(30%)hadapasthistoryoffracture. Thereweretwo femoralfracturesduringthe treatment,considered a treat-mentfailure,andpamidronatewassubstitutedbyteriparatide atthe12-and24-monthtimeperiod,respectively.The clini-calcharacteristicsaresummarizedinTable1.Renalfunction, assessedbyGlomerularFiltrationRate(MDRDstudyequation) betweentheperiodsofpamidronateapplicationwerenormal. Duetologisticreasons,renalfunctionwasnotassessed rou-tinelyimmediatelyafterinfusionofpamidronate,butbefore thenextinfusion.
Table1–Demographicandclinicalcharacteristicsof patients.
Totalnumber 70
Age(years)Mean 68.9(50–89)
BMI(kg/m2)Mean 25.9(15–42)
Ethnicity
White 65(92.85%)
Black 1(1.40%)
Mulatto 4(5.75%)
Risk
High 49(70%)
Non-high 21(30%)
Fracture
Vertebral 13(18.57%)
Femur 12(17.14%)
Non-vertebral 21(30%)
PTHMean 50.78(18–102)
Calcium(mg/dL)Mean 9.42(8.4–10.4)
GRFMean 77.82(35.1–168.8)
25OHDMean 33.88(12.8–76.8)
Calcium,(reference8.5–10.5);PTH,Parathyroidhormonepg/mL
(ref-erence12–68);GRF,GlomerularFiltrationRatemg/dL(MDRDstudy
equation);25OHD, 25(OH) Vitamin D3 (reference 30–100ng/mL);
BMI,bodymassindex.
EvaluationoftheeffectofthetreatmentonBMDincrement
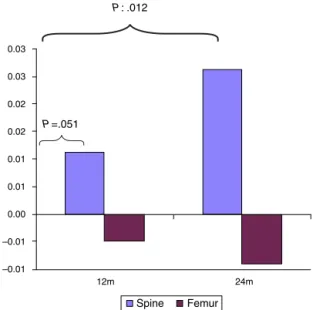
TheanalysisofBMDatthe spineat0,12,and24 months, byStudent’sttest,showedasignificantgain:anaverageof 0.024g/cm2(p=0.012)after24monthsoftreatmentanda
ten-dency(p=0.051)inthefirst12months.Nosignificantchange inBMDatthefemurwasobservedatthedifferenttimepoints (Fig.1).
Theinfluenceofage,PTH,fracturerisk,andannualdose
ofpamidronateontheBMDchange
Inthespine,thelinearassociationanalysisdidnotshowany correlationbetweentheBMDgainwithage,PTH,pastuseof bisphosphonates and thesubgroupsoffracture riskin any timepointofevaluation,however,theBMIhadaweak pos-itive associationwiththeBMDgain at12 months(p=0.046 andr=0.29).
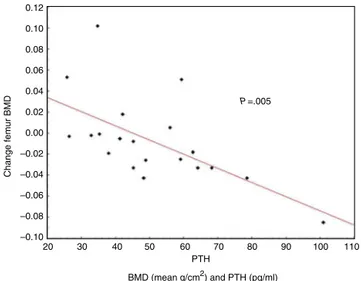
TheBMDgaininfemurshowedanegativeassociationwith PTHvaluesat24months(p=0.003andr=−0.61)(Fig.2)and
withBMIat36months(p=0.002andr=−0.78).
Themultivariate analysisoftheBMD gaininspine and femur in each time point, as a dependent variable, and age,PTH,fracturerisk,andtheannualdoseofpamidronate (consideringthereductionofthedoseperyearaccordingto thetimeoftreatment)asindependentvariables,revealedthat therewasnoevidenceofassociationbetweenthe explana-tory variables and the BMDgain inspine or femur in the first12monthsoftreatment.Nevertheless,at24months,a negativeassociationwasfoundbetweenthegaininfemoral BMDandthethreevariables:age,doseofpamidronateand PTH(p=0.002).WhencontrollingeitherforPTHanddoseof pamidronateorforageandPTH,nosignificancewasfound (p=0.220andp=0.788,respectively).However,controllingfor age and dose of pamidronate, a negative correlation was observedbetweenthePTHlevelsandfemoralBMDchanges (p=0.005).Thus,itwasestimatedthatforeveryincreaseof 1pg/mlinPTHlevels,therewasadecreaseof0.0015g/cm2in
–0.01
12m P: .012
P=.051
24m –0.01
0.00 0.01 0.01 0.02 0.02 0.03 0.03
Spine Femur
0.1500
0 20 40 60
PTH
BMD (mean g/cm2) and PTH (pg/ml)
Femur BMD
r=–0.61 P=.003
80 100 120
0.1000
0.0500
0.0000
–0.0500
–0.1000
Fig.2–CorrelationofthechangeinPTHlevelsandfemur BMDafter24monthsoftreatmentbyPearsoncorrelation coefficient.
0.12
0.10
0.08
0.04
0.00
–0.02
–0.04
–0.06
–0.08
–0.10
60 50 40 30 20
PTH
P=.005
BMD (mean g/cm2) and PTH (pg/ml)
Change femur BMD
90 80
70 100 110
0.02 0.06
Fig.3–PTHlevelsandfemurBMDchangeafter24months oftreatmentbyMultipleLinearRegression(Controlledfor ageanddoseofpamidronate).
theBMDoffemur;33.1%ofthefemoralBMDgainat24months wereexplainedbyage,PTHanddoseofpamidronate(Fig.3).
The multivariable analysis of the positive treatment response (defined as gain or stability of BMD in time), controlled for age, PTH, fracture risk, BMI and dose of pamidronate,demonstratedanassociationofBMIwitha pos-itiveresponseinfemur(p=0.043).Itwasestimatedthatfor eachincreaseinoneunitofBMI(kg/m2)thepatientwas1.25 timesmorelikelytorespondtotreatment–OR:1.25(1.0–1.55) (Table2).InthespineBMD,controllingforthesamevariables, onlyatrendofassociationwasobservedbetweenthepositive responsetotreatmentandthehighestadministereddoseof pamidronateperyear(p=0.052).
Discussion
ThisretrospectivestudyevaluatingtheBMDresponseto intra-venouspamidronateinagroupofpostmenopausalwomen showedan increaseinspine BMDonlyafter24 monthsof
Table2–Multivariableanalysisoftreatmentresponsein femurcontrolledforthemainvariablesat12months.
Variable pValue Oddsratio 95%C.I.
Age 0.36 1.05 0.94–1.17
PTH 0.625 1.01 0.97–1.05
Riskestratification 0.065 0.15 0.02–1.20
BMI(kg/m2) 0.043 1.25 1.00–1.55
Pamidronatedose
(mg/12months)
0.279 1.01 0.99–1.02
Pamidronatedosewasconsideredthereductionofthedoseperyear
accordingtothetimeoftreatment.
CI,confidenceinterval;Treatmentresponse,BMDgain/stability
ver-susBMDloss;BMI,bodymassindex.
treatment,unlikeotherstudiesshowingapositiveresponse after12monthsoftreatment.16–19 Inaddition,therewasno change in femoralBMD, explainedby the heterogeneityof etiologyoftheosteoporosisinthisgroup,short(24months) follow-up, and lower BMD speed gain at this site, which couldnotbeconsideredatreatmentfailure.20–22Butwemust emphasizethatwhenwestratifiedthewomenaccordingto twosubgroupsoftreatmentresponse(respondersand non-responders),themaindeterminantforthefemoralBMDgain wastheBMI.
Despitethelackofstudiesdemonstratingtheefficacyof pamidronateinreducingtheriskofvertebralornon-vertebral fractures,thismedicationhasbeenlongusedforthe treat-mentofdiseaseswithincreasedboneturnover.5–13
Regardless the exclusion of patients withthe diagnosis ofprimary hyperparathyroidism, theprevious treatmentof vitaminDdeficiencybeforepamidronateinfusionandthe rec-ommended supplementationofcholecalciferoland calcium accordingtothelocalprotocol,westillobservedanelevated PTH level in a subgroup of patients. Vitamin D deficiency during the two years oftreatment could not be excluded. This reality reflectsthe majority ofpatientstreated inour institution, withlow socioeconomicstatus, lowcapacityto understand the treatment, and low attendance atmedical visits.Otherpossibilitiesarethelowcomplianceofvitamin Duse,notavailableforfreeinahealthypublicsystem,orthe useofpharmaceuticalformulationswithoutreliablequality.
Asshown inthis study,bystatistical modelsof univari-ate and multivariate analysis, PTH levels were correlated with lower gain in femoral BMD, richin cortical bone, an observation already seen in either primary or secondary hyperparathyroidism.23–26
Thetimeoftreatmentexpectedformaximumanti-fracture efficacy and BMD gain is well establishedfor alendronate, butlittleisknownaboutpamidronate.20–22 Inthisstudywe observedabenefitinspineBMDafter24months. Unfortu-nately,thisstudydidnotallowananalysisofthefracturerisk reduction.
healthsystem patients. Thedemonstrated effectivenessof themedications bystudies underoptimalconditions, does nottranslatetothereallifeofourpatients.Thelong-term difficultyinmaintainingtreatment, aswellasthe required treatmentadherence,couldimpairtheresultsofthis thera-peuticregimen.
Numerouslimitationswereobserved,sincethiswasareal life,cross-sectionalstudyandnotadouble-blindrandomized controlledtrial.Thegroupthatreceivedpamidronatewasnot homogeneous,hadahighriskoffracture,lostinfusions,and possiblyhad aconcomitantvitamin Ddeficiency. However, theimportanceofthisstudywasnotlost,becauseitreflects therealityseeninpatientswithpoorsocioeconomicstatus andlowattendanceatmedicalvisits.Rather,itexposesa crit-icalview thatunderthesetreatmentconditions(eitherthe patientortheinfrastructureavailable)wewillnotgeta favor-ableresultaspresentedinotherstudies.16–19Moreover,asthe pamidronateisnotyetanapprovedmedicationfor osteoporo-sistreatmentandhasgreatadherenceconcerns,ourhealth caresystemshouldreviewitsstandardizationforthispurpose.
Conclusion
Our study demonstrated that the use of intravenous pamidronateincreasedspineBMDafter24monthsof treat-ment. No response was observed in femoral BMD. This population reflects the majority ofpatients treated inour service, and maybe in other tertiary care hospitalsin our country.Pamidronateisnotanapprovedmedicationfor osteo-porosis treatment; however, it is the only non-oraloption availableinourpublichealthsystemforpatientswho have osteoporosisandcontraindicationstooralbisphosphonates.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. RusselRGG,WattsNB,EbetinoFH,RogersMJ.Mechanismsof actionofbisphosphonates:similaritiesanddifferencesand theirpotentialinfluenceonclinicalefficacy.OsteoporosInt. 2008;19:733–59.
2. WattsNB,DiabDL.Long-termuseofbisphosphonatesin osteoporosis.JClinEndocrinolMetab.2010;95(4):1555–65.
3. RogersMJ,FrithJC,LuckmanSP,CoxonFP,BenfordHL, MonkkoneyJ,etal.Molecularmechanismsofactionof bisphosphonates.Bone.1999;24:73S–9S.
4. BoutsenY,JamartJ,EsselinckxW,DevogelaerJP.Primary preventionofglucocorticoid-inducedosteoporosiswith intravenouspamidronateandcalcium:aprospective controlled1-yearstudycomparingasingleinfusion,an infusiongivenonceevery3months,andcalciumalone.J BoneMinerRes.2001;16:104–12.
5. FuleihanGE,SalamounM,MouradYA,ChehalA,SalemZ, MahfoudZ,etal.Pamidronateinthepreventionof
chemotherapy-inducedbonelossinpremenopausalwomen withbreastcancer:arandomizedcontrolledtrial.JClin EndocrinolMetab.2005;90:3209–14.
6.ShaneE,RodinoMA,McMahonDJ,AdessoV,StaronRB,Seibel MJ,etal.Preventionofbonelossafterhearttransplantation withantiresorptivetherapy:apilotstudy.JHeartLung Transplant.1998;17:1089–96.
7.ReevesHL,FrancisRM,ManasDM,HudsonM,DayCP. Intravenousbisphosphonatepreventsosteoporoticvertebral collapseinpatientsafterlivertransplantation.Liver TransplantSurg.1998;4:404–9.
8.CocoM,GlicklichD,FaugereMC,BurrisL,BognarI,DurkinP, etal.Preventionofbonelossinrenaltransplantrecipients:a prospective,randomizedtrialofintravenouspamidronate.J AmSocNephrol.2003;14:2669–76.
9.BuchsN,HelgC,CollaoC,ChapuisB,SlosmanD,BonjourJP, etal.Allogeneicbonemarrowtransplantationisassociated withapreferentialfemoralneckboneloss.OsteoporosInt. 2001;12:880–6.
10.KananenK,VolinL,LaitinenK,AlfthanH,RuutuT,Välimäki MJ.Preventionofbonelossafterallogeneicstemcell transplantationbycalcium,vitaminD,andsexhormone replacementwithorwithoutpamidronate.JClinEndocrinol Metab.2005;90:3877–85.
11.GriggAP,ShuttleworthP,ReynoldsJ,SchwarerAP,SzerJ, BradstockK,etal.Pamidronatereducesbonelossafter allogeneicstemcelltransplantation.JClinEndocrinolMetab. 2006;91(10):3835–43.
12.KimS,ChoBS.Pamidronatetherapyforpreventing steroid-inducedosteoporosisinchildrenwithnephropathy. NephronClinPract.2006;102:c81–7.
13.AcottPD,WongJA,LangBA,CrockerJF.Pamidronate treatmentofpediatricfracturepatientsonchronicsteroid therapy.PediatrNephrol.2005;20:368–73.
14.DomicianoDS,MachadoLG,LopesJB,FigueiredoCP,Caparbo VF,TakayamaL,etal.Incidenceandriskfactorsfor
osteoporoticvertebralfractureinlow-income
community-dwellingelderly:apopulation-basedprospective cohortstudyinBrazil?OsteoporosInt.2014;25(12):2805–15.
15.KanisJA,JohnellO,OdenA,JonssonB,DawsonA,DereW.Risk ofhipfracturederivedfromrelativerisks:ananalysisapplied tothepopulationofSweden.OsteoporInt.2000;11:120–7.
16.ReidIR,WattieDJ,EvansMC,GambleGD,StapletonJP, CornishJ.Continuoustherapywithpamidronate,apotent bisphosphonate,inpostmenopausalosteoporosis.JClin EndocrinolMetab.1994;79:1595–9.
17.VisM,BultinkIEM,DijkmansBAC,LemsWF.Theeffectof intravenouspamidronateversusoralalendronateonbone mineraldensityinpatientswithosteoporosis.OsteoporosInt. 2005;6(11):1432–5.
18.CauzaE,EtemadM,WinklerF,Hanusch-EnsererH,PartschG, NoskeH,etal.Pamidronateincreasesbonemineraldensity inwomenwithpostmenopausalorsteroid-induced osteoporosis.JClinPharmTherapeut.2004;29:431–6.
19.PeretzA,BodyJJ,DumonJC,RozenbergS,HotimskiA,PraetJP, etal.Cyclicalpamidronateinfusionsinpostmenopausal osteoporosis.Maturitas.1996;25:69–75.
20.MacLeanC,AlexanderA,CarterJ,ChenS,DesaiSB,Grossman J,etal.Systematicreview:comparativeeffectivenessof treatmentstopreventfracturesinmenandwomenwithlow bonedensityorosteoporosis.AnnInternMed.
2008;148:197–213.
21.BoneHG,HoskingD,DevogelaerJP,TucciJR,EmkeyRD, ToninoRP,etal.Tenyears’experiencewithalendronatefor osteoporosisinpostmenopausalwomen.NEnglJMed. 2004;350:1189–99.
23.BilezikianJP,BrandiML,RubinM,SilverbergSJ.Primary hyperparathyroidism:newconceptsinclinical,densitometric andbiochemicalfeatures.JInternMed.2005;257(1):6–17.
24.SeemanE,WahnerHW,OffordKP,KumarR,JohnsonWJ,Riggs BL.Differentialeffectsofendocrinedysfunctionontheaxial andtheappendicularskeleton.JClinInvest.1982;69:1302–9.
25.SilverbergSJ,ShaneE,delaCruzL,DemsterDW,FeldmanF, SeldinD,etal.Skeletaldiseaseinprimary
hyperparathyroidism.JBoneMinerRes.1989;4:283–91.