www.jped.com.br
ORIGINAL
ARTICLE
Predictive
factors
of
mortality
in
pediatric
patients
with
acute
renal
injury
associated
with
sepsis
夽
,
夽夽
Marcia
C.
Riyuzo
a,∗,
Liciana
V.
de
A.
Silveira
b,
Célia
S.
Macedo
a,
José
R.
Fioretto
aaUniversidadeEstadualPaulista(UNESP),FaculdadedeMedicina,DepartamentodePediatria,Botucatu,SP,Brazil
bUniversidadeEstadualPaulista(UNESP),InstitutodeBiociênciasdeBotucatu,DepartamentodeBioestatística,Botucatu,
SP,Brazil
Received15October2015;accepted8April2016 Availableonline2July2016
KEYWORDS
Acutekidneyinjury; Sepsis;
Predictivefactors; Mortality
Abstract
Objective: Toevaluatetheprognosisfactorsofchildrenwithsepsisandacutekidneyinjury.
Methods: Thiswasaretrospectivestudyofchildrenwithsepsisandacutekidneyinjurythat
wereadmittedtothepediatricintensivecareunit(PICU)ofatertiaryhospital.Amultivariate analysiswasperformedtocompareriskfactorsformortality.
Results: Seventy-seven children (47 males) were retrospectively studied, median age of4
months.Meanlengthofhospitalstaywas7.33±0.16days,68.9%ofpatientsreceived mechan-ical ventilation, 25.9% had oligo-anuria, and peritoneal dialysis was performed in 42.8%. The pRIFLE criteria were: injury (5.2%) and failure(94.8%), and the staging system crite-ria were: stage 1 (14.3%), stage 2 (29.9%), and stage 3 (55.8%). The mortality rate was 33.7%. In themultivariate analysis, therisk factorsfor mortalitywere PICU length ofstay (OR=0.615, SE=0.1377, 95% CI=0.469---0.805, p=0.0004); invasive mechanical ventilation (OR=14.599,SE=1.1178,95%CI=1.673---133.7564,p=0.0155);needfor dialysis (OR=9.714, SE=0.8088,95%CI=1.990---47.410,p=0.0049),andhypoalbuminemia(OR=10.484,SE=1.1147, 95%CI=1.179---93.200,p=0.035).
Conclusions: Theriskfactorsformortalityinchildrenwithacutekidneyinjurywereassociated withsepsisseverity.
©2016PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradePediatria.Thisis anopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/
by-nc-nd/4.0/).
夽
Pleasecitethisarticleas:RiyuzoMC,SilveiraLV,MacedoCS,FiorettoJR.Predictivefactorsofmortalityinpediatricpatientswithacute renalinjuryassociatedwithsepsis.JPediatr(RioJ).2017;93:28---34.
夽夽
StudyconductedatUniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil.
∗Correspondingauthor.
E-mail:mriyuzo@fmb.unesp.br(M.C.Riyuzo).
http://dx.doi.org/10.1016/j.jped.2016.04.006
PALAVRAS-CHAVE
Lesãorenalaguda; Sepse;
Fatorespreditivos; Mortalidade
Fatorespreditivosdemortalidadeempacientespediátricoscomlesãorenalaguda associadacomsepse
Resumo
Objetivo: Avaliarosfatoresprognósticosdecrianc¸ascomsepseelesãorenalaguda.
Métodos: Estudo retrospectivo de crianc¸as internadas com sepse e lesão renal aguda em
unidade deterapia intensivapediátrica deservic¸oterciário.Usou-sea análisemultivariada nacomparac¸ãodosfatoresderiscoparamortalidade.
Resultados: Foram avaliados 77 pacientes (47 masculinos) com mediana de 4 meses de
idade. A média do tempo de internac¸ão foi de 7,33±0,16 dias, 68,9% necessitaram de ventilac¸ãomecânica,25,9%eramoligoanúricose42,8%necessitaramdediálise.Aclassificac¸ão da lesão renal aguda foi pRIFLE I em 5,2% e F em 94,8% e estágio 1 (14,3%), estágio 2 (29,9%) e estágio 3 (55,8%). A taxa de mortalidade foi de 33,7%. Na análise multivari-ada os fatores de risco foram tempo de internac¸ão (OR=0,615 erro padrão=0,1377, 95% CI=0,469-0,805, p=0,0004), ventilac¸ão mecânica (OR=14,599, erro padrão=1,1178, 95% CI=1,673-133,7564, p=0,0155), necessidade de diálise (OR=9,714, erro padrão=0,8088, 95%CI=1.990-47,410,p=0,0049)ehipoalbuminemia(OR=10,484,erropadrão=1,1147,95% CI=1,179-93,200,p=0,035).NomodelodeCoxasobrevidafoiinfluenciadapelanecessidade dediálise(HR=2,952,erropadrão=0,44862,95%CI=1,225-7,112,p=0,016)ehipoalbuminemia (HR=3,326,erropadrão=0,59474,95%CI=1,037-10,670,p=0,043).
Conclusões: Osfatoresderiscopara mortalidadenascrianc¸ascomlesão renalagudaforam
associadosàgravidadedasepse.
©2016PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradePediatria.Este ´
eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/
by-nc-nd/4.0/).
Introduction
Acute kidney injury (AKI) is a significant factor that con-tributes to the morbidity and mortality of children and newborns admitted to intensive care units.1 The admis-sion of patients with AKI to the pediatric intensive care unit (PICU) ranges between 48% and 68%.1,2 An associa-tionbetweensepsisandAKIwasobservedin71.03%ofthe patientsadmittedtothisPICU.
MultiplefactorsmaybeimplicatedintheetiologyofAKI inchildrenwithsepsis.1Thefrequencyofsepsis-associated AKIhasincreased3---5;between10%andover30%ofcasesof AKIwereduetosepsisandinfection.2,6---8Pediatricpatients with sepsis and multiple systemic organ dysfunction had lowersurvivalratesthan thosewithischemia.4 Sepsiswas associatedwithdeathin62%ofpatientswithAKIandwasa riskfactorformortality.8---10Childrenwithsepsishada ten-foldhigherriskofdeath.8Thereisascarcityofpublications abouttheriskfactorsformortalityinpediatricpatientswith AKIandsepsis.Moststudiesreporteddataonneonatesand childrenwithAKIafterheartsurgery.3,11,12
In pediatric patients admitted to the PICU with AKI associated withhemolytic uremicsyndrome or cancer, or post-heart surgery, the factors related to mortality were thrombocytopenia,age>12 years,and presenceof hypox-emia and/or hypotension and/or coagulopathy.5 In this study,themortalityofpatientswithAKIwashigher(29.6%) whencomparedwiththatofpatientswithoutit(2.3%).5The determinationofpredictivefactorsofmortalityinpediatric patients withsepsis-associated AKI maycontribute to the identificationofthesepatients,aswellasthe implementa-tionofearlytherapeuticmeasurestoreducemortality.
For years, the definition of AKI was heterogeneous. The proposal to standardize the definition of AKI using the pediatric RIFLE (pRIFLE) criteria13---17 and the staging system14,16,18,19favorsthecomparisonofresultsbetween dif-ferentstudies.Aprospectivestudyshowedthattheinjury andfailureclassificationofthepRIFLEwasapredictive fac-torofmortalityinchildrenadmittedtothePICU.17
This study assessed independent predictive factors of mortalityinapediatricpatientcohortwithsepsis-associated AKI.
Methods
Patients,definitions,andassessedparameters
Thiswasaretrospectiveobservationalstudyofapediatric patientcohortadmittedtothePICUofFaculdadede Medi-cina of Botucatu, UNESP-Universidade Estadual Paulista, which is a tertiary hospital. Data were obtained from a databaseofpatientsadmittedtothePICUfromJanuary1990 toDecember1994.Thestudyincludedchildrenaged1to132 monthsofage,ofbothgenders,admittedtothePICUwith adiagnosisofsepsisandAKI.
whentheserumcreatininevaluewashigherthanthenormal valueforageandheightaccordingtothereportsofGuignard andSantos.20Allpatientsincludedinthestudyhada diag-nosisofsepsisdefinedbytheInternationalPediatricSepsis ConsensusConferencecriteria.21,22
The analyzed data were: (a) demographic data (age, gender), (b) days in the PICU; (c) clinical data (olig-uria or anuria, hypotension or hypertension, number of vasoactive drugs, use and duration of mechanical venti-lation, need for dialysis, AKI classification criteria, and evolution during PICU stay); (d) laboratory data: serum albumin (hypoalbuminemia if value <2.5g/dL), serum bicarbonate(metabolicacidosisifvalue<15mEq/L), elec-trolytes(hypocalcemiaifserumcalciumvalue<7.9mg/dL; hyperkalemia if potassium >5.5mEq/L, or hypokalemia if potassium <2.5mEq/L, hyponatremia if sodium value <125mEq/L), and serum glucose (hypoglycemia if value <50mg%andhyperglycemiaifvalue>150mg%);hematocrit, plateletcount,andproteinuria(dipstickmethod+1or+2on urinalysis).
Oliguria was defined as diuresis <500mL/24h in older childrenor<1mL/kg/hinsmallerchildrenandinfants.23,24 Anuria was defined as complete cessation of diuresis for a period of 24h.23,24 Hypotension was defined as a sys-tolicbloodpressure lowerthanthefifth percentileofthe normal level for age.25 Hypertension was defined as sys-tolicand/ordiastolicbloodpressureequaltoorabovethe 95thpercentileforage,gender,andheight.26 Thrombocyto-peniawasdefinedasplateletlevel<50,000/mm3.Thislevel isconsideredasmoderatethrombocytopenia,andplatelet count>50,000/mcLdonotrequireroutinetreatment. The classificationcriterion wasappliedonthe firstday of AKI diagnosis.
The pRIFLE criteria defined AKI as: pRIFLE R, or Risk (25%decreaseintheestimatedcreatinineclearance[CrCl] or diuresis<0.5mL/kg/hfor 8h); pRIFLE I,or injury (50% decreaseinCrClordiuresis<0.5mL/kg/hfor16h);pRIFLEF, orfailure(75%decreaseinCrCl,orCrCl<35mL/min/1.73m, or diuresis <0.3mL/kg/h for 24h, or anuria for 12h); pRIFLEL,orloss(persistentfailure>fourweeks);and pRI-FLE E, or end-stage (end-stage kidney disease-persistent failure>three months).18,27 Only the R, I, and F classi-fications for AKI were used in the present study. The Schwartz equation was used to calculate CrCl.18,27 Basal CrCl was calculated through the Schwartz equation using theserumcreatininevalueuptothreemonthsbeforePICU admission.
ThestagingsystemdefinedAKIas:stage1---serum cre-atinineincrease>0.3mg/dL(>26.4mmoL/L)or≥150---200% increase (1.5- to two-fold) from baseline or urine out-put <0.5mL/kg/h for >6h); stage 2 --- serum creatinine increase >200---300% (two- to three-fold) frombaseline or urineoutput<0.5mL/kg/hfor>12h);stage3---serum cre-atinine increase >300% (> three-fold) >24h frombaseline or serum creatinine ≥4.0mg/dL [354moL/L] or with a sharpincreaseofatleast0.5mg/dL[44moL/L])ordiuresis <0.3mL/kg/horanuriafor12h).18
In this study, the use of the pRIFLE criterion was car-riedoutaccordingtoCrClalterationandthestagingsystem accordingtoalterationsinserumcreatininelevels,as74.1% ofthepatientshadnon-oliguricAKI.
ThestudywasapprovedbytheLocalEthicsCommittee.
Statisticalanalysis
TheresultswereanalyzedusingtheSASSystemforWindows (SAS InstituteInc.®, USA). Descriptive dataarepresented
as percentage. Continuous variables (age, PICU length of stay, daysof mechanical ventilation, urinary volume,and laboratory test values) were expressed as mean±SD or median.Categoricalvariables(gender,presenceofoliguria, hypotensionorhypertension,vasoactivedrugs,mechanical ventilation,need fordialysis,hypocalcemia, hyperkalemia or hypokalemia,hyponatremia,thrombocytopenia,and/or presence of proteinuria) were expressed as frequency of occurrence. When comparing the survivor and deceased groups, Mann---Whitney’s U test was used to analyze the continuousvariablesandFisher’sexacttestforcategorical variables.Multiple logisticregressionanalysiswasusedto define therisk factorsand theevolution ofvariables that showedp<0.20at theunivariateanalysis;oddsratiowere adjustedandconfidenceintervalswerecalculated.
Kaplan---Meier survival curves were generated and the log-rank analysiswasused tocomparesurvival rates. Cox regressionanalysiswasperformedtoassesstheriskfactors formortalityduringPICUstay.p-Values<0.05were consid-eredsignificant.
Results
Thestudyincluded77childrenwithsepsisandAKI.Diarrhea and/orpneumoniawerethemostcommoncausesofsepsis (84%).
The mean age of patients was 12.79±23.45 months (median 4 months); 77% were ≤10 months; 61.03% were boys.ThemeannumberofdaysinthePICUwas7.33±0.16 days(range1---18days);66patients(85.7%)hadadiagnosis ofAKIonthefirstdayofPICUadmission;11patients(14.3%) werehospitalizedforamedianof2days(range1---43days) beforeAKIdiagnosis.Diuresisrangedfrom0to11mL/kg/h; 57 patients (74.1%) had non-oliguric AKI and ten (12.9%) were anuric. Three patients (0.04%) hadhypotension and eight(10.3%)hadhypertension;98.7%requiredvasopressor drugsand92.2%receivedmorethantwovasoactivedrugs. Fifty-fourpatients(70.1%)requiredmechanicalventilation and42.8%requiredacuterenalreplacementtherapy; perit-onealdialysiswascarriedoutinthesepatients.Indications fordialysisincludedoliguria,increaseinserumurea, hyper-kalemia(K>5.5mEq/L),pulmonaryedema,andinsufficient diuresis to allow administration of medications and/or nutrition.
ThepRIFLEclassificationofAKIpatientswas:pRIFLEIin four(5.2%)andpRIFLEFin73(94.8%).CrClrangedfrom4.19 to56.66mL/min/1.73m2.As for theclassification
Table1 Clinicalfeaturesandevolutionofpatientswithsepsisandacutekidneyinjury.
Variable Survived(n=51) Deceased(n=26) pa
Age(months,median) 4 6 0.37b
Gender(male/female,n) 32/19 15/11 0.80c
PICUadmission(days,median) 8 4.5 0.001b
Diuresis(mL/kg/h,median) 2.0 1.4 0.19b
Oligoanuria(n) 9 11 0.039c
Hypotension(n)/hypertension(n) 1/6 2/2 0.50c
Vasoactivedrug(n)0/1/2ormore 1/4/46 0/1/25 0.77c
Mechanicalventilation(n) 30 24 0.0015c
Daysonventilation(median) 5 4 0.18b
Dialyzed(n) 14 19 0.0002c
Acutekidneyinjuryclassificationcriteria: pRIFLE
pRIFLEIn(%) 2(4) 2(7.6)
0.60c
pRIFLEFn(%) 49(96) 24(92.4)
Stagingsystem
Stage1n(%) 11(21.6) 0
0.021c
Stage2n(%) 13(25.5) 10(38.5)
Stage3n(%) 27(52.9) 16(61.5)
n,numberofpatients;PICU,pediatricintensivecareunit;pRIFLE,pediatricrisk,injury,failure,loss,endstagerenaldisease.
a Statisticalanalysis. b Mann---Whitney’sUtest. c Fisher’sexacttest.
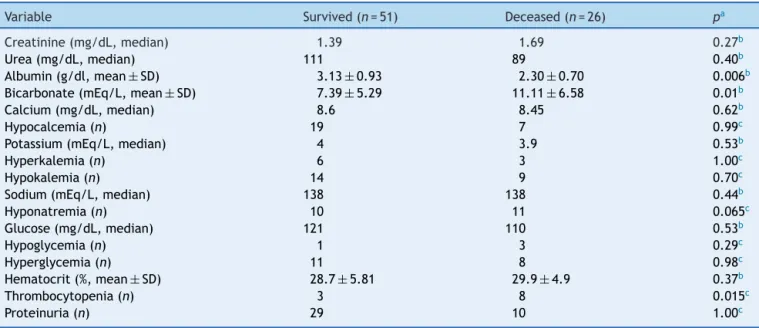
Patients’ laboratory data and evolution are shown in
Table 2. Hypoalbuminemia was observed in 28.3% and metabolicacidosisin90.7%(68/75)ofpatients.
The mortalityrate was 33.7% (26/77). Elevenpatients had disseminated intravascular coagulation, and ten died (onehadacuterespiratorysyndromeandonehadmultiple organfailure).
Attheunivariateanalysis,thefactorsPICUlengthofstay, oligo-anuria,invasivemechanicalventilation,needfor dial-ysis, AKI stage 2 and 3 criteria, hypoalbuminemia, serum bicarbonate, and thrombocytopenia were associated with mortality.
In the multiple logistic regression analysis, the inde-pendentrisk factors associated withmortality were PICU
Table2 Laboratoryfeaturesandevolutionofpatientswithsepsisandacutekidneyinjury.
Variable Survived(n=51) Deceased(n=26) pa
Creatinine(mg/dL,median) 1.39 1.69 0.27b
Urea(mg/dL,median) 111 89 0.40b
Albumin(g/dl,mean±SD) 3.13±0.93 2.30±0.70 0.006b
Bicarbonate(mEq/L,mean±SD) 7.39±5.29 11.11±6.58 0.01b
Calcium(mg/dL,median) 8.6 8.45 0.62b
Hypocalcemia(n) 19 7 0.99c
Potassium(mEq/L,median) 4 3.9 0.53b
Hyperkalemia(n) 6 3 1.00c
Hypokalemia(n) 14 9 0.70c
Sodium(mEq/L,median) 138 138 0.44b
Hyponatremia(n) 10 11 0.065c
Glucose(mg/dL,median) 121 110 0.53b
Hypoglycemia(n) 1 3 0.29c
Hyperglycemia(n) 11 8 0.98c
Hematocrit(%,mean±SD) 28.7±5.81 29.9±4.9 0.37b
Thrombocytopenia(n) 3 8 0.015c
Proteinuria(n) 29 10 1.00c
n,numberofpatients.
Days of PICU stay
0.0 2.5 5.0 7.5 10.0 12.5 15.0 17.5 20.0
Kaplan-Meier survival curve estimated by hypoalbuminemia
100
75
50
25
0
Without hypoalbuminemia: With hypoalbuminemia:
% survival
Figure1 SurvivalcurveinAKIrelatedtohypoalbuminemia.
0.0 2.5 5.0 7.5 10.0 12.5 15.0 17.5 20.0 100
75
50
25
0
Without dialysis: With dialysis:
Days of PICU stay
Kaplan-Meier survival curve estimated by dialysis
% survival
Figure2 SurvivalcurveinAKIrelatedtodialysis.
lengthofstay(OR=0.615SE=0.1377,95%CI=0.469---0.805,
p=0.0004), invasive mechanical ventilation (OR=14.599, SE=1.1178,95% CI=1.673---133.7564, p=0.0155),need for dialysis (OR=9.714, SE=0.8088, 95% CI=1.990---47.410,
p=0.0049), hypoalbuminemia (OR=10.484 SE=1.1147, 95% CI=1.179---93.200, p=0.035), and serum bicarbonate (OR=1.231,SE=0.0735,95%CI=1.066---1.422,p=0.0046).
Othervariableswerenotassociatedwithmortality: olig-uria, anuria (OR=1.13, SE=0.1302 95% CI=0.881---1.467,
p=0.32), thrombocytopenia (OR=1.469, SE=1.0595, 95% CI=0.184---11.718, p=0.72), and AKI stage (OR=0.060, SE=2.2017,95%CI≤0.001---4.557,p=0.20).
The estimated probabilitiesof survivalduring thePICU staywere25%inhypoalbuminemicpatients,whencompared with75% inpatientswithnormalalbumin(logrank=5.88,
p=0.015)and24%inpatientsrequiringdialysiscomparedto 76%ofpatientswhodidnotneeddialysis(logrank=8.513,
p=0.0035;Figs.1and2).
InthesurvivalanalysisusingCoxmodel,theparameters thatinfluencedsurvivalwere:needfordialysis(HR=2.952, SE=0.44862, 95% CI=1.225---7.112, p=0.016), hypoalbu-minemia (HR=3.326, SE=0.59474, 95% CI=1.037---10.670,
p=0.043),andserumbicarbonate(HR=1.097,SE=0.04098, 95%CI=1.042---1.198,p=0.024).Needforinvasive mechan-ical ventilation did not influence survival (HR=2.424, SE=1.07710,95%CI=0.294---20.016,p=0.411).
The median of daystoAKI improvementwas fivedays (range2---21days)inpatientswithAKI stage1;sevendays (3---19daysvariation)inpatientswithstage2;andeightdays (3---21daysvariation)inpatientswithstage3.AKIrecovery inthefirstweek occurredin72.7%(8/11)ofpatientswith AKIstage1,61.5%(8/13)ofpatientswithstage2,and48.1% (13/27)ofpatientswithstage3.
Discussion
An association between sepsis and AKI was observed in 71.03%ofthepatientsadmittedtothisPICU;thesepatients hadahighmortalityrate(33.7%),similartothatdescribed inotherstudies.4,8,13,28---31
There is a high incidence of sepsis-associated AKI in critically-illpatients.31TheidentificationofsevereAKI pre-dictivefactorshasthepotentialtooptimizetreatment.31,32 Among thefactors associatedwithmortality, the pres-ence of oliguria or anuria, need for dialysis, need for mechanical ventilation, and hypoalbuminemia should be emphasized.
did not remain as such in the multivariate analysis. The lowerproportion ofoligo-anuric patients must have influ-encedthestatisticalanalysis.Mostofthepresentpatients werenon-oliguric,differentfromwhatwasobservedinthe aforementionedstudies.Thepresenceofoliguriamakesthe disease more severe, hindering fluid administration, thus facilitatingthedevelopmentofhypervolemia,which com-plicatestheunderlyingdisease.31
The need for dialysis increased by 3.76 times the risk of mortality in children with AKI,29 especially in patients undergoingdialysisforlongerperiods.9Thepresentdataare consistentwiththeaforementionedstudies.9,29
Needformechanicalventilationwasassociatedwith mor-talityinpatientswithAKIunrelatedtoprimaryurinarytract disorder9,23 and in those with prerenal and non-prerenal AKI11,29; the present findings are consistent with these studies.9,11,23 Patientswithsepsis-associated AKI aremore likelytorequiremechanical ventilationandhemodynamic supportwithvasoactivetherapy,andtoreceivelarge vol-umes of fluid for resuscitation.31 This fact contributes to longerhospitalstayinthePICUandincreasedmortality.33
In the present study, patients with decreased serum bicarbonatelevelshadhighersurvival.Intheliterature,the presenceofacidosiswasnotanindependentfactorforthe mortalityofpatientswithAKI.24Thepresentstudywas con-ductedinatertiaryinstitutionthatisareferencecenterfor medicalorsurgicalcritically-illpatients,whohadprobably beentreatedforacidosiswithbicarbonatesolutionsbefore arrivalatthisservice.
Hypoalbuminemiawasassociated withhighermortality inpediatric patients.12 In228pediatric patientswithAKI, serumalbuminwashigheramongsurvivors(3.3±0.9g/dL) than in non-survivors (2.6±0.7g/dL).12 Hypoalbumine-mia may result from accelerated protein catabolism of metabolic alterations in AKI.30 Moreover, albumin synthe-sisissuppressedinresponsetoinflammatoryconditions,34 and inflammatorymediators areinvolved in children with sepsis.21,31 Inchildren withseveredisease, hypoalbumine-miawasassociatedwithhigh mortalityandlongertimeof mechanicalventilation.35
Theclassificationofrenalinjuryseverityhasbeen asso-ciatedwithincreasedhospitallengthofstayandincreased in-hospital relativemortalityrisk.31 According tothe pRI-FLEcriteria, the patientsin thepresent study hadsevere AKI(mostwereclassifiedaspRIFLEF).Incontrast,the stag-ing criterion showed an evendistribution between stages 1,2,and3.This factmustbeassociatedwithdifferences in theuse of parameterstodefine AKI. The pRIFLE crite-ria used CrCl and the staging criteria used the increase in serum creatinine levels. Evidence suggests that small changesinserumcreatinineareassociatedwithincreased patientmortality.18Otherauthorshavefoundsignificant dif-ferencesinAKIseveritydistributionwhenserumcreatinine increasewasusedinsteadofCrCltodefineAKI; thelatter showedgreatersensitivity.14,16,18
PatientswithpRIFLEIorFatadmissionshowedatwo-fold higherriskofmortality,whencomparedtopatientswith pRI-FLER.13,17Noassociationwasobservedbetweenthestrata ofpRIFLEcriteriaandmortality,similartothedatareported byPlötzetal.15
WhentheAKIstagingcriterionwasappliedtothepresent patients,resultssimilartothosereportedbyOzc¸akaretal.19
were observed. The mortality rate was 33%, and it was higher in patients with AKI stage 2 and 3, similarto the presentresults.Insepsis-associatedAKI,theprobabilityof deathwashigherinpatientsclassifiedasstage3AKI,when comparedwiththoseclassifiedasstage1.31
Studieshaveshownanassociationbetweenthedegreeof kidneydiseaseseverityandimprovementinrenalfunction: 46%ofpatientsshowedrenalfunctionrecoverywithin48h, predominatingin62.5%patientswithpRIFLERatadmission, whencomparedtothosewithpRIFLEI(38.1%)orpRIFLEF (26.7%).13TherecoveryfromAKIinthefirstweek,according tothe stagingcriterion, occurred in allpatients with AKI stage1, in half of thepatients with stage2, andin one-thirdof patients withstage3.19 The present resultswere consistentwiththeaforementionedstudies.
Theassessedpredictive factorsofmortalityinchildren with sepsis-associated AKI comprised clinical, laboratory, andAKIclassificationparameters.Thereisnosingle consen-susonwhichparameter isidealforearlydiagnosis ofAKI, whichwouldimplyinearly-onsettherapyaimedatreducing mortality.
The constant monitoring of critically-ill patients, assessingthepresenceofoliguria,hypertensionor hypoten-sion,andhypoalbuminemia,aswellastheevolutiontothe needformechanicalventilationand/ordialysis,shouldraise theearlysuspicionofAKIdevelopment.Atthesametime, theAKIclassificationshouldberoutinely carriedoutsince thefirstdayofhospitalization,andonthethirddayforthe earlydetectionofAKI,accordingtoparameterevolution.31 Authors have validated the Renal Angina Index (RAI) usingtheproductof theriskfactors (admissiontoPICU ---score1,stemcelltransplantation---score3,ventilationand inotropics---score5)andtheinjuryfactors(deathrate evo-lutionassociatedwithfluidoverloadpercentage,decrease intheestimatedcreatinine clearance,percentageoffluid overload---scorerangingfrom1,2,4,and8),whoseRAIvalue rangesfrom1to40.32 TheRAIcutoffvalue≥8isindicative ofhighriskforAKI.
Thepresent studyhaslimitations,suchasthe observa-tionalretrospectivedesignwithasmallnumberofpatients studied in a single center; however, this cohort included theevaluation of AKI inpediatric patients witha specific condition,i.e., sepsis.The smallnumberof patients with thepRIFLEIclassificationmayhaveinfluencedthepowerof statistics.
It can be concludedthat the mortality rate is high in patientswithsepsisandAKI;thepredictivefactorsrelated tomortalitywere easytoapply, aswell astheAKI classi-ficationbythestagingsystemor pRIFLEandreflectedthe evolutionofpatientswithsepsisandAKI.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
2.GokcayG,EmreS,TanmanF,SirinA,ElciogluN,DolunayG.An epidemiologicalapproachtoacuterenalfailureinchildren.J TropPediatr.1991;37:191---3.
3.Moghal NE, Brocklebank JT, Meadow SR. A review of acute renalfailureinchildren:incidence,etiologyandoutcome.Clin Nephrol.1998;49:91---5.
4.Hui-StickleS,BrewerED,GoldsteinSL.PediatricARF epidemi-ologyatatertiarycarecenterfrom1999to2001.AmJKidney Dis.2005;45:96---101.
5.BaileyD,PhanV,LitalienC,DucruetT,MérouaniA,LacroixJ, etal.Riskfactorsofacuterenalfailureincriticallyillchildren:a prospectivedescriptiveepidemiologicalstudy.PediatrCritCare Med.2007;8:29---35.
6.Anochie IC,EkeFU.Acuterenal failurein Nigerianchildren: PortHarcourtexperience.PediatrNephrol.2005;20:1610---4. 7.DuzovaA,BakkalogluA,KalyoncuM,PoyrazogluH,DelibasA,
OzkayaO,etal.Etiologyandoutcomeofacutekidneyinjuryin children.PediatrNephrol.2010;25:1453---61.
8.VachvanichsanongP,DissaneewateP,LimA,McNeilE.Childhood acuterenalfailure:22-yearexperienceinauniversityhospital insouthernThailand.Pediatrics.2006;118:e786---91.
9.OtukeshH,HoseiniR,HoomanN,ChalianM,ChalianH, Tabar-roki A. Prognosis of acute renal failure in children. Pediatr Nephrol.2006;21:1873---8.
10.Loza R,Estremadoyro L, Loza C,Cieza J.Factorsassociated withmortalityinacuterenalfailure(ARF)inchildren.Pediatr Nephrol.2006;21:106---9.
11.GallegoN,GallegoA,Pascual J,Lia˜noF,EstepaR,Ortu˜noJ. Prognosisofchildrenwithacuterenal failure:astudyof138 cases.Nephron.1993;64:399---404.
12.WilliamsDM,SreedharSS,MickellJJ,ChanJC.Acutekidney fail-ure:apediatricexperienceover20years.ArchPediatrAdolesc Med.2002;156:893---900.
13.Akcan-ArikanA,ZappitelliM,LoftisLL,WashburnKK,Jefferson LS,GoldsteinSL.ModifiedRIFLEcriteriaincriticallyillchildren withacutekidneyinjury.KidneyInt.2007;71:1028---35. 14.ZappitelliM,ParikhCR,Akcan-ArikanA,WashburnKK,Moffett
BS,GoldsteinSL.Ascertainmentandepidemiologyofacute kid-neyinjuryvarieswithdefinitioninterpretation.ClinJAmSoc Nephrol.2008;3:948---54.
15.Plötz FB, Bouma AB, van Wijk JA, Kneyber MC, Bökenkamp A. Pediatric acutekidney injury in theICU:an independent evaluation of pRIFLE criteria. Intensive Care Med. 2008;34: 1713---7.
16.KavazA,Ozc¸akarZB,KendirliT,OztürkBB,EkimM,Yalc¸inkaya F. Acute kidney injury in a paediatric intensive care unit: comparison of the pRIFLE and AKIN criteria. Acta Paediatr. 2012;101:e126---9.
17.SolerYA,Nieves-PlazaM,PrietoM,García-DeJesúsR, Suárez-RiveraM.Pediatricrisk,injury, failure,loss,end-stage renal diseasescoreidentifiesacutekidneyinjuryandpredicts mor-talityincriticallyillchildren:aprospectivestudy.PediatrCrit CareMed.2013;14:e189---95.
18.BaggaA,BakkalogluA,DevarajanP,MehtaRL,KellumJA,Shah SV,etal.Improvingoutcomesfromacutekidneyinjury:report ofaninitiative.PediatrNephrol.2007;22:1655---8.
19.Ozc¸akarZB,Yalc¸inkayaF,AltasB,ErgünH,KendirliT,Ates¸C, etal.ApplicationofthenewclassificationcriteriaoftheAcute
KidneyInjuryNetwork:apilotstudyinapediatricpopulation. PediatrNephrol.2009;24:1379---84.
20.GuignardJP,SantosF.Laboratoryinvestigations.In:AvnerED, HarmonWE,NiaudetP,editors.Pediatricnephrology.5thed. Baltimore:Lippincott,WilliamsandWilkins;2004.p.399---424. 21.FiorettoJR,BorinFC,BonattoRC,RicchettiSM,KurokawaCS, deMoraesM,etal. Procalcitonininchildrenwithsepsisand septicshock.JPediatr(RioJ).2007;83:323---8.
22.Goldstein B, Giroir B, Randolph A, International Consensus ConferenceonPediatricSepsis.Internationalpediatric sepsis consensusconference:definitionsforsepsisandorgan dysfunc-tioninpediatrics.PediatrCritCareMed.2005;6:2---8.
23.Gallego N, Pérez-Caballero C,Gallego A, Estepa R, Lia˜noF, Ortu˜noJ.Prognosisofpatientswithacuterenalfailurewithout cardiopathy.ArchDisChild.2001;84:258---60.
24.AroraP,KherV,RaiPK,SinghalMK,GulatiS,GuptaA. Prog-nosisofacuterenalfailureinchildren:amultivariateanalysis. PediatrNephrol.1997;11:153---5.
25.ECCCommittee,SubcommitteesandTaskForcesofthe Amer-ican Heart Association. 2005 American Heart Association Guidelinesfor CardiopulmonaryResuscitationandEmergency CardiovascularCare.Circulation.2005;112.IV1-203.
26.NationalHighBloodPressureEducationProgramWorkingGroup on High Blood Pressure in Children and Adolescents. The fourthreportonthediagnosis,evaluation, andtreatmentof high blood pressure in children and adolescents. Pediatrics. 2004;114:555---76.
27.Schwartz GJ, Brion LP, Spitzer A. The use of plasma creat-inine concentration for estimating glomerular filtration rate ininfants,children,and adolescents.Pediatr ClinNorthAm. 1987;34:571---90.
28.MedinaVillanuevaA, López-HerceCid J,López FernándezY, AntónGameroM,ConchaTorreA,ReyGalánC,et al.Acute renalfailure incritically-illchildren.Apreliminary study.An Pediatr(Barc).2004;61:509---14.
29.BresolinN,SilvaC,HalllalA,ToporovskiJ,FernandesV,Góes J,etal.Prognosisforchildrenwithacutekidneyinjuryinthe intensivecareunit.PediatrNephrol.2009;24:537---44. 30.DrumlW.Proteinmetabolisminacuterenalfailure.Miner
Elec-trolyteMetab.1998;24:47---54.
31.Alobaidi R, Basu RK, Goldstein SL, Bagshaw SM. Sepsis-associatedacutekidneyinjury.SeminNephrol.2015;35:2---11. 32.BasuRK, Zappitelli M,Brunner L,Wang Y, WongHR,Chawla
LS,etal.Derivationand validationoftherenalanginaindex toimprovethepredictionofacutekidneyinjuryincriticallyill children.KidneyInt.2014;85:659---67.
33.AlkandariO,EddingtonKA,HyderA,GauvinF,DucruetT, Gottes-manR,etal.Acutekidneyinjuryisanindependentriskfactor forpediatricintensivecareunitmortality,longerlengthofstay andprolongedmechanicalventilationincriticallyillchildren:a two-centerretrospectivecohortstudy.CritCare.2011;15:R146. 34.MoshageHJ,JanssenJA,FranssenJH,HafkenscheidJC,YapSH. Studyofthemolecularmechanismofdecreasedliversynthesis ofalbuminininflammation.JClinInvest.1987;79:1635---41. 35.LeiteHP,Rodrigues daSilvaAV,deOliveiraIglesiasSB,Koch