ORIGINAL ARTICLE
Use of psychotropic medications during pregnancy:
perception of teratogenic risk among physicians in two
Latin American countries
Amaury Cantilino,
1Laura Lorenzo,
2Juliane dos A. de Paula,
1,3Adrienne Einarson
41Department of Neuropsychiatry, Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil.2Psinapsys Psychiatric Private Center, La Plata, Argentina.3Graduate Program in Health Sciences, Faculdade de Medicina do ABC, Santo Andre´, SP, Brazil.4The Motherisk Program, The Hospital for Sick Children, Toronto, Canada.
Objective: Pregnant women and their health care professionals commonly believe that use of medications during pregnancy may be harmful to the unborn fetus. The objective of this study was to evaluate the risk perception of psychotropic drug use in pregnancy among physicians in different medical specialties.
Method:This was a convenience survey conducted at outpatient clinics in the cities of Recife, Brazil, and La Plata, Bahı´a Blanca, and Buenos Aires, Argentina. Physicians who agreed to participate were asked to rate their perception of teratogenic risk among different classes of drugs, which included antidepressants, antipsychotics, anticonvulsants, and benzodiazepines.
Results:Two hundred and thirty-eight physicians completed the survey (response rate, 98%). These included psychiatrists, obstetricians, neurologists, cardiologists, gastroenterologists, and general practitioners. Among different specialties, a minority of psychiatrists perceived psychotropic drugs to be highly teratogenic (antidepressants, 12.5%; antipsychotics, 15%; benzodiazepines, 25%) as compared with other specialties (p,0.003 for each drug class). There was no difference in perceived risk of antiepileptic drugs among specialties, including psychiatrists.
Conclusion:The risk associated with use of psychotropic drugs in pregnancy was overestimated by physicians of all medical specialties, except psychiatry. All physicians should be aware of the safety/ risk of psychotropic agents in pregnancy, as they may be required to give advice and/or prescribe these drugs to pregnant women.
Keywords: Perception; psychotropic drugs; pregnancy; teratogens
Introduction
It is commonly believed that exposure to medications during pregnancy can be harmful to the unborn child. Women requiring drug treatment for chronic diseases are often concerned and, consequently, seek information from family, friends, and health care providers to assist them in this decision-making process. It is crucial that women receive balanced, evidence-based information concerning drug exposures during pregnancy.1,2
Unfortunately, health care professionals do not always disseminate evidence-based information. Results from an international survey recorded that a relatively small proportion of community pharmacists provided evi-dence-based information regarding the drugs in question. Only 14% referred to current medical literature, while 60% consulted the product monograph (which does not include evidence-based pregnancy data). More than 90% of pharmacists referred the client to their physician.3
Family physicians are usually the first health care professional that women see to confirm a diagnosis of pregnancy. A study conducted in Canada and Australia evaluated family physicians’ attitudes and practices surrounding the use of antidepressants in pregnancy. The study found that physicians from both countries felt strongly that advice regarding antidepressant use during pregnancy was a difficult task, and most did not feel comfortable giving information.4
Health care professionals are generally more suppor-tive than family and friends about taking medications during pregnancy. However, negative information given by a health care provider is generally more upsetting, because these individuals are trusted to provide evi-dence-based information. After receiving negative infor-mation from a health care provider, especially a physician, it is difficult for women to accept that reassuring evidence-based information is accurate. Consequently, despite such evidence-based reassur-ance, women who continue using the medication remain worried and feel guilty because they cannot forget the initial negative information they received.5
This can be particularly critical in relation to psychiatric
Correspondence: Adrienne Einarson, The Motherisk Program, The Hospital for Sick Children, 555 University Avenue, Toronto, ON M5G 1X8, Canada.
E-mail: einarson_hsc@yahoo.ca
perception of the risk of antidepressant drugs by preg-nant women with depression and the efficacy of evidence-based counseling. Women who called The Motherisk Program requesting information about the safety of an antidepressant during pregnancy were compared with two other groups: 1) women who called about antibiotic use (i.e., non-teratogenic drugs used short-term); and 2) women who called about gastric medications (i.e., non-teratogenic drugs used long-term). Their perception of risk was measured before and after evidenced-based information was given. Despite receiv-ing evidence-based reassurreceiv-ing information, 15% of antidepressant users, compared to 4% using gastric drugs and 1% using antibiotics, chose to discontinue their medication.1
There are few studies in the peer-reviewed literature documenting physicians’ attitudes and practices regard-ing the use of psychotropic drugs in pregnancy, and none from Latin America. The objective of this study was to evaluate risk perception of psychotropic use during pregnancy among different medical specialties.
This study followed the standards required by the Helsinki Declaration and was approved by the Research Ethics Committee of Universidade Federal de Pernambuco (protocol no. 305).
Methods
This was a convenience survey that was conducted at outpatient clinics in cities in Brazil (Recife) and Argentina (Buenos Aires, La Plata, and Bahı´a Blanca). Each physician was personally approached and asked to complete a questionnaire after signing a consent form.
Information such as age, sex, and date of graduation was collected. Participants were asked to rate their perception of teratogenic risk regarding different drug classes between two options: each particular drug may cause malformations between 1-5%, or higher than 5%. The following drug classes were evaluated: antidepres-sants, antipsychotics, anticonvulantidepres-sants, and benzodiaze-pines. A specific item (whether the respondent considers that psychotropic medications may be more harmful to the fetus than other medications) was included as the last question. To verify physicians’ degree of interest in this topic, they were also asked whether they had read anything, either in the lay press or the scientific literature, or if they had attended a lecture or taken a course on this topic.
The responses of different medical specialists were compared. Statistical analyses consisted of the chi-square
or Fisher’s exact test for categorical data and the Kruskal-Wallis test for continuous data. Differences were consid-ered significant when p,0.05.
Results
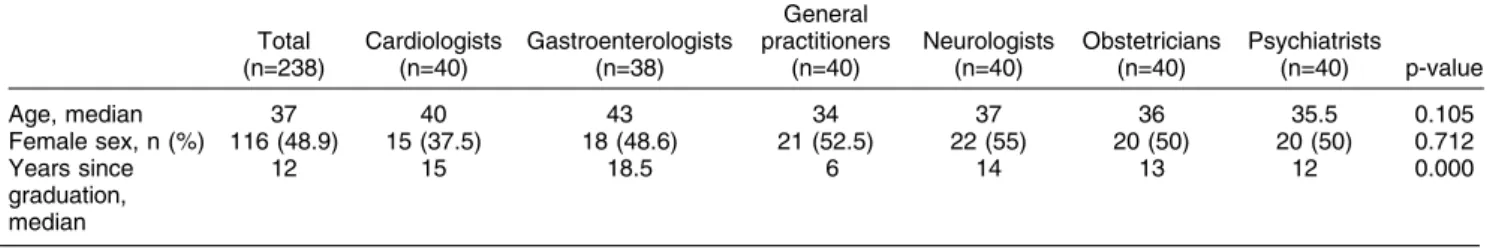
A total of 238 surveys from medical professionals, 120 from Brazil and 118 from Argentina, were analyzed. The sample consisted of medical specialists in psychiatry, obstetrics, neurology, cardiology, gastroenterology, and family medicine. Each medical specialty was represented by 40 participants (except for gastroenterologists, n=38), 20 from each country. The mean age of the sample was 37 years, and the gender distribution was similar (116 women and 121 men, 48.9 and 51.1% respectively); mean time since graduation was 12 years. The median age and gender distribution did not show differences among specialties. Family physicians were the more recent graduates (Table 1).
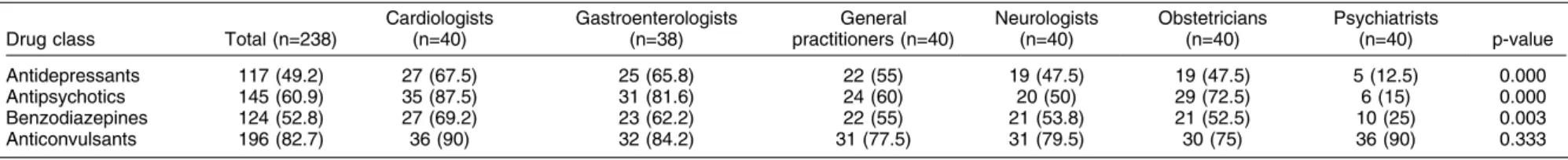
Perception of higher teratogenic risk (malformations in more than 5% of cases when used during pregnancy) was reported by most of the sample (82.7%) regarding anticonvulsants, followed by antipsychotics (60.9%), benzodiazepines (52.8%), and antidepressants (49.2%). For anticonvulsants, a perception of higher teratogenic risk (malformations in more than 5% of cases when used during pregnancy) was reported by 82.7% of the sample, vs. 60.9% for antipsychotics, 52.8% for benzodiazepines, and 49.2% for antidepressants.
Among different specialties, there were differences in risk perception regarding antidepressants, antipsycho-tics, and benzodiazepines, but not anticonvulsants. Psychiatrists perceived the least risk regarding these drug classes, compared with other specialists (Table 2).
For the specific question at the end of the questionnaire, 42.6% (101 of 237) of the sample considered that psychiatric medications during pregnancy were potentially more harmful than other drug classes (Table 3).
Among specialties, only 7 of 40 (17.5%; p = 0.004) psychiatrists considered psychotropics to be more harm-ful. Excluding this group, there were no statistical differences in risk perception among the other specialists (p = 0.334), but cardiologists and family physicians tended to perceive a higher risk regarding psychotropics compared with other medications. Following psychia-trists, neurologists were the specialists that most often prescribed psychotropics (95%), whereas obstetricians prescribed them least (35%).
Regarding questions about interest in the subject, more respondents answered having read some scientific
Table 1 Demographics of participants
Total (n=238)
Cardiologists (n=40)
Gastroenterologists (n=38)
General practitioners
(n=40)
Neurologists (n=40)
Obstetricians (n=40)
Psychiatrists
(n=40) p-value
Age, median 37 40 43 34 37 36 35.5 0.105
Female sex, n (%) 116 (48.9) 15 (37.5) 18 (48.6) 21 (52.5) 22 (55) 20 (50) 20 (50) 0.712 Years since
graduation, median
12 15 18.5 6 14 13 12 0.000
Psychotropic risk perception among physicians 107
Table 2 Perception of risk regarding whether psychotropic drugs are likely to cause malformations at a frequency higher than 5%
Drug class Total (n=238)
Cardiologists (n=40)
Gastroenterologists (n=38)
General practitioners (n=40)
Neurologists (n=40)
Obstetricians (n=40)
Psychiatrists
(n=40) p-value
Antidepressants 117 (49.2) 27 (67.5) 25 (65.8) 22 (55) 19 (47.5) 19 (47.5) 5 (12.5) 0.000 Antipsychotics 145 (60.9) 35 (87.5) 31 (81.6) 24 (60) 20 (50) 29 (72.5) 6 (15) 0.000 Benzodiazepines 124 (52.8) 27 (69.2) 23 (62.2) 22 (55) 21 (53.8) 21 (52.5) 10 (25) 0.003 Anticonvulsants 196 (82.7) 36 (90) 32 (84.2) 31 (77.5) 31 (79.5) 30 (75) 36 (90) 0.333
Table 3 Comparison among all specialties regarding additional questions
Total (n=238)
Cardiologists (n=40)
Gastroenterologists (n=38)
General practitioners
(n=40)
Neurologists (n=40)
Obstetricians (n=40)
Psychiatrists
(n=40) p-value
Consider psychiatric medications in pregnancy more harmful than other drug classes.
101 (42.6) 22 (55) 16 (42.1) 23 (57.5) 15 (37.5) 18 (46.2) 7 (17.5) 0.004*
Usually indicate psychiatric medication. 167 (70.2) 27 (67.5) 26 (68.4) 22 (55) 38 (95) 14 (35) Na 0.000
Read article or scientific material on the use of medications during pregnancy.
167 (70.5) 26 (65) 22 (57.9) 18 (45) 28 (71.8) 37 (92.5) 36 (90) 0.000
Attended class or course on the use of medications during pregnancy.
95 (40.1) 8 (20) 7 (18.4) 14 (35) 13 (32.5) 32 (82.1) 21 (52.5) 0.000
A
C
antilino
et
al.
B
ras
P
siquiatr.
2014
material about use of medication during pregnancy during past years (70.5%). Among specialties, the majority of obstetricians and psychiatrists reported having read scientific material (92.5 and 90%, respectively), while only 45% of general practitioners reported this activity.
Only 40.1% of the sample, represented mainly by obstetricians (82.1%), reported having attended lectures or courses about this topic.
Discussion
To our knowledge, this is the first survey of its kind to be conducted in Latin America (specifically, Brazil and Argentina), and the results appear to be similar to those of surveys conducted in North America and Europe. This suggests that fear surrounding the use of psychotropic drugs in pregnancy is a worldwide phenomenon. This is a concern, because mental illness is prevalent world-wide and, to date, few guidelines are available for treatment of pregnant women diagnosed with a psy-chiatric disorder. We could find only two guidelines specifically designed for pregnant women with depres-sion and other psychiatric disorders, published by the UK National Institute for Clinical Excellence (NICE)6and by the American Psychiatric Association.7 However, these guidelines are very conservative regarding the use of psychotropic drugs in pregnancy, and are intended primarily for women who are planning to become pregnant. As almost half of all pregnancies are unintended,8 many women approach their health care providers when they are already pregnant and taking a medication, requesting information regarding drug safety.
In our survey, 42.6% of the sample thought that psychotropics during pregnancy were more harmful than other drug classes. Anticonvulsants as a group were perceived to cause malformations in more than 5% of cases by the majority of the sample, which was consistent with each specialty and with the evidence-based litera-ture.9 Antipsychotics were considered potentially more harmful by more than 60% of the sample, mostly by non-psychiatrists, perhaps because there is less information about risk and safety, although antipsychotics have not been definitively associated with a higher risk of birth defects.10
Benzodiazepines were considered more harmful by 52.8% of the sample, although available information regarding potential teratogenic risk considers them relatively safe for use in pregnancy. In a recent updated meta-analysis,11 the overall risk of malformations asso-ciated with benzodiazepines from cohort studies was 1.07 (95% confidence interval 0.91-1.25). However, a former finding of increased risk of oral clefts detected in case-control studies12could not be reassessed, as there were no new studies addressing this specific malformation.
Antidepressants were considered to have less terato-genic potential, as less than half of the participants believed them to cause malformations in more than 5% of cases. This is consistent with available evidence-based information regarding the safety of these drugs,
as antidepressants do not appear to pose a major teratogenic risk.13 Currently, other medical specialties (especially family physicians) are more often called upon to prescribe antidepressants in pregnancy. This is likely for a number of reasons, including a higher prevalence of depression in the population, shortage of psychiatrists in many geographic regions, and more reassuring informa-tion regarding the safety of antidepressants in pregnancy compared with other psychotropic drugs.
Most of the sample, including psychiatrists (98.3%), perceived that chemotherapeutics are more harmful when administered to pregnant women, followed by anticonvulsants (82.7%). Other medications, such as antibiotics, antihypertensives, corticosteroids, and gas-tric medications, were considered harmful by 38.6, 29.8, 20.4, and 9.9% of the sample, respectively. In addition, the other specialists were specifically asked if they were comfortable with prescribing medications other than psychotropics during pregnancy, and 110 (46.2%) physicians answered that they were. We therefore interpreted this response to mean that the overestimated risk related with the prescribing of psychotropics by other specialties was not due to a general cautiousness towards prescribing medications during pregnancy.
Most psychiatrists considered that, excluding antiepi-leptics, psychotropic agents (antipsychotics, benzodiaze-pines, and antidepressants) did not pose a.5% risk of producing birth defects. Other specialists tended to overestimate the teratogenic risk associated with these drug classes. This may be explained by the fact that psychiatrists are more likely to treat a pregnant woman requiring psychotropic drugs and consult the scientific literature more frequently.
The limitations of this study include a small sample size and the possible selection bias inherent to a convenience sample. In addition, this was not a randomized sample of physicians in each country; therefore, findings cannot necessarily be generalized. Some of the respondents were casually known to the authors in their respective medical communities, and this was likely responsible for the high response rate. However, it is unlikely to have had an effect on their responses to the questionnaire.
In summary, in this sample of physicians from Brazil and Argentina, the perception of risk associated with the use of psychotropic drugs in pregnancy was overesti-mated by non-psychiatric specialists, while psychiatrists reported a perception of risk consistent with evidence-based information.
Therefore, increased training (lectures, courses, etc.) on the use of psychotropic drugs in pregnancy is recommended among non-psychiatric specialists, as they also care for pregnant women taking these medications.
Disclosure
AE serves as a consultant for The Motherisk Program and for Eli Lilly Inc, Toronto, Canada. AC has worked as a
Psychotropic risk perception among physicians 109
speaker for Sanofi and Abbott Laboratories (Brazil). The other authors report no conflicts of interest.
References
1 Bonari L, Koren G, Einarson TR, Jasper JD, Taddio A, Einarson A. Use of antidepressants by pregnant women: evaluation of perception of risk, efficacy of evidence based counseling and determinants of decision making. Arch Womens Mental Health. 2005;8:214-20. 2 Einarson A, Mazzieri MR, Sola NH, Uema S, Einarson TR. Evidence
based information on drug use during pregnancy: assessment of community pharmacist in Cordoba, Argentina. Pharm Care Esp. 2002;4;209-21.
3 Lyszkiewicz DA, Gerichhausen S, Bjo¨rnsdo´ttir I, Einarson TR, Koren G, Einarson A. Evidence based information on drug use during pregnancy: a survey of community pharmacists in three countries. Pharm World Sci. 2001;23:76-81.
4 Bilszta JL, Tsuchiya S, Han K, Buist AE, Einarson A. Primary care physician’s attitudes and practices regarding antidepressant use during pregnancy: a survey of two countries. Arch Womens Ment Health. 2011;14:71-5.
5 Mulder E, Davis A, Gawley L, Bowen A, Einarson A. Negative impact of non-evidence-based information received by women taking
antidepressants during pregnancy from health care providers and others. J Obstet Gynaecol Can. 2012;34:66-71.
6 National Collaborating Centre for Mental Health. Antenatal and postnatal mental health: the NICE guideline on clinical management and service guidance. Leicester: British Psychological Society; 2007. 7 American Psychiatric Association. Practice guideline for the treat-ment of patients with major depressive disorder [Internet]. 3th edition. [cited 2013 Apr 27]. http://psychiatryonline.org/content. aspx?bookid=28§ionid=1667485#654024.
8 Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities. Contraception. 2011;84:478-85. 9 Galbally M, Roberts M, Buist A, Perinatal Psychotropic Review
Group. Mood stabilizers in pregnancy: a systematic review. Aust N Z J Psychiatry. 2010;44:967-77.
10 Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15:183-92.
11 Enato E, Moretti M, Koren G. The fetal safety of benzodiazepines: an updated meta-analysis. J Obstet Gynaecol Can. 2011;33:46-8. 12 Dolovich LR, Addis A, Vaillancourt JM, Power JD, Koren G, Einarson
TR. Benzodiazepine use in pregnancy and major malformations of oral cleft: meta-analysis of cohort and case-control studies. BMJ. 1998;317:839-43.