scoping review
Danielle Yuri Takaui Saito 1, Elma Lourdes Campos Pavone Zoboli 2
Abstract
The ageing populaion has increased the incidence of chronic health condiions, requiring the inclusion of diferent levels of palliaive care (PC) in diferent parts of the health system, including the Primary Health Care (PHC). This new reality might interfere with the ethical issues of PHC. This research aimed to idenify, from the point of view of health professionals, the ethical problems which arise from the palliaive care in PHC. We carried out a systemaic review in PubMed, EMBASE, LILACS, CINAHL, using the descriptors ‘ethics’, ‘bioethic’s, ‘Primary Health Care’ and ‘Palliaive Care’. We found 3,915 aricles of which 16 remained ater analyses. The ethical problems found were: lack of resources; lack of knowledge about palliaive care; lack of communica -ion skills; diiculty in establishing limits in clinical rela-ionship; work overload; lack of support from referral services. These problems, in general are similar to those experienced in the PHC but with diferences in spe -ciic situaions. The incorporaion of palliaive care to the Primary Health Care spe-ciic guidelines and training as well as the custom of shared and co-responsible care.
Keywords:Palliaive Care. Chronic Disease. Primary Health Care. End-of-life. Bioethics. Ethics.
Resumo
Cuidados paliaivos e a atenção primária à saúde: scoping review
O envelhecimento da população aumentou a incidência de doenças crônicas, demandando a inserção dos cuidados paliaivos (CP) em diferentes níveis da rede, incluindo a atenção primária à saúde (APS). Isso po -derá interferir nas questões éicas da APS. A presente pesquisa teve como objeivo ideniicar, na visão dos proissionais de saúde, os problemas éicos decorrentes da práica dos CP na APS. Fez-se revisão sistemáica nas bases PubMed, Embase, Lilacs, CINAHL, com os descritores “éica”, “bioéica”, “atenção primária à saú -de” e “cuidados paliaivos”. Localizaram-se 3.915 arigos, restando 16, após a análise. Os problemas éicos detectados foram: escassez de recursos; desconhecimento sobre CP; falta de habilidades comunicacionais; diiculdade de estabelecer limites na relação clínica; sobrecarga de trabalho; falta de apoio dos serviços de referência. Na abrangência, esses problemas assemelham-se aos vividos na APS, com diferenças nas situações especíicas. Para incorporar os CP na APS, são necessárias normaizações e formação especíicas, além da cultura do cuidado comparilhado e corresponsável.
Palavras-chave: Cuidados paliaivos. Doença crônica. Atenção primária à saúde. Terminalidade de vida. Bioéica. Éica.
Resumen
Los cuidados paliaivos y la atención primaria de salud: scoping review
El envejecimiento poblacional aumentó las enfermedades crónicas, planteando la inclusión de diferentes ni -veles de cuidados paliaivos (CP) en la red sanitaria, incluyendo la Atención Primaria de Salud (APS). Esto puede interferir con la éica de la APS. Nuestra invesigación objeivó ideniicar, según los profesionales, cua -les son los problemas éicos de los CP en la APS. La revisión sistemáica en PubMed, EMBASE, LILACS, CINAHL, con descriptores “éica”, “bioéica”, “Atención Primaria de Salud” y “Cuidados Paliaivos”, ideniicó 3.915 arículos, restando 16, después del análisis. Los problemas éicos fueron: falta de recursos; desconocimiento en CP; falta de habilidades comunicacionales; diicultad con los límites de la relación clínica; sobrecarga de trabajo; insuiciente soporte de servicios de referencia. En general, los problemas se asemejan a los experi -mentados en la APS, con las peculiaridades de situaciones más especíicas. La incorporación del CP en la APS requiere: directrices y formación especíicas; cultura de la atención comparida y corresponsabilidad. Palabras-clave: Cuidados Paliaivos. Enfermedad Crónica. Atención Primaria de Salud. Fin de la vida. Bioéica. Éica.
1. Mestrandadanielle.saito@usp.br 2. Doutora elma@usp.br – Universidade de São Paulo, São Paulo/SP, Brasil.
Correspondência
Danielle Yuri Takaui Saito – Programa de Pós-Graduação da Escola de Enfermagem da Universidade de São Paulo. Rua Dr. Enéas de Carvalho Aguiar, 419 CEP 05403-000. São Paulo/SP, Brasil.
Declaram não haver conlito de interesse.
R
esear
The demographic and epidemiological transi -ion has changed the morbidity and mortality proile of the Brazilian populaion. Infecious diseases were the most frequent causes of death unil the irst half of the twenieth century but, currently, noncommu -nicable chronic diseases are epidemic, in paricular cardiovascular diseases, cancer and type 2 diabe -tes. The highest morbidity and mortality rates, due to these diseases, grow each year and account for about 70% of the health spending in the country 1.
Chronic health condiions, because of their progressive and degeneraive evoluion, demand coninuous and ongoing assistance - which includes palliaive care- in various parts of the health care system (Rede de Atencao a Saude -RAS). The conin -ued assistance in chronic health condiions involves atenion to the latent moments of the disease when it evolves without percepion of the person who will sufer the deterioraion of quality of life 2.
It is a challenge for the Uniied Health System (Abbreviated as SUS in Brazil - Sistema Unico de Saude) and the Primary Health Care (PHC) to reorga -nise themselves in order to meet the current health needs and demands of an ageing populaion with chronic diseases. Historically, the health systems were organised and focused on responding to acute condiions or episodes of worsening of chronic con -diions 2.
Palliaive care has the objecive of promoing a beter quality of life, through therapeuic projects planned by a mulidisciplinary team, for people with chronic degeneraive diseases or are in a terminal state. The care is not restricted to speciic contexts and insituions and must be performed at every level of the health system. Specialised Palliaive Care is an assignment atributed to specialists in hospi -ces, while primary health care provides the overall palliaive care. All health workers should be trained for the palliaive care approach, since this kind of atenion needs to be established early, from the moment of the diagnosis of chronic health condi -ions, and aimed at a good quality of life 3.
The main challenge for the palliaive care at an internaional level is to go beyond the care of ter -minally ill paients with cancer. It is proposed that palliaive cases should be: introduced as soon as possible in caring for diseases, not only during ter -minal stages; go beyond the physical dimensions of care and cover the social, psychological and exis -tenial aspects; span from hospices and specialised services to the general services in hospitals and in the community, disseminaing in the community in
order to support caregivers and paient’s relaives 3.
The best results in providing palliaive care de -pend on the integrated operaion of services as well as the alliance between specialists, generalists and home caregivers 4. Given the demographic and ep
-idemiological transiion, the demand for palliaive care in the Primary Health Care became a reality, so much so that both teams of the Family Health Strat -egy (abbreviated as ESF in Brazi) face situaions of atenion linked to the death process 5.
However, this demand for palliaive care at a local level is not properly evaluated or esimated. Nevertheless, it is possible to foresee the “impact” that it would bring to ethical issues experienced in the primary health care. But what would this impact be?
Method
This is a systemaic review based on the sco -ping study or sco-ping literature reviews. The strategy called scoping review (SR) consists of a systemaic review, exploratory, aimed at mapping scieniic producion and relevant studies in a given area. The scoping review has a comprehensive approach, as the search quesion is extensive and the evaluaion of studies’ quality is less strict 6 .
In this review, we used the PICo strategy for the formulaion of the quesion, “P” being for pop -ulaion , “I” for phenomenum of interest , “Co” for context . Adjusing the object of study to the PICO strategy, the guiding quesion is: What are the ethi -cal issues, for health professionals, in palliaive care in the primary health care ? In order to ensure a cov -erage adequate to a Scoping review, the gathering of informaion used two search strategies. The irst was held in the databases Lilacs, Embase, CINAHL and PubMed, using the descriptors “ethics,” “bio -ethics” and “primary health care”.
The second search used the descriptors “eth -ics,” “bioethics” and “palliaive care”. The data bases were the same as those from the irst search, with the excepion of Embase, due to the the University of São Paulo (Universidade de Sao Paulo-USP) hav -ing disconinued its subscripion to that data base. Both searches were limited to the scieniic pro-ducion in the period from December 31, 2002 to January 1, 2013. We included aricles in Portuguese, Spanish and English. When the aricles contained empirical studies, the subjects of interest were healthcare professionals of the Primary Health Care. The inclusion criteria were aricles related to ethical
R
esear
and operaional conlicts as well as the relaionships of the professionals with the users of the health sys -tem. Studies that did not meet these criteria were excluded from the review.
When the aricles were not fully available in the databases, we tried to obtain them through the Portal of Magazines of the USP’s libraries, the Portal of pe -riodicals of the Coordinaion for the Improvement of Higher Educaion Personnel (abbreviated as Capes in Brazil -Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) or direct contact with the author by e-mail or through Research Gate. The aricles were not considered in the survey if, ater these atempts, we couldn’t have access to the text in its whole.
We introduced, in addiion to the search in those databases and in accordance with the inclu -sion criteria, aricles from the private collecion of one of the authors, who specialises in the bioeth -ics area in the Primary Health Care and already had works collected in previous searches.
We evaluated, for the systemaisaion of data, the following: periodical (itle, volume, number and year); itle of the aricle; authorship; origin of the ar -icle (thesis, dissertaion or monograph); existence of funding for the research; locaion of the study
(insituion, country, state and city); goals (aricle or research); method (type of research, sample, paric -ipants, seing, data analysis); results; reference to ethical problems concerning palliaive care the in primary health care.
The aricles were ideniied with leters and numbers, according to the database used and the sequence in which they were found. One example: P1 is the irst study taken from the PubMed data -base, and so forth.
Results
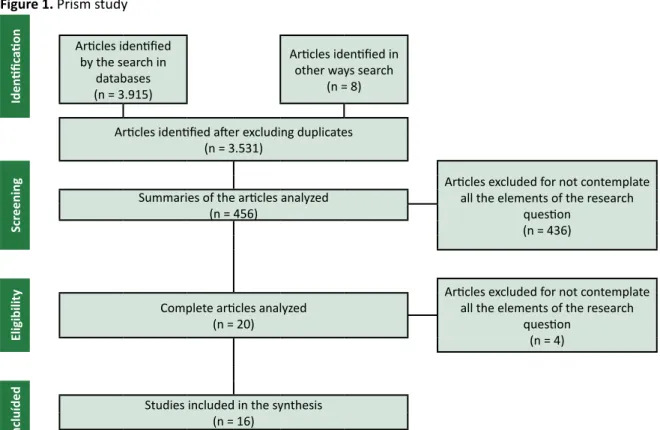
The irst search strategy ideniied 2,366 stu -dies; the second search ideniied 1,549 studies, besides 8 aricles taken from the private collecion of one of the authors. The Prisma (preferred report -ing items for systemaic reviews and meta-analyses) is in Figure 1. The screening covered the analysis steps according to their itles and abstracts. Based on the itle, 3,075 aricles were excluded, remaining then 456 for analysis of the abstracts. The 16 ari -cles included in the review refer to 15 studies, since the A11 and A12 have results which are diferent as -pects of the same research.
Figure 1. Prism study
Iden
iic
aion Aricles ideniied by the search in
databases (n = 3.915)
Aricles ideniied in other ways search
(n = 8)
Aricles ideniied ater excluding duplicates (n = 3.531)
Scr
eening
Aricles excluded for not contemplate all the elements of the research
quesion (n = 436) Summaries of the aricles analyzed
(n = 456)
Eligibility
Aricles excluded for not contemplate all the elements of the research
quesion (n = 4) Complete aricles analyzed
(n = 20)
Incluíded
Studies included in the synthesis (n = 16)
Source: Moher D, Liberai A, Tetzlaf J, Altman DG, The PRISMA Group (2009) 7.
R
esear
The table 1, annexed to the end of this paper, shows the included aricles and their respecive au -thors as well as original locaions of the study. The Table 2, also presented as an annex, exposes the ethical problems found in each aricle included in the review.
Diferent scenarios in which palliaive care are provided afect signiicantly, the manifestaion and the kind of ethical quesion, being necessary to em -phasise that such problems are inextricably linked to the peculiariies of each service. Aricle E1, the aim of which was to analyse ethical problems expe -rienced by paediatricians whilst associaing them to their workplace, found that the 16 UBS doctors (UBS stands for Unidade Basica de Saude - Health system Basic Unit) had no ethical problems relaing to end-of-life care 8. Despite these peculiariies, the ethical issues are focused on decision making, the fuility of therapy, the paient’s autonomy and nursing work 9.
The non-resuscitaion orders and the choice made by paients not to be treated, with considera -ion of their quality of life, stand out in the decis-ion making . The usefulness of treatments is determined by the expectaion of beneits. Decisions to prolong life are avoided. As for the autonomy, paients must be well informed about their situaion because many euthanasia requests result from the loss of control about the care. In their work, the nurses feel respon -sible for defending the rights of paients and stand irm in their defence, to the point of even confroning the medical team. Nevertheless, these professionals complain about “diicult paients” who are never saisied with the nursing work. In these situaions, they need to make an efort to feel sympathy for those paients, besides remaining moivated to watch them and talk to them about death 9.
Primary health care professionals feel the duty to accompany paients in their last days of life 10. Doctors jusify such an obligaion as a way
to compensate for the powerlessness they feel be -cause of the impossibility to provide to paients in palliaive care a treatment as efecive as the one for paients with normal life expectancy. Therefore they devote more ime and atenion to paients in the palliaive care 11.
When it comes to terminally ill paients with cardio-respiratory diseases, the feeling of impo -tence of physicians increases. Because they were insuiciently trained to ofer palliaive care in the terminal stage of this class of diseases, doctors rec -ognise that their help is lower in these cases than in the inal stages of cancer. Therefore, in these situa -ions, professionals no longer inform paients that
they are in the inal stage of their illness 12. If a doc -tor from the Primary Health Care did not follow the curaive treatment phase, then the communicaion about the transfer to palliaive care is more com -plicated 11. Physicians ind it diicult to determine whether the person is terminally ill in the absence of a diagnosis of underlying malignant disease 12.
Doctors believe that to discuss palliaive care is ime consuming and therefore it is unlikely that they will have this kind of conversaion with pa -ients. They consider that this discussion is not beneicial to the paient, as it is exhausing and uncomfortable 13. In turn, nurses recognise the im
-portance of talking about death with paients who have no chance of a cure, although they only have this kind of conversaion when they are willing to or when there is an opportunity 14. The lack of truth
-fulness whilst talking to paients and their families about their actual health situaion is another ethical problem ideniied in the relaionship and communi -caion of primary health care professionals working in palliaive care 15. Besides the lack of informaion,
professionals report breach of conideniality in the treatment and prognosis of paients 16.
This deiciency in the communicaion and relaionship between professionals and paients as well as their families may explain why most of Primary Health Care doctors were unaware of the inal wishes of their paients, even when they had already expressed those wishes in anicipated direc -ives in another health service. Another example of the consequence of inefecive communicaion hap -pens when paients say that they had not expressed any anicipated direcive whilst doctors claim oth -erwise. Although the review leaves unclear the reason of this disagreement, at least it is indicaive of communicaion problems 17. Nurses atribute the
inadequate communicaion with paients and fam -ilies to their poor training in this requirement 15. In
the United States, anicipated direcives are legal documents, not clinical documents; that is, they are a paricular iniiaive of the paient or anyone else, regardless of their health status 17.
Communicaion also fails between doctors and nurses, among members of the Primary Health care team 18,19 and teams of diferent services 12,16,20.
Primary Health Care doctors complain that the specialists do not share informaion 20. In cases of
cardiorespiratory diseases, Primary Health Care physicians feel frustrated for failing to take full care of the paients as, during the worsening crisis of un -derlying diseases, the specialists of the hospital are the ones who manage the palliaive care.
R
esear
Primary health care doctors say that medical specialists fail in the transmission of informaion, since they do not inform the decisions taken at the hospital about the paients’ treatment regimens who are under their care. As a result, they lose con -idence in the hospital which, in addiion to failing to communicate about treatments and intervenions, oten gets in to conlict with the prescripions al -ready given by primary health care doctors . Conlicts arising from inadequate communicaion between services are worse in cases of cancer paients who paricipate in clinical trials because the team of re -searchers prohibits that the primary health care and the hospital modify or introduce any conduct with -out their consent 12.
Nurses from the primary health care see in doctors a reluctance to accept new iniiaives and to respond to the needs of paients and requests from the nurses. Nurses get an idea about the “good” or “bad” doctor based on the willingness of that pro -fessional to receive and respond to requests from paients or the nursing staf and also on the respect with which doctors treat other professionals. Thus, in the assessing of the nurses, technical experise and medical knowledge are less important than in -terpersonal relaionships 21.22.
For nurses, the quality of interpersonal rela -ionships and the percepion that each professional has about the performance of other professionals are factors that inluence teamwork and the refer -ral of users to another services. The team cohesion depends more on the relaionships among its mem -bers than in the care to be provided to the user. For doctors, the negoiaing issues and interpersonal relaionships count less on the assessment made of the professionals. This could be due to the difer -ence of authority between doctors and nurses. The quesion of the leadership of doctors became clear in the focus groups of aricles: nurses did not give their opinions, and the groups were to be represent -ed, formally or informally, by a doctor, who chooses the day of the meeing and would eventually lead it, direcing the discussion 21.22.
The excessive importance atached to inter -professional relaionships is evident when Primary health care professionals assess the beneits of in -troducing a program to improve the quality of care solely on the basis of those relaions, without taking into account the interacions with paients and the impact on the direct care. When professionals from the primary health care need to refer the paient to specialists, and make that decision considering only the relaionship with these professionals, it is pos
-sible that they will be successful. In such cases, it would indicate the possibility of obtaining faciliies now and in the future, which ulimately inluence the judgment that the primary health care team makes of the professionals from the specialised services 21,22.
Nurses don’t have availability for palliaive care intervenions 15. Insecurity, lack of access to
emergency drugs, the lack of interpreters to atend the aboriginal populaion, the high cost of overime and the limited cell phone coverage are aspects that jusify the non-availability of these professionals to work at night. They claim that an amendment of the legislaion in order to allow nurses to make the as -sessment of death could increase the paricipaion of these professionals in the palliaive care, espe -cially in shits ater opening hours of the primary health care 18.
Doctors of primary health care, in turn, also menion some obstacles to their involvement with palliaive care: lack of ime; home visits; personal or family commitments; lack of interest; unavailability for work ater hours; lack of knowledge of pallia -ive care; emoional reasons, and lack of support of specialists 20. The nurses agree that the limited
availability of doctors to work ater hours is one of the limiing factors for palliaive care in the primary health care system. In turn, doctors claim that the unavailability of nurses for work ater hours is also a limiing factor 18.
Doctors and nurses have proposed some strategies for improvement of work in home-based palliaive care: regular mulidisciplinary meeings; easiness of referral to specialised services of pal -liaive care; more nurses for home visits; nursing training in telephone service ater the opening hours of the primary health care and, especially, the devel -opment and adopion of standardised protocols for the plan of treatment concerning each paient 18.
Professionals in the primary health care in -volved in palliaive care wish to coninue in the program, but the scarcity of resources, lack of or -ganisaion and management of services cause overload 10,16. The lack of resources and referral ser
-vices, the work overload and lack of space to discuss the experiences in the care of dying paients are fac -tors that make nurses more prone to psychological illnesses, besides creaing frustraion among them, because they can not provide care of good quality23.
The diiculty of access to referral services, mainly the ones specialised in palliaive care, is higher for paients with cardiorespiratory disease and lower for paients with cancer, as reported by nurses and doctors in one of the studies 12.
R
esear
Nurses and doctors ind it diicult to set limits to the relaionship with terminally ill paients and their families 15,23. The close proximity of profes
-sionals to users of the primary health care creates intense bonds, which causes distress to nurses 11,23.
Primary health care professionals go to the point of giving the number of their personal phones to fa -mily members of paients in palliaive care so they can get in touch if necessary. Those professionals also do voluntary home visits ater working hours 10.
This atachment is also present when families and caregivers require acions outside the scope of the competence of the primary health care when the family requests, for example, constant visits to the paient 23.
The proximity between primary health care professionals and paients in palliaive care inter -feres with communicaion of the truth about the paient’s health condiion. Some PHC doctors do not report poor prognosis to paients for fear that if they do, paients and/or family will nurture resentment towards them, leaving this task to the specialists who will have to watch the paients unil the end 9.
Doctors report that fatalisic thoughts, insecuri -ty and helplessness of caregivers tend to compromise the autonomy of paients, making them dependent and suscepible to emoional sufering 11. Therefore, while recognising the importance of family support, nurses believe that such support someimes hinders the care 14. They also menion suspicion of physical,
psychological and economical abuse praciced by the paient’s family towards the paient. 16. When faced
with abuse, carelessness and neglect by family mem -bers, nurses change their behaviour in the atenion to the paient , restricing their care to an exclusively technical scope.
As for the family members who mistreat pa -ients, nurses do not assess that they also need care 23. Doctors feel lack of support for dealing with
ethical issues related to palliaive care 11 and assur -ance of the coninuity of home care to paients, especially ater the opening hours of the primary health care services 18,19. They suggest courses on
standards and ethical values, including how to dis -cuss and confront problemaic situaions from an ethical point of view in the sphere of operaion of the primary health care staf 11.
Doctors’ lack of informaion about available services and resources in the community and in the primary health care ater opening hours contributes to the disconinuity of care for paients in palliaive care at home 18. Another factor is the poor cooper
-aion between teams and between professionals 19,
such as the absence of reports from nurses about intervenions in mulidisciplinary teams 15.
Doctors report that informal caregivers are the main collaborators in the provision of palliaive care at home 19. The relaionship between professionals of
the PHC and the family and informal caregivers is of poor quality, according to those professionals 16. The
nurses claim lack of condiions, ime and prepara -ion to accompany the mourning family and informal caregivers 15, while recognising their emoional suf
-fering 11.
The PHC professionals consider that the lack of their knowledge about palliaive care limits their aciviies 11, especially in the management of symp -toms 9,11,15,20 and complex clinical situaions 10,20. In
such cases, they base themselves on their accu -mulated clinical experience through professional pracice, but do not feel safe on the best approach to be adopted 10. Doctors menion the lack of ime to
devote to studies as an obstacle to their coninued training in palliaive care 18.
Doctors think that the most important aspect of palliaive care is more in the somaic domain than in psychosocial and spiritual grounds, which is why they rarely cooperate with religious ministers or dis -cuss spiritual issues with paients 19. Nurses also feel
unprepared to address spiritual or religious maters with paients, although they recognise the impor -tance of these talks at the inal stage of life 14.
When dying paients in home care ask PHC professionals about issues related to the search for the meaning of life, the professionals, though un -prepared, feel the duty to talk about it with paients and their family. Due to the prolonged coexistence of PHC professionals with the people in their care, many of them visit homes of friends and relaives of hospital’s paients. It is a peculiarity of the palliaive care in the PHC that is not as common in other areas of the Health System 9.
Doctors do not accept that ethical issues such as euthanasia can be solved by just good provision of palliaive care 11. In Sweden for example, even if rare -ly and despite couning with an excellent palliaive care service, doctors feel obliged to ofer euthanasia as a last resort due to unfavourable social condiions of some paients 9. This inding drew atenion of
the authors of this aricle, as it is diicult to guess what would be the unfavourable social condiions in Sweden, when we live in a country much poorer and socially uneven; however, the aricle included in the review does not specify those situaions.
R
esear
Discussion
Aitudes and skills necessary to provide high quality palliaive care overlap with those needed for opimal PHC: communicaion skills; understand -ing of reality and the peculiariies of the way of life of the paient; commitment to comprehensive and integrated care of the paient and family; atenion to the psychosocial and spiritual issues; emphasis on quality of life and independence of the paient; respect for the values, objecives and prioriies of paients in managing their own health condiion; provision of care in the community, depending on its cultural diversity; collaboraion with other pro -fessionals, including specialists. This way, it appears that the palliaive care and the PHC can, and should, be strengthened and also strengthen each other 24.
With regard to collaboraion among pro -fessionals, we need to face several challenges: conlict, ambiguity and overlapping of the roles of the professionals; inadequate communicaion, and leadership problems. The introducion of mulidis -ciplinary teams is a necessity for the provision of health services in order to increase the eiciency of care, especially the palliaive care. The team rep -resents a workspace focused on creaive problem solving, especially when the contribuion of all its professionals is based on respect and when there is a sense of responsibility towards the paient’s well-being 25.
This review found out that the type of ethical problem faced by professionals is closely related to the place where the palliaive care is provided, which reinforces the fact that such conlicts are inextricably linked to the peculiariies of each health service. Ethics in health care implies the acing of moral subjects in situaions of life and in the process of health-disease 26. As the situaions and processes
are peculiar to each subject, ethical issues deriving from them will also be speciic. Problems arise with their own characterisics in the various spheres of social life. Therefore, it is necessary to grasp, in each one of these contexts, the logic and modulaion of ethical principles which are peculiar to them 27.
At the prospect of introducing palliaive care in the PHC, especially through the ESF ( Abbrevia -ion, in Portuguese, of Estrategia Saude da Familia - Family Health Strategy) , two aspects are funda -mental: that the informal caregiver can rely on the provision of educaional aciviies aimed at the com -prehensive care of the paient 5 and the presence of
a professional in the team 28.
In the professional pracice of palliaive care at home, the informal caregivers consider important the knowledge, behaviour, communicaion skills and relaionship quality of the professionals with their paients and their family members 28. In general, the
ethical problems found by this review are close to the ethical issues experienced by PHC professionals and ideniied in other studies 26:
• Closer and more intense bond of PHC professio -nals with paients and families, which ends up creaing diiculies for the maintenance of impar -iality in clinical relaions
• Request of unnecessary or improper procedures, which in the case of the palliaive care, are consi -dered extraordinary or outside the scope or the potenial of the PHC
• Lack of collaboraion between teams, creaing dif -iculies in interprofessional work
• Lack of interprofessional respect, bad relaionship between members of the mulidisciplinary team • Lack of insituional support for the management
of ethical problems
• Work overload
• Disregard, by the reference and specialised ser -vices, of medical prescripions made by PHC doc -tors
• Lack of resources to carry out home visits
Considering the axes on which the ethical problems of PHC are placed, the ethical issues of the palliaive care, according to this review, focus on the pracice of the teams and their professional proile. The irst aspect presents ethical problems arising from the fragmentaion of the work of teams and diiculies in interdisciplinary pracice. The profes -sional proile covers the ethical issues related to the behaviour of the PHC Professionals 26.
These two axes are focused on ethical problems related to the following aspects: bad relaionship between the teams and diicult interprofessional communicaion, which interferes negaively with the quality of the care provided; training and prepa -raion insuicient to act in the PHC and palliaive care ; lack of communicaion skills of professionals for conversaions in the scope of the clinical re -laionship, the interprofessional relaionship and other points of atenion of the RAS (Abbreviaion of ‘Redes de Atencao a Saude” in Brazil - Health System Network) ; lack of shared informaion.
Apparently, the introducion of the palliaive care in the PHC will not interfere in the axes of ethi
-R
esear
cal problems in this area of care, even if the speciics and peculiariies of palliaive care reveal themselves in new situaions.
In their pracice, the ESF teams face the de -mand for palliaive care at the end of life stage and, earlier, in the diagnosis of chronic degeneraive dis -eases 5. As a result, the systemaisaion of guidelines
for palliaive care acions in the PHC is essenial, considering especially those aimed at addressing the ethical issues involved in this type of care.
Dying with dignity is a result of living with dig -nity; before the right to a digniied death, there is a right to a digniied life, with condiions to blossom fully - that means right to health 29. Thus, ethical pal
-liaive care are the result of an ethical PHC.
Final consideraions
This research aimed to discuss the ethical di -lemmas relaing to palliaive care in the PHC. For this, we developed a systemaic literature review to idenify, from the point of view of health profes -sionals, what are the ethical issues that arise from the pracice of the services. The review also served to detect the diiculies in the professional proile, in the pracice of the teams, management of ser -vices and health care systems in diferent parts of the world that ofer palliaive care in the PHC. Such diiculies are indicaive that the lack of organisa -ion of services and the lack of speciic qualiica-ions of professionals to deal with demands and needs of chronic health condiions is present also in coun -tries which have had an ageing populaion for longer than Brazil.
There is a shortage of knowledge from pro -fessionals about palliaive care, which contributes to the emergence of ethical problems in situaions more tradiionally associated with this kind of care such as the accompaniment of the death and grieving process, the communicaion of bad news, management of complex symptoms and clinical con -diions. In the SUS (abbreviaion of “Sistema Unico de Saude” in Brazil - Uniied Health System), one must take into account that the ESF (abbreviaion of “Estrategias Saude da Family” in Brazil- Family
Health Strategies) teams already face the demands of terminal paients and users with chronic health condiions. And in this aspect, perhaps the biggest ethical challenge for incorporaion of palliaive care in the PHC is: to change the view of the professionals about the palliaive care in order to introduce them earlier in the services, staring from the diagnosis of chronic health condiions.
Palliaive care is not only suitable for people with cancer or people who are close to death. It is an extremely beneicial care and its early intervenion, well before the inal stage of the disease, may be -come essenial to the excellence of the PHC before the demographic- epidemiological transiion and its impact on the populaion’s morbidity and mortality proiles. The palliaive care must be ofered accord -ing to the health needs of the populaion, so that the Primary Health Care and the RAS (Abbreviaion of ‘Redes de Atencao a Saude” in Brazil - Health Sys -tem Network) can realize their social funcion.
Communicaion diiculies also afect the in -ternal work of the team and of the team with the RAS. Poliical deiniions and guidelines for the ef -feciveness of the health care network in the SUS are not enough; It is necessary to invest in interper -sonal and inter professional communicaion as well as between the diferent levels of services, creaing a collaboraive culture based on the co-responsibili -ty for the health of the populaion.
The survey results highlighted the work over -load of the PHC teams, which is an obstacle to the implementaion of palliaive care. The ESF teams, in addiion to caring for the health of the popula -ion in their area of work, have to contribute for the UBS to be able to deal with the many spontaneous demands that are required from them. Moreover, chronic health condiions require constant moni -toring, including periods when the disease is latent, because this condiion implies the need for early palliaive care, that is, general palliaive care aimed at maintaining good quality of life in the present and during the disease progression. For the introducion of palliaive care under the SUS’s Primary Health Care, it is essenial to review the number of ascribed families in the ESF teams and reorganise the work process and the primary health care services.
This aricle is based on a master’s study produced under the post graduaion program of the School of Nursing of the University of São Paulo, São Paulo / SP.
R
esear
References
1. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis (DCNT) no Brasil – 2011-2022. Brasília: Ministério da Saúde; 2011. (Série B. Textos Básicos de Saúde).
2. Mendes EV. O cuidado das condições crônicas na atenção primária à saúde: o imperaivo da consolidação da Estratégia da Saúde da Família. Brasília: Opas; 2012. Capítulo 3, A atenção primária à saúde nas redes de atenção à saúde; p. 55-65.
3. Mitchell GK, Johnson CE, Thomas K, Murray SA. Palliaive care beyond that for cancer in Australia. Med J Aust (MJA). 2010;193(2):124-6.
4. Brasil. Ministério da Saúde. Portaria GM/MS nº 19, de 3 janeiro de 2002. [Internet]. 2002 [acesso 27 maio 2015]. Disponível: htp://www.saude.mg.gov.br/images/documentos/portaria_019.pdf 5. Combinato DS. Cuidados no inal da vida: análise do processo de trabalho na atenção primária
[tese]. Botucatu: Universidade Estadual Paulista, Faculdade de Medicina de Botucatu [FMB-Unesp]; 2011.
6. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2003;8(1):19-32.
7. Moher D, Liberai A, Tetzlaf J, Altman DG, The PRISMA Group (2009). Preferred reporing items for systemaic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(6):e1000097. DOI: 10.1371/journal.pmed.1000097
8. Guedert JM, Grosseman S. Ethical problems in paediatrics: what does the seing of care and educaion show us? BMC Med Ethics. 2012;13(2):1-9.
9. Hermsen MA, ten Have HA. Moral problems in palliaive care pracice: a qualitaive study. Med Health Care Philos. 2003;6(3):236-72.
10. Cameron BL, Santos Sala A. Understanding the provision of palliaive care in the context of primary health care: qualitaive research indings from a pilot study in a community seing in Chile. J Palliat Care. 2009;25(4):275-83.
11. Meijler WJ, Van Heest F, Otor R, Sleijfer DTH. Educaion needs of general praciioners in palliaive care: outcome of a focus group study. J Cancer Educ. 2005;20(1):28-33.
12. Exley C, Field D, Jones L, Stokes T. Palliaive Care in the community for cancer and end-stage cardiorespiratory disease: the views of paients, lay-carers and health care professional. Palliat Med. 2005;19(1):76-83.
13. Snyder S, Allen K, Hezelet S, Raswany S. Primary care physician knowledge, uilizaion, and aitude regarding advance care planning, hospice, and palliaive care: much work remains. J Pain Symptom Manage. 2011;41(1):307.
14. Brown H, Johnston B, Ostlund U. Idenifying care acions to conserve dignity in end-of-life care. Br J Community Nurs. 2011;16(5):238-45.
15. Carvalho SCC, Botelho MAR. Os cuidados paliaivos no âmbito dos cuidados de saúde primários: as intervenções dos enfermeiros. Pensar Enfermagem. 2011;15(1):2-24.
16. Ribas S, Aguado H, Tella M, Márquez I, Viñas P, Himénez J et al. Ideniicación de los conlictos éicos en la atención sociosanitaria. Un estudio exploratorio. Rev Calidad Asistencial. 2005;20(1):30-4.
17. Kahana B; Dan A, Kahana E, Kercher K. The personal and social context of planning for end-of-life care. J Am Geriatr Soc. 2004;52(7):1.163-7.
18. Tan HM, O’Connor MM, Miles G, Klein B, Schatner P. GP and nurses’ percepions of how ater hours care for people receiving palliaive care at home could be improved: A mixed methods study. BMC Palliat Care. 2009;8(13):1-10.
19. Borgsteede SD, Deliens L, van der Wal G, Francke AL, Stalman WAB, van Eijk JTM. Interdisciplinary cooperaion of GPs in palliaive care at home: a naionwide survey in the Netherlands. Scand J Prim Health Care. 2007;25(4):226-31.
20. Rhee JJO, Zwar N, Vagholkar S, Dennis S, Broadbent AM, Mitchell G. Aitudes and barriers to involvement in palliaive care by Australian urban general praciioners. J Palliat Med. 2008;11(7):980-5.
21. Walshe C, Todd C, Caress AL, Chew-Graham C. Judgements about fellow professional and the management of paients receiving palliaive care in primary care: a qualitaive study. Br J Gen Pract. 2008;58(549):264-72.
22. Walshe C, Todd C, Caress AL, Chew-Graham C. Implementaion and impact of the Gold Standards Framework in community palliaive care: a qualitaive study of three primary care trusts. Palliat Med. 2008;22(6):736-43.
23. Valente SH, Teixeira MB. Estudo fenomenológico sobre a visita domiciliária do enfermeiro à família no processo de terminalidade. Rev Esc Enferm USP. 2009;43(3):655-61.
24. Block SD, Bernier GM, Crawley LM, Farber S, Kuhl D, Nelson W et al. Incorporaing palliaive care into primary care educaion. J Gen Intern Med. 1998;13(11):768-73.
R
esear
25. Peduzzi M, Carvalho BG, Mandú EN, Souza GC, Silva JAM. Trabalho em equipe na perspeciva da gerência de serviços de saúde: instrumentos para a construção da práica interproissional. Rev Saúde Coleiva. 2011;21(2):629-46.
26. Junges JR, Zoboli ELCP, Patussi MP, Schaefer R, Della Nora CR. Construção e validação do instrumento “Inventário de problemas éicos na atenção primária em saúde”. Rev. bioét. (Impr.). 2014;22(2):309-17.
27. Zoboli ELCP. Deliberação: leque de possibilidades para compreender os conlitos de valores na práica clínica da atenção básica [tese de livre-docência]. São Paulo: Escola de Enfermagem, Universidade de São Paulo [EEUSP]; 2010.
28. Neegard MA, Olesen F, Jensen AB, Sondergaard J. Palliaive care for cancer paients in primary health care seing: bereaved relaives’ experience, a qualitaive group interview study. BMC Palliat Care. 2008;7(1):1-8.
29. Pessini L, Bertachini L. Novas perspecivas em cuidados paliaivos: éica, geriatria, gerontologia, comunicação e espiritualidade In: Pessini L, Barchifontaine CP, organizadores. Bioéica e longevidade humana. São Paulo: Centro Universitário São Camilo/Loyola; 2006. p. 353-91.
Paricipaion of the authors
Danielle Yuri Saito Takaui developed the master’s study in which this aricle is based, paricipated as the irst reviewer in the scoping review and drated the original aricle. Elma Lourdes Campos Pavone Zoboli directed the master’s study from which this aricle has been originated. She also paricipated as secondary reviewer of the scoping review and revised the original aricle.
Recebido: 19.12.2014 Revisado: 6. 4.2015 Aprovado: 13. 5.2015
R
esear
Annex
Table 1. List of Studies included in the revisionAricle Title Authors Country of
origin
E1 8 Ethical problems in paediatrics: What does the
seing of care and educaion show us? Guedert JM, Grosseman S Brasil
E2 17 The personal and social context of planning for
end-of-life care Kahana B, Dan A, Kahana E, Kercher K EUA
E3 13 Primary care physician knowledge, uilizaion, and aitude regarding advance care planning, hospice, and palliaive care: Much work remains
Snyder S, Allen K, Hezelet S, Raswany S EUA
P4 10 Understanding the provision of palliaive care in the context of primary health care: Qualitaive research indings from a pilot study in a community seing in Chile
Cameron BL, Santos Sala A Canadá
C5 11 Educaion needs of general praciioners in
palliaive care: Outcome of a focus group study Meijler WJ, Van Heest F, Otor R, Sleijfer DTH EUA P6 14 Idenifying care acions to conserve dignity in
end-of-life care Brown H, Johnston B, Ostlund U Reino Unido
A7 15 Os cuidados paliaivos no âmbito dos cuidados de saúde primários: as intervenções dos enfermeiros
Carvalho SCC, Botelho MAR Portugal
A8 16 Ideniicación de los conlictos éicos en la
atención sociosanitaria. Un estudio exploratorio Ribas S, Aguado H, Tella M, Márquez I, Viñas P, Himénez J, Asens G Espanha A9 20 Aitudes and barriers to involvement in
palliaive care by Australian urban general praciioners
Rhee JJO, Zwar N, Vagholkar S, Dennis S,
Broadbent AM, Mitchell G Austrália
A10 18 GP and nurses’ percepions of how ater hours care for people receiving palliaive care at home could be improved: A mixed methods study
Tan HM, O’Connor MM, Miles G, Klein
B, Schatner P Austrália
A11 21 Judgements about fellow professional and the management of paients receiving palliaive care in primary care: A qualitaive study
Walshe C, Todd C, Caress AL,
Chew-Graham C Inglaterra
A12 22 Implementaion and impact of the Gold Standards Framework in community palliaive care: A qualitaive study of three primary care trusts
Walshe C, Todd C, Caress AL,
Chew-Graham C Inglaterra
A13 23 Estudo fenomenológico sobre a visita
domiciliária do enfermeiro à família no processo de terminalidade
Valente SH, Teixeira MB Brasil
A14 19 Interdisciplinary cooperaion of GPs in palliaive care at home: A naionwide survey in the Netherlands
Borgsteede SD, Deliens L, van der Wal G,
Francke AL, Stalman WAB, van Eijk JTM Holanda
A15 12 Palliaive care in the community for cancer and end-stage cardiorespiratory disease: The views of paients, lay-carers and health care professional
Exley C, Field D, Jones L, Stokes T Reino Unido
P16 9 Moral problems in palliaive care pracice: A
qualitaive study Hermsen MA, ten Have HA Holanda
R
esear
Table 2. Ethical problems concerning palliaive care in the primary health care
Aricle Ethical issues
E1 8 • None of the 16 doctors from the UBS (UBS stands for Unidade Basica de Saude - Health system Basic Unit) had a problem with end-of-life care
E2 17 • 75% of PHC doctors were unaware of their paients inal wishes of life, even if these paients had already stated them in anicipated direcives (AD) in another service
• 11% of doctors did the anicipated direcives without the paient's consent
E3 13 • Most doctors believe that to discuss palliaive care is ime consuming, so it is unlikely that they will have that discussion with paients
• To discuss palliaive care with the paient is stressful and uncomfortable for most doctors • Most doctors do not believe that this discussion is beneicial to the paient
P4 10 •Primary health care staf professionals feel obliged to accompany paients in their last days of life; therefore, they give their personal phone numbers so they can be contacted by the family of the paient. They even visit the paient's home ater working hours
• The professionals involved in palliaive care show enthusiasm to stay in the program, but the scarcity of resources causes overload
• The biggest concern of the professionals was related to the inadequacy of their experise in palliaive care. They see this as a limitaion when faced with complex clinical situaions because, although they work based on clinical work learned through pracice, many imes they have doubts about the best course of acion
C5 11 Doctors feel powerless in the palliaive care as to what they can do for terminally ill paients, compared to what they can do for those paients whose life expectancy is normal. To compensate for this impotence, they feel compelled to pay more atenion to paients in palliaive care, staying next to them for a longer ime.
• Doctors report emoional distress of paients, families and professionals
• Doctors menion that fatalisic thoughts, insecurity and helplessness of informal caregivers tend to compromise the autonomy of paients, creaing dependency and sufering
• One doctor reports a crisis of conidence between the paient and the doctor of the PHC who was not involved in curaive care because the specialist was in charge of it.
• According to doctors of the PHC, the poor quality of communicaion in the moving of a paient from the second to the irst level of atenion disturbs the applicaion of the palliaive care at home. • Doctors feel lack of support for dealing with ethical issues in palliaive care and suggest the need for a course on the subject, including noions of norms and values, as well as ways to discuss and share these problems within the work team
• Doctors report a lack of knowledge and training of professionals in the management of symptoms (pain, nausea, dysphagia, delirium, depression etc.) of paients in palliaive care
• Doctors refuse to accept that ethical issues such as euthanasia can be solved only with the good performance of palliaive care
P6 14 • Nurses recognise the importance of talking about death with paients; however, they only do so when they are willing to or when the opportunity arises
• Nurses report that they do not feel prepared to talk to users about spirituality or religiosity, even knowing that this subject is essenial in the inal stage of life
• Nurses recognise the importance of family support, but they say that someimes that support hinders care
A7 15 • Nurses don’t have availability for intervenions in palliaive care
• Three nurses menion the lack of veracity whilst talking to the paient and the family about the paient’s actual health situaion
• Nurses recognise that they lack knowledge in the management of symptoms of paients in palliaive care
• The communicaion with paients, according to nurses, is not appropriate because of the deicient training of the professionals
• Nurses report lack of condiions, ime and training to accompany the mourning • None of the nurses reported intervenions in mulidisciplinary teams
R
esear
Aricle Ethical issues
A8 16 • Professionals menion the lack of informaion and breach of conideniality about the treatment and the prognosis
• Professionals report suspicion that paients sufer physical, psychological, economic or other types of abuse by family members
• Professionals report poor relaionship with the team and of the team with the diferent levels of the health care network
• Professionals report poor relaionship with family members of paients and / or informal caregivers • Professionals menion the lack of social and inancial resources of the services
A9 20 • Between 20% and 30% of 269 PHC doctors who provide palliaive care report that the specialists do not share informaion with them
• 25.2% of 269 doctors from the PHC menion, as obstacles for their involvement with palliaive care: lack of ime; home visits; personal and family commitments; lack of interest; unavailability for work ater hours; lack of knowledge; emoional reasons and a lack of support of specialists
• 25.2% of 269 doctors of the PHC do not feel safe to deal with issues related to palliaive care, such as terminal restlessness, psychosocial aspects, agitaion and neuropathic pain
A10 18 • 82% of 114 doctors and 85% of 52 nurses report that the communicaion between professionals is lawed
• 59% of 114 doctors and 62% of 52 nurses menion that paients are reluctant to call in the professionals who are available ater work hours
• 58% of 114 doctors and 87% of 52 nurses claim that the amendment of legislaion to allow the nurse to review the death could increase the ofer of ater hours palliaive care services.
• The professionals report a lack of coninuity in the care for people receiving palliaive care at home, ater the closing ime of Primary Health care services
• 54% of 114 doctors and 67% of 52 nurses menion the high cost of overime on the provision of palliaive care
• 41% of 114 doctors and 63% of 52 nurses claim that the insecurity in services leads them to give up night shits
• 40% of 114 doctors and 44% of 52 nurses reported that the limited coverage of mobile telephony has a negaive impact on the provision of palliaive care
• 76% of 114 doctors and 90% of 52 nurses consider that the limited availability of doctors to work ater hours is a limiing factor of palliaive care in the PHC
• 79% of 114 doctors and 83% of 52 nurses esimate that the limited availability of nurses to work ater hours is a limiing factor of palliaive care in the Primary Health Care
• 49% of 114 doctors and 54% of 52 nurses report the lack of interpreters, ater opening hours, to atend the needs of aboriginal populaions
• 69% of 114 doctors and 71% of 52 nurses menion that the access to emergency medicaions is limited ater hours
• Doctors reported lack of training to provide palliaive care as they don’t have ime to devote to a coninuous training in this specialty
• Doctors are unaware of which services and resources, available in the community and in the primary health care (PHC), are able to ensure coninuity of care ater hours or are adequate to plan the support to atend the needs of paients in palliaive care
A11 21/A12 22 • 14 nurses from PHC consider that doctors are resistant to new iniiaives and are reluctant to meet the needs of paients and the requests of the nursing staf
• The concepts of "good" or "bad" doctor, in the view of nurses, do not necessarily relate to technical experise or knowledge, but to the availability of the professional to receive and respond to requests, be them from the nurse or the paient
• Nurses recognise that interpersonal relaionships and percepions of each other about their respecive performances inluence the work of the staf and the referrals of users to other services. The team cohesion stems more from interpersonal relaionships than from the paient care
• Doctors enjoy friendly working relaionships with nurses; however, trading issues and interpersonal relaionships do not weigh much on the assessment made of these professionals, probably by the diference in authority between the two categories
• Professionals describe the posiive impact of the introducion of a program to improve the quality of care in the PHC based only on the professional relaionship, ignoring interacions with paients and the inluence on their care
R
esear
Aricle Ethical issues
A13 23 • Nurses claim that the work overload and the lack of space in everyday life to discuss the feelings experienced in the care of dying paients, causes the professionals to be more suscepible to emoional distress
• Nurses feel frustrated because they can not provide quality care because of the lack of resources in the PHC and reference services as well
• Nurses can not establish limits for their relaionship with terminally ill paients and their families • Nurses create intense links with terminal paients in their care, which leads to sufering at work • Nurses, given their close proximity to users, go beyond technical limitaions in their work in the ESF (abbreviaion of “Estrategias Saude da Family” in Brazil- Family Health Strategies) staf.
• When faced with abuse, lack of care and neglect of the paient by the family, nurses change their behaviour: they start to ofer merely technical care to the paient, and do not consider the possibility of family members also being part of the care
• Nurses report that families and informal caregivers request care or acions that are beyond the means of Primary Health Care, such as constant visits to the paient
A14 19 • Doctors consider the somaic domain as the most important in palliaive care, followed by psychosocial and spiritual care
• 63% of doctors report that informal caregivers are the main collaborators in palliaive care
• Few doctors cooperate with religious ministers, which may indicate that they alone deal with such problems, or that few paients have spiritual problems, or that few doctors recognise the spiritual problems
• In 71% of cases, doctors describe that cooperaion with colleagues was present. This number could be considered low and provoke quesions about the quality of communicaion and coninuity of care, considering that an eicient exchange of informaion about paients is expected so 24 hours healthcare services can provide proper care ater the end of working hours in the primary health care
A15 12 • In cases of paients with cardiorespiratory disease, PHC doctors report frustraion because they can not take full care, as specialists from hospitals are the ones who manage these paients palliaive care when the underlying disease gets worse.
• According to doctors from the PHC, hospitals’ specialists fail to give them informaion, not making them aware of decisions taken in the hospital about the treatment regimen of paients under their care • PHC doctors lose conidence in the hospital because communicaion about treatments and intervenions is lawed, and conlict with the requirements of PHC, especially in cases of cancer paients enrolled in clinical trials prohibiing the PHC and the hospital to change or introduce treatment without the consent of the research team
• Doctors and nurses from the PHC say it is easier to get specialised services for palliaive care paients with cancer than for those in the inal stage of cardiorespiratory diseases
• PHC doctors recognise that they provide less help when it comes to paients with end-stage cardiorespiratory diseases, than in the case of cancer paients at the same stage as they were not suiciently trained to deal with the irst situaion
• For doctors of PHC, it is more diicult to reach the conclusion that the person is dying when the person does not have a malignancy. This makes professionals less willing to communicate to these people that they are in a state of terminal illness
R
esear
Aricle Ethical issues
P16 9 • PHC professionals face moral problems when, in respect for the principle of the paient autonomy, must decide on the resuscitaion or not, or the performance or nonperformance of fuile medical acions for the paient who has no chance of cure
• PHC Professionals face moral problems when the treatment chosen by the paient is considered fuile by doctors but improves their quality of life
• PHC professionals struggle to create a bond and moivate themselves to look and talk about death when the paient is considered "diicult," such as the one who is never saisied with the work of nursing. This compromises the quality of care
• PHC doctors ofer the opion of euthanasia to the paient when there is no possible treatment to relieve their symptoms, although this procedure is not carried out under the PHC and even terminal paients in home care raise quesions regarding the search for the meaning of life, oten appealing to the PHC professionals. These, unprepared, try to answer the paient and family members, who are also their paients
• PHC Doctors prefer that the specialist inform the paient about the poor prognosis because they believe that if they do, it can generate conlict in their relaionship with the paient and the family, and they fear it may interfere with keeping a care of quality
• The PHC professionals face moral problems in the management of symptoms such as terminal sedaion, principle of the double efect and use of opioids