www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Quality
indicators
in
a
newborn
hearing
screening
service
夽
,
夽夽
Gabriela
Cintra
Januário
a,∗,
Stela
Maris
Aguiar
Lemos
b,
Amélia
Augusta
de
Lima
Friche
b,
Claudia
Regina
Lindgren
Alves
caSecretariadeEstadodeSaúdedeMinasGerais,BeloHorizonte,MG,Brazil
bDepartmentofPhonoaudiology,UniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil cDepartmentofPediatrics,UniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil
Received22November2013;accepted24May2014 Availableonline28August2014
KEYWORDS
Neonatalscreening; Infant;
Hearingloss; Qualityindicatorsof healthcare; Programevaluation
Abstract
Introduction:Newbornhearingscreening(NHS)programsareimplementedacrosstheglobeto detectearlyhearingimpairment.Inordertomeetthisobjective,thequalityoftheseprograms shouldbemonitoredusinginternationallyrecognizedindicators.
Objective: Toevaluateanewbornhearingscreeningservice(NHSS)usinginternationalquality indicators.
Methods:AretrospectivecohortstudyontheNHSSofMinasGeraiswasconducted,analyzing theservicesperformedbetween2010and2011. Resultswereanalyzed accordingtocriteria fromtheAmericanAcademyofPediatricsandtheJointCommitteeonInfantHearing.
Results:This study assessed6987children.The proportionsofcases thatwerereferred for aretest,thatfollowedthroughwithretest,andthatwerereferredfordiagnosiswere8.0%, 71.9%,and2.1%,respectively.Theproportionofassessednewbornchildreninthefirst30days oflifeinthisstudywas65%.ThemedianageofthosechildrenwhofailedboththeNHSand theretestwassignificantlyhigherthantheotherchildren.Thechanceofachildwithahearing impairment riskindicatortofailtheNHSwas 2.4timeshigherthanofthosewithoutarisk indicator.
夽 Pleasecitethisarticleas:JanuárioGC,LemosSMA,deLimaFricheAA,AlvesCR.Qualityindicatorsinanewbornhearingscreening
service.BrazJOtorhinolaryngol.2015;81:255---63.
夽夽Institution:UniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil.
∗Correspondingauthor.
E-mail:gbcintraj@gmail.com(G.C.Januário). http://dx.doi.org/10.1016/j.bjorl.2014.08.008
Conclusion:NHSSachievedthreeoffourevaluatedindicators.Despitethis,itisstillnecessary toperformNHSearlierandtoensurethatthesubsequentstepsarefollowed.
© 2014Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Triagemneonatal; Lactente;
Perdaauditiva; Indicadoresde qualidadeem assistênciaàsaúde; Avaliac¸ãode
programaseprojetos desaúde
Indicadoresdequalidadeemumservic¸odetriagemauditivaneonatal
Resumo
Introduc¸ão:ProgramasdeTriagemAuditivaNeonatal(TAN)sãoimplantadosem todomundo objetivandoadetecc¸ãoprecoce dadeficiênciaauditiva.A qualidadedestesprogramasdeve sermonitoradautilizandoindicadoresreconhecidosinternacionalmente,paraqueesteobjetivo sejaalcanc¸ado.
Objetivo:AvaliarumServic¸odeTriagemAuditivaNeonatal(STAN)combasenosindicadores internacionaisdequalidade.
Método: CoorteretrospectivacomanálisedosatendimentosrealizadosporumSTANdeMinas Gerais entre 2010 a 2011. Os resultados foram analisados segundo critérios da American AcademyofPediatricsedoJointCommitteeonInfantHearing.
Resultados: Foramavaliadas6.987crianc¸as.Asproporc¸õesdeencaminhamentoparareteste, adesãoaoretesteeencaminhamentoparadiagnósticoforam8,0%,71,9%e2,1%, respectiva-mente.Aproporc¸ãodecrianc¸asavaliadasnosprimeiros30diasdevidafoi65,0%.Amediana deidadedascrianc¸asquefalharamnaTANenoretestefoisignificativamentemaiordoque paraasdemais.Oriscodeumacrianc¸acomindicadorderiscoparadeficiênciaauditiva(IRDA) falharnaTANfoi2,4vezesmaiordoqueparaasdemais.
Conclusão:OSTANalcanc¸ou3dos4indicadoresavaliados.Noentanto,aindasãonecessários esforc¸osparacaptac¸ãoprecocedeneonatosparaatriagemauditivaeadesãoàsetapas subse-quentes.
©2014Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Hearingis thesensethatconnectsthe individualwiththe worldofsound.Hearing lossin newborns, ifnotdetected and treated early, compromises not only the language development of the child, but also emotional and social development.1
Programs for early identification of hearingloss in the neonatalperiodarebeingimplementedaroundtheworld, withtheaimtopromoteanearlyinterventionand,hence, the development of language by children with hearing impairment.2,3
The evaluation of health services and programs is requiredaspartofroutinehealthcare,toenablethe identifi-cationofdeficienciesandtovisualizehearingimprovement opportunities.The planningof healthactionsandthe tar-getingoffinancialresourcesshouldpreferablybebasedon theevidencefoundinevaluationstudies.4
According to the National Health Services Assess-ment Program, the evaluations can address four aspects: structure, working process, outcomes, and patients’ and professionals’ satisfaction.5 Most studies targeted to the
evaluationofneonatalhearing screeningprograms(NHSP) focusprimarily on the areas of working process and out-comes, because it is possible to verify the quality of
care and the change of health status of the patient, respectively.6,7
InMinasGerais,Brazil,theStateDepartmentofHealth (SES-MG) implantedthe Newborn Hearing Screening State Program (NHSSP) using an outpatient model in October 2007.8 Currently, the Programis beingimplemented with
the accreditation of maternity units as newborn hearing screeningreferenceservices(NHSRS).
The Municipality of Belo Horizonte has six accredited NHSRSs.Theseservicesarenetwork-based,accordingtothe flow of references and counter-referencesestablished by theHealthDepartmentof thatcity,andareaccredited by theNHSSP,establishedbyResolutionNo.1321SESof2007, thusfollowingitsguidelines,assessmentprotocols, health-careflow,andnomenclature.
Neonateswithnochangein theNHStest(i.e.,passed) are counter-referredto BHUsfor monitoring of the over-alldevelopmentbythefamilyhealthteam.Neonateswitha riskindicatorwhopasstheNHStestarereferredto reassess-mentintheserviceitself,sixmonthsaftertheNHStest,for auditorymonitoring.
NewbornswhofailtheNHStest(somechangeinthetest) arescheduledforretestin15---20daysinthesameservice. Those who fail the retest are referred to the Children’s DiagnosticAudiologyServiceinamunicipalitypublic hospi-tal.Newbornsidentifiedwithsensorineuralhearinglossare formalizedbytheHearingHealthRegulatoryBoardofBelo Horizonte,andreferredtooneofthetwoHigh-Complexity Hearing Health Care Services in Belo Horizonte for com-plementarystudies;selection,adaptation,andprovisionof individual hearing aids; and care monitoring and speech therapy.Itisnoteworthy,therefore,thatthephasesof diag-nosisandinterventionarenotperformedinthematernity itself,butindistinctandspecializedinstitutions.
ThisstudyaimedtoevaluateanNHSRSinthecityofBelo Horizonte fromJanuary 2010 toFebruary 2011, with ref-erence tothe quality indicators (referral toretest index, ageofthenewbornatthetimeofNHStest,attendanceto theretestindex,referralfordiagnosis index)proposedby the AmericanAcademy of Pediatrics (AAP)9 and theJoint
CommitteeonInfantHearing(JCIH).10
Methods
Thiswasalongitudinal,historicalcohortstudy,inwhichthe databaseofaNHSRSinthecityofBeloHorizontewas ana-lyzedwithregardtoservicesperformedfromJanuary2010 toFebruary2011.DatawereanalyzedfromtheNHStothe stageofreassessmentandreferraltospecialistservicesfor diagnosis.
TheNHSRSwherethisstudywasconductedisintegrated into a philanthropic hospital linked to the Brazilian Uni-fiedHealthSystem(SistemaÚnicodeSaúde---SUS),andis a referral center in obstetrics and gynecologyin the city of BeloHorizonte,and alsoa referralcenter for high-risk casesforothermunicipalitiesinthestate.Itsmaternityunit has134bedsandperformsanaverageof850deliveriesper month.NHSRShastheabilitytoassess700children/month, accountingforapproximately35%ofNHStestsbilledinBelo Horizonte.
The strategy for evaluation of children in this Service isthatrecommendedbytheNHSSP:measurementof tran-sient evoked otoacoustic emissions to stimuli (TEOAES), in association with the observation of children’s behav-ior to uncalibrated sound stimuli. To measure emissions, Audix Plus/Bio-logic® or AccuScreen Madsen® (both
annu-ally standardized and calibrated) equipment was used. Theinstrumentschosenforobservationofauditory behav-ior were a rattle (‘‘chocalho’’) with four ball-bells and an ‘‘agogô’’ (with a big bell). The child was considered unchangedwhenthecochlear-blinkreflex(CBR)andTEOAES werebilaterallypresent.Inthiscase,thechildpassedthe test. The remainingpatients wereclassifiedasfailing the NHStest.
AsevaluationcriteriaforTEOAES,thisstudyconsidered thepresence of adifferencebetween signal andnoise >6
in1.5,2.0,3.0,and4.0kHz;>70%reproducibilitywhenthe testwasperformedwithAudix;andapassed/failedprotocol whenthetestwasperformedwithAccuScreen.
The following were considered as risk indicators for hearingloss:historyofpermanentfamilialdeafness start-ing from childhood; length of stay in neonatal intensive care unit greater than five days; use of assisted ventila-tion;exposure toototoxicdrugs, such asaminoglycosides andloop diuretics; hyperbilirubinemiarequiring exchange transfusion;congenital infections (toxoplasmosis, rubella, cytomegalovirus,herpes,syphilis,humanimmunodeficiency virus);craniofacialanomaliesinvolvingtheearandtemporal bone;geneticsyndromes andneurodegenerativedisorders thatusuallyareexpressedwithhearingloss;andpostnatal bacterialorviralinfections.11
Twenty-onechildrenfromtheservicedatabasewerenot includedinthestudyduetolackof informationregarding birthdateand/ortestresults(0.3%),and58wereexcluded whounderwenttheNHStestatover180daysoflife(0.8%), fromatotalpopulationof6987children.
AlldatawereorganizedinExcel® spreadsheetsoftware,
andallinformationwasprocessedandanalyzedwithPASW Statistics,version18.
A descriptiveanalysis of frequency distributionof cat-egoricalvariables, andan analysis ofmeasures of central tendency and of dispersion for continuous variables were performed. The chi-squared test wasusedto analyzethe associationbetween NHStest outcomes,the resultofthe retest,retestabsenteeismandreassessmentabsenteeism, withthepresenceofriskindicatorsforhearingimpairment. TheKruskal---Wallistestwasusedtoanalyzetheassociation ofthesevariableswiththechild’sageat thetimeofNHS test.The relativerisk(RR)wascalculatedasameasureof themagnitudeoftheassociations.Forallanalyzes,a signif-icancelevelof5%andaconfidenceintervalof95.0%were adopted.
The qualityindicators proposed by international scien-tificcommunitieswereused9,10:
Phase1:NHStest
• Referraltoretestratebetween5.0%and20.0%ofchildren
whofailedtheNHStest;
• CompletionoftheNHStestinthefirst30daysoflifein
95.0%oftheaccessedchildren.
Phase2:Retest
• Follow-upofatleast95.0%ofchildrenwhofailedtheNHS
test.Fortheinitiationofprograms,consideraminimum of70%;
• Percentageofdiagnosisreferral<4.0%ofallchildren
eval-uated.
Table1 Generalcharacteristicsofthepopulationincluded inthestudy,BeloHorizonte,2010---2011.
Characteristics n %
Origin
BeloHorizonte 5843 83.6 Othermunicipalities 742 10.6 Noinformation 402 5.8
Birthinstitution
Localofresearch 2346 33.6 Other 4623 66.1 NoInformation 18 0.3
Timeofexamination
Beforehospitaldischarge 709 10.1 Afterhospitaldischarge 6266 89.7 Noinformation 12 0.2
Riskindicatorforhearingloss
Absent 6082 87 Present 905 13 Total 6987 100
Results
The informationregarding 6987 children evaluatedin the NHSRSoutpatientclinicwasanalyzedfromJanuary2010to February2011.Table1showsthemaincharacteristicsofthe childrenincludedinthestudy.
If 33.6% of the evaluated children were born in the institutionwhere thisstudy wasconducted.Mostchildren (89.7%)receivedtheNHStestattheoutpatientclinicafter theirhospital discharge,and 83.6% werefromthe city of BeloHorizonte.Thepercentageofchildrenwithriskfactors forhearinglosswas13.0%.
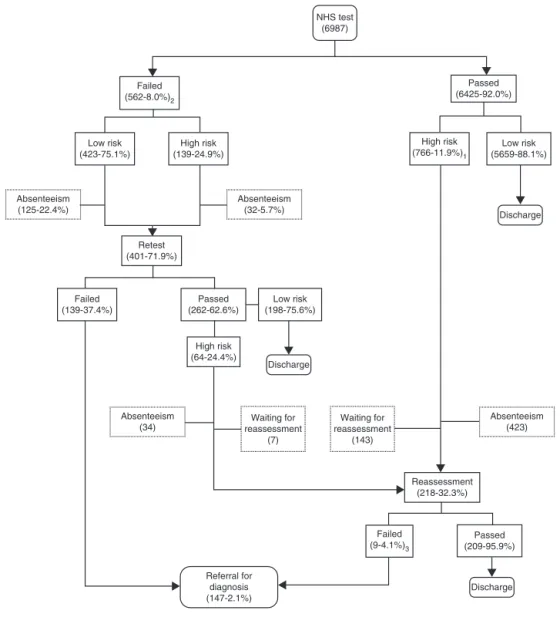
Fig.1showsthedistributionofchildrenaccordingtothe testresultsatvariousstagesoftheNHStestandthe pres-enceofriskindicators.Ofthe6987children,6425(92.0%) passed and 562 (8.0%) failed the NHS test. Of those who passed,766(11.9%)hadHIRI.Ofthese,761werereferred forreassessmentsixmonthsaftertheNHStest,andfivewere dischargedbecausetheywerealreadycloseto6monthsof age.
Among the 562 children who failed, 139 (24.9%) had HIRI.Of these,fourwerereferred directly tothe diagno-sis without the retest step, due to optimal conditions of assessmentandtothelatetimeof testing(children close to3monthsofage).OnlysixchildrenwereCBR-negative, although they showed TEOAES bilaterally. Of these, five attendedthe retest andone remained CBR-negative,and wasreferredfordiagnosis.
558childrenwerereferredforretesting,corresponding to 8.0% of the total of children assessed. Of these, 401 (71.9%)attended theretest, 262 (62.6%) passed, and139 (37.4%)remainedwiththealteredresultandwerereferred fordiagnosis.
825 high-risk children were referred for reassessment (761 who passed the NHS test and 64 who passed the retest).Of these, 150 (143 who passed the NHS test and sevenwhopassed the retest)still hadnot completedthe six months necessary for reassessment by the close of
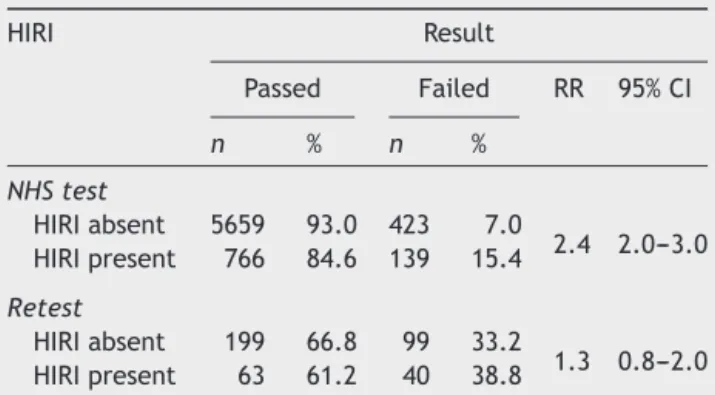
Table 2 Association between risk indicators for hearing loss and newborn hearing screening test and retest out-comes,BeloHorizonte,2010---2011.
HIRI Result
Passed Failed RR 95%CI
n % n %
NHStest
HIRIabsent 5659 93.0 423 7.0
2.4 2.0---3.0 HIRIpresent 766 84.6 139 15.4
Retest
HIRIabsent 199 66.8 99 33.2
1.3 0.8---2.0 HIRIpresent 63 61.2 40 38.8
NHS,neonatalhearingscreening;HIRI,hearingimpairmentrisk indicator;RR,relativerisk;CI,confidenceinterval.
this study. Of those 675 who had already completed six months,218 attendedthereassessment,correspondingto anabsenteeismof67.7%.Ofthosechildrenwhoattended, 209 (95.9%)passedand nine(4.1%)hadan altered assess-ment;fourofthesechildrenwerereferredfordiagnosis.The remainingfivechildrenwerereferredforasecond revalua-tionintheNHSRSitself,butdidnotreturnforconclusionof thetests.
Absenteeism in the retest and reassessment phases amounted to 28.1% and 67.7% of all referred children, respectively.
147children were referredfor audiological diagnostics (fourwhofailedNHS test,139 whofailedthe retest,and 4 whofailed the reassessment),correspondingto 2.1% of allchildrenincludedinthestudy.Theauthorswereunable to obtain the number of children with confirmed hearing loss, becausethe stages of diagnosis and treatment were conductedindifferentinstitutions,andalsobecauseofthe lackofacomprehensiveinformationsystem.
Theevaluationof theassociationamongriskindicators for hearinglossandtheresultof theNHStest isshown in Table 2. At themoment of theNHS test, the risk of fail-ingtheexamwas2.4timeshigherinthegroupofchildren withriskindicator(s)versusthegroupwithoutHIRI(95%CI: 2.0---3.0). There was no statistically significant difference betweengroupsduringtheretest.
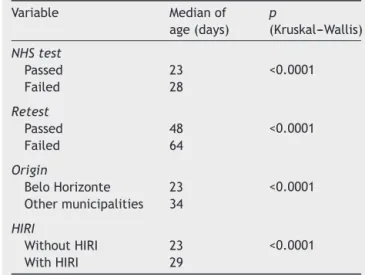
ThemedianageofNHStestcompletionwas23days, ran-gingfrom1to180days.Mostchildren(65.0%)receivedthe NHStestinthefirst30daysoflife.
Intheretestphase,208children(51.9%)wereevaluated after50daysoflifeand82.3%before90 daysoflife.The medianageattherevaluationstagewas209days,i.e.,close to7monthsofage.
Table 3 presents an analysis of the association among the child’s age and the result of the NHS test, retest results, child’s origin, and HIRI. Children who failed the NHS test were evaluatedat an older age than thosewho passed(p<0.0001).ChildrenfromBeloHorizontewere eval-uatedat ayoungeragethanchildrenfromthehinterlands (p<0.0001).ChildrenwithHIRIwere accessedat an older agethantheothers(p<0.0001).
NHS test (6987)
Failed (562-8.0%)2
Failed (139-37.4%)
Failed (9-4.1%)3
Low risk (423-75.1%)
Low risk (5659-88.1%)
Low risk (198-75.6%)
Discharge Discharge
Discharge
1 – Five children were discharged due to age close to 6 months. 2 – Four children were sent directly to the diagnosis. 3 – Five children did not return to complete the tests.
Retest (401-71.9%)
Passed (6425-92.0%)
Passed (262-62.6%)
Passed (209-95.9%) High risk
(139-24.9%)
High risk (766-11.9%)1
High risk (64-24.4%)
Absenteeism (32-5.7%) Absenteeism
(125-22.4%)
Absenteeism (34)
Absenteeism (423)
Referral for diagnosis (147-2.1%)
Waiting for reassessment
(7)
Reassessment (218-32.3%) Waiting for
reassessment (143)
Figure 1 Assistance trajectoryof children evaluated by a newbornhearing screeningservice in thecity of BeloHorizonte, 2010---2011.
Phase1:NHStest
• Referraltoretestindexequalto8.0%;
• CompletionoftheNHStestinthefirst30daysoflifein
65.1%ofthechildren.
Phase2:Retest
• Follow-upof71.9%ofchildrenwhofailedtheNHStest. • Percentage ofreferral fordiagnosis equalto2.1%of all
childreninitiallyevaluated.
Discussion
Indicatorsareinstrumentsconstitutedbyvariablesthat per-mittheidentificationandmeasurementofaspectsrelated to a particular reality, and should be chosen to highlight
therelevant issuesinvolvedintheevaluation.The quality indicatorsfor each phaseof an NHSPwere establishedby scientificinstitutionsandshouldbeusedasatooltocontrol theeffectivenessoftheprograms.9---11
In Brazil, several NHSPs have used the international indicatorsproposed by theAAP and theJCIH, withmixed results.12---14
Table3 Associationamong child’sageandthe resultof newborn hearing screening test and retest, origin ofthe child,andriskindicatorsforhearingloss,BeloHorizonte ---2010---2011.
Variable Medianof age(days)
p
(Kruskal---Wallis)
NHStest
Passed 23 <0.0001 Failed 28
Retest
Passed 48 <0.0001 Failed 64
Origin
BeloHorizonte 23 <0.0001 Othermunicipalities 34
HIRI
WithoutHIRI 23 <0.0001 WithHIRI 29
NHS,neonatalhearingscreening;HIRI,hearingimpairmentrisk indicator.
AlthoughtheliteraturerecommendstheNHStestbefore thechild’shospitaldischarge,9insomesituations the
out-patient model may be the most appropriate --- or even the only viable option. In Recife, given the absence of resourcesfortheimplementationoftheNHStest inthree publicmaternityunitsofthecity,asingleoutpatientmodel was organized, in order to offer the exam for newborns delivered in these hospitals.15 With regards to the high
rateofbirthsoutsideofhospitalunitsin Nigeria,theNHS test program wasimplemented in health centers respon-sible for child immunization.16 A cost-effectiveness study
of England’s NHSPs, considering the existinghospital and non-hospital models, demonstrated no significant differ-encebetween thecostandeffectivenessof eachofthese models.17
InthestateofMinasGerais,thevastmajority ofbirths occur in hospitals. In 2010, 420 hospitals that performed deliveries in the state were registered, and in 33%, the average number of births was less than 100 live births permonth.18 The introductionoftheNHStestinallthese
maternityunitswould beunfeasible,duetolackof finan-cialresources.ThisledthestateofMinasGeraistochoose an outpatient model with referral units for a particular region,considering the principle of regionalizationof the SUSand thehypothesis thatan excessivedecentralization ofhealthservicescanleadtoalossofefficiencyinhealth care, increasing the costs without increasing the quality, contradicting the principle of economy of scale. A study inColorado, USA, revealed that maternity units that per-formedagreaternumberofscreeningtestspermonthhad betterqualityindicatorsthanhospitals witha lower num-berofmonthlyscreeningtests.19However,itisquestionable
whetherthe outpatientmodel would be moresuitable as astrategyforachievinguniversalcoverage20;thus,studies
thataimtoanalyzethecoverageoftheNHSSParerequired. ItwasobservedthatchildrenwithHIRIwereevaluated at an older age than children without HIRI, probablydue
totheneedforprolongedhospitalizationforsomeofthese children. The origin of the child was alsoa variable that influenced the age of assessment: children living in Belo Horizontewere evaluatedat a youngerage thanthe oth-ers,suggestinggreaterdifficultyinaccessingtheServicefor childrenlivinginthehinterland.
In neonatal hearing screening outpatient programs in Nigeria and Maceió, Brazil, 86.4% and 73.5% of children, respectively, were evaluatedin the first30 daysof life ---percentagessuperiortothosefoundinthepresentstudy.12,16
Althoughthequalityindicatorof95.0%ofchildrenevaluated inthefirstmonthoflifewasnotreached,itisconsidered that a large enough number of children have been eval-uated in a timely manner to enable the diagnosis in the first 3months of life. However,it is clear thatthere is a needtoinvestinstrategiestofacilitateclientaccess,such astheadequacy ofmedicalappointment schedules, facil-itationoftransportation,anddecentralizationofservices, particularlyfor familiesliving inother municipalities.The authors emphasize that, in thisstudy, it wasnot possible toidentifytheflowofchildcareintheremainingstagesof diagnosis andof intervention,which iscriticaltoevaluate theeffectivenessofaprogramforearlyidentification.
Inthestudypopulation,13%ofchildrenhadarisk indica-torforhearingimpairment.ThisfindingissimilartoBrazilian studies in Vila Velha and Maceió, which found 12.6% and 10.0%ofchildrenwithHIRI,respectively.11,12
In the present study, it was observed that the risk of failing the screening is 2.4 times higher in the group of children with HIRI. A study in a SãoPaulo maternity unit foundanassociationoffailureinthehearingscreeningtest withthefollowingindicators:prematurity,familyhistoryof hearing loss, andcongenital syndromesigns.21 The
litera-turesuggeststhattheprevalenceofhearinglossisgreater inchildrenwithHIRI.22 Inastudyof53,121newborns
sub-mittedtoascreeningtestinRhodeIsland,USA,aprevalence ofhearinglossof2.12:1000wasfound,risingto9.75:1000 inthegroupofchildrenwithoneormoreHIRI.23 InTurkey,
a studydemonstrated afrequency of 2.9% ofhearing loss in newborns withHIRI, and of 0.19%in newborns without HIRI.24
Theliteraturerecommendsthatchildrenwithrisk indi-cator(s) for hearing loss undergo hearing and language developmentmonitoringuntil2or3yearsofage,duetoa greaterchanceofdevelopingaprogressiveloss.8,10In
accor-dancewiththatestablishedintheNHSSP,theNHSRSsshould reassesschildren withHIRIsixmonths aftertheNHStest, both to monitor progressive losses and to identify cases of retrocochlear loss not identified by the measurement of otoacoustic emissions nor by the observation of audi-torybehaviorintheneonatalperiod.Inthepresentstudy, only32.3%ofchildren attendedtheHIRIrevaluation,with amedian ageof209 days(approximately7months).Most studies have not submitted attendance data for reassess-ment,probablybecausetheydidnotincludethisphasein their assistanceprotocols.In astudy in VilaVelha, where NHS test protocols included a semiannual auditory moni-toringofchildrenwithHIRIoveraperiodofthreeyears,a returnindexof52.6%inthefirstreassessmentandof10.3% bythesecondyearwasfound.12Fromtheseresults,onecan
suggestingtheneedtoinvestinactivesearchingstrategies to ensure the return of the child. Thus, the involvement of the BHUs becomes essential for continuity in hearing healthcare of children. Continuing actions targeting fam-ilyorientation,andprofessionalguidanceonthepossibility of developing hearingloss andits consequences,can also reducetheabsenteeism.
The AAP recommends that, in biphasic screening pro-grams,the expectedrateof referral tothe second phase (retest)shouldfallbetween5%and20%ofthetotalof chil-dren assessed. In this study, a rate of 8% of referral for retestingwasfound,whichis inagreementwiththat pro-posedbytheAAP.However,somescreeningprogramswith different evaluation methodologies obtained rates <3% of referralstothesecond phase,25 suggesting thepossibility,
oreventheneed,toreducethisrate.Althoughtheresults ofNHStestprogramsintheliteratureshowwidevariation, mostofthestudiesreportedratesofreferralforretesting between6.0%and10.0%.12,26
The high rate of children who fail the NHS test has become a major concernamong professionals. Highrates ofunnecessaryreferralsincreasethecostoftheprograms, considering the need for skilledprofessionalsand theuse of highly complex procedures,19,27 as well as promoting
increasedabsenteeismatvariousstagesoftheprocess. The proportionof failures in the firststage of an NHS testprogramcanbeinfluencedbyseveralfactors,including theevaluationprotocolused,27professionalexperience,16,19
physiologicalconditionsoftheexternalear,28andthechild’s
ageatthetimeofevaluation.29
Inthis study,thosechildrenwhofailedtheNHStestas wellastheretestwereolderthanthosewhopassed.These resultsareconsistentwithfindingsof astudyinNigeria.16
Studieshavebeenperformedwiththeaimtodefinethebest timeforthehearingscreeningtestinnewborns.In Luxem-bourg,2496neonatesundergoingNHStestwereevaluated, anditwasobservedthattheproportionofunchangedresults rosefrom67.0%fornewbornsbetween24and48hoflifeto 87.6%forthosewith>72h,andto95.1%forthosebetween the4thand5thdayoflife.29
DespitetherecommendationtoperformtheNHStestin thefirstmonth,themeasurementofotoacousticemissions in thefirst hoursof life hasnot been recommended,due to the possible presence of vernix in the external earof thenewborn,jeopardizingthequalityoftheexamination.30
Datafromthisstudyalsosuggestthatthetestresultisalso influencedbytheageofthechild.Itisknownthatthe mea-surementofotoacousticemissionsisstronglyinfluencedby the clinical condition of theinfant, for instance, conduc-tionimpairmentsandgastroesophagealreflux,30andalsois
influencedbytheinternalnoise,morecommoninthemost activechildren. It is possible that infants aremore likely topresenttheseclinicalconditions,andthustheyaremost likelytofailanNHStest.Suchargumentsreiteratetheneed for performingthe NHStest in thefirst30 daysof child’s life.
AccordingtotherecommendationoftheAAP,thenewly implemented biphasic NHSP should reach more than 70% attendanceinitssecondphase.Programswithlonger imple-mentation must achieve a rate greater than 90%. In the presentstudy,inthefirstyearofoperation,71%attendance fortheretestphasewasobserved.Similarvalueswerefound
inastudyofSãoPaulo(73.1%).31Betterresultswerefound
inastudyconductedinSpain(95.9%).26
The investment in follow-up systems to increase the attendancerateforretestandalsointhediagnosticphase hasbeen a majorchallengefor screeningprograms, even in developed countrieswith structuredprograms for over adecade.6,7The absenteeisminsubsequentphases tothe
NHStest seriously jeopardize the diagnosis and the early intervention for children with hearing loss.3,6 The
atten-dancerateforretestisanindicatorthatmeasurestheactual adherenceofthefamilyandtheeffectivenessofthelogistics forchild’sreturnimplementedbytheprogram.3
Studies have been conducted to determine the varia-bles that can influence family adherence. A statistically significantdecreaseofadherencewasobservedingroupsof childrenolderthan30days,16non-firstborninfants,14,16and
newbornswithunmarriedmothersinthefamily,withalow frequencyofprenatalcareandalowlevelofeducation.14
Inthepresentqualitativeanalysis,thefollowingwere con-sidered asbarriers toretest: restrictionof opening hours tothepublic,lackofinformationabouttheimportanceof the NHS test, lack of material resources to travel tothe placeofexamination,theneedtobringallchildrentothe placeoftheexam,lackofsomeonetoassistwiththeolder children, the home observation of the child’s reaction to soundstimuli ofgreater intensity, andespecially thefact thatpediatricianscaringforthechilddonotreiteratethe needfor attendancetoretests.14 Inthisrespect,the
par-ticipationof all professionals involved in neonatalcare is essential, either in the maternity or in the BHU, so that thereisnoconflictintheguidelinesabouttheimportanceof returningforfurtherevaluation.Therefore,itisnecessary theresultsoftheexaminationanditsrespectiveconductare properlyrecorded,preferablyinthechildhealthbooklet,to facilitateinterdisciplinarywork.32
Although the absenteeism in this study was significant (29%intheretestphaseand67.7% atre-assessment),the informationavailable allowedonlyascertainingthat there wasnoinfluenceoftheoriginofthefamily,thechild’sage, andthepresenceofsomeriskindicatorforhearinglossin thechild’sattendancetoretest.
Thepercentageofchildrenreferredfordiagnosisinthis study(2.1%), while agreeing withthe recommendationof the American Academy of Pediatrics, may be underesti-mated,whenconsidering thehigh absenteeismduringthe retest.Values of referral for diagnosis similarto thoseof thepresentstudywerefoundinSãoPaulo,where1.1% refer-ralfordiagnosiswasobserved,withanabsenteeismrateof 26.9%intheretest.31
Given the absence of information from post-retest stages,thisstudywaslimitedtotheanalysisofdatauntil thetimeofreferralfordiagnosis.Theliteratureisclearin statingthat earlydetectionalone does notguaranteethe auditorydevelopmentofthechildwithhearingloss,andan effectivetherapeuticinterventionisneeded,aswellasan interfacewiththeeducationalsystem.1
Since 1999, the AAP and the JCIH have recommended theimplementationofscreeningprogramswiththeuseof an information system for the consolidation and analysis of data. This same recommendation has been reiter-ated by severalstudies andby national and international organizations.10Theabsenceofacomputerizedsystemhas
clearly hampered or even made it impossible to obtain theresultsofassistance.Lack ofknowledgeof thehealth trajectoryof children after referral to diagnosis seriously jeopardizesthe measurement of the effectiveness of the NHSP,i.e.,theidentificationofthenumberofchildrenwith hearinglosswhohaveachievedgoodhearingfunctionand languagedevelopment.Thelackofinformationalso jeopar-dizestheprocessofevaluationofprogramsbyitsmanagers andhindersthebettertargetingofresourcesandof correc-tiveactionsforensuringacomprehensivecareforchildren withhearingimpairment.
Regionalization strategies for reference services may evenbeconsidered,sothattheexamsarescheduledinthe servicewithgreater easeof accessfor thefamily. Educa-tionalprogramsfor the patientpopulation and for health professionals about the importance of early detection of hearingloss arefundamental to theunderstanding of the necessity of the child’s attendance, not only at the first examination, but also at the retest and/or reassessment phase,ifneeded.
Futurestudiesarenecessarytoknownotonlythe evo-lution of the NHSRS work process, but also the quality indicatorsofotherNHSservicesinthemunicipalityandin thestate.Theknowledgeofthelimitationsandadvancesof theseprogramsiscriticaltothefoundationoftheactionsof therespectivelevelsofmanagement.Strategiesfor imple-mentation of integration systems among the service and otherpointsofcareofthehearingcarenetworkareessential fortheconsolidationandanalysisofdata,toprovide knowl-edgeofoneofthemainqualityindicatorsproposedbythe scientificcommunity:thepercentageofchildrenwith hear-ingimpairmentatbirthsubmittedtoanintervention,i.e., theadaptationofindividualhearingaidsandspeech ther-apy,inatimelymanner,forthesatisfactorydevelopmentof orallanguage.
Conclusion
The NHSRS where this study was conducted has reached threeofthefourindicatorsofqualityreviewed.Therates of referral to retest, retest attendance, and referral for diagnosisareinagreementwiththoserecommendedbythe scientificcommunity. However,theNHS test wasnot per-formed withinthe frameof timerecommendedin 35% of thechildren,suggesting theneed for actionsthatprovide aneasieraccesstotheexaminlesstime.Althoughover70% attendancewasachievedin theretestin thefirstyear of theprogram,theauthorsexpectmorethan90%attendance inthesubsequentperiods.
Thus,investmentsinactivesearchstrategiesandinthe studyofevaluationprotocolsthatreducethenumberof chil-drenreferredforretestingareimportant.Theintegrationof children’shearinghealthinprimarycareactionsshouldbe emphasized,toensurethecontinuityofcare.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Yoshinaga-Itano C. Levels of evidence: universal newborn hearingscreening(UNHS)andearlyhearingdetectionand inter-ventionsystems(EHDI).JCommunDisord.2004;37:451---65. 2.Aurélio FS, Tochetto TM. Triagem auditiva neonatal:
exper-iências de diferentes países. Arq Int Otorrinolaringol. 2010;14:355---63.
3.OlusanyaBO,SwanepoeldeW,ChapchapMJ,CastilloS,Habib H,MukariSZ,etal.Progresstowardsearlydetectionservices forinfantswithhearinglossindevelopingcountries.BMCHealth ServRes.2007:7---14.
4.BevilacquaMC,MeloTM,MorettinM,LopesAC.Aavaliac¸ãode servic¸osemAudiologia:concepc¸õeseperspectivas.RevSocBras Fonoaudiol.2009;14:421---6.
5.MinistériodaSaúde--- Brasil.ProgramaNacionaldeAvaliac¸ãode Servic¸osdeSaúde;2007.
6.GaffneyM,GreenDR,GaffneyC.Newbornhearingscreening andfollow-up:arechildrenreceivingrecommendedservices? PublicHealthRep.2010;125:199---207.
7.ShulmanS,BesculidesM,SaltzmanA,IreysH,WhiteKR, Fors-manI.Evaluationoftheuniversalnewbornhearingscreening andinterventionprogram.Pediatrics.2010;126Suppl1:S19---27. 8.MinasGerais.SecretariadeEstadodeSaúde.Resoluc¸ãoSESn 1321de18deoutubrode2007. InstituioPrograma Estadual deTriagemAuditivaNeonatal,definecritérios,normas opera-cionaiseprocedimentosparaaprestac¸ãodeservic¸os.Imprensa OficialdoEstadodeMinasGerais;2007.
9.Erenberg A, Lemons J, Sia C, Trunkel D, Ziring P.Newborn andinfanthearingloss:detectionandintervention.American AcademyofPediatrics.TaskForceonNewbornandInfant Hear-ing,1998---1999.Pediatrics.1999;103:527---30.
10.AmericanAcademyofPediatricsJCIH.Year2007position state-ment:principlesandguidelinesforearlyhearingdetectionand interventionprograms.Pediatrics.2007;120:898---921. 11.LewisDR,Marone SAM,Mendes BCA, CruzOLM, Nóbrega M.
Comitêmultiprofissionalem saúdeauditiva:COMUSA.Braz J Otorhinolaryngol.2010;76:121---8.
12.Barreira-Nielsen C, Futuro Neto HA, Gattaz G. Processo de implantac¸ãodePrograma deSaúdeAuditivaem duas mater-nidadespúblicas.RevSocBrasFonoaudiol.2007;12:99---105. 13.DantasMBS,AnjosCAL,CamboimED,PimentelMCR.Resultados
deumprogramadetriagemauditivaneonatalemMaceió.Braz JOtorhinolaryngol.2009;75:58---63.
14.FernandesJC,NozawaMR.Estudodaefetividadedeum pro-grama de triagem auditiva neonatal universal. Ciênc Saúde Coletiva.2010;15:353---61.
15.Griz S, Merces G, Menezes D, Lima ML. Newborn hearing screening:anoutpatientmodel.IntJPediatrOtorhinolaryngol. 2009;73:1---7.
16.OlusanyaBO,EbuehiOM,SomefunAO.Universalinfant hear-ing screening programme ina community withpredominant non-hospitalbirths:athree-yearexperience.JEpidemiol Com-munityHealth.2009;63:481---7.
ofhospital-andcommunity-basedscreening.BMCHealthServ Res.2006:6---14.
18.MinistériodaSaúde---Brasil.DATASUS.Informac¸õesdeSaúde. 19.MehlAL,ThomsonV.TheColoradonewbornhearingscreening
project,1992---1999:onthethresholdofeffective population-based universal newborn hearing screening. Pediatrics. 2002;109:E7.
20.NoronhaJC.Coberturauniversaldesaúde:comomisturar con-ceitos,confundirobjetivos,abandonar princípios.Cad Saúde Pública.2013;29:847---9.
21.PereiraPKS,MartinsAS,VieiraMR,AzevedoMF.Programade triagemauditivaneonatal:associac¸ãoentreperdaauditivae fatoresderisco.Pró-FonoRAtualCient.2007;19:267---78. 22.TiensoliLO,GoulartLMHF,ResendeLM,ColosimoEA.Triagem
auditivaemhospitalpúblicodeBeloHorizonte,MinasGerais. Brasil:deficiênciaauditivaeseusfatoresderiscoemneonatos elactentes.CadSaúdePública.2007;23:1431---41.
23.VohrBR,CartyLM,MoorePE,LetourneauK.TheRhodeIsland HearingAssessmentProgram:experiencewithstatewide hear-ingscreening(1993---1996).JPediatr.1998;133:353---7. 24.ArslanS,IsikAU,ImamogiuM,TopbasM,AslanY,UrolA.
Uni-versalnewbornhearingscreening:automatedtransientevoked otoacousticemissions.B-ENT.2013;9:122---31.
25.BasuS,EvansKL,OwenM,HarbotleT.OutcomeofNewborn HearingScreeningProgrammedeliveredbyhealthvisitors.Child CareHealthDev.2008;34:642---7.
26.Angulo CM, Linos AGA, Miera CB, Gutiérrez AM, Aja FJS, Benito JB, et al. Programa de detección precoz de la hipoacusia en neonatos en cantabria. Resultados delprimer a˜no de funcionamiento. Acta Otorrinolaringol Esp. 2003;54: 475---82.
27.FreitasVS,AlvarengaKF,BevilacquaMC,MartinezMAN,Costa OA.Análisecríticadetrêsprotocolosdetriagemauditiva neona-tal.Pró-FonoRAtualCient.2009;21:201---6.
28.Marques TR, Mendes PC, Bochnia CFP, Jacob LCB, Roggia SM, Marques JM. Triagem Auditiva Neonatal: relac¸ão entre banho eíndice dereteste.BrazJOtorhinolaryngol.2008;74: 375---81.
29.PanosettiE,ShiBX,EloyJP,OrbandD,RasqueE.Oto-émissions provoquéesàlanaissance:l’expérienceluxembourgeoise.Arch Pediatr.1999;6:353---5.
30.SimonekMCS,AzevedoMF.Respostasfalso-positivasnatriagem auditiva neonataluniversal:possíveis causas.Revista CEFAC. 2011;13:292---8.
31.DuranteAS,CarvalloRMM,CostaMTZ,CianciarulloMA,Voegels RL, TakahashiGM, et al. A implementac¸ão de programa de triagem auditiva neonatal universal em um hospital univer-sitáriobrasileiro.Pediatria(SãoPaulo).2004;26:78---84. 32.AlvesCRL,LasmarLMLBF,GoulartLMHF,AlvimCG,MacielGVR,