Revista
Española
de
Cirugía
Ortopédica
y
Traumatología
www.elsevier.es/rot
ORIGINAL
ARTICLE
Fresh
bipolar
osteochondral
allograft
of
the
ankle.
Review
of
the
literature
and
case
report
of
a
young
patient
with
bilateral
post-traumatic
osteoarthritis
夽
R.
Pimenta
a,b,∗,
P.
Carvalho
a,
P.
Amado
a,baUnidaddeTobillo-Pie,InstitutoCUF,Porto,Portugal
bFacultaddeCienciasdelaSalud,UniversidadFernandoPessoa,Porto,Portugal
Received16October2011;accepted8November2011
KEYWORDS
Post-traumatic arthritis; Ankle; Cartilage; Osteochondral allograft
Abstract
Objectives:Thetreatmentofseverepost-traumaticanklearthritisremainsachallenge nowa-days.Sincepatientssufferingfromthispathologyaremainlyyoungandactivepeople,acorrect reconstruction, if possible, ofthe articular cartilage defects ofthe tibiotalar joint is very importanttoachieveagoodresult.Freshbipolarosteochondralallograft(FBOA)isa promis-ingoperativetechnique,asanalternativetoarthrodesisandtotalanklereplacement,inpain relief,restorationoffunctionandindefinitedelayofarthriticdiseaseprogression.
Methods:Theauthorsmadeareviewoftheliteratureandpresentacasereportofayoung 30-year-oldman,withbilateralpost-traumaticosteoarthritisoftheankle,treatedwith(FBOA). Thepatientwasevaluatedclinicallyandradiographicallymonthly.
Results:Painreliefandpostoperativefunctionwassignificantlyimprovedreaching94points intheleftankle(preoperativeof40points),and92 pointsintherightankle(preoperative 42points)AOFASscore.
Conclusions:Freshtibiotalarallograftingseemstobeagoodalternativetoarthrodesisand pros-theticreplacement,inthetreatmentofanklearthropathyandbigarticularcartilagedefects mainlyinyoungandactivepatients.Thisprocedureachievesagoodpainrelief,maintaining functionaljointmotionanddecreasingtheriskofadjacentjointarthritis.
©2011SECOT.PublishedbyElsevierEspaña,S.L.Allrightsreserved.
夽 Pleasecitethisarticleas:PimentaR,etal.Aloinjertoosteocondralbipolarfrescodeltobillo.Revisióndelaliteraturaypresentación
delcasodeunpacientejovenconartrosisbilateralpostraumática.RevEspCirOrtopTraumatol.2012;56(2):120---6. ∗Correspondingauthor.
E-mailaddresses:ruipimentaribeiro@gmail.com,pamado@ufp.edu.pt(R.Pimenta).
PALABRASCLAVE Artrosis postraumática; Tobillo; Cartílago; Aloinjertos osteocondrales
Aloinjertoosteocondralbipolarfrescodeltobillo.Revisióndelaliteraturay presentacióndelcasodeunpacientejovenconartrosisbilateralpostraumática
Resumen
Objetivo: Eltratamientodelaartrosispostraumáticagravedeltobillosiguesiendounretoen nuestrosdías. Dadoquelospacientesafectosdeestaafección sonfrecuentementejóvenes y activos, la reconstrucción apropiada de los defectos articulares de la articulación tibio-astragalina,siesposible,esmuyimportanteparaobtenerunbuenresultado.Losaloinjertos osteocondralesbipolaresfrescos(ABOF)constituyenunatécnicaquirúrgicaprometedora,como unaalternativaalaartrodesisoalaartroplastiadetobilloencuantoalaliviodedolor, recu-peraciónfuncionalyretrasodelaprogresiónalaartrosis.
Método: Serealizaunarevisióndelaliteraturaysepresentaelcasodeunpacientevarónde 30 a˜nos con artrosis bilateral postraumática del tobillotratado con ABOF; elpaciente fue revisadoclínicayradiográficamentecadamesdurante15meses.
Resultados: Tanto el dolor como la función post-operatoria mejoraron de forma significa-tiva,alcanzando94puntoseneltobilloizquierdo(puntuaciónpreoperatoriade40puntos)y 92puntoseneltobilloderecho(puntuaciónpreoperatoriade42puntos).
Conclusiones:El aloinjerto tibio-astragalino fresco parece ser una buena alternativa a la artrodesisoalaartroplastiaeneltratamientodelaartropatíadegenerativadeltobilloyde losdefectoscondralesarticulares,principalmenteenpacientesjóvenesyactivos.Estatécnica consigueunbuenaliviodeldolor,mantienebuenamovilidadarticularydisminuyeelriesgode artrosisdelasarticulacionesadyacentes.
©2011SECOT.PublicadoporElsevierEspaña,S.L.Todoslosderechosreservados.
Introduction
Osteoarthritis of the ankle can be secondary to any numberof causes, includingidiopathic osteoarthritis, sys-temic polyarthritis, such as rheumatoid arthritis and other polyarthritides, and post-traumatic osteoarthritis. Post-traumatic osteoarthritis is the most common form, accountingformorethan70%ofallcasesofosteoarthritis oftheankle.1Togetherwiththat,thereareseveralreasons
that make osteoarthritis of the ankle a different disease from osteoarthritis of the hip or knee: patients are gen-erally youngerand theweight-bearingarticular surfaceis significantly smaller, causing greater pressure per unit of surface area; the ankle is surrounded by a fine layer of softtissue,whichcanleadtoseriouscomplicationsinskin healing.2
Lesionsofthearticularcartilageofthetibio-astragaline jointandsecondaryosteoarthritisoftheankleoftencause pain,limitedmobility,andfunctionaldisability.Thesurgical optionswhenconservativetreatmentfailsarelimited.For alongtime,arthrodesishasbeenconsideredtobethe stan-dardforcomparisonduetoitsabilitytoachievesatisfactory reliefofpain,3 althoughitdoes entailinherent functional
limitations,4 affects overall gait efficiency, and leads to
predictable, progressive osteoarthritis of the ipsilateral hindfoot.5 Total arthroplasty of the ankle conserves joint
mobility, with improvement in the gait, decreasing the overloading affecting neighboring joints, although it does notappeartoachievethesamelevelofsuccessandsurvival rateasotherarthroplastiesofthelowerlimb,6,7especially
in young,active patients,8 thanksto ahigh rateof
mobi-lizationofthecomponents.Theseissuesprovokethesearch foramethodtorepairtheosteoarthritic joint.Theuseof frozen allografts asa salvage procedure inthe treatment
ofmalignantbone tumors,ontheirownor incombination withprostheses,hasalsobeenwelldocumented.9
Material
and
method
We present the case of a 30-year-old male patient with bilateral post-traumatic osteoarthritis of the ankle. At 18 years of age, the patient fell from a height of some 15m while jumping from one balcony to another, suf-fering several limb fractures. His left ankle presented a fracture of the medial malleolus and astragalus, and his right ankle suffered bimaleolar and astragalus fractures. Allthefracturesweretreatedsurgically:ontheleftankle, osteotaxiswasperformed inassociation with osteosynthe-sis of the medial malleolus and the astragalus, whereas on the right ankle, osteosynthesis of the astragalus and both malleoli was carried out. All fractures consolidated andthe osteosynthesismaterial wasremoved threeyears later.
However,thepatient developedserious post-traumatic osteoarthritisofbothankles(Figs.1and2),withsignificant functionallimitationthatforcedhim touseinsolesonthe outeredgeofbothfeettoimprovesupport,aswellasthe formationofhyperkeratosisonthelateraledgesofhisfeet. Attheageof29,herequestedsurgerytotreathisserious disorderandlimitedgait.Thephysicalexaminationrevealed mobilitythatwasallbutabsent,withoccasionalpainthat got worse when he walked, above all in his left ankle (40pointsonthescaleoftheAmericanOrthopedicFootand AnkleSurgeons[AOFAS]).
Figure1 X-rayoftherightankle.
Surgicalprotocol
Thepre-operative evaluation included acomplete clinical history and examination, weight-bearing anteroposterior andlateralX-raysofbothankles,andacomputed tomogra-phy(CT)oftheleftankle.Anappropriatedonorwaschosen based on joint size and the transplant was performed 7 days after the donor’s death. Blood work was done to detectHIV,syphilis,andhepatitisBandC.Theextraction ofthedonor’sankleconsistedofresectingtheentirejoint, includingthecapsuleandsynovialmembrane.Theimplant wascarriedoutthroughananteriorapproachoftheankle, betweentheanteriortibialandtheextensorhallucislongus
tendons; the neurovascular pedicle was mobilized and
Figure2 Computedtomographyoftheleftankle.
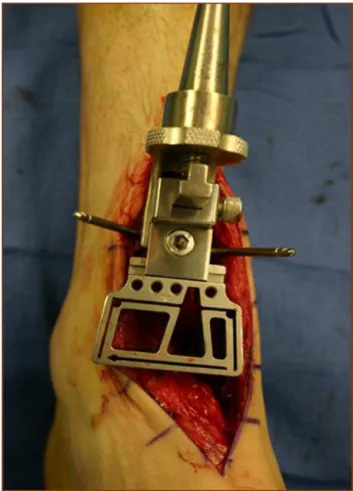
displacedlaterally,severingtheretinaculumlongitudinally toapproachthearticularcapsule.Thecuttingguideofthe Agility®prosthesis(DePuy,Johnson&Johnson,NJ,USA)was
usedtoperformtheosteotomiesofthetibiaandastragalus (Fig. 3).2 The medial aspect of the medial malleolus was
also severed using the same guide, leaving the articular aspect ofthefibularmalleolus intact.The allograftswere pressfittedintothehostboneandfixedwithcompression screws.
Thepatientremainedhospitalizedforoneweek;hisfoot was immobilized witha plaster boot for 4 weeks and he wasnotallowedtoputweightonit.Beginninginthefifth week,hebegantouseawalkingorthosisfor24h,untilthe fifthpost-operativemonth.Startinginthesixthmonth,the orthosiswasremovedandfullweight-bearingwasallowed. InJune2011,oneyearfollowingsurgeryontheleftankle, thesametechniquewascarriedoutontherightanklethat presentedascoreof42ontheAOFASscale.
Results
Fifteenmonthsfollowingthesurgeryonhisleftankle(Fig.4) andthreemonthsaftertheinterventiononhisrightankle (Figs.5and6),thepatientisasymptomatic, walkingwith plantigrade support, without pain, wearing a boot-type walking orthosis 24h a day on his right leg. The physi-calexaminationshows verygoodmobility intheleftankle (45◦plantarflexionand25◦dorsalflexion),withascoreof94
ontheAOFASscale.Therightanklepresents40◦dorsal
flex-ionand20◦plantarflexion(92pointsontheAOFASscale).
Figure 3 Cutting guide of the Agility® (DePuy, Johnson &
Johnson,NJ,USA)prosthesisplacedonthedistaltibiainJeng CL.2
certaindegree of osteocondensation(Figs. 5and 6)three monthsafter surgery,which couldgeneratecomplications in the future, such as collapse of the graft, osteolysis, and osteonecrosis, previously described in the literature. However,forthetimebeing,thepatientissatisfied, asymp-tomatic,pain-free,andhasgoodmobilityinbothankles.
Figure5 X-rayoftherightanklethreemonthsaftersurgery.
Discussion
Ankle joint transplants using fresh osteochondral allo-grafts of both surfaces have been sporadically reported intheliterature.The conceptofbiological reconstruction usingosteochondralgraftsrepresentsanalternativeinthe treatment of degenerative articular injury. Although the
Figure6 X-rayoftherightanklethreemonthsaftersurgery.
clinicaluseofallograftsinthekneehasbeenmorewidely reported, their use in other joints, such as the ankle, is still in the pipeline.8 Fresh osteochondral allografts are
compounds consistingof viable, mature hyalinecartilage, anatomicallyand architecturally appropriate,anchoredin acellular subchondral scaffolding, practically forming a structurally and functionally intact unit to replace the impairedor absent componentscorrespondingtothehost joint.Ahighpercentageofchondrocyteshavebeenshown to survive for several years after being transplanted.10,11
The support bone eventually consolidates with the host bonethroughprogressivereplacement.11 Studiesof
recov-ered pieces have shown that the chondrocytes survive, both when stored at low temperatures12,13 as well as
when transplanted, and they maintain their metabolic activity14 and the surrounding extracellular matrix,15,16
thus protecting them from host immunosurveillance.17
Nonetheless, a certain risk of disease transmission does persist.8
Properpatientselection isessential.The pre-operative evaluationincludesacompleteclinicalhistoryandfull phys-icalexamination.Thehistorymustdocumentpriortrauma, surgicalinterventions,andco-morbidities.Furthermore,it is important to understand the patient’s functional and occupational needs, as well astheir expectations insofar asthe outcome of the intervention is concerned. A good resultoftheankletransplantdependsonproperselection ofthesize ofthe allograftwithrespecttothe host,ona meticulouspreparationoftheimplantandofthereceptor bed,maintainingproperthicknessofthetransplantedpieces and adequate stabilization by means of osteosynthesis.2
The ankle transplantcan be performed through an ante-rior approach, as in this case, or through a transfibular lateral approach.2,9 A meticulous rehabilitation protocol
is essential toachieving an adequate amplitude of move-ments. Our patient followed the protocol described by Gianninietal.18:twoweekswithplaster,beginning
continu-ouspassivemobilityimmediatelyafterremovingtheplaster; non-weight-bearingwalkingwithcrutchesforthethreefirst months; on the fourth month, start partial support once earlysignsofconsolidationbecomeapparent,allowingfull supportbetween6and8monthsafterthesurgery.Atthis time,thepatientcanbeallowedtocycleandswim,withall high-impactsportsprohibitedforthefirstyear.9
Thesesame authors18 have conducteda post-operative
evaluation of their patients by means of arthroscopy and biopsy;oneyearafterimplantation,thehistologicalstudy showed few proteoglycans with disorganized collagenous fibers, butwithmore than90% ofthe chondrocytesbeing viable.9,18 Iffailureisdefinedashavingtoremovethe
allo-graftfromtheankle,Kimetal.20obtaineda100%survival
rateat21months;Meehanetal.23achievedasurvivalrate
of54%attwoyears;Gianninietal.19,at31months,attained
81%survival.
In the case we report, the screws were placed from anteriorandobliquely,insteadof perpendicularandmore posteriorinthejoint.Thismayaccountforacertaindegree of collapse in the posterior part of the allograft (Fig. 6). Together with this, the patient began to use a walking orthosis (boot) 24h a day on week five, although partial weight-bearingwasnotalloweduntilthefifthmonth.Total support, with normal footwear, began around the sixth monthfollowingsurgery.
In the review of the literature, we have found differ-entmodesoffailureoftheimplant:non-uniontothehost bone,osteoarthritis,fracture,andcollapse.Theearly fail-ures were attributed to a suboptimal adaptation of the implantsizeandtotechnicalmistakes,whichtendedtolead tofragmentationandcollapseinthisbiomechanicallyhighly demandingenvironment.18,19Thereareothercomplications
associatedwiththetechnique,suchasintra-operative frac-tures(ofthegraftor ofthefibula),poorimplant fixation, sub-luxation, infection, and osteolysis. Structural failures usuallyoccurinthefirst6---12months.8Theevolutive
radio-graphicstudyshowedjointimpingement,osteophytosis,and sclerosis,evenincaseswithexcellentclinicaloutcomes.If thesecomplicationsappear,thesurgeonmustbeprepared totreat them by meansof articulardebridement, repeti-tion of the graft, or removal of the material. When the procedurefails,thesolutionsarereplacementarthroplasty orarthrodesis.20
Improvementsin surgicaltechnique andgraftselection haveyieldedbettershort-termoutcomes,butgraftsurvival isasyetunknown.Theclinicalresultsofankletransplants appeartobequitegoodinitially,butdeteriorateovertime. Experiencelowerscomplicationrates,duetobettersoft tis-suetreatment,adequateexposure,theuseofcorrectsize grafts,cleaningofthemedialandlateraloutlets,avoiding impactionandbettergraftalignment.Gianninietal.18
ankleand92fortheright,althoughshort-termresultsare similartothoseofotherauthors.18,20,21
Someauthorsbelieveankletransplantationtobethe pri-marytreatment in osteochondrallesionsof theastragalus andasaninterventiontogainsometimeinsalvagesituations forpost-traumatic osteoarthritides,secondary toarthritis, toosteonecrosis,or tohaemophilicjoint diseaseinyoung patients. Jeng etal.22 suggest that transplant candidates
should be patients who are too young for a replacement arthroplasty, with a low body mass index, and normal limbalignment.Gianninietal.18,19putforth morespecific
inclusionandexclusioncriteria: patientsundertheageof 55 years; grade III unilateral osteoarthritis of the ankle; unalteredankleanatomy;noosteopenia,rheumatoid arthri-tis, infection or vascular or neurological disease. Poor alignmentof thelimb orinstabilitywould constitute rela-tivecontraindications.Görtzetal.8considerinflammatory
arthritistobearelativecontraindicationfortheprocedure; theyhadworseoutcomesinyoungpatientswithahighbody massindex,andsignificantpre-operativeangularalteration. Thebipolarfreshosteochondralallograft(BFOA)appears tobeagoodalternativetoarthrodesisandarthroplastyin post-traumaticosteoarthritisoftheankle.Itprovidespain reliefandrecoveryofanklejointmobility,aspectsthatare veryimportantinyoung,activepatients,whoarenotgood candidatesforarthrodesisortotalarthroplasty.The distinc-tiveadvantages ofthearticularallograftareconservation of the bony substrate and prevention of osteoarthritis of nearbyjoints.The procedureentailsvarioustechnical dif-ficulties that require a long learning curve. Proper graft sizeselection,adaptationandstablefixationanddeferring supportappeartobeessentialfactorsinobtaining agood result.
Withthelimitednumberof ankletransplantspublished andtherelativelyhighrateoffailure,itisdifficultto deter-minewhoisthebestpatientforthistechnique.Althoughthe preliminaryresultsarepromising,withverygoodresultsand morethanhalfofthepatientsachievingpainreliefinseveral published series, controlled comparative studies, against both arthrodesis andankle arthroplasties andwith longer follow-up periods,are needed toconfirm bettercartilage survivalandthevalidityofthistechnique.
Level
of
evidence
LevelofevidenceII.
Ethical
responsibilities
Protectionofpeopleandanimals.Theauthorsstate that noexperimentshavebeencarriedoutonhumansoranimals. Confidentialityofthedata.Theauthorsstatethatthis arti-clecontainsnopatientdata.
Righttoprivacyandinformedconsent.Theauthorsstate thatthisarticlecontainsnopatientdata.
Conflict
of
interests
Theauthorshavenoconflictofintereststodeclare.
Acknowledgements
WewouldliketoexpressourspecialthankstoProfessorS. Giannini,RizzoliOrthopaedicInstitute,BolognaUniversity, Italy.
References
1.HubbardTJ,Hicks-LittleC,CordovaM.Mechanicaland senso-rimotorimplicationswithankleosteoarthritis.ArchPhysMed Rehabil.2009;90:1136---41.
2. Jeng CL. The current status of fresh osteochondral allo-grafttransplantation for anklearthritis.SeminArthro. 2010; 21:253---8.
3.CoesterLM,SaltzmanCL,LeupoldJ,PontarelliW.Long-term resultsfollowinganklearthrodesisforpost-traumaticarthritis. JBoneJointSurgAm.2001;83-A:219---28.
4.ThomasR,Daniels TR,ParkerK.Gait analysisand functional outcomesfollowinganklearthrodesisforisolatedankle arthri-tis.JBoneJointSurgAm.2006;88:526---35.
5.Sheridan BD, Robinson DE, Hubble MJ, Winson IG. Ankle arthrodesis and its relationship to ipsilateral arthritis of the hind- and mid-foot. J Bone Joint Surg Br. 2006;88: 206---7.
6.Anderson T, Montgomery F, Carlsson A. Uncemented STAR totalankleprostheses.Threetoeight-yearfollow-upof fifty-one consecutive ankles. J Bone Joint Surg Am. 2003;85-A: 1321---9.
7.KnechtSI,EstinM,CallaghanJJ,ZimmermanMB,AllimanKJ, Alvine FG,et al. The agility totalankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86-A:1161---71.
8.GörtzS,BugbeeWD.Freshosteochondralallograftresurfacing oftheankle.OperTechOrthop.2006;16:244---9.
9.GianniniS,BudaR,VanniniF,BevoniR,GrogoloB.Totaljoint reconstructionofthearthritic anklejoint usingbipolarshell allograft.OsteoarthritisCartilage.2007;15:B34.
10.McGoveranBM,PritzkerKP,ShashaN,PriceJ,GrossAE. Long-termchondrocyteviabilityinafreshosteochondralallograft.J KneeSurg.2002;15:97---100.
11.OakeshottRD,FarineI,PritzkerKP,LangerF,GrossAE.Aclinical andhistologicanalysisoffailedfreshosteochondralallografts. ClinOrthopRelatRes.1998:283---94.
12.AllenRT,RobertsonCM,PennockAT,BugbeeWD,HarwoodFL, Wong VW, et al. Analysis of stored osteochondral allografts at the time of surgical implantation. Am J Sports Med. 2005;33:1479---84.
13. Williams RJ, Dreese JC, Chen CT. Chondrocyte survival and material properties of hypothermically stored cartilage: an evaluationoftissueusedforosteochondralallograft transplan-tation.AmJSportsMed.2004;32:132---9.
14.GrossAE,Aubin P,CheahHK,DavisAM,Ghazavi MT.Afresh osteochondral allograft alternative. J Arthroplasty. 2002;17 Suppl1:50---3.
15.Convery FR, Akeson WH, Amiel D, Meyers MH, Monosov A. Long-termsurvivalofchondrocytesinanosteochondral artic-ularcartilageallograft.Acasereport.JBoneJointSurgAm. 1996;78:1082---8.
16.Czitrom AA, Keating S, Gross AE. The viability of articular cartilageinfreshosteochondralallograftsafterclinical trans-plantation.JBoneJointSurgAm.1990;72:574---81.
17.LangerF,GrossAE.Immunogenicityofallograftarticular carti-lage.JBoneJointSurgAm.1974;56:297---304.
19.GianniniS,BudaR,FaldiniC,VanniniF,RomagnoliM,Grandi G,etal.Thetreatmentofsevereposttraumaticarthritisofthe anklejoint.JBoneJointSurgAm.2007;89ASuppl3:15---28. 20.KimCW,JamaliA,TontzWJr,ConveryFR,BrageME,BugbeeW.
Treatmentofpost-traumaticanklearthrosiswithbipolar tibio-talar osteochondral shellallografts.Foot AnkleInt.2002;23: 1091---102.
21. MeehanR,McFarlinS,BugbeeW,BrageM.Freshankle osteo-chondralallografttransplantationfortibiotalarjointarthritis. FootAnkleInt.2005;26:793---802.