w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Initial
digital
vasculitis
in
a
large
multicenter
cohort
of
childhood-onset
systemic
lupus
erythematosus
Ana
Paula
Sakamoto
a,
Clovis
Artur
Silva
b,c,
Marco
Felipe
Castro
da
Silva
b,
Anandreia
Simões
Lopes
a,
Gleice
Clemente
Souza
Russo
a,
Adriana
Maluf
Elias
Sallum
b,
Katia
Kozu
b,
Eloisa
Bonfá
c,
Claudia
Saad-Magalhães
d,
Rosa
Maria
Rodrigues
Pereira
c,
Claudio
Arnaldo
Len
a,
Maria
Teresa
Terreri
a,∗aUniversidadeFederaldeSãoPaulo(UNIFESP),UnidadedeReumatologiaPediátrica,SãoPaulo,SP,Brazil
bUniversidadedeSãoPaulo(USP),FaculdadedeMedicina,UnidadedeReumatologiaPediátrica,SãoPaulo,SP,Brazil cUniversidadedeSãoPaulo(USP),FaculdadedeMedicina,DivisãodeReumatologia,SãoPaulo,SP,Brazil
dUniversidadeEstadualPaulista(UNESP),FaculdadedeMedicinadeBotucatu,HospitaldasClínicasdeBotucatu,Botucatu,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received26September2016
Accepted10May2017
Availableonline16October2017
Keywords:
Digitalvasculitis
Childhood-onsetsystemiclupus
erythematosus Vasculitis Sledai-2K
a
b
s
t
r
a
c
t
Objectives: Toassessclinicaldigitalvasculitis(DV)asaninitialmanifestationof
childhood-onsetsystemiclupuserythematosus(cSLE)withinalargepopulation.
Methods:Multicentercross-sectionalstudyincluding852cSLEpatients(ACRcriteria)
fol-lowedintenPediatricRheumatologycentersinSãoPauloState,Brazil.
Results:DVwasobservedin25/852(3%)cSLEpatients.Periungualhemorrhagewas
diag-nosedin12(48%),periungualinfarctionin7(28%),tipfingerulcerationin4(16%),painful
nodulesin1(4%)andgangrenein1(4%).Apooroutcome,withdigitalresorption,occurred
in5(20%).ComparisonofpatientswithandwithoutDVrevealedhigherfrequencyofmalar
rash(80%vs.53%,p=0.008),discoidrash(16%vs.4%,p=0.017),photosensitivity(76%vs.
45%,p=0.002)andothercutaneousvasculitides(80%vs.19%,p<0.0001),whereasthe
fre-quencyofoverallconstitutionalfeatures(32%vs.61%,p=0.003),fever(32%vs.56%,p=0.020)
andhepatomegaly(4%vs.23%,p=0.026)werelowerinthesepatients.Frequencyoffemale
gender,severemulti-organinvolvement,autoantibodiesprofileandlowcomplementwere
alikeinbothgroups(p>0.05).SLEDAI-2Kmedian,DVdescriptorexcluded,wassignificantly
lowerinpatientswithDVcomparedtothosewithoutthismanifestation[10(0–28)vs.14
(0–58),p=0.004].VisceralvasculitisordeathwerenotobservedinthiscSLEcohort.The
fre-quencyofcyclophosphamideuse(0%vs.18%,p=0.014)wassignificantlylowerintheDV
group.
∗ Correspondingauthor.
E-mail:teterreri@terra.com.br(M.T.Terreri).
https://doi.org/10.1016/j.rbre.2017.09.002
2255-5021/© 2017 Published by Elsevier Editora Ltda. This is an open access article under the CC BY-NC-ND license (http://
Conclusion: OurlargemulticenterstudyidentifiedclinicalDVasoneoftherareinitial
man-ifestationofactivecSLEassociatedwithamildmultisystemicdisease,inspiteofdigital
resorptioninsomeofthesepatients.
©2017PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Vasculite
digital
inicial
em
uma
grande
coorte
multicêntrica
de
pacientes
com
lúpus
eritematoso
sistêmico
de
início
na
infância
Palavras-chave:
Vasculitedigital
Lúpuseritematososistêmicode
inícionainfância
Vasculite Sledai-2K
r
e
s
u
m
o
Objetivos: Avaliaravasculitedigital(VD)clínicacomoumamanifestac¸ãoinicialdolúpus
eritematososistêmicodeinícionainfância(LESi)emumagrandepopulac¸ão.
Métodos: Estudotransversalmulticêntricoqueincluiu852pacientescomLESi(critériosdo
ACR),acompanhadosemdezcentrosdereumatologiapediátricadoEstadodeSãoPaulo.
Resultados:Observou-seVDem25/852(3%)pacientescomLESi.Diagnosticaram-se
hemorra-giaperiunguealem12(48%),infartoperiunguealemsete(28%),úlceradepontadedígitoem
quatro(16%),nódulosdolorososemum(4%)egangrenaemum(4%).Umdesfechoruim,com
reabsorc¸ãodigital,ocorreuemcinco(20%)pacientes.Acomparac¸ãoentrepacientescome
semVDreveloumaiorfrequênciadeerupc¸ãomalar(80%vs.53%,p=0,008),erupc¸ãodiscoide
(16%vs.4%,p=0,017),fotossensibilidade(76%vs.45%p=0,002)eoutrasvasculitescutâneas
(80%vs.19%,p<0,0001),enquantoafrequênciadecaracterísticasconstitucionaistotais
(32%vs.61%,p=0,003),febre(32%vs.56%p=0,020)ehepatomegalia(4%vs.23%,p=0,026)
forammenoresnessespacientes.Afrequênciadogênerofeminino,oenvolvimentograve
demúltiplosórgãos,perfildeautoanticorposebaixocomplementoforamsemelhantesnos
doisgrupos(p>0,05).AmediananoSledai-2K,exclusiveodescritordeVD,foi
significativa-mentemenornospacientescomVDemcomparac¸ãocomaquelessemessamanifestac¸ão
[10(0a28)vs.14(0a58),p=0,004].Nãoforamobservadasvasculitevisceralnemmorte
nessacoortedepacientescomLESi.Afrequênciadeusodeciclofosfamida(0%vs.18%,
p=0,014)foisignificativamentemenornogrupoVD.
Conclusão: Este grande estudo multicêntrico identificou a VD clínica como uma rara
manifestac¸ão inicialdoLESi ativo,associadaa doenc¸amultissistêmicaleve, apesarda
ocorrênciadereabsorc¸ãodigitalemalgunsdessespacientes.
©2017PublicadoporElsevierEditoraLtda.Este ´eumartigoOpenAccesssobuma
licenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Systemic lupus erythematosus (SLE) is a multisystemic
autoimmunechronicdiseasemorecommoninadults(aSLE),
with only 10–20% of cases beginning during childhood or
adolescence.1–3Childhood-onsetSLE(cSLE)ischaracterizedby
moresevereandcumulativeacuteorganandsystem
involve-mentcomparingtoaSLE.Mucocutaneousinvolvementisone
ofthemostcommonmanifestationsandhasbeenreported
in up to 80% of children and adolescents at the time of
diagnosis.1,2
Vascularinflammatoryprocessisanimportantfeatureof
SLEandaffectsalargesubsetofpatientswithskin
manifes-tationsatany timeofdiseasecourse.4–7 SLEclinicaldigital
vasculitis(DV)includespainfululcerationandnodulesmay
resultinsplinterhemorrhagesanddigitalinfarcts1,8,9andit
maybepresentin16–45%ofaSLEpatients.5,7,8,10
DataoncSLEpatientsarelimitedtocasereportsandsmall
series.1,9,11TherearenopublisheddatacharacterizingDVin
alargepopulationofchildhoodlupuspatients.
Therefore,theobjectiveofthisstudywastoassessDVas
aninitialmanifestationinalargemulticenterstudy,
evalu-atingthepossibleassociationwithdemographicandclinical
features,laboratorialexams,treatmentandoutcomesincSLE
onset.
Methods
Studydesignandpatients
Thisisaretrospectivemulticenterstudyincluding1017cSLE
patientsfollowedintenPediatricRheumatologytertiary
refer-ral centers in São Paulo state, Brazil. One hundred and
sixty-five patientswere excludeddueto: incomplete
medi-calcharts(n=96),undifferentiatedconnectivetissuedisorder
with3orfewerAmericanCollegeofRheumatology(ACR)
crite-riaforSLE12(n=43),isolatedcutaneouslupuserythematosus
(n=11), neonatal lupus erythematosus(n=8), drug-induced
lupus(n=5)andotherautoimmunediseases(n=2).Thus,the
criteria12and presenteddiseaseonsetbefore18yearsold13
withacurrentage upto25years.CommitteeforResearch
Ethicsofeachcenterapprovedthestudy.
Aninvestigatormeetingwasheldforthisstudytodefine
theprotocol,includingdefinitionsofclinical,laboratoryand
treatmentparametersanddiseaseactivityanddamagescore.
Allinvestigatorsusedthesamespecificdatabase.
Patient’smedicalchartsweremeticulouslyrevised
accord-ing to a standardized protocol for demographic data, DV
characteristics,other clinicalfeatures, laboratorialfindings,
therapeuticdataandDVoutcome(digitalresorption,visceral
vasculitis and death). Clinical DV was defined as
ulcera-tion,gangrene,tenderfingernodules,periungualinfarction
orsplinterhemorrhagesofthedigitsaccordingtoSLEDisease
ActivityIndex2000score(SLEDAI-2K).14
Demographicdata,clinicalevaluation,diseaseactivity, diseasedamageanddrugtherapy
Demographicdataincludedgender,ethnicityandageatcSLE
onset.Descriptors and definitions of SLEDAI-2Kwere used
toscorediseaseactivity.14OtherSLEclinicalmanifestations
included: fever (axillary temperature higher than 37.8◦C),
weightloss>2kg,lymphadenopathy(peripherallymphnode
enlargement>1.0cm),hepatomegaly[basedonphysicalexam
withliveredge≥2cmbelowtherightcostalmarginor
imag-ing (ultrasound or computer tomography when available)]
and splenomegaly [based on physical exam with palpable
spleenorimaging(ultrasoundorcomputertomographywhen
available)].15Neuropsychiatriclupusincluded19syndromes
according to ACR classification criteria.16 Antiphospholipid
syndromewas diagnosed accordingto the preliminary
cri-teria for the classification of pediatric antiphospholipid
syndrome.17 High blood pressure was defined as systolic
and/ordiastolicbloodpressures≥95thpercentileforgender,
ageandheighton≥3occasions.18 Acutekidneyinjurywas
determined by sudden increase in serum creatinine above
2mg/dl19 or by modified RIFLE (Risk, Injury, Failure, Loss
ofkidney functionand End-stagekidneydisease)criteria.20
Chronicrenaldiseasewasdefinedasstructuralorfunctional
abnormalitiesofthekidneyfor≥3months(withorwithout
decreasedglomerularfiltrationrate)orglomerularfiltration
rate<60ml/min/1.73m2for≥3months.21
Laboratorial assessment was comprised of
retrospec-tive analysis of erythrocyte sedimentation rate (ESR),
C-reactive protein (CRP), complete blood cell count, serum
urea and creatinine, urinalysis and 24-h urine protein
excretion. Complement levels (CH50, C3 and C4) were
assessed by immunodiffusion, turbidimetric immunoassay
orimmunonephelometry.Antinuclearantibodies(ANA)were
testedbyindirectimmunofluorescence;anti-double-stranded
DNA(anti-dsDNA)byindirectimmunofluorescenceorEnzyme
Linked Immuno Sorbent Assay (ELISA) and anticardiolipin
(aCL)IgGand IgMbyELISAwerecarriedoutateachcenter.
Thecutoffvaluesgivenbythekit manufacturerwereused
todefinenormalorabnormalfindings.Lupusanticoagulant
wasdetectedaccordingtotheguidelinesoftheInternational
SocietyonThrombosisandHemostasis.22
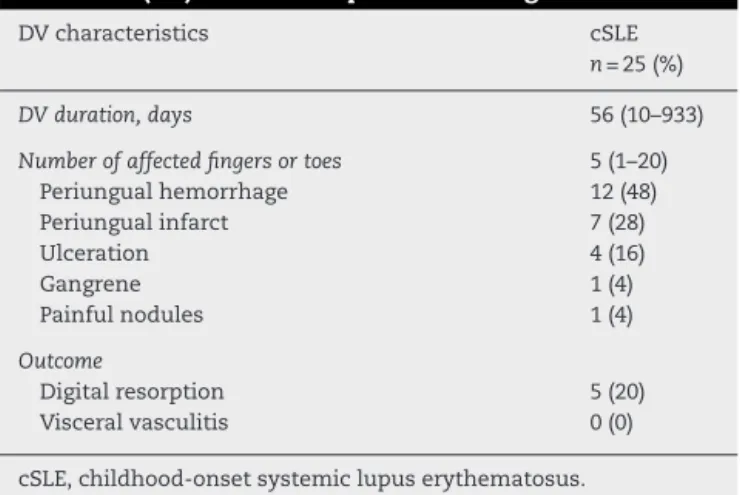
Table1–Clinicalcharacteristicsandoutcomeofdigital vasculitis(DV)in852cSLEpatientsatdiagnosis.
DVcharacteristics cSLE
n=25(%)
DVduration,days 56(10–933)
Numberofaffectedfingersortoes 5(1–20) Periungualhemorrhage 12(48) Periungualinfarct 7(28)
Ulceration 4(16)
Gangrene 1(4)
Painfulnodules 1(4)
Outcome
Digitalresorption 5(20) Visceralvasculitis 0(0)
cSLE,childhood-onsetsystemiclupuserythematosus. Resultsarepresentedasmedian(range)andn(%).
Drug treatment data (prednisone, intravenous methyl-prednisolone,chloroquinediphosphate,hydroxychloroquine sulfate,methotrexate,azathioprine,cyclosporine, mycophe-nolate mofetil,intravenous cyclophosphamide,intravenous immunoglobulin, rituximab and plasmapheresis) were also recorded.
PatientsweredividedintwogroupsatthecSLEdiagnosis fortheassessmentofcSLEmanifestations,laboratoryexams andtreatment:patientswithDVandwithoutDV.
Statisticalanalysis
All statistical analyses were performedwith the Statistical Packageforthe SocialSciences (SPSS),version13.0.Results weregivenasnumbers(percentage)forcategoricalvariables, median (range)or mean±standard deviation (SD)for con-tinuousvariables.Comparisonsbetweencategoricalvariables were assessed by Pearson -square or Fisher’s exact test and continuous variables comparisons were compared by Mann–Whitney testor ttest. Thesignificancelevels ofthe independentvariableweresetat5%(p<0.05).
Results
DVwasobservedin25/852(2.9%)cSLEpatientsatdiagnosis. Periungualhemorrhageonthefingerswasfoundin12(48%) cSLEpatients,periungualinfarctin7(28%),digitalulceration in4(16%),digitalgangrenein1(4%)anddigitalpainfulnodules in1(4%)patient.Themedianofaffectedfingersortoeswas five(1–20).ThefeaturesofDVanditsoutcomein25/852cSLE areshowninTable1.
Further comparisons of demographic data and current
clinicalmanifestationsin852cSLEpatientswithandwithout
DVatdiagnosis areillustratedinTable2.Thefrequencyof
constitutional features (32% vs. 61%, p=0.003), fever (32%
vs. 56%,p=0.020),hepatomegaly(4% vs.23%,p=0.026)and
arterialhypertension(0%vs.25%,p=0.001)weresignificantly
lowerincSLEpatientswithDVcomparedtothosewithoutthis
manifestation.Onthe otherhand,mucocutaneous
involve-ment (100%vs. 79%,p=0.005),rash(80%vs.53%,p=0.008),
Table2–Demographicdataandcurrentclinicalmanifestationsin852childhood-onsetsystemiclupuserythematosus (cSLE)patientsgroupedaccordingtodigitalvasculitis(DV)atthediagnosis.
Variables WithDV(n=25) WithoutDV(n=827) p
Demographicdata
Femalegender,n=852 22/25(88) 710/827(86) 1.000
Caucasian,n=830 8/24(33) 230/806(29) 0.609
AgeatcSLEonset,years,n=852/852 13(4.25–17) 11.8(0.25–17.8) 0.067
Clinicalmanifestations
Constitutionalfeatures,n=843 8/25(32) 501/818(61) 0.003
Fever,n=837 8/25(32) 451/812(56) 0.020
Weightloss>2kg,n=822 7/25(28) 251/797(32) 0.385
Reticuloendothelialsysteminvolvement,n=831 5/25(20) 267/806(33) 0.199
Lymphadenopathy,n=825 4/25(16) 164/800(21) 0.801
Hepatomegaly,n=831 1/25(4) 181/806(23) 0.026
Splenomegaly,n=830 0/25(0) 76/805(9) 0.157
Mucocutaneousinvolvement,n=848 25/25(100) 651/823(79) 0.005
Rash,n=842 20/25(80) 434/817(53) 0.008
Discoidlupus,n=844 4/25(16) 31/819(4) 0.017
Photosensitivity,n=844 19/25(76) 367/819(45) 0.002 Mucosalulcer,n=845 8/25(32) 276/820(34) 0.863
Alopecia,n=843 11/25(25) 251/818(31) 0.156
Otherskinvasculitislesions,n=844 20/25(80) 152/819(19) <0.0001
Musculoskeletalinvolvement,n=846 18/25(72) 561/821(68) 0.697
Myositis,n=843 2/25(8) 32/818(4) 0.267
Arthritis,n=850 17/25(68) 555/825(67) 0.939
Serositis,n=847 5/25(20) 233/822(28) 0.499
Pleuritis,n=846 1/25(4) 148/821(18) 0.104
Pericarditis,n=846 5/25(20) 163/821(20) 1.000
Neuropsychiatricinvolvement,n=847 2/25(8) 202/822(25) 0.059
Peripheralnervoussysteminvolvement,n=847 0/25(0) 7/818(1) 1.000 Centralnervoussysteminvolvement,n=843 2/25(8) 198/822(24) 0.090
Nephritis,n=836 8/25(32) 406/811(50) 0.075
Hematuria,n=825 9/25(36) 358/800(45) 0.386
Pyuria,n=821 4/25(16) 269/796(34) 0.083
Urinarycast,n=822 3/25(12) 171/797(22) 0.326
Proteinuria>0.5g/day,n=804 7/25(28) 368/779(47) 0.058
Anti-phospholipidsyndrome,n=785 0/25(0) 15/760(2) 1.000
Ocularinvolvement,n=841 1/25(4) 13/816(2) 0.347
Other
Arterialhypertension,n=840 0/25(0) 202/815(25) 0.001 Acuterenalfailure,n=839 1/25(4) 98/814(12) 0.346 Chronicrenalfailure,n=835 0/25(0) 18/810(2) 1.000
Resultsarepresentedinn(%)andmedian(range).
45%,p=0.002)andotherskinvasculitislesions(80%vs.19%,
p<0.0001)weresignificantlyhigherincSLEpatientswithDV comparedtothosewithoutthiscutaneousinvolvement.A ten-dencyoflowerfrequencyofneuropsychiatric(p=0.059)and renalinvolvement(p=0.075)wasobservedinpatientswithDV (Table2).NoneofthepatientswithDVhadantiphospholipid
syndromeorthromboticthrombocytopenicpurpura.
Diseaseactivityandlaboratorytestsof852cSLEpatients
areshowninTable3.ThemedianofSLEDAI-2Kincludingthe
DVscoreitem[20(8–36)vs.14(0–58),p=0.014]wassignificantly
higherinDVpatientscomparedtopatientswithoutthis
com-plication.Ontheother hand,whencalculatingthe median
ofSLEDAI-2KexcludingDVdescriptor[10(0–28)vs.14(0–58),
p=0.004],itwaslowerinthegroupwithDV,scoredmainlyby
mucocutaneousinvolvement[rash(80%)andmucosalulcers
(32%)].Inspiteofthat,allpatientswithDVhadSLEDAI-2K>8.
Thelaboratorytestscomparisonwassimilarinbothgroups
(p>0.05,Table3).
TherapyincSLEpatientswithandwithoutDVatthetime
ofdiagnosisisshowninTable4.Thefrequencyof
cyclophos-phamideuse(0%vs.18%,p=0.014)wassignificantlylowerin
patientswithDVcomparedtothosewithoutthis
manifesta-tion.Frequencyofothermedicationsusewassimilarinboth
groups (p>0.05,Table 4). NocSLEpatientwas treatedwith
intravenousimmunoglobulin,rituximaborplasmapheresisat
diagnosis.
Regarding outcome,digital resorption was evidenced in
5/25 (20%).Visceralvasculitis ordeathwasnotobservedin
cSLEpatientswithDV,withnostatisticalsignificance
com-paredtothepatientswithnoDV.
Discussion
OurlargemulticentercohortwasthefirstcharacterizingDVas
oneoftherareinitialmanifestationsofcSLEpatients,mainly
Table3–Currentdiseaseactivityandlaboratorytestsin852childhood-onsetsystemiclupuserythematosus(cSLE) patientsgroupedaccordingtodigitalvasculitis(DV)atdiagnosis.
Variables WithDV(n=25) WithoutDV(n=827) p
Currentdiseaseactivity/damagescores
SLEDAI-2KwithDVscore,n=789/852 20(8–36) 14(0–58) 0.014 SLEDAI-2KwithoutDVscore,n=789/852 10(0–28) 14(0–58) 0.004
SLEDAI-2K≥8,n=789/852 25(100) 743(90) 0.062
Laboratorytests
ESRmm/1st/hour,n=717/852 44(10–130) 50(1–160) 0.601
CRPmg/dL,n=454/852 1.85(0–47) 3(0–413) 0.531
Autoimmunehemolyticanemia,n=830 3/25(12) 170/805(21) 0.328 Leucopenia<4000mm−3,n=836 5/25(20) 222/811(27) 0.500 Lymphopenia<1500mm−3,n=834 9/25(36) 349/809(43) 0.157 Thrombocytopenia,<100,000mm−3,n=834 1/25(4) 128/809(16) 0.540 LowC3,C4and/orCH50,n=727 21/23(91) 511/704(73) 0.054 Anti-dsDNAantibody,n=801 15/25(60) 542/776(70) 0.292 Lupusanticoagulant,n=415 1/18(6) 64/397(16) 0.330 AnticardiolipinIgMantibody,n=498 1/19(5) 110/479(23) 0.090 AnticardiolipinIgGantibody,n=496 3/18(17) 130/478(27) 0.270
SLEDAI-2K,SystemicLupusErythematosusDiseaseActivityIndex2000;ESR,erythrocytesedimentationrate;CRP,C-reactiveprotein. Resultsarepresentedinn(%)andmedian(range).
Table4–Therapyin852childhood-onsetsystemiclupuserythematosus(cSLE)patientsgroupedaccordingtodigital vasculitis(DV)atdiagnosis.
Variables WithDV(n=25) WithoutDV(n=827) p
Nonsteroidalanti-inflammatory,n=836 2/25(8) 115/811(14) 0.380
Glucocorticosteroids
Prednisone,n=836 24/25(96) 757/811(93) 1.000
Currentdose,mg/day,n=762/852 40(10–75) 40(3–180) 0.421 mg/kg/day,n=728/852 1.0(0.2–2) 1.0(0.1–4) 0.438 Intravenousmethylprednisolone,n=821 10/25(40) 348/796(44) 0.712
Antimalarialdrugs,n=838 18/25(72) 444/813(55) 0.085
Immunosuppressiveagents
Azathioprine,n=839 6/25(24) 100/814(12) 0.082
Cyclosporine,n=839 0/25(0) 8/814(1) 1.000
Methotrexate,n=840 3/25(12) 33/815(4) 0.087
Mycophenolatemofetil,n=838 1/25(4) 8/813(1) 0.240
Cyclophosphamide,n=841 0/25(0) 144/816(18) 0.014
Others
Intravenousimmunoglobulin,n=845 0/25(0) 28/820(3) 1.000
Rituximab,n=843 0/25(0) 0/818(0) –
Plasmapheresis,n=841 0/25(0) 11/816(1) 1.000
Resultsarepresentedinn(%).
TheadvantageofincludingalargecSLEpopulationselected intertiaryreferralcentersallowedabetterevaluationofthis rarevasculiticmanifestation.Theuseofastandardized com-bineddatabase,withproperDVdefinition,minimizedpossible bias.However,themainlimitationofthisstudywasthe ret-rospectivedesignand possiblemissing data, aswell asno biopsyor angiographic evidenceofvasculitis inany ofour patients.Itwasnotpossibletoexaminenailfoldcapillaroscopy becauseitwasnotaroutineprocedureinallparticipant Pedi-atricRheumatologycenters.Thisexamcouldbeusefulasa toolfordiseaseactivityassessmentrelatedtosmallvessels involvementincaseswithDV.23,24
VascularskininjuryisanimportantcharacteristicofSLE
andaffectsthemajorityofpatientsduringthewholedisease
courseanditwasreportedinassociationwithlupusflaresor
thrombosis.8–10 Weconfirmedthepossibleassociationwith
activediseaseand lessprobableassociationwith
antiphos-pholipid syndromedue totheabsence ofantiphospholipid
antibodiesinDVcases.Ofnote,SLEDAI-2Kevaluationrevealed
a predominanceofmucocutaneous involvementandlower
frequencyofmajororganinvolvements(neuropsychiatricand
renal)reinforcingtheconceptthatDVisassociatedwithmild
systemic disease activity andmoreactive skindisease.DV
descriptorhasweightof8andconsequentlycontributeswith
highvaluesofSLEDAI-2Kscore,despiteofthemilddisease
thatthismanifestationrepresentedinourpatients.9
Despite the factthat skinvasculitis isacommon lupus
clin-icalDV wasrarelyreportedinadults11,25 and cSLE.1,8,9 Ina
cross-sectional study with 168aSLE patients, DV appeared
in16%ofthepatientsassociatedwithconstitutional
symp-toms,mucocutaneousandhematologicalmanifestations.7In
anotherstudyreporting670aSLEcases,11%presenteddigits
ulcerationand/orischemiclesions.25 Weobservedfrom our
resultsthatalthoughthefrequencyofDVatcSLEdiagnosisis
verylow,itisinfactassociatedwithpermanentdamagein1/5
ofthepatients.
DVwasnotassociatedwithany lupusspecificantibody.
Onlyafewpatients hadantiphospholipidantibodies,
char-acterizing a distinct profile from those with more severe
organinvolvement.26–28Althoughitisnotpossibletoexclude
antiphospholipid syndrome in these patients, the absence
ofclinical criteria makes this diagnosis very unlikely. The
onlyclinicalfeaturewasthedigitalthromboticvascular
dam-age that may have had a similar clinical aspect to lupus
vasculitis.4–7 Further studies regardingthis association are
necessary.
ThemajorityofSLEpatientswithsmallvessellesionshad
clinicalDVcharacterizedbyerythematouspunctuatelesions
onthefingers,7asobservedinourstudy.Thisfeatureis
dif-ferentfromthosecSLEpatientswithvisceralmediumvessel
vasculitisassociatedwithincreasedmorbidityandmortality
duetoinvolvementofcerebrovascular,gastrointestinal,renal,
cardiovascularandpulmonaryinvolvements.29–32Intravenous
cyclophosphamidetreatment was less frequentreinforcing
theconceptofmildersystemicactivityofthecases.
Further-more,concomitant visceraland cutaneousvasculitis israre
inaSLE(2%),33emphasizingtheimportanceofdistinguishing
betweenthesetwosubtypesofvasculitis.
Inconclusion,ourlargemulticenterstudyidentified
clini-calDVasarareinitialmanifestationofactivecSLEassociated
withmildmultisystemicdiseaseinspiteofaccrueddamage
withdigitalresorptioninsomeofthesepatients.
Funding
This study was supported by grants from Conselho
Nacional de Desenvolvimento Científico e Tecnológico
(CNPq303422/2015-7toClovis ArturSilva,301805/2013-0 to
RosaMariaRodriguesPereira,305068/2014-8toEloisaBonfá,
301479/2015 to Claudia Saad-Magalhães and 303752/2015-7
to Maria Teresa Terreri), Federico Foundation (to Clovis
ArturSilva,RosaMariaRodriguesPereira andEloisa Bonfá)
andbyNúcleodeApoio àPesquisa“Saúdeda Crianc¸aedo
Adolescente”ofUSP(NAP-CriAd)toClovisArturSilva.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
OurgratitudetoUlyssesDoria-Filhoforthestatistical
analy-sis.TheauthorsthankthefollowingPediatricRheumatology
Divisions and colleagues forincluding their patients:
Pedi-atricRheumatologyUnit,FMUSP(AdrianaAlmeidadeJesus,
AdrianaMalufEliasSallum,CristinaMiukiAbeJacob,Gabriela
Blay,GabrielaNunesLeal,GabriellaErlacherLubedeAlmeida,
Heloisa Helenade SouzaMarques, JoãoDomingosMontoni
daSilva,JoaquimCarlosRodrigues,JulianaCaíresdeOliveira
AchiliFerreira, LailaPinto Coelho,LucianadosSantos
Hen-riques,MariaHelenaVaisbich,NadiaEmiAikawa,LuciaMaria
Arruda Campos, Victor Marques, Werther Brunow de
Car-valho);PediatricRheumatologyUnit,UNIFESP(AlineNicácio
Alencar,DanielaGerentPetryPiotto,GiampaoloFaquin,Gleice
ClementeSouzaRusso,LuisEduardoCoelhoAndrade,Maria
OdeteEstevesHilário,MelissaMaritiFraga,OctavioAugusto
BedinPeracchi);DivisionofRheumatology,FMUSP(JulianeA.
Paupitz,GlauceLeão Lima);UNESP (PriscilaR.Aoki, Juliana
deOliveiraSato,SilvanaPaulaCardin,TacianaAlbuquerque
PedrosaFernandes);IrmandadedaSantaCasade
Misericór-diadeSãoPaulo(AndressaGuariento,EuniceOkuda,Maria
Carolina dosSantos,Natali WenigerSpellingGormenzano);
StateUniversityofCampinas(MaraísaCenteville,Renata
Bar-bosa, SimoneAppenzeller);RibeirãoPreto MedicalSchool–
University ofSão Paulo (FranciscoHugo Gomes,Gecilmara
SalviattoPileggi,PaolaPontesPinheiro,VirginiaPaesLeme
Fer-riani);HospitalInfantilDarcyVargas(JonatasLibório,Luciana
TudechPedroPaulo);HospitalMunicipalInfantilMeninoJesus
(SimoneLotufo,TâniaCarolineMonteirodeCastro)and
Pon-tificalCatholicUniversityofSorocaba(ValériaC.Ramos).
r
e
f
e
r
e
n
c
e
s
1.BenselerSM,SilvermanED.Systemiclupuserythematosus. PediatrClinNorthAm.2005;52:443–67.
2.MinaR,BrunnerHI.Pediatriclupus–aretheredifferencesin presentation,genetics,responsetotherapy,anddamage accrualcomparedwithadultlupus?RheumDisClinNorth Am.2010;36:53–80.
3.TarrT,DérfalviB,GyöriN,SzántóA,SiminszkyZ,MalikA, etal.Similaritiesanddifferencesbetweenpediatricandadult patientswithsystemiclupuserythematosus.Lupus.
2015;24:796–803.
4.DanningCL,IlleiGG,BoumpasDT.Vasculitisassociatedwith primaryrheumatologicdiseases.CurrOpinRheumatol. 1998;10:377–86.
5.D’CruzD.Vasculitisinsystemiclupuserythematosus.Lupus. 1998;7:217–24.
6.Ramos-CasalsM,NardiN,LagruttaM,Brito-ZerónP,BovéA, DelgadoG,etal.Vasculitisinsystemiclupuserythematosus: prevalenceandclinicalcharacteristicsin670patients. Medicine(Baltimore).2006;85:950–1004.
7.GomesC,CarvalhoJF,BorbaEF,BorgesCTL,VendraminiMB, BuenoC,etal.Digitalvasculitisinsystemiclupus
erythematosus:aminormanifestationofdiseaseactivity. Lupus.2009;18:990–3.
8.ChiewchengcholD,MurphyR,EdwardsSW,BeresfordMW. Mucocutaneousmanifestationsinjuvenile-onsetsystemic lupuserythematosus:areviewofliterature.Pediatr RheumatolOnlineJ.2015;13:1.
9.BouazizJD,BareteS,LePelletierF,AmouraZ,PietteJC, FrancèsC.Cutaneouslesionsofthedigitsinsystemiclupus erythematosus:50cases.Lupus.2006;16:163–7.
10.CalamiaKT,BalanovaM.Vasculitisinsystemiclupus erythematosus.ClinDermatol.2003;22:148–56.
nationalcohortofjuvenile-onsetsystemiclupus erythematosuspatients.Rheumatology.2014;53:1504–12.
12.HochbergMC.UpdatingtheAmericanCollegeof
Rheumatologyrevisedcriteriafortheclassificationofsystemic lupuserythematosus.ArthritisRheum.1997;40:17–25.
13.SilvaCA,AvcinT,BrunnerHI.Taxonomyforsystemiclupus erythematosuswithonsetbeforeadulthood.ArthritisCare Res(Hoboken).2012;64:1787–93.
14.GladmanDD,Iba ˜nezD,UrowitzMB.Systemiclupus erythematosusdiseaseactivityindex2000.JRheumatol. 2002;29:288–91.
15.GuarientoA,SilvaMF,TassetanoPS,RochaSM,CamposLM, ValenteM,etal.Liverandspleenbiometricsin
childhood-onsetsystemiclupuserythematosuspatients.Rev BrasReumatol.2015;55:346–51.
16.AmericanCollegeofRheumatologyAdHocCommitteeon NeuropsychiatricLupusSyndromes.TheAmericanCollegeof Rheumatologynomenclatureandcasedefinitionsfor neuropsychiatriclupussyndromes.ArthritisRheum. 2009;2:599–608.
17.AvcinT,CimazR,RozmanB.ThePed-APSRegistry:the antiphospholipidsyndromeinchildhood.Lupus. 2009;18:894–9.
18.NationalHighBloodPressureEducationProgramWorking GrouponHighBloodPressureinChildren,Adolescents.The fourthreportonthediagnosis,evaluation,andtreatmentof highbloodpressureinchildrenandadolescents.Pediatrics. 2004;114:555–76.
19.ChanJC,WilliamsDM,RothKS.Kidneyfailureininfantsand children.PediatrRev.2002;23:47–60.
20.Akcan-ArikanA,ZappitelliM,LoftisLL,WashburnKK, JeffersonLS,GoldsteinSL.ModifiedRIFLEcriteriaincriticallyill childrenwithacutekidneyinjury.KidneyInt.2007;71:1028–35.
21.NationalKidneyFoundation.K/DOQIclinicalpractice guidelinesforchronickidneydisease:evaluation, classification,andstratification.AmJKidneyDis.2002;39. S1–266.
22.BrandtJT,TriplettDA,AlvingB,ScharrerI.Criteriaforthe diagnosisoflupusanticoagulants:anupdate.Onbehalfofthe SubcommitteeonLupusAnticoagulant/Antiphospholipid AntibodyoftheScientificandStandardisationCommitteeof theISTH.ThrombHaemost.1995;74:1185–90.
23.PiottoDG,LenCA,HilárioMO,TerreriMT.Nailfold capillaroscopyinchildrenandadolescentswithrheumatic diseases.RevBrasReumatol.2012;52:722–32.
24.PetryDG,TerreriMT,LenCA,HilárioMO.Nailfold
capillaroscopyinchildrenandadolescentswithrheumatic diseases.ActaReumatolPort.2008;33:395–400.
25.Ramos-CasalsM,NardiN,LagruttaM,Brito-ZerónP,BovéA, DelgadoG,etal.Vasculitisinsystemiclupuserythematosus. Medicine(Baltimore).2006;85:95–104.
26.AikawaNE,JesusAA,LiphausBL,SilvaCA,SampaioMC, SallumAM.Organ-specificautoantibodiesandautoimmune diseasesinjuvenilesystemiclupuserythematosusand juveniledermatomyositispatients.ClinExpRheumatol. 2010;30:126–31.
27.HoffmanIE,LauwerysBR,DeKeyserF,HuizingaTW,Isenberg D,CebecauerL,etal.Juvenile-onsetsystemiclupus
erythematosus:differentclinicalandserologicalpatternthan adult-onsetsystemiclupuserythematosus.AnnRheumDis. 2009;68:412–5.
28.LivingstonB,BonnerA,PopeJ.Differencesinautoantibody profilesanddiseaseactivityanddamagescoresbetween childhoodandadult-onsetsystemiclupuserythematosus:a meta-analysis.SeminArthritisRheum.2012;42:271–80.
29.DinizJC,AlmeidaRT,AikawaNE,SallumAM,SakanePT,Silva CA.Kawasakidiseaseandjuvenilesystemiclupus
erythematosus.Lupus.2012;21:89–92.
30.Albuquerque-NettoAF,CavalcanteEG,SallumAM,Aikawa NE,TannuriU,SilvaCA.Mesentericvasculitisinajuvenile systemiclupuserythematosuspatient.RevBrasReumatol. 2013;53:219–22.
31.MarquesVL,GuarientoA,SimõesMS,BlayG,LotitoAP,Silva CA.Childhood-onsetsystemicpolyarteritisnodosaand systemiclupuserythematosus:anoverlapsyndrome.Rev BrasReumatol.2016;56:551–3.
32.AraujoDB,BorbaEF,SilvaCA,CamposLM,PereiraRM,Bonfa E,etal.Alveolarhemorrhage:distinctfeaturesofjuvenileand adultonsetsystemiclupuserythematosus.Lupus.
2012;21:872–7.