www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
ProACS
risk
score:
An
early
and
simple
score
for
risk
stratification
of
patients
with
acute
coronary
syndromes
Ana
Teresa
Timóteo
a,∗,
Sílvia
Aguiar
Rosa
a,
Marta
Afonso
Nogueira
a,
Adriana
Belo
b,
Rui
Cruz
Ferreira
a,
on
behalf
of
the
ProACS
Investigators
aCardiologyDepartment,SantaMartaHospital,CentroHospitalardeLisboaCentral,Lisbon,Portugal bNationalCenterforDataCollectioninCardiology,PortugueseSocietyofCardiology,Coimbra,Portugal
Received29March2016;accepted18May2016 Availableonline31January2017
KEYWORDS Riskstratification score; Acutecoronary syndromes; Prognosis Abstract
Introduction:There are barriers to proper implementation of risk stratification scores in patientswithacutecoronarysyndromes(ACS),includingtheircomplexity.Ourobjectivewasto developasimplescoreforriskstratificationofall-causein-hospitalmortalityinapopulation ofpatientswithACS.
Methods:ThescorewasdevelopedfromanationwideACSregistry.Thedevelopmentand inter-nalvalidationcohortswereobtainedfromthefirst31829patients,randomlyseparated(60%and 40%,respectively).Theexternalvalidationcohortconsistedofthelast8586patientsincluded intheregistry.Thiscohortissignificantlydifferentfromtheothercohortsintermsof base-linecharacteristics,treatmentandmortality.Multivariatelogisticregressionanalysiswasused toselectfourvariableswiththehighestpredictivepotential.Ascorewasallocatedtoeach parameterbasedontheregressioncoefficientofeachvariableinthelogisticregressionmodel: 1pointforsystolicbloodpressure≤116mmHg,Killipclass2or3,andST-segmentelevation; 2pointsforage≥72years;and3pointsforKillipclass4.
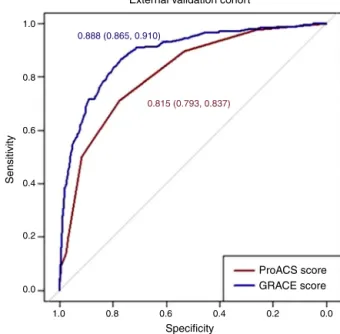
Results:Thenewscorehadgooddiscriminativeabilityinthedevelopmentcohort(areaunder thecurve[AUC]0.796),anditwassimilarintheinternalvalidationcohort(AUC0.785,p=0.333). Intheexternalvalidationcohort,therewasalsoexcellentdiscriminativeability(AUC0.815), withanadequatefit.
∗Correspondingauthor.
E-mailaddress:anatimoteo@yahoo.com(A.T.Timóteo).
http://dx.doi.org/10.1016/j.repc.2016.05.010
Conclusions:TheProACSriskscoreenableseasyandsimpleriskstratificationofpatientswith ACS for in-hospital mortality thatcan beused atthe first medical contact,with excellent predictiveabilityinacontemporarypopulation.
©2016SociedadePortuguesadeCardiologia.PublishedbyElsevier Espa˜na, S.L.U.Allrights reserved. PALAVRAS-CHAVE Scorede estratificac¸ão derisco; Síndromescoronárias agudas; Prognóstico
ScorederiscoProACS:emscoresimpleseprecoceparaestratificac¸ãoderisco emdoentescomsíndromescoronáriasagudas
Resumo
Introduc¸ão:Existemalgumasbarreirasàimplementac¸ãoadequadadosscoresdeestratificac¸ão de risco em doentes comsíndrome coronária aguda(SCA), tais como a suacomplexidade. Onossoobjetivofoidesenvolverumscoresimplesparaestratificac¸ãoderiscodemortalidade hospitalardetodasascausasnumapopulac¸ãodedoentescomSCA.
Métodos: O score foi desenvolvido a partir de um registo nacional de SCA. A coorte de desenvolvimentoedevalidac¸ãointernafoiobtidaapartirdosprimeiros31829doentes, aleato-riamenteseparados (60e40%,respetivamente). A coortedevalidac¸ãoexternaé composta pelosúltimos8586doentesincluídosnoregisto.Estacoorteésignificativamentediferentedas restantes(característicasbasais,tratamentoemortalidade).Foiutilizadaanálisederegressão logísticamultivariadaparaselecionarasquatrovariáveiscommaiorpotencialpreditivoefoi atribuídaumapontuac¸ãobaseadanocoeficientederegressãodecadavariávelnomodelode regressãologística:umpontoparaTAS≤116mmHg,classeKillip2ou3,eelevac¸ãosegmento ST,doispontosparaidade≥72anosetrêspontosparaclasseKillip4.
Resultados: Onovo scoretemuma boacapacidadepreditiva nacoortededesenvolvimento (areaundercurve[AUC]0,796),semelhanteàcoortedevalidac¸ãointerna(AUC0,785,p=0,333). Nacoortedevalidac¸ãoexternatambémapresentouumaexcelentecapacidadediscriminativa (AUC0,815),comcalibrac¸ãoadequada.
Conclusões:Oscore deriscoProACS permite umaestratificac¸ãode riscoprecocee simples emdoentescomSCAparamortalidadehospitalar,quepodeserutilizadanoprimeirocontacto médico,comexcelentecapacidadepreditivanumapopulac¸ãocontemporânea.
©2016SociedadePortuguesadeCardiologia.PublicadoporElsevierEspa˜na,S.L.U.Todosos direitosreservados.
Introduction
The management of acute coronary syndromes (ACS) has
changeddramaticallyinthepast20yearsfollowing
demon-strationofthebenefitsassociatedwithinvasivestrategies,
particularly in high-risk patients.1---5 Selection for these
strategiesis an importanttaskin every patientwithACS.
Severalrisk scores have been developedfor this purpose,
fromboth clinicaltrials andregistries.Theydifferin
pre-dictive accuracy as well as in the number and type of
variablesincluded.ThefirsttobedevelopedwastheTIMI
riskscore,6,7butitspredictiveaccuracyisusuallylowerthan
morerecentscores.Themostrecentandmostwidelyused
istheGlobalRegistryofAcuteCoronaryEvents(GRACE)risk
score,developedfromtheGRACEregistry.8,9 Thishasvery
highpredictiveaccuracy,butincludesmanyvariableswith
significant complexity, which may explain why it is often
underused.10,11
Previously,ourgroupandothershavedemonstratedthat
theseriskscorescanbesimplified,withaslightreductionin
predictiveaccuracycomparedtotheGRACEscore,butthat
can beconsidered acceptable.12,13 These simplifiedscores
showsimilaraccuracytotheTIMIriskscore.6,7,14
Ourobjectivewastodevelopasimplescoreforrisk
strat-ificationofin-hospitalmortalityinpatientswithACS,tobe
usedvery early in patientmanagement, includingat
pre-hospitallevel.
Methods
The Portuguese Registry on Acute Coronary Syndromes
(ProACS)isamulticenternationwideregistryofACS.Itisa
prospective,continuousobservationalregistry,with33
par-ticipatingcardiologydepartmentsfromPortugal(mainland
andislands).15Patientinclusionintheregistrybeganon
Jan-uary1,2002,andallconsecutiveadultpatients(≥18years)
registered until October 31, 2014 were included in the
present study.Criteriafor inclusioninthe registrywerea
historyofchestpainat restorother symptomssuggestive
of an ACS (with themost recent episodeoccurring within
48hoursofadmission)withorwithoutneworpresumednew
Jan 1, 2002 - Oct 30, 2014 40 415 patients Jan 1, 2002 - Jun 30, 2011 31 829 patients Jul 1, 2011 - Oct 30, 2014 8586 patients 60% for development 19 128 patients
17 380 patients 11 548 patients 8532 patients
Missing values
40% for internal validation 12 701 patients
External validation 8586 patients
Figure1 Flowchartofpatientinclusion.
branchblockorelevatedbiomarkersofmyocardialdamage
witha riseand/or fall inlevels. Acutemyocardial
infarc-tion(MI)wasdefinedaccordingtotheuniversaldefinitionof
type1myocardial infarction.16 Adiagnosisof ST-elevation
myocardialinfarction(STEMI)wasmadeinthepresenceof
persistent(>30min) ST-segmentelevation.Allother cases
withelevatedbiomarkersofmyocardialdamagewere
con-siderednon-STEMI(NSTEMI).
Data were collected in a dedicated computer
database, and included demographic,clinical and patient
management-related characteristics, as well as clinical
outcome.Hypertension,diabetesandhyperlipidemiawere
definedaseitherpreviouslyknownoronspecifictherapy.If
thepatientshadsmoked duringtheprevious 30daysthey
were classified as smokers and were self-reported.
Deci-sions on patient management strategy, including referral
forcoronaryangiographyandmodeofmyocardial
revascu-larization,ifany,werelefttotheattendingphysicianand
site-specificprotocols.Theprimaryendpointwasall-cause
mortalityduringtheindexhospitalization.
From the main study population (40415 records), we
obtainedthreecohortsofpatients(Figure1).FromJanuary
1, 2002 to June 30, 2011, 31829 patients were included
in the registry and were randomly divided into a cohort
for risk score development(60% of the patients) and the
cohort for internal validation (the remaining 40%). All
patients included between July 2011 and October 2014
(8586 patients) were included in the external validation
cohort.Patientswithmissingvaluesforthemainvariables
wereexcluded(2955 patients---7.3%of theinitialpatient
sample).
The study complies with the 1975 Declaration of
Helsinki.The nationaldataprotectioncommitteefor
clin-ical research approved the study protocol and informed
consentwasobtainedfromeachpatient.Theregistryis
reg-isteredatClinicalTrials.govwiththeidentification number
NCT01642329.
This manuscript was written in accordance with the
Transparent Reporting of a Multivariable Predictor Model
forIndividualPrognosisorDiagnosis(TRIPOD)statementon
appropriatedescriptionofstudiesforscorevalidation.17
Statisticalanalysis
Categoricalvariablesarereportedaspercentagesand
dif-ferencesbetweengroups weretested withthechi-square
test or Fisher’s exact test, as appropriate. Continuous
variables are reported as means and standard deviation.
Normality was tested with the Kolmogorov-Smirnov test.
One-wayANOVAwasusedtocomparecontinuousvariables
withnormaldistribution.Continuousvariableswithout
nor-maldistributionarereportedasmediansandinterquartile
rangeandwerecomparedwiththeKruskal-Wallistest.
Multivariablestepwiseforwardlogisticregressionmodels
were used to select the four variables with the
high-est predictive potential for score development. Variables
wereremovedfromthemodelwhenthep-valueexceeded
0.10 and were kept in the final model when less than
0.05. The variables included were age, admission heart
rate, systolic blood pressure and Killip class, creatinine,
ST-segment deviation, gender, diabetes, smoking status,
previous myocardial infarction, percutaneous coronary
intervention(PCI),coronaryarterybypassgrafting,strokeor
peripheralarterialdisease.The selectedcontinuous
varia-bleswerecategorized(dichotomized)byreceiveroperating
characteristic(ROC)curveanalysis.Cut-offswereobtained
bymaximizingthesumofsensitivityandspecificity.Foreach
variable,appropriateweightsweredeterminedbasedonthe
regressioncoefficientofthefinallogisticmodel(tothe
clos-estwholenumber).Pointsweresummedtoobtainthefinal
riskscore.ROCcurveanalysisandtheareaunderthecurve
(AUC)wereusedtostudythepredictive valueofthenew
riskscoreineach cohort.Bootstraptechniques wereused
forROCcurvecomparisonandforconfidenceintervals.
IBMSPSSStatisticssoftware(version19.0.0.2)wasused
for all statistical analyses. All statistical tests were
Table1 Clinicalcharacteristicsofthepatientsineachcohort. Development cohort(n=17380) Internalvalidation cohort(n=11548) Externalvalidation cohort(n=8532) p Age,years 66(13) 66(13) 66(13) 0.155 Male(%) 69.9 70.1 72.1 <0.001 BMI(kg/m2) 27(4) 27(4) 27(4) 0.785 Previoushistory(%) Hypertension 62.2 62.9 69.8 <0.001 Smoking 24.0 24.5 27.9 <0.001 Diabetes 27.0 27.8 30.4 <0.001 Hyperlipidemia 45.2 45.4 57.5 <0.001 Myocardialinfarction 18.4 18.6 20.2 0.002 PCI 8.0 8.3 14.5 <0.001 CABG 4.1 4.3 5.0 0.005 Stroke/TIA 7.0 7.3 7.6 0.132 PAD 3.1 3.5 5.8 <0.001 COPD 6.6 6.1 5.5 0.195 Admission STEMI(%) 43.6 42.3 40.8 <0.001 Heartrate(bpm) 79(20) 79(20) 77(19) <0.001 SBP(mmHg) 141(30) 141(30) 138(29) <0.001 Killipclass≥2(%) 18.9 19.3 15.5 <0.001 Killipclass4(%) 2.0 2.0 1.9 0.801 Creatinine(mg/dl) 0.9(0.8-1.2) 0.9(0.8-1.2) 0.9(0.8-1.2) 0.130 Bloodglucose(mg/dl) 130(108-170) 130(107-175) 129(106-174) 0.739 Hemoglobin(g/dl) 13.7(1.9) 13.8(1.9) 13.7(1.9) 0.618 Coronaryangiography(%) 68.9 69.1 86.8 <0.001 Multivesseldiseasea(%) 50.6 50.6 50.7 0.994 PCI(%) 43.8 43.4 65.0 <0.001 CABG(%) 1.4 1.5 0.5 <0.001 LVEF<50%(%) 39.9 39.9 36.7 <0.001 Outcome(%) Re-infarction 1.5 1.4 1.2 0.120 Stroke/TIA 0.8 0.9 0.8 0.807 Majorbleeding 1.3 1.2 1.4 0.298 Death 5.4 5.0 4.0 <0.001
BMI:bodymassindex;CABG:coronaryarterybypassgrafting;COPD:chronicobstructivepulmonarydisease;LVEF:leftventricularejection fraction;PAD:peripheralarterialdisease;PCI:percutaneouscoronaryintervention;SBP:systolicbloodpressure;STEMI:ST-elevation myocardialinfarction;TIA:transientischemicattack.
aPercentageofpatientswhounderwentcoronaryangiography.
Results
Patients were included in each cohort according to the
flowchart presented in Figure 1. Patients in the
develop-ment cohort had fewer risk factors and less past history
of coronary artery disease compared to the internal and
external validation cohorts (Table 1). On admission they
had higher heart rate and systolic blood pressure and
worse Killip class and STEMI was more frequent,
partic-ularly compared to the external validation cohort. They
lessoftenunderwentcoronaryangiographyand
revascular-izationprocedures.In-hospital mortalitywaslower inthe
validation cohorts, particularly in the external validation
cohort.
Inthe multivariatemodel,the variableswiththe
high-estpredictiveability wereage,systolicblood pressureon
admission,KillipclassonadmissionandST-segment
eleva-tion. The cut-off obtained for age was 72 years and for
systolicbloodpressureitwas116mmHg.TheProACSscore
was developed according to these cut-offs with a simple
scoringsystem(Table2).
The ProACSscore wasthen tested in the development
cohort as well as in the internal and external validation
cohorts.Inallcohortsthediscriminativeabilitywasalsovery
good(AUC>0.75)andsimilarbetweenallcohorts,although
slightly higherin theexternal validationcohort (Table 3).
The fit of the developed logistic model was also good in
thedevelopmentcohort(Figure2).Performancewassimilar
comparingpatientswithSTEMIandnon-ST-elevationacute
coronary syndrome (NSTACS). However, compared to the
GRACErisk score,thepredictive abilitywasslightlylower
Table2 ProACSriskscore.
Variable Cut-off Points
Age <72years ≥72years 0 2 SBP <116mmHg ≥116mmHg 1 0 Killipclass 1 2 3 4 0 1 1 3 ST-segmentelevation No Yes 0 1
SBP:systolicbloodpressure.
Table3 AreaunderthecurvefortheProACSriskscorein thedifferentcohorts.
Cohort C-statistic(95%CI)
Development 0.796(0.782-0.810)
Internalvalidation 0.785(0.767-0.803)
Externalvalidation 0.815(0.793-0.837)
STEMI 0.799(0.768-0.830)
NSTACS 0.809(0.774-0.845)
CI:confidenceinterval;NSTACS:non-ST-elevationacute coro-narysyndrome;STEMI:ST-elevationmyocardialinfarction.
400 Hosmer-Lemeshow chi-square (6 df)=8072 p=0.233 300 200 Predicted deaths 100 Observed deaths 0 0 100 200 300 400
Figure2 Fitofthefinalmultivariatelogisticregressionmodel inthedevelopmentcohort.df:degreesoffreedom.
OntheProACSriskscore,patientswithascore0havea
lowriskofin-hospitaldeath(<1%)andthosewithascore≥3
haveahighrisk(>4%).Patientswithscore1-2have
interme-diaterisk(1-4%)(Figure4).
Discussion
Inthepast20years,invasivestrategiesforthetreatmentof
ACShavehadasignificantimpactonprognosis.1---5Itisthus
importanttoidentifyandselectthepatientswhocanderive
themostbenefitfromthesestrategies.InSTEMIprimaryPCI
isnowgenerallyrecommended1,3 andsoriskstratification
1.0 0.8 0.888 (0.865, 0.910) 0.815 (0.793, 0.837) 0.6 0.4 0.2 Sensitivity 0.0 1.0 0.8
External validation cohort
0.6 Specificity 0.4 0.2 ProACS score GRACE score 0.0
Bootstrap test for two correlated ROC curves (D=-7.6893, p<0.001) Figure3 ComparisonofProACSandGRACEriskscoresinthe externalvalidationcohort.ROC:receiveroperating character-istic. 12 10 8 6 4 2 0 0.4% Score 0 Obser ve d in-hospital mor tality Score 1-2 Score ≥3 2.1% 11.2% %
Figure4 Observedin-hospitalmortalityintheexternal vali-dationcohortaccordingtotheriskcut-offs.
forthesepatientsislessimportant,butsomecasesrequire
urgent pre-hospitalreferral to amore specialized center.
NSTACS patients are a heterogeneous group and invasive
strategiesarerecommendedinhigh-andintermediate-risk
patients.2,4 Forthis reason,several risk scores have been
developed in the past 15 years. The TIMI risk scores for
STEMI and unstable angina/NSTEMI were developed from
largeclinicaltrials.6,7Thesescoresweresimpleandintuitive
withsimple variables,andtheir usespreadrapidly
world-wide.Other risk scores werealso developed but theTIMI
scoreremainedthemostuseduntil2003,whentheGRACE
registrygrouppublishedariskscoreforin-hospital
mortal-ityinpatientswithACSandlaterforsix-monthmortality.8,9
Thisscorewasdevelopedfromaregistrythatrepresented
real-world patients instead of the highly controlled and
selectedpopulations of clinical trials, fromwhich elderly
patientsandthosewithsevererenaldysfunctionwere
usu-allyexcluded.TheGRACEriskscoreshowedhighpredictive
themostusedscore,andwassubsequentlyupdated.18
How-ever,theGRACEscore’snomogramincludesseveralvariables
withawiderangeofcategories,someofwhichcanonlybe
obtainedafterinitialdiagnostictests.Thisaddscomplexity
toriskscoringandmeansitcannotbeusedatanearlystage.
Thismightexplainitsunderuseinclinicalpracticeinspite
ofthedevelopmentofseveraltools.10,11
Ourgroupdemonstratedinasingle-centerstudythatitis
possibletosimplifytheseriskscoreswithsimpleandfewer
variables,withsimilarpredictiveaccuracy,althoughwedid
notsetouttoproposeanewriskscoreduetotheinherent
limitationsofourstudy.12 ACanadiangrouphasdeveloped
anotherscore, the Canada Acute Coronary Syndrome risk
score (C-ACS), based onlarge ACS registries in Canada.13
Theselectedvariableswereage,Killipclass,systolicblood
pressureandheartrate,withasimple dichotomizationof
continuousvariables.Thisscoreenablesrapidstratification
ofpatientswithACS,evenbyhealthcareprofessionals
with-outadvanced medicaltraining,in pre-hospitalsettings or
emergencydepartments.Itshowedagoodpredictivevalue
forboth short-andlong-term mortalityandinbothSTEMI
andNSTACS.The c-statistic ofthis newscoreis adequate
(≥0.75)butslightlylowerthanclassicalriskscoresforthe
predictionofshort-andlong-termmortality.13
SinceNorth Americanpopulations have different
char-acteristicsfromotherpopulations,includingEuropeanand
particularlyMediterranean(low-risk)countries,wethought
itwouldbevaluabletodevelopasimilarriskscoreforearly
useinACSthatwouldbesimpleandeasytomemorize.19,20
The ProACS risk score was developed from a nationwide
registry of ACS in Portugal. The sample is large and is
representativeofreal-worldpatients.Inourscore,weused
simplevariables (age,systolicblood pressure,ST-segment
elevation and Killip class on admission), similar to the
C-ACS score, and confirmed the validity of the selected
variables(thosewiththehighest predictivevalue).It also
showed good predictive accuracy, which although lower
thantheGRACEriskscore,isstillacceptable.Itisalsoeasy
tocalculate andcan beappliedinpre-hospitalsettingsor
emergencydepartmentsbynon-medicalhealthcare
profes-sionals.Itimprovesreferralofhigh- andintermediate-risk
patientstohospitalswithcatheterizationfacilities,
partic-ularly in NSTACS. External validation was performed in a
morerecentcohortofpatients,whichmayexplainsomeof
thedifferencesobserved,comparedwiththedevelopment
andinternalvalidationcohorts,particularlythelower
pro-portionof STEMIand higher rateof coronary angiography
andrevascularization.Itis alsoimportanttomentionthat
predictive accuracy was higher in the external validation
cohort,whichhighlightsitsutilityincontemporarycohorts.
Predictive accuracy was similar in patients with STEMI
and NSTACS, suggesting that it can also be used in
STEMI patients, although in this group the recommended
strategyisprimaryPCI.
Limitations
ThisscorewasdevelopedandvalidatedinaPortuguese
pop-ulation.Itrequiresfurthervalidationinother populations,
preferablyincontemporarycohorts.
Wechosetoexcludefromtheanalysisallpatientswith
missingvaluesofthescorevariables.Overall,only7.3%of
the patients were excluded, which is acceptable because
of our large sample size. Data from the external
vali-dationcohortweremorecompleteandfewerpatientswere
excludedfromthiscohort.
Wecouldnottestgoodnessoffitwiththenewriskscore
becausethisis acategoricalscoreandisthusnotsuitable
forthistypeofanalysis.
Conclusion
TheProACSriskscoreenableseasyandsimplerisk
stratifi-cationforin-hospitalmortalityatthefirstmedicalcontact
ofpatientswithACS.Italsohasexcellentpredictiveability
inacontemporarypopulationofpatientswithACS,although
slightlylowerthantheGRACEriskscore.Itssimplicitycan
improveimplementationof scores forrisk stratification in
clinicalpractice,althoughfurthervalidationinother
popu-lationsandcountriesiswarranted.
Ethical
disclosures
Protection of human and animal subjects.The authors
declarethatnoexperimentswereperformedonhumansor
animalsforthisstudy.
Confidentialityofdata.Theauthorsdeclarethattheyhave
followedtheprotocolsoftheirworkcenteronthe
publica-tionofpatientdata.
Right to privacy and informed consent.The authors
declarethatnopatientdataappearinthisarticle.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology(ESC)StegG, JamesSK,AtarD,etal.ESC Guide-lines for the management of acute myocardial infarction in patientspresenting with ST-segment elevation. EurHeart J. 2012;33:2569---619.
2.HammCW,BassandJP, AgewallS,etal.,ESCCommitteefor Practice Guidelines. ESC Guidelines for the management of acutecoronarysyndromesinpatientspresentingwithout per-sistentST-segmentelevation.EurHeartJ.2011;32:2999---3054.
3.O’GaraPT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/AmericanHeartAssociationTaskForceonPractice Guidelines.Circulation.2013;127:e362---425.
4.AmsterdamEA,WengerNK,BrindisRG,etal.2014AHA/ACC Guideline for the management of patients with non-ST-elevationacutecoronarysyndromes:areportoftheAmerican CollegeofCardiology/AmericanHeartAssociationTaskForceon PracticeGuidelines.Circulation.2014;130:e344---426.
5.Moreira D, Marmelo B, Delgado A, et al. A decisão de não revascularizar o enfarte agudo do miocárdio sem
supradesnivelamento de ST--- condicionantes e prognóstico. Arealidadenacional.RevPortCardiol.2015;34:315---28.
6.AntmanEM,CohenM,BerninkPJ,etal.TheTIMIriskscorefor unstableangina/non-ST-elevationMI.Amethodfor prognostica-tionandtherapeuticdecisionmaking.JAMA.2000;284:835---42.
7.MorrowDA,AntmanEM,CharlesworthA,etal.TIMIriskscore forST-elevationmyocardialinfarction:aconvenient,bedside, clinicalscoreforriskassessmentatpresentation.Circulation. 2000;102:2031---7.
8.GrangerCB,GoldbergRJ,DabbousO,etal.Predictorsof hos-pitalmortalityintheglobalregistryofacutecoronaryevents. ArchInternMed.2003;163:2345---53.
9.EagleKA, LimMJ,DabbousOH,et al.Avalidatedprediction modelforallformsofacutecoronarysyndromes:estimatingthe riskof6-monthpostdischargedeathinaninternationalregistry. JAmMedAssoc.2004;291:2727---33.
10.YanAT,YanRT,HuynhT,etal.Understandingphysicians’risk stratificationofacutecoronarysyndromes:insightsfrom the CanadianACSIIRegistry.ArchInternMed.2009;169:372---8.
11.BagnallAJ,GoodmanSG,FoxKA,etal.Optimalmedical ther-apyfornon-ST-elevationacutecoronarysyndromes:exploring whyphysiciansdonotprescribeevidence-basedtreatmentand whypatientsdiscontinuemedicationsafterdischarge.Cir Car-diovascQualOutcomes.2010;3:530---7.
12.TimóteoAT,PapoilaAL,LopesJP,etal.Isitpossibletosimplify riskstratificationscoresforpatientswithST-segmentelevation
myocardialinfarctionundergoingprimaryangioplasty?RevPort Cardiol.2013;32:967---73.
13.HuynhT,KrouzS,YanA,etal.CanadaAcuteCoronarySyndrome RiskScore:anewriskscoreforearlyprognosticationinacute coronarysyndromes.AmHeartJ.2013;166:58---63.
14.Gonc¸alves PA, Ferreira J, Aguiar C, et al. TIMI, PURSUIT, and GRACErisk scores:sustained prognosticvalueand inter-action with revascularization in NSTE-ACS. Eur Heart J. 2005;26:865---72.
15.FerreiraSantosJ,AguiarC,GavinaC,etal.RegistoNacional deSíndromesCoronáriasAgudas:seteanosdeactividadeem Portugal.RevPortCardiol.2009;28:1465---500.
16.ThygesenK,AlpetJS,JaffeAS,etal.Thirduniversaldefinition ofmyocardialinfarction.EurHeartJ.2012;33:2551---67.
17.CollinsGS, ReitsmaJB,AltmanDG,etal. Transparent repor-tingofamultivariablepredictionmodelforindividualprognosis or diagnosis (TRIPOD). The TRIPOD statement. Circulation. 2015;131:211---9.
18.Pieper KS, Gore JM, Fitzgerald G, et al. Validity of a risk-predictiontool for hospital mortality:theGlobal Registryof AcuteCoronaryEvents.AmHeartJ.2009;157:1097---105.
19.SansS,KestelootH,KromhoutD.Theburdenofcardiovascular diseasesmortalityinEurope.EurHeartJ.1997;18:1231---48.
20.D’AgostinoR, Grundy S,Sullivan LM,etal. Validationofthe Framinghamcoronaryheartdiseasepredictionscores:resultsof amultipleethnicgroupsinvestigation.JAMA.2001;286:180---7.