www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Predictive
factors
of
occult
neck
metastasis
in
patients
with
oral
squamous
cell
carcinoma
夽
Renato
Fortes
Bittar
∗,
Homero
Penha
Ferraro,
Marcelo
Haddad
Ribas,
Carlos
Neutzling
Lehn
HospitaldoServidorPúblicoEstadual(IAMSPE),SãoPaulo,SP,Brazil
Received30June2015;accepted18September2015 Availableonline17December2015
KEYWORDS
Headandneck neoplasms; Oralneoplasms; Survivaloutcomes; Lymphnode metastasis; Prognosis; Squamouscell carcinoma
Abstract
Introduction:Itiswellestablishedthatcervicallymphnodemetastasisisthemostimportant prognostic factor inpatients withoral squamous cellcarcinomaofthe upperaerodigestive tract.Thedefinitionofparametersandclassificationsthatcouldseparatepatientsingroupsof low,intermediateandhigh-riskisbeingattemptedforseveralyears.
Objective: Theobjectiveofthisstudywastodeterminepossiblepredictivefactorsrelatedto theoccurrenceofoccultcervicallymphnodemetastasisthroughtheanalysisof histopatholog-icalreportsofsurgicalspecimensobtainedafteroralsquamouscellcarcinomaresectionand selectiveneckdissectionsofpatientsinitiallyclassifiedasN0.
Methods:Thiswasaprimary,retrospective,observational,case---controlstudy. Histopatholog-ical reportswere reviewedtodetermineif somefindingswere relatedtotheoccurrenceof occultlymphnodemetastasis.Theeventsanalyzedwereoralcavitysubsites,pT-stage, mus-cularinfiltration, desmoplasia, vascularemboli,perineuralinfiltration, tumor thickness and compromisedmargins.
Results:Occult cervicalmetastasisaccounted for 19.10percent ofthecases. Desmoplasia, perineuralinfiltration,tumor thicknessandpT4astage arepredictivefactorsofoccultneck metastasis(p-value=0.0488,0.0326,0.0395,0.0488,respectively).
Conclusion: Theaccuratedefinitionofpredictivefactorsofoccultcervicalmetastasismayguide the selectionofpatients thatshouldbe referred toradiotherapy,avoiding theunnecessary exposureoflow-riskpatientstoradiationandallowingabetterregionalcontrolofthedisease inthoseofmoderateorhighrisk.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽
Pleasecitethisarticleas:BittarRF,FerraroHP,RibasMH,LehnCN.Predictivefactorsofoccultneckmetastasisinpatientswithoral squamouscellcarcinoma.BrazJOtorhinolaryngol.2016;82:543---7.
∗Correspondingauthor.
E-mails:renatobittar@yahoo.com,rfbittar@gmail.com(R.F.Bittar).
http://dx.doi.org/10.1016/j.bjorl.2015.09.005
PALAVRAS-CHAVE
Neoplasiasdecabec¸a epescoc¸o;
Neoplasiasorais; Resultadosde sobrevida;
Metástaselinfática; Prognóstico; Carcinoma espinocelular
Fatorespreditivosdemetástasescervicaisocultasempacientescomcarcinoma epidermóidedeboca
Resumo
Introduc¸ão:Já ébemestabelecido queametástase oculta em linfonodo cervicalé ofator prognósticomaisimportanteempacientescomCarcinomaepidermóidedeboca(CEB)dotrato aerodigestivosuperior.Háanospesquisadorestentamdefinirparâmetroseclassificac¸õesque poderiamsepararospacientesemgruposdebaixo,médioealtorisco.
Objetivo:Oobjetivodesteestudofoideterminarpossíveisfatorespreditivosrelacionadoscom aocorrênciademetástaseocultaemlinfonodocervical,pormeiodaanálisedelaudos histopa-tológicos de espécimescirúrgicos obtidos após ressecc¸ão de CEBe dissecc¸ões seletivas do pescoc¸oempacientesinicialmenteclassificadoscomoN0.
Método: Estefoiumestudoprimário,retrospectivo,observacionaledecaso-controle.Laudos histopatológicosforamrevisadospara determinarsealgunsresultadosestavamrelacionados comaocorrência de metástases em linfonodosoculto. Oseventosanalisados foram: subsí-tiosdentrodacavidadeoral,estágio-pT,infiltrac¸ãomuscular,desmoplasia,emboliavascular, infiltrac¸ãoperineural,espessuradotumoremargenscomprometidas.
Resultados: Metástasescervicaisocultasforamresponsáveispor19,10%doscasos.Desmoplasia, infiltrac¸ãoperineural,espessuradotumoreestágiopT4aforamfatorespreditivosdemetástase cervicaloculta(p=0,0488,0,0326,0,0395,0,0488,respectivamente).
Conclusão:A definic¸ãoprecisadosfatorespreditivos demetástasecervicalocultapode ori-entaraselec¸ãodepacientesquedevemsersubmetidosaradioterapia,evitandoaexposic¸ão desnecessáriadospacientesdebaixoriscoàradiac¸ão,emelhorarocontroleregionaldadoenc¸a empessoasderiscomoderadooualto.
© 2015 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Itiswellestablishedthatcervicallymphnodemetastasisis themostimportantprognosticfactor inpatientswithoral squamouscellcarcinoma(OSCC)oftheupperaerodigestive tract.1---4
Thereisadistinctrelationshipbetweenthenumberand levelofcervicalnodescompromised,capsularruptureand positivemarginswithfive-yearsurvival.1---5
Neck palpation during clinical exam still has great value; however, it has been shown that this may result in a false-negative rate of around 28.9 percent.2
Pal-pation sensitivity was estimated at 75 percent, and specificity at 83 percent, against 81 percent of sensi-tivity and 83 percent of specificity shown by computed tomography. Other authors demonstrated palpation sen-sitivity at 82 percent and specificity at 80 percent and found no significant differences comparing with cervical ultrasound.6,7
Neckdissectioniswellacceptedfordefinedevidenceof cervicallymphnodemetastasis;however,thereisstillgreat controversyaboutthetypeandextensionofnecktreatment inclinicallynegativecervicaldisease.2---5
The definition of parameters and classifications that couldseparatepatientsingroupsoflow,intermediateand highriskisbeingattemptedforseveralyears.Studieshave impliedfactorssuchashistologicgrade,muscular infiltra-tion,desmoplasia, vascularemboli,perineuralinfiltration, tumorthicknessandcompromisedmargins.5,8---11
Thepresence ofthesemultiple variablesofrecurrence wasapreciseindicatorofpoorprognosis.5,12,13Other
stud-ies have shown that lymphatic or vascular invasion is an independentriskfactor.14,15
Theobjectiveofthisstudywastodeterminepossible pre-dictivefactorsrelatedtotheoccurrenceofoccultcervical lymphnodemetastasis throughtheanalysisof histopatho-logical reports of surgical specimens obtainedafter OSCC resectionandselectiveneckdissectionsofpatientsinitially classifiedasN0.
Methods
This was a primary, retrospective, observational, case---controlstudy.
Datawasobtainedfromasingleinstitution.Theresearch wasperformedfrom1995to2014.
Histopathological data was obtained using chart num-bers. No intervention was performed and no attempt to contactpatientstoobtainanykindofinformationwasmade. Patient’snamesor anyother meansofidentification were notused.Thisstudywasinaccordancewithallprinciplesof theHelsinkiDeclaration.
The search started with the gathering of all records involving oral cancer.After eliminatingalldoubleentries, wereviewedallpatients’chartsandselectedeverypatient thatwasinitiallyclassifiedasN0.
refusedsurgicaltreatment,patientswhohadtheneck stag-ing changed at the pre-operative period, patients with tumorssmallerthan1cmwhowerenotsubmittedto elec-tiveneckdissection.
Patientswerethendistributedintotwogroups:
GroupA:patientsN0whoweresubmittedtooralcancer resectionwithelectiveneckdissection(levelsI,IIandIII) andtheabsenceofoccultlymphnodemetastasis. GroupB:patientsN0whoweresubmittedtooralcancer resectionwithelectiveneckdissection(levelsI,IIandIII) andthepresenceofoccultlymphnodemetastasis.
Histopathologicalreports werethenaccessed to deter-mine if some findings were related to the occurrence of occult lymph node metastasis. The events analyzed were oral cavity subsites, pT-stage, muscular infiltration, desmoplasia,vascularemboli,perineuralinfiltration,tumor thickness and compromised margins. These were individ-ually analyzed to determine whether those events could be relatedto occult lymph node metastasis with statisti-calsignificance,andifitcouldbeusedaspredictivefactor todetermine thepresenceofnodemetastasis inclinically negativenecks.
Results
Initially, we retrieved 183 patients, and after the exclu-sion criteria remained with 157 patients. One hundred and twenty-seven patients did not present with occult lymphnodemetastasis andwereincluded ingroupA.The remaining30patientswereincludedingroupB.Occult cer-vicalmetastasis accounted for 19.10 percentofthe cases (30/157).
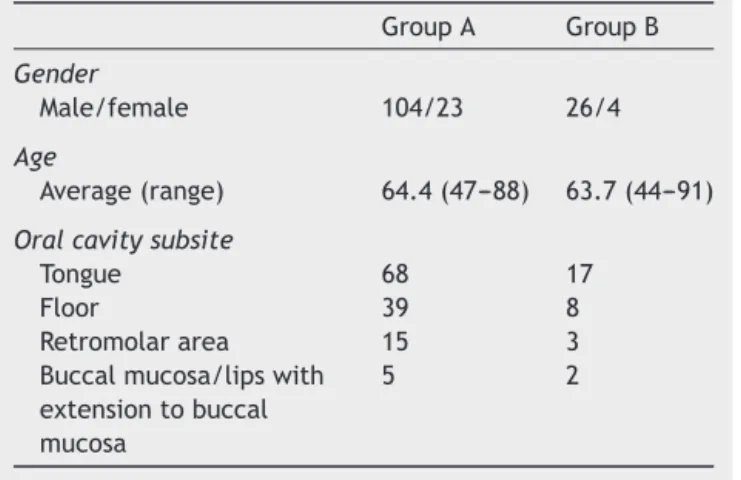
IngroupA,theaverageagewas65.4years(47---88years old).Maleswere104,andfemales23.IngroupB,the aver-ageage was63.7 years(44---91yearsold).Maleswere 26, andfemales4.
Thecompromisedoralcavitysubsitesweretongue54.14 percent(68casesingroupAand17ingroupB),floor29.93 percent(39casesingroupAand8ingroupB), retromolar area11.46percent(15casesingroupAand3ingroupB),and buccal mucosa/lipswithextension tobuccal mucosa 4.45 percent(5 cases in group Aand 2 in group B). All of the casesinthegingivaweresmallerthan1cmandsubmitted tolocalresectionwithsafetymarginswithoutelectiveneck dissection---therefore,werenotincluded(Table1).
Oddsratio,confidenceintervalandp-valueaccordingto oralcavitysubsitesareshowninTable2.
The analysis of the compromised levels revealed that levelIwaspositivein23.33percent(7/30),levelIIin53.3 percent(16/30),andlevelIIIin23.33percent(7/30).Five patients were submitted to bilateral dissections of levels I,II, III becausethe tumor had alreadycrossedthe facial midline.
Oftheeventsanalyzed,muscularinfiltrationwaspresent in49.04percentofthecases,desmoplasiain7.64percent, vascularemboliin12.73percent,perineuralinfiltrationin 27.38percent,tumorthickness(≥4mm)in66.87percent,
compromised marginsin 20.38percent,pT1 in 17.19 per-cent,pT2in34.39percent,pT3in40.76percent,andpT4a
Table1 Demographicsandoccurrencesubsites.
GroupA GroupB
Gender
Male/female 104/23 26/4
Age
Average(range) 64.4(47---88) 63.7(44---91)
Oralcavitysubsite
Tongue 68 17
Floor 39 8
Retromolararea 15 3
Buccalmucosa/lipswith extensiontobuccal mucosa
5 2
Table 2 Odds ratio, confidence interval and p-value accordingtooralcavitysubsites.
OR 95%CI p-Value
Tongue 1.1346 0.5088---2.5300 0.7576 Floor 0.8205 0.3360---2.0035 0.6641 Retromolararea 0.8296 0.2241---3.0714 0.7797 Buccalmucosa/lips
withextensionto buccalmucosa
1.7429 0.3214---9.4502 0.5195
in7.64percentofthecases.AllpT4bcaseswereamongthe excludedones.
Ofthesevariables,desmoplasia, perineuralinfiltration, tumorthickness(≥4mm),andpT4presentedwithapositive
associationwithoccultcervicalmetastasis,withstatistical significance(p<0.05)(Table3).
Discussion
Thiscase---controlstudywascomposedof157patientswith oralsquamouscellcarcinomawhowereinitiallydiagnosed asN0.Thesamplewasgatheredfrom1995to2014.
Ourprimaryconcernwastotrytodetermineany predic-tivefactorsinhistopathologicalreportsthathadapositive relationshipwiththeoccurrenceofoccultcervical metasta-sis.
The estimated rateof occult lymphnode metastasis is around15---34 percent, according to some studies.16---18 In
ourstudy,of the157 patients,we have found 30 tohave occultcervicalmetastasisaftersurgery,whichcorresponds to19.10percent.
Itwasacomprehensivestudywithasignificantnumber ofcasesoforalcancerandwithmultivariateanalysis.
Mosttumorswerelocatedatthetongueandfloorofthe mouth,andaccordingtoliteraturethesesubsitesaremore relatedtoahigherriskofoccultcervicalmetastasis; how-ever,ouranalysis,showninTable2,doesnotallowtheclear indicationofaparticularoralcavitysubsiteasapredictive factorwithstatisticalsignificance.
Table3 Theincidenceofthestudiedfactorsinbothgroups,oddsratio,confidenceintervalandp-value.
n=157 GroupA(127) GroupB(30) OR 95%CI p-Value
Muscularinfiltration 60 17 1.4603 0.6550---3.2556 0.3547
Desmoplasia 7 5 3.4286 1.0063---11.6818 0.0488
Vascularemboli 13 7 2.6689 0.9602---7.4182 0.0598
Perineuralinfiltration 30 13 2.4725 1.0780---5.6712 0.0326
Tumorthicknessa 80 25 2.9375 1.0534---8.1915 0.0395
Compromisedmargins 27 5 0.7407 0.2592---2.1170 0.5754
pT1 25 2 0.2914 0.0650---1.3058 1.611
pT2 48 6 0.4115 0.1569---1.0787 1.806
pT3 47 17 2.2259 0.9932---4.9885 0.0520
pT4a 07 5 3.4286 1.0063---11.6818 0.0488
a≥4mm.
B.The calculatedoddsratio(1.4603---CI:0.6550---3.2556) doesnotallowtodetermineitasariskfactorforoccultneck metastasis(p>0.005).Asamatteroffact,muscular infiltra-tionremainsanunclearfactor,withsomeauthorsdiscussing anincreasedriskwhentheinvasionexceeds4mm.2,11,19,20
Desmoplasiaandvascularemboliwererelatedwiththe presence of cervical metastasis by some authors. In this study,desmoplasia occurred in seven patients in group A and five in group B, with an odds ratio of 3.4286 (CI: 1.0063---11.6818) being a risk factor for occult cervical metastasiswithstatisticalsignificance(p=0.0488).10,11
Brandwein-Gensler etal. didnot findstatistical signif-icancewith vascular invasion.We have found 13 cases in groupA andseven casesin groupB withan oddsratioof 2.6689(CI:0.9602---7.4182),buta p-valueof 0.0598---not statisticallysignificant,butwithalikelytendencytoit.21
Regarding perineural infiltration, several studies have shownit asan independentrisk factorfor theoccurrence ofoccultcervical metastasis.21---23 We havefound 30cases
ingroup A and13 at group B.Odds ratio was2.4725 (CI: 1.0780---5.6712),withap-valueof0.0326---therefore,with statistical significance and in concordance with previous studies.
Anotherwell-studied factoristumorthickness.Itisnot welldefinedwhatshouldbethecorrectparameterto con-sider. Different measures can be found in the literature, somewithacut-offof3mm,others,4mm.23---25
Weadoptedthe4mmparametersinceitisthemostused inthecurrentliterature.Wehaveobserved80casesingroup Aand25ingroupB.Thecalculatedoddsratiowas2.9375(CI: 1.0534---8.1915),witha p-value of0.0395, andthat result seemstoberatherintuitivetoexplainitsrelationshipwith occultcervicalmetastasis.
TumorlengthwasalsoanalyzedbasedonthepTNMscale, andpT4apresented asariskfactor, withanoddsratioof 3.4286(CI:1.0063---11.6818) anda p-value of0.0488. The otherstagesdidnotdemonstrateapositiveassociationwith occultneckmetastases;however,itisworthmentioningthat pT3 with an odds ratioof 2.2259 (CI:0.9932---4.9885), p-value0.0520, showedapossible tendency toitaswell as vascularinvasion,aspreviouslymentioned.
Atlast,wehaveanalyzedifmarginswerecompromised. Wehavefound27casesingroupAandfivepatientsingroup B.Theestimatedoddsratiowas0.7407(CI:0.2592---2.1170), andap-valueof0.5754.
The constant evolution of the treatment of oral squa-mous cell carcinoma has made possible to better select patientswhowillundergoelectiveneckdissections.When correctlyindicated,surgicaltreatmentoffersgreatoutcome in five-yearsurvival. However,thisoperation evolves pos-siblemajorcomplications, suchasspinal nervelesionand significantestheticcompromise.
Theuseofthesentinellymphnodemappingisone tech-niquethatisbeingstudiedinheadandneckcancersfor a longtime.Ithasprovenitsvalueinmelanomasandbreast cancers, and several centers around the globe are using itwithsatisfactoryresults.26,27 Inourservice,none ofthe
caseswassubmittedtothistechnique.
ElectiveneckdissectionevolvedlevelsI,II andIII.This type of neck treatment is the standard procedure in our service,withitseffectivenessprovenintheliterature.28---30
We found that levels I and III were equally compromised with 23.33 percent of the cases. Level II was positive in 53.3 percent of the cases. These cases were posteriorly referredtotherapeuticnecktreatmentwithmodified radi-calneckdissectionorradiochemotherapyinthecaseswhere patients refused to undergo another surgery or did not presentthemselveswithclinicalconditionsforasecondary surgery(5/30).
The present study focused only at the histopatholog-ical analysis to determine possible predictive factors for occultneckmetastasis;therefore, someinformation,such asalcoholandtobaccoconsumption,wasnotevaluated,and neitherwasoverall survival rate.We considerthatfuture prospective studies correlating all of these variables are extremelynecessary,consideringthatthevastmajority of studiesinthisfieldareretrospectiveones.
Ontheotherhand,theaccuratedefinitionofpredictive factors for occult cervical metastasis may also guide the selection of patients who shouldbe referred to radiothe-rapy,avoidingtheunnecessaryexposureoflow-riskpatients toradiation and allowing abetter regionalcontrol of the diseaseinthoseofmoderateorhighrisk.
Conclusion
In thisstudy,we have found that desmoplasia, perineural infiltration, pT4a stage and tumor thickness(≥4mm) are
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.KumarT,PatelMD.Patternoflymphaticmetastasisinrelation tothedepthoftumorinoraltonguecancers:aclinico patholog-icalcorrelation.IndianJOtolaryngolHeadNeckSurg.2013;65 Suppl.1:59---63.
2.SparanoA,WeinsteinG, ChalianA,YodulM,WeberR. Multi-variatepredictorsofoccultneckmetastasisinearlyoraltongue cancer.OtolaryngolHeadNeckSurg.2004;131:472---6. 3.DiTroiaJF.Nodalmetastasesandprognosisincarcinomaofthe
oralcavity.OtolaryngolClinNorthAm.1972;5:333---42. 4.TeichgraeberJF,ClairmontAA.Theincidenceofoccult
metas-tasesfor cancer oftheoral tongueand floorof themouth: treatmentrationale.HeadNeckSurg.1984;7:15---21.
5.FanKH,Wang HM,KangCJ,Lee LY,HuangSF, LinCY, etal. Treatmentresultsofpostoperativeradiotherapyonsquamous cellcarcinomaoftheoralcavity:coexistenceofmultipleminor riskfactorsresultsinhigherrecurrencerates.IntJRadiatOncol BiolPhys.2010;77:1024---9.
6.Merritt RM, Williams MF, James TH, Porubsky ES.Detection ofcervical metastasis.A meta-analysis comparingcomputed tomographywithphysicalexamination.ArchOtolaryngolHead NeckSurg.1997;123:149---52.
7.GiancarloT,PalmieriA,GiacomarraV,RussoloM.Pre-operative evaluationofcervical adenopathies intumoursofthe upper aerodigestivetract.AnticancerRes.1998;18:2805---9.
8.Tai SK, Li WY, Yang MH, Chu PY, Wang YF, Chang PM. Perineuralinvasionasamajordeterminantforthe aggressive-nessassociated withincreased tumor thickness in t1-2 oral tongueandbuccalsquamouscellcarcinoma.AnnSurgOncol. 2013;20:3568---74.
9.TaiSK,LiWY,YangMH,ChuPY,WangYF.PerineuralinvasioninT1 oralsquamouscellcarcinomaindicatestheneedforaggressive electiveneckdissection.AmJSurgPathol.2013;37:1164---72. 10.LehnCN,RapoportA.Thedesmoplasticlymphnodereaction
asaprognosticfactorofcancerofthetongueandfloorofthe mouth.SaoPauloMedJ.1994;112:591---6.
11.PimentaAmaralTM,DaSilvaFreireAR,CarvalhoAL,PintoCA, KowalskiLP.Predictivefactorsofoccultmetastasisand prog-nosisofclinicalstagesIandIIsquamouscellcarcinomaofthe tongueandfloorofthemouth.OralOncol.2004;40:780---6. 12.Jonkman A, Kaanders JH, Terhaard CH, Hoebers FJ, van
den Ende PL, Wijers OB, et al. Multicenter validation of recursivepartitioninganalysisclassificationfor patientswith squamouscellheadandneckcarcinomatreatedwithsurgery andpostoperativeradiotherapy.IntJRadiatOncol BiolPhys. 2007;68:119---25.
13.ParsonsJT,MendenhallWM,StringerSP,CassisiNJ,MillionRR. Ananalysisoffactorsinfluencingtheoutcomeofpostoperative irradiationforsquamouscellcarcinomaoftheoralcavity.IntJ RadiatOncolBiolPhys.1997;39:137---48.
14.LiaoCT, ChangJT, WangHM,NgSH,Hsueh C,LeeLY,etal. Analysisofriskfactorsofpredictivelocaltumorcontrolinoral cavitycancer.AnnSurgOncol.2008;15:915---22.
15.OlsenKD,CarusoM,Foote RL,Stanley RJ,LewisJE,Buskirk SJ,etal.Primaryheadandneckcancer.Histopathologic pre-dictorsof recurrence after neck dissection in patients with
lymph node involvement. Arch Otolaryngol Head Neck Surg. 1994;120:1370---4.
16.NogutiJ,DeMouraCF,DeJesusGP,DaSilvaVH,HossakaTA, Oshima CT, et al. Metastasisfrom oral cancer:an overview. CancerGenomicsProteomics.2012;9:329---35.
17.LeaJ, Bachar G, Sawka AM,Lakra DC,GilbertRW, IrishJC, etal.MetastasestolevelIIbinsquamouscellcarcinomaofthe oralcavity:asystematicreviewandmeta-analysis.HeadNeck. 2010;32:184---90.
18.Fan S,Tang QL,Lin YJ,ChenWL,Li JS,Huang ZQ,et al.A reviewofclinicalandhistologicalparametersassociatedwith contralateralneckmetastasesinoralsquamouscellcarcinoma. IntJOralSci.2011;3:180---91.
19.ByersRM,El-NaggarAK,LeeYY,RaoB,FornageB,TerryNH, etal.Canwedetectorpredictthepresenceofoccultnodal metastasesinpatients withsquamouscarcinoma oftheoral tongue.HeadNeck.1998;20:138---44.
20.KarakidaK,OtaY,AokiT,YamazakiH,TsukinokiK.Examination offactors predictingoccult metastasisofthecervical lymph nodesinT1and T2tonguecarcinoma.TokaiJExp ClinMed. 2002;27:65---71.
21.Brandwein-GenslerM,TeixeiraMS,LewisCM,LeeB,Rolnitzky L, Hille JJ, et al. Oral squamous cell carcinoma: histologic riskassessment,butnotmarginstatus,isstronglypredictive oflocal disease-freeand overallsurvival. AmJ SurgPathol. 2005;29:167---78.
22.FaganJJ,CollinsB,BarnesL,D’AmicoF,MyersEN,JohnsonJT. Perineuralinvasioninsquamouscellcarcinomaoftheheadand neck.ArchOtolaryngolHeadNeckSurg.1998;124:637---40. 23.Chinn SB, Spector ME, Bellile EL, McHugh JB, Gernon TJ,
BradfordCR,etal.Impactofperineuralinvasioninthe patho-logically N0 neck in oral cavity squamous cell carcinoma. OtolaryngolHeadNeckSurg.2013;149:893---9.
24.Po Wing Yuen A, Lam KY, Lam LK, Ho CM, Wong A, Chow TL, et al. Prognostic factors ofclinically stage I and IIoral tongue carcinoma-A comparative study of stage, thickness, shape, growth pattern, invasive front malignancy grading, Martinez-Gimenoscore,andpathologicfeatures.Head Neck. 2002;24:513---20.
25.Spiro RH, Huvos AG,Wong GY, SpiroJD, Gnecco CA,Strong EW.Predictivevalueoftumorthicknessinsquamouscarcinoma confinedto the tongue and floor ofthe mouth.Am J Surg. 1986;152:345---50.
26.Alkureishi LW, Ross GL, Shoaib T, Soutar DS, Robertson AG, ThompsonR,etal.Sentinelnodebiopsyinheadandneck squa-mouscellcancer:5-yearfollow-upofaEuropeanmulticenter trial.AnnSurgOncol.2010;17:2459---64.
27.MelkaneAE,MamelleG, WyciskG, TemamS, JanotF, Casir-aghi O, et al. Sentinel node biopsy in early oral squamous cellcarcinomas:a10-yearexperience.Laryngoscope.2012;122: 1782---8.
28.KowalskiLP,SanabriaA.Electiveneckdissectioninoral carci-noma:acriticalreviewoftheevidence.ActaOtorhinolaryngol Ital.2007;27:113---7.
29.Bajwa MS, McMillan R, Khattak O, Thomas M, Krishnan OP, WebsterK.NeckrecurrenceafterlevelI---IVorI---IIIselective neckdissection inthemanagementoftheclinicallyN0neck in patients with oral squamous cell carcinoma. Head Neck. 2011;33:403---6.