w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Risk
factors
for
cardiovascular
disease
in
rheumatoid
arthritis
patients
from
Mato
Grosso
do
Sul
Ramão
Souza
de
Deus
Junior
a,∗,
Andressa
Leite
Ferraz
b,
Silvia
Aparecida
Oesterreich
a,c,
Wanderlei
Onofre
Schmitz
b,d,
Marcia
Midori
Shinzato
a,b,eaHealthSciencesSchool,UniversidadeFederaldaGrandeDourados(UFGD),Dourados,MS,Brazil
bUniversityHospitalofDourados,UniversidadeFederaldaGrandeDourados,Dourados,MS,Brazil
cUniversidaddeLeón,Leon,Spain
dUniversidadeEstadualdeLondrina,Londrina,PR,Brazil
eUniversidadedeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received24October2013 Accepted2February2015 Availableonline3September2015
Keywords:
Rheumatoidarthritis Autoantibodies Comorbidities
a
b
s
t
r
a
c
t
Objective:ToidentifyriskfactorsforcardiovasculardiseaseinpatientswithRheumatoid
Arthritis(RA).
Materialandmethods:Adescriptivecross-sectionalstudywith71patientswithestablished
RA.Theinstrumentsusedwere:DAS-28,HAQandSF-36,andthefollowingparameters weredetermined:theerythrocytesedimentationrate,capillarybloodglucose;total choles-terol(TC)anditsfractions,thyroidhormones,antinuclearantibodies(ANA),rheumatoid factor(RF)andantibodiesagainstcitrullinatedproteins(ACPAs).Patientswereclassified intogroupsHAQ≤1(milddysfunction)andHAQ>1(moderateandseveredysfunction)and, accordingtotheHAQscores,ingroupstreatedwithcorticosteroids(CS)andwithoutCS.
Results:9patientsweremaleand62femalewithmeanageanddurationofdiseaseof53.45
(±10.7)and9.9(±8.6),respectively.RFwaspositivein52(76%),ACPAsin54(76.1%)andANA in12(16.9%). Thirty-sixpatients(50.7%)hadsystemichypertension,9(12.68%)diabetes mellitus,16(22.5%)hypothyroidism,33(46.5%)dyslipidemiaand8(11.27%)weresmokers. TheresultsofTC>240werefoundin53.8%forgroupHAQ>1(26)andin24.4%forgroup HAQ≤1(45)(p=0.020).Thesegroupsdidnotdifferastopresenceofcomorbiditiesordrug treatment.Triglyceridelevels>200forthegroupwithCS(42.4%)versuswithoutCS(18.42%) weresignificant(p=0.025).
Conclusion: AnassociationofincreasedTCandtriglycerideswithresultsofHAQ≤1and
withCSusewasnoted,reinforcingtheimportanceofscreeningriskfactorsassociatedwith cardiovasculardiseaseinRA.
©2015ElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthor.
E-mail:ramaojunior@ufgd.edu.br(R.S.d.DeusJunior). http://dx.doi.org/10.1016/j.rbre.2015.07.012
Caracterizac¸ão
de
pacientes
com
artrite
reumatoide
quanto
a
fatores
de
risco
para
doenc¸as
vasculares
cardíacas
no
Mato
Grosso
do
Sul
Palavras-chave:
Artritereumatoide Autoanticorpos Comorbidades
r
e
s
u
m
o
Objetivo: CaracterizarpacientescomArtriteReumatoide(AR)quantoàpresenc¸adefatores
deriscoparadoenc¸ascardiovasculares.
Materialemétodos: Estudo transversaldescritivocom71 pacientesdiagnosticadoscom
ARdefinida.Foramutilizadososinstrumentos:DAS-28,HAQeSF-36edeterminadosos parâmetros:velocidadedehemossedimentac¸ão,glicemiacapilar;colesteroltotal(CT)esuas frac¸ões,hormôniostiroidianos,anticorposantinúcleo(ANA),fatorreumatoide(FR)e anti-corposcontraproteínascitrulinadas(ACPAs).Ospacientesforamclassificadosemgrupos HAQ≤1(disfunc¸ãoleve)eHAQ>1(disfunc¸ãomoderadaegrave)e,segundoosescoresdo HAQ,emgrupotratadocomcorticosteroides(CE)esemCE.
Resultados: Proporc¸ãode9homenspara62mulherescomidadeetempomédiodedoenc¸a
de53,45(±10,7)e9,9(±8,6),respectivamente.OFRfoipositivoem52(76%),osACPAsem 54(76,1%)eANAem12(16,9%).Trintaeseispacientes(50,7%)apresentaramhipertensão arterialsistêmica,9(12,68%)Diabetesmellitus,16(22,5%)hipotireoidismo,33(46,5%) dislipi-demiae8(11,27%)tabagismo.OgrupoHAQ>1(26)apresentouresultadosdeCT>240(53,8%) eogrupocomHAQ≤1(45)(24,4%)(p=0,020).Osgruposnãodiferiramquantoàpresenc¸a decomorbidadesoutratamentofarmacológico.Osníveisdetriglicérides>200(42,4%)entre osgruposemusodeCEesemuso(18,42%)foisignificativo(p=0,025).
Conclusão: Houveassociac¸ãodoaumentoCTetriglicerídeoscomresultadosdeHAQ≤1e
comusodeCE,reforc¸andoaimportânciadorastreamentodefatoresderiscoassociadosàs doenc¸ascardiovascularesnaAR.
©2015ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
RheumatoidArthritis(RA)isachronic,inflammatory,
autoim-mune disease, with unknown etiology, associated with
progressivejointdysfunction,whoseconsequenceforpatients isfunctionallimitationfortheirdailyandprofessional activi-ties.Furthermore,RAcanleadtosystemiccomplicationsand earlymortality.1
ThepharmacologicalresearchinvolvingRAhaschanged
considerably, and the current treatment recommends the
introduction ofanearly and aggressivetherapeutic action, guidedbydiseaseactivityindexes.However,whathasbeen observedisthatsomepatientsdonotpresenteffectiveresults toavailabletreatments.2
Inaddition,higherseverityandearlymortalityfrom car-diovasculardiseaseinthesepatients,whencomparedtothe healthypopulation,3remainsachallengeforphysicianswho aremonitoringthesepatients.
Currentpublishedliteratureadvocatestheidentificationof subgroupsofpatientswithdifferentprognosisand therapeu-ticresponses.4Thus,thisstudyaimedtocharacterizepatients diagnosedwithRAintermsofriskfactorsforcardiovascular disease,identifyingpossiblemarkersthatshowthosepatients withworseprognosis,treatedornottreatedwith corticoste-roids,suchas:IgMclassrheumatoidfactor antibodies(RF), antibodiesagainstcitrullinatedproteins(ACPAs),and antin-uclearantibodies(ANA);presenceofcomorbidities:systemic hypertension(SH),diabetesmellitus(DM),hypo-or hyperthy-roidism and dyslipidemias,and to correlatethese markers
withclinicalactivityofdisease,functionalstatusandquality oflife.
Material
and
methods
Thisisadescriptivecross-sectionalstudythatevaluated con-secutive patientsfromJuly2012toFebruary 2013,attended at the RheumatoidArthritis OutpatientClinic, Department of Rheumatology, University Hospital (UH) of Universidade
Federal de Grande Dourados (UFGD). The study included
71 patients ofboth genderspreviouslydiagnosed withRA,
whometthe1987AmericanCollegeofRheumatology
crite-riaforRA.5Patientswhoagreedtoparticipateinthis study signedaninformedconsentform.Theprojectwasapproved
bythe ResearchEthics CommitteeofUFGD, protocol
num-ber14136013.0.0000.5160.Patientswereclinicallyassessedby rheumatologistswhocalculateddiseaseactivitywiththe Dis-easeActivityScorefor28joints(DAS-28),usingaslaboratory parametertheerythrocytesedimentationrate.6
alsothoseshowingchangesinbloodglucoseatthe diagno-sis,laterconfirmedaccordingtoBrazilianSocietyofDiabetes guidelines.8
Intestsforplasmalipids,weconsideredasdyslipidemic thosepatientsinuseofmedicationforthisconditionand/or withdietarymeasuresrecommendedforthedisease,aswell asthosewhohadtheirresultsfordyslipidemiaconfirmed dur-ingfollow-upinatleastonemorelaboratoryanalysis.
FunctionalstatuswasassessedusingtheHealth Assess-mentQuestionnaire (HAQ)(simplified) validatedand trans-latedintoPortuguese.9Theparameterswerecorrelatedwith HAQresultsassociatedwithuseornotuseofcorticosteroids; andpatientswereclassifiedaccordingtothescoreingroups HAQ≤1(milddysfunction)andHAQ>1(moderateandsevere
dysfunction), considering the reduced number of patients
withseveredysfunctioninthisstudy.
QualityoflifewasanalyzedbytheinstrumentTheShort Form(36)HealthSurvey(SF-36)validatedandtranslatedinto Portuguese.10
Wecollected15mLofeachpatient’sbloodonclinical eval-uationday,forperforminganerythrocytesedimentationrate (ESR)testbyWestergreenmethod(mm/1sthour)inthesame dayofcollection.
For determining blood glucose, a drop of blood was
depositedinthebloodglucoseteststripmeter(G-TECHmodel Free1).
To test anti-nuclear antibodies (ANA), HEp-2 cells were
used (EUROIMMUN, Germany) and analyzed by indirect
immunofluorescenceaccordingtotheprotocolsuggestedby themanufacturer.
The enzyme-linked immunosorbent assay (ELISA) was
usedtoidentifythepresenceofanti-cycliccitrullinated pep-tide(Anti-CCP-3)(INOVA),rheumatoidfactor(RF)(ORGENTEC), andanti-mutatedcitrullinatedvimentin(Anti-MCV) (ORGEN-TEC).Triiodothyronine(T3andfreeT3)andthyroxine(T4and
freeT4)hormonesweremeasuredby
electrochemilumines-cencewiththeuseofaCobasE411(ROCHELTD.)analyzerand usingkitssuppliedbythemanufacturer.
Total cholesterol and its fractions were performed in a CobasIntegraE400plus(ROCHELtd.)analyzer,alsousingkits suppliedbythemanufacturer.
Thepresenceofrheumatoidfactorwasevaluatedbylatex agglutination,butalsobyWaaler–Rosetest,forIgMisotypes, accordingtomanufacturer’sprotocols.
Statisticalanalysis wasperformed withSPSS(Statistical PackageforSocialSciences)version20.0.Tocharacterizethe sample,weuseddescriptivestatistics;anddataarepresented asmean (X)±standarddeviation(SD)forquantitative vari-ables,andabsolute(f)andrelative(%)frequenciesfor qualita-tivevariables.Statisticalinferencewasusedfortheremaining analyzes.Tocomparecontinuousvariableswithnormal distri-bution,Student’st-testwasperformed;otherwiseMann Whit-neytestwasused.Categoricalvariableswerecomparedusing Fisherexacttest.Thesignificancelevelwassetatp<0.05.
Results
Seventy-onepatientsofbothgenders,previouslydiagnosed withRA,were evaluated;ofthese,62 (87.32%)were female
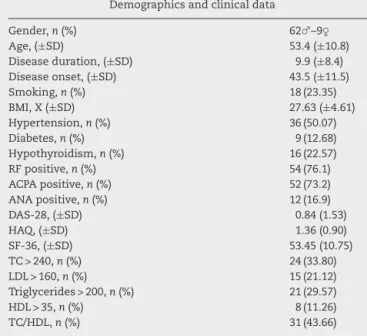
Table1–Demographicsandclinicaldataofpatients withRA.
Demographicsandclinicaldata
Gender,n(%) 62♂–9♀
Age,(±SD) 53.4(±10.8)
Diseaseduration,(±SD) 9.9(±8.4)
Diseaseonset,(±SD) 43.5(±11.5)
Smoking,n(%) 18(23.35)
BMI,X(±SD) 27.63(±4.61)
Hypertension,n(%) 36(50.07)
Diabetes,n(%) 9(12.68)
Hypothyroidism,n(%) 16(22.57)
RFpositive,n(%) 54(76.1)
ACPApositive,n(%) 52(73.2)
ANApositive,n(%) 12(16.9)
DAS-28,(±SD) 0.84(1.53)
HAQ,(±SD) 1.36(0.90)
SF-36,(±SD) 53.45(10.75)
TC>240,n(%) 24(33.80)
LDL>160,n(%) 15(21.12)
Triglycerides>200,n(%) 21(29.57)
HDL>35,n(%) 8(11.26)
TC/HDL,n(%) 31(43.66)
TC, total cholesterol; LDL, low-density lipoprotein; HDL, high-densitylipoprotein.
and 9(12.68%) weremale, anapproximateratio of7:1.The meanageofpatientswas53.4(±10.8)years.Themean dis-easedurationwas9.9(±8.4)years,withamedianof7years, rangingfrom1to42years.Themeanfordiseaseonsetwas 43.5(±11.5)years,withamedianof43years,rangingfrom17 to73yearsold(moredemographicsdatainTable1).
Ten (14.08%) of 71 patients were smokers, while eight
(11.27%) of71 wereformer smokers,totaling18/71 (25.35%) patientsthathadhadcontactwithtobacco.Serafrom15of thesepatientswerepositiveforanti-citrullinatedprotein anti-bodies(ACPAs).Ofthethreenegativeserafortheseantibodies,
onecamefromaformersmokerandtwofromcurrent
smok-ers.
The mean BMI was 27.63±4.61. About 1/3 of patients
(30.98%)hadanadequateweight/heightrelationintheperiod ofdatacollection.Theothersweredistributedintooverweight (28/71,40%)orobese(21/71,29.58%)category.
Asforsystemichypertension(SH),35/71(49.29%)patients hadthisdiseasediagnosedandwereusingantihypertensive medication.Duringthescreeningtests,32(44.44%)patients presentedwithelevatedbloodpressure.Ofthese32patients, twohadnopreviousdiagnosisofhypertension.SHwas con-firmedinanotherpatientduringtheimplementationperiod ofthestudy,totaling36/71(50.7%)patientswithadiagnosisof hypertension.
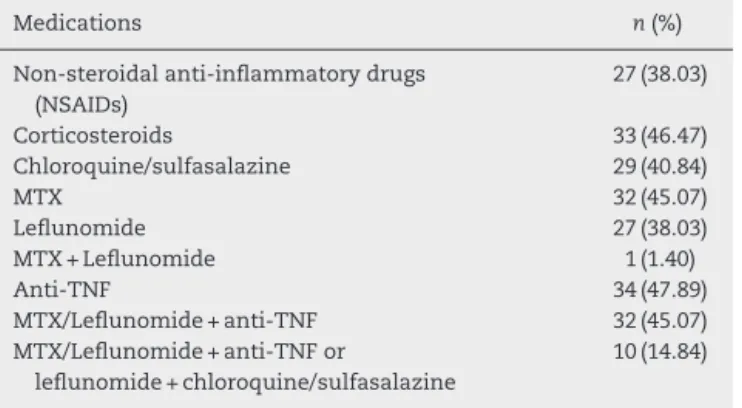
Table2–MedicationsusedinpatientswithRA(n=71).
Medications n(%)
Non-steroidalanti-inflammatorydrugs (NSAIDs)
27(38.03)
Corticosteroids 33(46.47)
Chloroquine/sulfasalazine 29(40.84)
MTX 32(45.07)
Leflunomide 27(38.03)
MTX+Leflunomide 1(1.40)
Anti-TNF 34(47.89)
MTX/Leflunomide+anti-TNF 32(45.07)
MTX/Leflunomide+anti-TNFor
leflunomide+chloroquine/sulfasalazine
10(14.84)
MTX,metotrexate;Anti-TNF,anti-tumornecrosisfactor.
Asforthyroiddisease,13/71(18.30%)wereonthyroid
hor-mone replacement therapy, while 2/71 (2.81%) were being
treated for hyperthyroidism. However, according to results oflaboratorytests,fourpatientsshowedserologicalchanges consistentwithhypothyroidismandonlyoneofthesepatients hadbeenalreadyintreatment,totaling16/71(22.53%)patients
withhypothyroidism.
Seropositivitywascharacterizedasfollows:37/71(52.1%) patientswerepositiveforrheumatoidfactor(RF)byELISA,and 9/71(12.67%)werepositiveonlyforRF.Usingthelatexmethod, positivitywasofonly28/71(39.4%)and17ofthesepatients werealsopositivebyWaaler–Rosemethod.Thepositivityfor
RF wasof 54/71(76.1%), and those patientswho had their
resultsconfirmedbythesamemethod,orwhowerepositive bytwodifferentmethods,wereregardedaspositivecases.
Astoanti-cyclicCitrullinatedPeptide(Anti-CCP)byElisa, 36/71(50.70%)patientswerepositive,and3/71(4.22%)were positive onlyforanti-CCP. As toanti-mutated citrullinated vimentin(anti-MCV)byElisa,48/71(67.60%)patientswere pos-itive, with 11/71(15.49%) positive only foranti-MCV.Thus, 52/71(73.2%)werepositiveforanti-citrullinatedprotein anti-bodies(ACPAs).
PositivityforRFandACPAwasdiagnosedin34/71(47.9%) ofsera.
Serological analysis for antinuclear antibodies (ANA)
resultedin12/71(16.90%)positiveresults,andnopatientwas positiveexclusivelyfortheseantibodies.
Regarding the positivity association for autoantibodies, 7/71(9.9%)patientswerepositiveforallanalyzedantibodies.
ThesamenumberwasnegativeforRFandACPAs.
As for prescription drugs for treatment of RA, Table 2
shows that 27/71 (38.03%) and 33/71 (46.47%) patients had
nonsteroidal anti-inflammatory drugs and corticosteroids
prescribed, respectively. Leflunomide was taken by 27/71
(38.03%) and methotrexate(MTX) by32/71(45.07%); and in 1/71(1.40%)bothmedicationswereused.34/71(47.89)patients hadprescriptionforbiologicals(anti-TNFblockers),and32/34 (94.11%)wereassociatedwithleflunomideorMTX.
Regardingdyslipidemia,6/71(8.45%)ofpatientshadbeen previouslydiagnosed,andfourweretakingmedication(two treatedwithsimvastatin,onewithatorvastatinandonewith benzafibrate) and two other were in dietary therapy. Only 1/6 (16.7%) had normal lipid levels. However, according to screeningtests,33/71(46.5%)hadsometypeofdyslipidemia
Table3–Associationofclinicalandlaboratory parameterswithHAQ.
HAQ≤ 1(45) HAQ>1(26) p
Age,(±SD) 52.91± 10.62 54.38± 11.31 0.47 Diseaseduration,(±SD) 9.76± 7.32 10.31± 10.29 0.64 Diseaseonset,(±SD) 43.16± 11.43 44.08± 11.72 0.73
Smoking(f) 13(28.88) 5(19.23) 0.37
Bodymassindex,(±SD) 27.22± 4.42 28.11± 5.84 0.39 Systemichypertension(f) 22(48.88) 14(53.84) 0.63 Diabetesmellitus(f) 6(13.33) 3(11.53) 1.00 Hypothyroidism(f) 13(28.88) 4(15.38) 0.084 Corticosteroids(f) 17(37.77) 16(61.53) 0.083 Metotrexate(f) 21(29.57) 11(24.44) 0.91 Leflunomide(f) 17(23.94) 10(22.22) 0.84
Anti-TNF(f) 19(42.22) 14(53.84) 0.46
Totalcholesterol>240(f) 11(24.44) 14(53.84) 0.020
HDL<35(f) 7(15.55) 1(3.84) 0.24
LDL>160(f) 6(13.33) 9(34.61) 0.067
Triglycerides>200(f) 10(22.22) 10(38.46) 0.17
DAS-28(±SD) 4.48± 1.28 5.13± 1.42 0.024
SF-36P(±SD) 39.2± 12.92 27.12± 12.71 <0.0001 SF-36M(±SD) 48.69± 9.35 34.19± 10.50 <0.0001 SF-36T(±SD) 42.55± 8.13 29.35± 7.37 <0.0001
anti-TNF,anti-tumornecrosisfactor;HDL,highdensitylipoprotein; LDL,lowdensitylipoprotein;DAS-28,diseasesactivityscorein28 joints;SF-36P,short-formhealthsurvey(physicaldomain);SF-36 M,short-formhealthsurvey(mentaldomain);SF-36T,short-form healthsurvey(totalscore).
(Table3),confirmedinatleastoneprevioustest,or subse-quentlyduringfollow-up.
AsfordiseaseactivitythroughDAS-28,4/71(5.63%)patients werefoundinastateofremission,5/71(7.04%)withmild dis-easeactivity,29/71(40.84%)withmoderatediseaseactivityand 33/71(46.47%)patientswithseverediseaseactivity.
SF-36wasthequestionnaireusedtoevaluatethequalityof lifeofpatientswithRA.Theresultsindicatedthatthemean valueswere34.68±13.05forPhysicalHealthDimensionand 43.33±15.28forMentalHealthDimension,withameantotal SF-36scoreof36.68±13.35.
Regardingphysicaldisabilityofpatients(HAQ),theresults were 45/71 (63.38%) with a mild level of disability, 21/71 (29.57%)foramoderateconditionand5/71(7.04%)forasevere condition.Statisticalsignificancewasnotedfortotal choles-terol (p=0.020), DAS-28 (p=0.024) and forphysical domain (p<0.0001),mentaldomain(p<0.0001)and total(p<0,0001) SF-36,asshowninTable3.Ofthesepatients,37.78%(17/54) weretakingCSinHAQ>1groupand61.54%(16/26)inHAQ≤1 group(p=0.084).
Table4showstheresultsoftheanalysisofcholesterol lev-els anditsfractionsinpatientsnottakingCSinrelationto HAQ>1.
StatisticallysignificantdifferenceswerefoundinTC>240 (p=0.019), HAQ≤1 (5/28=21.42%), HAQ>1 (6/10=60%) and SF-36 (p=0.013) variables.Theresultsofthese biochemical parametersforpatientsintreatmentwithCSwerenot pre-sented,becausethetreatmentwithCS isassociatedwitha higherprevalenceofriskfactors.
Table4–Analysisofcholesterollevelanditsfractions, diseaseactivityindexandqualityoflifeinpatients withoutuseofCSinrelationtoHAQ>1.
HAQ ≤ 1(28) HAQ>1(10) p
Totalcholesterol>240(f) 5(17.86) 6(60) 0.019
HDL<35(f) 5(17.86) 0(0) 0.96
LDL>160(f) 3(10.71) 4(40) 0.60
Triglycerides>200(f) 5(17.86) 2(20) 0.61 DAS-28(±SD) 4.5 ± 1.48 5.29 ± 0.89 0.089 SF-36(±SD) 43.39± 12.10 31.30± 13.81 0.013
HDL,high-densitylipoprotein;LDL,low-densitylipoprotein; DAS-28,diseaseactivity scorein 28joints;SF-36, short-formhealth survey.
levelsastatisticaldifference(p=0.025)wasnoted,according toTable5.
The higher prevalence of cardiovascular diseases, par-ticularlycoronaryartery disease,iswell establishedinRA.
Regarding CS and dyslipidemias, admittedly CS treatment
increase total cholesterol, LDL and triglyceride levels and reduceHDL;thus,inthisstudythesevariableswerenot ana-lyzedinrelationtotheresultsofHAQ≤1.0.
Discussion
Rheumatoidarthritisisadiseasethataffectsbothgendersin aproportionof3–4womenforeveryman.11Inthisstudythe genderratioinoursamplewas7:1,corroboratingtheresults foundbyBoechatetal.,12 who studied350non-indigenous patientsinthestateofAmazonas,andalsoemphasizes find-ingsofEuropeanandAmericanstudies,whoobtainedaratio ofabout7:1.13–15
PresenceofantibodiessuchasRFandanti-CCPare impor-tant prognosticmarkers forresponse totreatment. In this studyitwasobservedthat12/71(16.90%)patientswere pos-itive for ANA, a resultthat differs from a Japanese study, whoseresultwas39/104(37.5%)(p=0.038)16andfroma
Euro-pean study that showed positivity for ANA in 16/36 (44%)
patients(p=0.0045).17 Researchofanti-MCVantibodieswas positivein48/71(66.66%)patients–aresultsimilartothe Nor-wegianstudybyBesada etal.,who foundpositivecasesin
Table5–Comparisonoflipidlevelsinpatientswithor withoutuseofCS.
WithCS(n=33) WithoutCS (n=38)
p
Totalcholesterol>240 12(36.36) 12(31.58) 0.20
HDL<35 3(9.09) 5(13.16) 0.44
LDL>160 7(21.21) 8(21.05) 0.61
Triglycerides>200 14(42.42) 7(18.42) 0.025
HAQ 0.98± 0.72 0.73± 0.61 0.12
DAS-28 4.69± 1.14 4.74± 1.18 0.85
SF-36 34.85± 12.9 40.21± 13.41 0.094
HDL,high-densitylipoprotein;LDL,low-densitylipoprotein;HAQ, healthassessmentquestionnaire;DAS-28,diseaseactivityscorein 28joints;SF-36,short-formhealthsurvey.
57/75 (76%),18 and to the European study by Sghiri et al., whoseresultwas74.1%ofpositivityforanti-MCVin170sera from RApatients.19 Asfor anti-CCP, our resultswere sim-ilar to those found instudies inother Brazilian areas,for instance,Teixeiraetal.andSilvaetal.,withresultsof24/38 (63.15%)and68/100(68%),respectively.20,21 Ourresultswere higherthanthoseofaColombianstudy,whichshowed53/165 (33.1%)ofreactiveseraforanti-CCP(p=0.0084).22Theresults ofRFpositivityhavebeencontroversialinBrazilianstudies, rangingfrom49.3 to91%.20,23,24 InaKoreanstudythe inci-denceofreactivesampleswas209/302(69.2%),25asignificantly higherpositivitythanthatfoundinthisstudy:37/71(52.11%) (p=0.0077).
RAisadiseaseassociatedwithlowerlifeexpectancy,when comparedtothegeneralpopulation.26Thisfactisexplainedby theincreaseinprevalenceaswellasbyagreaterprogression ofcardiovasculardiseasesinthesepatients.27Geneticfactors andclassicriskfactorsassociatedwithinflammationforthese diseasescontributetoanincreaseandgreaterseverityof car-diovasculardiseasesinRA.28
Current and former smoking are considered oneof the
fewriskfactorsassociatedwithRAwithconfirmationin epi-demiological studies.29,30 This risk factor was identified in 1/4 ofthe patients in this study, which indicates a higher proportion of smokers than that found by Mikuls et al.,31 who identified smoking in 52/605(8.52%)patients withRA (p<0.0001).
AsforBMI,resultsofaGermanstudywith551patients, whichidentifiedvaluesof26.7±5.1,corroborateourresults of27.6±4.94.Ourresultswere similartothose of Myasoe-dovaetal.,32whoreportedthat3/4ofpatientswithRAhave BMI above the normalindex.33 In addition, the proportion
ofoverweight andobese patients, asdetermined fromBMI
accordingtothecriteriaforthegeneralpopulation,maybe underestimated,becauseithasbeenshownthat,foragiven amountofbodyfat,patientswithRAhave2pounds/m2less
thannormalcontrols.Therefore,BMIforthesepatientsshould be defined as23 and 28kg/m2 foroverweight and obesity,
respectively.34
Inrelationtosystemichypertension,theresultsshowed that36/71(50.70%)ofRApatientshadthisdisease,reinforcing thefindingsofCunhaetal.,whoreportedsystemic hyperten-sionin95/228(41.66%)patientswithRA.35 Ourresultswere similartothosefoundbyFerraz-Amaroetal.,showing sys-temichypertensionin36/101(35.74%)ofRApatients.36
As for thyroid disease, 16/71 (22.53%) of patients had
hypothyroidism and 2/71 (2.82%) hyperthyroidism, results
similartothoseofChanetal.,whofound12/69(17.4%)casesof hypothyroidismand4/69(5.8%)ofhyperthyroidisminpatients withRA.37
InastudybyParketal.,diabeteswasdiagnosedin27/302 (8.9%)patients,25whileinthestudybyGiuseppeetal.,the dis-easewasdiagnosedin4/132(3%)ofpatients.38Inthepresent study,thediagnosiswasconfirmedin9/71(12.67%)patients, afinding similartothatinthe firststudy,andsignificantly higherthaninthesecondstudy(p=0.0035),respectively.
Theanalyzedsampleshowedahigherprevalenceof dia-betic patients, 9/71 (12.67%),when compared to the study
conducted in the state of Amazonas, Brazil, 4/142 (3%)
Asforqualityoflife,theresultsindicatethatfewpatients
achieved remission or mild disease activity, 4 and 5%,
respectively,althoughonly5%ofpatientshadHAQassociated withseverefunctionalstatus.
Thedecreasedqualityoflifeinpatientswithless physi-caldysfunctionwasassessedbySF-36,admittedlyareliable and validtool and ableto measureimportant clinical fea-turesinRApatients.Itsusehasalsobeenadvocatedduring clinical follow-up ofthesepatients, asSF-36 evaluates dif-ferent areas,notjust the physicaldomain.39 In this study,
besidesthe physicaldomain, the mentaldomain was also
decreased inpatients with high HAQ score. Mental health
isanimportanttopic,becausedepressionisassociatedwith poortreatmentadherenceandwithincreasedmorbidityand mortality.40
Thepresenceofdyslipidemiasin36/71(50.70%)patients showedasignificantlyhigherfrequencythanthatfoundby Parketal.,where58/302(19.2%)ofaKoreanpopulationwith RAweredyslipidemicpatients.25
Lipid disorders are one ofthe most importantrisk fac-torsforcardiovasculardiseaseandstudieshaveshownthat
they are more prevalent in RA patients than in the
gen-eralpopulation.41 InuntreatedpatientswithRA,Parket al. demonstratedthatthesepatientspresentreductioninHDL cholesterollevelsandthatthischangeisrelatedtoC-reactive proteinlevels.42Inuntreatedpatients,totalcholesteroland LDLreductionsalsooccur.41Someauthorsalsodescribedthat
a decrease in inflammation coincides with an increase in
serumlevelsoflipids.13,43,44
Despitethelimitationsofthisstudy,ofacross-sectional nature,wefoundthattotalcholesterollevelsareassociated withhigherphysicaldysfunction.Theuseofcorticosteroids wasmoreprevalentamongpatientswithincreasedlevelsof triglycerides,butnotamongpatientswithhightotal choles-terollevels.Thus,Ferraz-Amaroetal.demonstrateddecrease intheactivityofcholesterolestertransferprotein(CETP)inRA patientswhoareundergoingtreatmentwithCS,butshowed nodifferenceinlipidlevelsinpatientswhowereundergoing treatmentwithversuswithoutcorticosteroids.36Thefunction ofthisproteiniscomplexanditsrelationtocardiovascular riskisnotwellunderstood.
The use of DMARDs can also induce increases in
total cholesterol and in HDL and triglyceride fractions,
especiallymethotrexate,leadingtochangescalled “normal-ization” according to Saiki.45 Regarding anti-TNF blockers, thepublishedliteraturehaveshownincreasedratesoftotal cholesterolandalsoofall its fractions;however, Choyand Sattarreportedthatameta-analysisisnotpossible,because thestudiesdifferonthetypeofinterventionandfollow-up time.41
Inthisstudy,itwasfoundthatpatientsinRAtreatment hadlipidlevelsconsideredasariskfactorforcardiovascular disease.46 However,therewasnocorrelationbetweenthese levelsanddiseaseactivity,asassessedbyDAS-28,similarto NavarroMillánetal.’sresults,13whoalsofoundnodifference betweenpatientstreatedwithmethotrexatemonotherapy ver-susthosetreatedwithacombinationtherapywithanti-TNF blockers.However,theauthorsreportedasignificantincrease intotalcholesterolandinall itsfractionsinthosepatients assessed.
ThepatientsinthisstudyhadbeenreferredfromtheBasic Health Unit.It wasobserved that, beforethe treatmentby a specialist, little was added to the diagnosis of systemic hypertension, diabetes and thyroid disease. These findings corroboratedatafromDesaietal.,whoshowedthatgeneral practitionersweretheprofessionalswhotreatedriskfactors forcardiovascular disease,notrheumatologists.47 However, generalpractitionersidentifiedmoreriskfactorsinthegeneral populationandindiabeticsthanintheRApopulation.
In this sense, the diagnosis of dyslipidemia has been
underestimated,probablybecauseRAassociationwith cardio-vascularriskandlipidabnormalitiesarenotyetestablished intheliteratureand,therefore,thisfeaturewasnot dissem-inated amonggeneralpractitioners.13Therecentpublished
data shows evidence that dyslipidemiasare present years
before the onset of clinical symptoms of RA.48 Park et al. reportedthatpolymorphismsassociatedwithLDLcholesterol (rs688 and rs4420638) are also related to RA susceptibility, severityandprogression.49
Therefore we emphasize that the screening of several
riskfactorsforcardiovasculardiseaseindicatestheneedfor pharmacologicaltreatmentandlifestylechanges,inorderto achieve a bettercontrol ofRA, sothat these patients may improvetheirqualityoflifeanddecreasetheriskforsystemic complications.
Conclusion
From this studyit wasconcludedthat: (1)notwithstanding thetherapeuticarsenalavailabletothesepatients,onlyafew haveachievedremissionorastateofmilddiseaseactivity; ontheotherhand,5%wereevolvingtoseveredysfunction.
(2) A high prevalence ofunderdiagnoseddyslipidemia was
observed in these patients. (3) Treatment with corticoste-roidsisassociatedwithahigherprevalenceofpatientswith hypertriglyceridemia.(4)Higherlevelsoftotalcholesterolare associatedwithmorephysicaldisability.(5)Thequalityoflife isreducedinpatientswithmajorphysicaldisability;however, thisfactorisnotassociatedwiththeuse,ornot,of corticoste-roids.(6)Follow-upofpatientswithRAisacomplextask,due tothe highriskfordevelopingcardiovasculardisease,thus requiringcontrolnotonlyofthediseaseactivity,butalsoof traditionalriskfactors.
Forfuturestudies,itissuggestedtheestablishmentofmore homogeneousgroupstodeterminetheinfluenceofthe dis-easeanddrugtreatmentsusedwithrespecttothepresence ofriskfactorsforcardiovasculardiseaseinpatientswithRA.
Funding
Coordenac¸ãodeAperfeic¸oamentodePessoaldeNível Supe-rior(CAPES),throughHealthSciencesPost-Graduation,Health SciencesSchool(FCS),UFGD.
Conflict
of
interests
r
e
f
e
r
e
n
c
e
s
1. McInnesIB,SchettG.Thepathogenesisofrheumatoid arthritis.NEnglJMed.2011;365:2205–19.
2. Lopez-OlivoMA,TayarJH,Martinez-LopezJA,PollonoEN, CuetoJP,Gonzales-CrespoMR,etal.Riskofmalignanciesin patientswithrheumatoidarthritistreatedwithbiologic therapy:ameta-analysis.JAMA.2012;308:898–908. 3. Amaya-AmayaJ,Sarmiento-MonroyJC,MantillaRD,
Pineda-TamayoR,Rojas-VillarragaA,AnayaJM.Novelrisk factorsforcardiovasculardiseaseinrheumatoidarthritis. ImmunolRes.2013;56:267–86.
4. KlareskogL,RonnelidJ,LundbergK,PadyukovL,AlfredssonL. Immunitytocitrullinatedproteinsinrheumatoidarthritis. AnnuRevImmunol.2008;26:651–75.
5. ArnettFC,EdworthySM,BlochDA,McShaneDJ,FriesJF, CooperNS,etal.TheAmericanRheumatismAssociation 1987revisedcriteriafortheclassificationofrheumatoid arthritis.ArthritisRheum.1988;31:315–24.
6. Gaujoux-VialaC,MouterdeG,BailletA,ClaudepierreP,Fautrel B,LeLoetX,etal.Evaluatingdiseaseactivityinrheumatoid arthritis:whichcompositeindexisbest?Asystematic literatureanalysisofstudiescomparingthepsychometric propertiesoftheDAS,DAS28,SDAIandCDAI.JointBone Spine.2012;79:149–55.
7. VIBrazilianGuidelinesonHypertension.ArqBrasCardiol. 2010;95:1–51.
8. DiabetesSBd.DiretrizesdaSociedadeBrasileiradeDiabetes. DiretrizesSBD.2009.
9. FerrazMB,QuaresmaMR,AquinoLR,AtraE,TugwellP, GoldsmithCH.Reliabilityofpainscalesintheassessmentof literateandilliteratepatientswithrheumatoidarthritis.J Rheumatol.1990;17:1022–4.
10.CampolinaAG,BortoluzzoAB,FerrazMB,CiconelliRM. Healthpreferencesmeasures:comparingBrazilSF-6Dversion withSF-36derivedversions,inpatientswithrheumatoid arthritis.ActaReumatolPort.2010;35:200–6.
11.AlarconGS.Epidemiologyofrheumatoidarthritis.RheumDis ClinNorthAm.1995;21:589–604.
12.BoechatNdeO,OguskuMM,BoechatAL,SadahiroA. InteractionbetweensmokingandHLA-DRB1*04geneis associatedwithahighcardiovascularriskinBrazilian Amazonpatientswithrheumatoidarthritis.PLOSONE. 2012;7:e41588.
13.Navarro-MillanI,Charles-SchoemanC,YangS,BathonJM, BridgesSLJr,ChenL,etal.Changesinlipoproteinsassociated withmethotrexateorcombinationtherapyinearly
rheumatoidarthritis:resultsfromthetreatmentofearly rheumatoidarthritistrial.ArthritisRheum.2013;65:1430–8. 14.StraubRH,PaimelaL,PeltomaaR,ScholmerichJ,
Leirisalo-RepoM.Inadequatelylowserumlevelsofsteroid hormonesinrelationtointerleukin-6andtumornecrosis factorinuntreatedpatientswithearlyrheumatoidarthritis andreactivearthritis.ArthritisRheum.2002;46:654–62. 15.RadnerH,SmolenJS,AletahaD.Comorbidityaffectsall
domainsofphysicalfunctionandqualityoflifeinpatients withrheumatoidarthritis.Rheumatology(Oxford). 2011;50:381–8.
16.NishimuraS,NishiyaK,HisakawaN,ChikazawaH,OokuboS, NakataniK,etal.Positivityforantinuclearantibodyin patientswithadvancedrheumatoidarthritis.ActaMed Okayama.1996;50:261–5.
17.BrunsA,Nicaise-RolandP,HayemG,PalazzoE,DieudeP, Grootenboer-MignotS,etal.Prospectivecohortstudyof effectsofinfliximabonrheumatoidfactor,anti-cyclic citrullinatedpeptideantibodiesandantinuclearantibodiesin
patientswithlong-standingrheumatoidarthritis.JointBone Spine.2009;76:248–53.
18.BesadaE,NikolaisenC,NossentH.Diagnosticvalueof antibodiesagainstmutatedcitrullinatedvimentinfor rheumatoidarthritis.ClinExpRheumatol.2011;29:85–8. 19.SghiriR,BouaginaE,ZaglaouiH,MestiriH,HarzallahL,
HarrabiI,etal.Diagnosticperformancesofanti-cyclic citrullinatedpeptideantibodiesinrheumatoidarthritis. RheumatolInt.2007;27:1125–30.
20.SilvaAF,MatosAN,LimaAMS,LimaEF,CorreaMICC, CarvalhoEM.Associationofanti-cycliccitrullinatedpeptide antibodyandsevererheumatoisarthritis.RevBrasReumatol. 2006;46:165–73.
21.TeixeiraRCA,GabrielAJr,deMartinoMC,MartinsLC,Lopes AC,TufikS.Markersofendothelialactivationand
autoantibodiesinrheumatoidarthritis.RevBrasReumatol. 2007;47:411–7.
22.Rojas-VillarragaA,Ortega-HernandezOD,GomezLF,Pardo AL,Lopez-GuzmanS,Arango-FerreiraC,etal.Riskfactors associatedwithdifferentstagesofatherosclerosisin Colombianpatientswithrheumatoidarthritis.Semin ArthritisRheum.2008;38:71–82.
23.DavidJM,MatteiRA,MauadJL,deAlmeidaLG,NogueiraMA, MenolliPV,etal.Clinicalandlaboratoryfeaturesofpatients withrheumatoidarthritisdiagnosedatrheumatology servicesintheBrazilianmunicipalityofCascavel,PR,Brazil. RevBrasReumatol.2013;53:57–65.
24.CorbachoMI,DapuetoJJ.Assessingthefunctionalstatusand qualityoflifeofpatientswithrheumatoidarthritis.RevBras Reumatol.2010;50:31–43.
25.ParkYJ,YooSA,ChoiS,YooHS,YoonHS,ChoCS,etal. Associationofpolymorphismsmodulatinglow-density lipoproteincholesterolwithsusceptibility,severity,and progressionofrheumatoidarthritis.JRheumatol. 2013;40:798–808.
26.ErhardtCC,MumfordPA,VenablesPJ,MainiRN.Factors predictingapoorlifeprognosisinrheumatoidarthritis:an eightyearprospectivestudy.AnnRheumDis.1989;48:7–13. 27.KitasGD,ErbN.Tacklingischaemicheartdiseasein
rheumatoidarthritis.Rheumatology(Oxford).2003;42:607–13. 28.Stavropoulos-KalinoglouA,MetsiosGS,KoutedakisY,Kitas
GD.Obesityinrheumatoidarthritis.Rheumatology(Oxford). 2011;50:450–62.
29.ChristensenAF,LindegaardHM,JunkerP.Smoking–arisk factorforrheumatoidarthritisdevelopment.UgeskrLaeger. 2008;170:2864–9.
30.MichouL,TeixeiraVH,PierlotC,LasbleizS,BardinT,DieudeP, etal.Associationsbetweengeneticfactors,tobaccosmoking andautoantibodiesinfamilialandsporadicrheumatoid arthritis.AnnRheumDis.2008;67:466–70.
31.MikulsTR,SaylesH,YuF,LevanT,GouldKA,ThieleGM,etal. Associationsofcigarettesmokingwithrheumatoidarthritis inAfricanAmericans.ArthritisRheum.2010;62:3560–8. 32.MyasoedovaE,CrowsonCS,KremersHM,Fitz-GibbonPD,
TherneauTM,GabrielSE.TotalcholesterolandLDLlevels decreasebeforerheumatoidarthritis.AnnRheumDis. 2010;69:1310–4.
33.OelznerP,SchwabeA,LehmannG,EidnerT,FrankeS,WolfG, etal.Significanceofriskfactorsforosteoporosisisdependent ongenderandmenopauseinrheumatoidarthritis.
RheumatolInt.2008;28:1143–50.
34.Stavropoulos-KalinoglouA,MetsiosGS,PanoulasVF,Douglas KM,NevillAM,JamurtasAZ,etal.Cigarettesmoking associateswithbodyweightandmusclemassofpatients withrheumatoidarthritis:across-sectional,observational study.ArthritisResTher.2008;10:R59.
rheumatoidarthritispatientsandisassociatedwithdisease activity.ScandJRheumatol.2012;41:186–91.
36.Ferraz-AmaroI,Gonzalez-GayMA,Garcia-DopicoJA, Diaz-GonzalezF.Cholesterylestertransferproteininpatients withrheumatoidarthritis.JRheumatol.2013;40:1040–7. 37.ChanAT,Al-SaffarZ,BucknallRC.Thyroiddiseasein
systemiclupuserythematosusandrheumatoidarthritis. Rheumatology(Oxford).2001;40:353–4.
38.DiGiuseppeD,OrsiniN,AlfredssonL,AsklingJ,WolkA. Cigarettesmokingandsmokingcessationinrelationtorisk ofrheumatoidarthritisinwomen.ArthritisResTher. 2013;15:R56.
39.RutaDA,HurstNP,KindP,HunterM,StubbingsA.Measuring healthstatusinBritishpatientswithrheumatoidarthritis: reliability,validityandresponsivenessoftheshortform 36-itemhealthsurvey(SF-36).BrJRheumatol.1998;37:425–36. 40.AngDC,ChoiH,KroenkeK,WolfeF.Comorbiddepressionis
anindependentriskfactorformortalityinpatientswith rheumatoidarthritis.JRheumatol.2005;32:1013–9. 41.ChoyE,SattarN.Interpretinglipidlevelsinthecontextof
high-gradeinflammatorystateswithafocusonrheumatoid arthritis:achallengetoconventionalcardiovascularrisk actions.AnnRheumDis.2009;68:460–9.
42.ParkDC,HertzogC,LeventhalH,MorrellRW,LeventhalE, BirchmoreD,etal.Medicationadherenceinrheumatoid arthritispatients:olderiswiser.JAmGeriatrSoc. 1999;47:172–83.
43.PopaC,vandenHoogenFH,RadstakeTR,NeteaMG,Eijsbouts AE,denHeijerM,etal.Modulationoflipoproteinplasma
concentrationsduringlong-termanti-TNFtherapyinpatients withactiverheumatoidarthritis.AnnRheumDis.
2007;66:1503–7.
44.SchimmelEK,YaziciY.Increasedlipidlevelsbutunchanged atherogenicindexinrheumatoidarthritispatientstreated withbiologicdiseasemodifyingantirheumaticdrugs: publishedexperience.ClinExpRheumatol.2009;27:446–51. 45.SaikiO,TakaoR,NaruseY,KuharaM,ImaiS,UdaH.
Infliximabbutnotmethotrexateinducesextra-highlevelsof VLDL-triglycerideinpatientswithrheumatoidarthritis.J Rheumatol.2007;34:1997–2004.
46.daMotaLM,CruzBA,BrenolCV,PereiraIA,FronzaLS,Bertolo MB,etal.2011ConsensusoftheBrazilianSocietyof
Rheumatologyfordiagnosisandearlyassessmentof rheumatoidarthritis.RevBrasReumatol.2011;51:199–219. 47.DesaiSS,MylesJD,KaplanMJ.Suboptimalcardiovascularrisk
factoridentificationandmanagementinpatientswith rheumatoidarthritis:acohortanalysis.ArthritisResTher. 2012;14:R270.
48.vanHalmVP,NielenMM,NurmohamedMT,van
SchaardenburgD,ReesinkHW,VoskuylAE,etal.Lipidsand inflammation:serialmeasurementsofthelipidprofileof blooddonorswholaterdevelopedrheumatoidarthritis.Ann RheumDis.2007;66:184–8.