www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
ORIGINAL
ARTICLE
Frequency
of
overweight
and
obesity
in
children
and
adolescents
with
autism
and
attention
deficit/hyperactivity
disorder
Arthur
Kummer
a,∗,
Izabela
Guimarães
Barbosa
a,
David
Henrique
Rodrigues
b,
Natália
Pessoa
Rocha
b,
Marianna
da
Silva
Rafael
b,
Larissa
Pfeilsticker
b,
Ana
Cristina
Simões
e
Silva
b,
Antônio
Lúcio
Teixeira
baFaculdadedeMedicina,UniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil bUniversidadeFederaldeJuizdeFora(UFJF),GovernadorValadares,MG,Brazil
Received12March2015;accepted16June2015 Availableonline28December2015
KEYWORDS
Attentiondeficitand hyperactivity disorder;
Austisticdisorder; Pediatricobesity; Overweight
Abstract
Objective: Toassessthefrequencyofoverweightandobesityinchildrenandadolescentswith autismspectrumdisorder(ASD)andwithattentiondeficit/hyperactivitydisorder(ADHD)and theirparents,incomparisonwithchildrenandadolescentswithoutdevelopmentaldisorders. Methods: Anthropometricmeasureswereobtainedin69outpatientswithASD(8.4±4.2years old), 23 with ADHD (8.5±2.4) and 19 controls without developmental disorders (8.6±2.9) between AugustandNovember2014. Parentsofpatientswith ASDandADHD alsohadtheir anthropometricparameterstaken.Overweightwasdefinedasapercentile≥85;obesityasa percentile≥95;andunderweightasapercentile≤5.Foradults,overweightwasdefinedasa BMIbetween25and30kg/m2andobesityasaBMIhigherthan30kg/m2.
Results: ChildrenandadolescentswithASDandADHDhadhigherBMIpercentile(p<0.01)and z-score(p<0.01)thancontrols,andincreasedfrequencyofoverweightandobesity(p=0.04). Patients withASD andADHD didnot differbetween them inthesevariables,norregarding abdominal circumference. Parents of children with ASD and ADHD did not differ between themselves.
Conclusions: ChildrenandadolescentswithASDandADHDareatahigherriskofoverweight andobesitythanchildrenwithoutdevelopmentalproblemsinthecommunity.
©2015SociedadedePediatriadeSãoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(https://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:r2kummer@hotmail.com(A.Kummer). http://dx.doi.org/10.1016/j.rppede.2015.12.006
PALAVRAS-CHAVE
Transtornododéficit deatenc¸ãoe hiperatividade; Transtornoautístico; Obesidade
pediátrica; Sobrepeso
Frequênciadesobrepesoeobesidadeemcrianc¸aseadolescentescomautismoe transtornododéficitdeatenc¸ão/hiperatividade
Resumo
Objetivo: Avaliar a frequência de sobrepeso e obesidade em crianc¸as e adolescentescom transtorno doespectro doautismo (TEA)e transtorno dodéficit de atenc¸ão/hiperatividade (TDAH) e em seus pais, em comparac¸ão com crianc¸as e adolescentesda comunidade sem transtornosdodesenvolvimento.
Métodos: Medidasantropométricasforamcoletadasde69pacientescomTEA(8,4±4,2anos), 23 com TDAH (8,5±2,4) e19 controlessem transtornos desenvolvimentais(8,6±2,9)entre agostoe novembrode 2014.Ospaisdos pacientescomTEAeTDAH tambémforam avalia-dosemrelac¸ãoaosparâmetrosantropométricos.Sobrepesofoidefinidocomopercentil≥85; obesidadecomopercentil≥95;ebaixopesocomopercentil≤5.Paraosadultos,sobrepesofoi definidocomoIMCentre25e30kg/m2eobesidade,IMCacimade30kg/m2.
Resultados: Crianc¸as e adolescentes comTEA e TDAH exibirammaior percentil (p<0,01) e escore-z(p<0,01) doIMC em relac¸ão aoscontroles, bemcomo frequência maiselevada de sobrepesoeobesidade(p=0,04).OspacientescomTEAeTDHAnãodiferiramentresiquanto aessasvariáveisouquantoàcircunferênciaabdominal.Ospaisdascrianc¸ascomTEAeTDAH tambémnãodiferiramentresi.
Conclusões: Crianc¸aseadolescentescomTEAeTDAHestãoemmaiorriscodetersobrepesoe obesidadeemrelac¸ãoacrianc¸asdacomunidadesemproblemasdodesenvolvimento.
©2015SociedadedePediatriadeSãoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Prevalenceofoverweightandobesityindevelopedcountries isalarmingandreaches31.8%ofchildrenandadolescents.1
IntheUS,despitecontinuedeffortstoreducethesepublic
healthproblems,rateshavebeenstableinthelastdecade.1
InBrazil,epidemiologicalstudieshaveshownan increased
frequency of overweight and obesity in this age group.2,3
Comparison of the 1989 National Survey on Health and
Nutrition(PNSN)andthe2008---2009ConsumerExpenditure
Surveyshowsthatoverweightfrequencyinchildrenbetween
fiveandnineyearsoldincreasedfromabout9---33%.3
Internationalstudieshavefoundanassociationbetween
overweight/obesity and psychiatric disorders in children,
such as autism spectrum disorder (ASD) and
atten-tion deficit/hyperactivity disorder (ADHD). Nevertheless,
whetherthisassociationischaracteristicofASDandADHDor
commontobehavioralanddevelopmentalproblemsin
gen-eralremainsunclear.Furthermore,theassociationislikely
tobe bidirectional;that is, not only behavioral problems
mayleadtoobesity,butobesitymaybeariskfactorforthe
developmentofbehavioralanddevelopmentalproblems.4
Moststudiesofthenutritionalstatusofyoungpeopleand
adultswithADHDreportsahighfrequencyofoverweightand
obesity,aswellasameanbodymassindex(BMI)higherin
patientswithADHDcomparedtocontrolswithout
develop-mentaldisorders.5---7 The frequency of obesity is higherin
adultswithADHD thanin adultswithchildhoodADHD
his-tory,butwhosesymptomsremittedinadulthood.8Similarly,
obeseyoungpeoplealsohave higherfrequencyof ADHD.5
Furthermore,behavioralproblemssuchasADHDhinder
obe-sitytreatment.9
Similarly,studiesalsoreportedthatchildrenand
adoles-centswithASDaremoreoftenoverweightandobese.10---13
In ASD, weight changes have been associated with sleep
disorders,10,11 older age,11 and using food as a reward,12
amongothers.Inaddition,parentsofchildrenwithautism
are also more frequently obese.14 These factors suggest
a complex interaction between genetic, molecular, and
behavioralfactors.
Despitethesealarmingdata,therearenostudiesofthe
nutritionalstatusofchildrenwithASDandADHDinBrazil.
Inaddition,fewstudieshavecomparedtheBMIand/orthe
overweightfrequencyindifferentdevelopmentaldisorders.
In this context, the aim of this study wasto evaluate
the frequency of overweight and obesity in children and
adolescentswithASDandADHDandtheirparents.
Method
Childrenandadolescents seenin theoutpatientclinics of ASD(n=69)andAttentionDeficit(n=23)ofthePsychiatry Ser-viceoftheHospitaldasClinicas,FederalUniversityofMinas Gerais(UFMG),Brazil,andtheirparentswereinvitedto par-ticipateinthisstudy.DatawerecollectedbetweenAugust andNovember2014,andnoneofthoseinviteddeclinedto participate.AllpatientswithASDandADHDmetthe diag-nostic criteriaof the DSM-5.15 It wasconsidered thegold
standard.PatientsinASDgrouphadnoADHDascomorbidity
andvice versa.Noteworthy,some patientswithASDwere
taking methylphenidate, but medicalrecords information
indicatedthatitsusewasfor‘‘disruptivebehavior’’’(e.g.,
heteroorself-aggressiveness).Thecontrolgroup(n=19)
development, recruited from the local community. The
study wasapproved bythe Research EthicsCommitteeof
UFMGandallparticipantsand/orlegalguardiansgavetheir
writteninformedconsentbeforeenteringthestudy.
Patientsandcontrolswereinterviewedusingastructured
questionnairetocollectdemographic(ageandsexofchild
andguardians) andclinical data.Parents ofchildren with
ASDresponded totheinventorySocialandCommunication
Disorders Checklist(SCDC)16 and parents of children with
ADHD respond to the Swanson, Nolan, and Pelham scale
--- version IV(SNAP-IV).17 SCDC is a self-completion
ques-tionnaire with 12 questions that assesses the severity of
behaviorsrelatedtoautisminthelastsixmonths.16
SNAP-IVis aself-administeredinstrumentthat,in itsversionof
26 items, evaluates the severity of inattentive,
hyperac-tive/impulsive,andopponent/defiantbehavior.17
All subjects included in the study had their weight
(kg) and height (m) measured at the time of interview.
BMI was calculated using the formula: weight (expressed
in kg) divided by height (expressed in meters) squared
(kg/m2).Ageandsex-specificBMIz-scoreandpercentilesof
patientsandcontrolswerecalculatedusingCDC2000growth
charts.18Overweightwasdefinedasapercentile≥85;
obe-sity asa percentile≥95; andunderweightasa percentile
≤5.Foradults,overweightwasdefinedasBMIbetween25
and30kg/m2andobesityasBMIover30kg/m2.
Subjects werealsoevaluatedfor abdominal
circumfer-ence,whichwasalsoconvertedintopercentilesaccordingto
CDC 2007---2010 graphics.19 Anthropometricmeasurements
weretakenwithparticipantsinlightclothesandbarefoot,
using a portable digital scale, wall mounted stadiometer,
andinelastictapemeasure.Waistcircumferencewas
mea-suredovertheskinintheupperpartofthelateralborder
oftherightiliumandattheendofnormalexpiration,and
thenearestmillimeterwasrecorded.20
Statistical analyzes were performed using SPSS
soft-wareversion22.0(SPSSInc.,Chicago,IL,USA).Descriptive
statisticswere usedtopresent the sociodemographic and
clinicalcharacteristicsofthesample.Associationbetween
dichotomous variables was assessed with Pearson’s
chi-square or Fisher’s exact test, as appropriate. Continuous
variables were expressed as mean and standard
devia-tion.Allvariablesweretestedfornormaldistributionusing
the Shapiro---Wilk test and no data had a normal
distri-bution. Therefore, the differences between groups were
compared using the Mann---Whitney test or Kruskal---Wallis
test, asappropriate.Correlations were investigatedusing
theSpearmancoefficient.Allp-valuesweretwo-tailedand
thesignificancelevelofp<0.05wasused.
Results
There was prevalence of male in the ASD (86.9%), ADHD (78.9%),and control (86.9%) groups. There wasno statis-ticallysignificantdifferencebetweengroups(p=0.66).Also, therewasnodifferenceinagebetweenindividualswithASD (8.4±4.2;range:2---18years),ADHD(8.5±2.4;range:5---15 years),andcontrols(8.6±2.9;range:5---15years)(p=0.603). Ageandsex-specificBMIz-scoreandpercentilesof con-trolsweresignificantlylowerthanthoseofpatientswithASD andADHD(Table1).Similarfindingswereseenwhengroups
werecomparedregardingweightchangeproportions,with
higherpercentageofoverweightandobesityinbothgroups
ofpatients(ASDandADHD)comparedwiththecontrolgroup
(Table1).On theotherhand,therewasnosignificant
dif-ferencebetweenpatientswithADHDandASDinanyofthe
comparisons(Table1).Regardingwaistcircumference
per-centile,groupswithASD(56.4±29.9)andADHD(65.0±18.3)
alsodidnotdiffer(p=0.453).
The severity of ADS symptoms did not correlate with
anthropometric measurements (Table 2). In ADHD group,
the BMI percentile correlated negatively with the
sever-ityof oppositionanddefiance symptomsofandtherewas
nocorrelationwithinattentionorhyperactivity/impulsivity
symptoms.
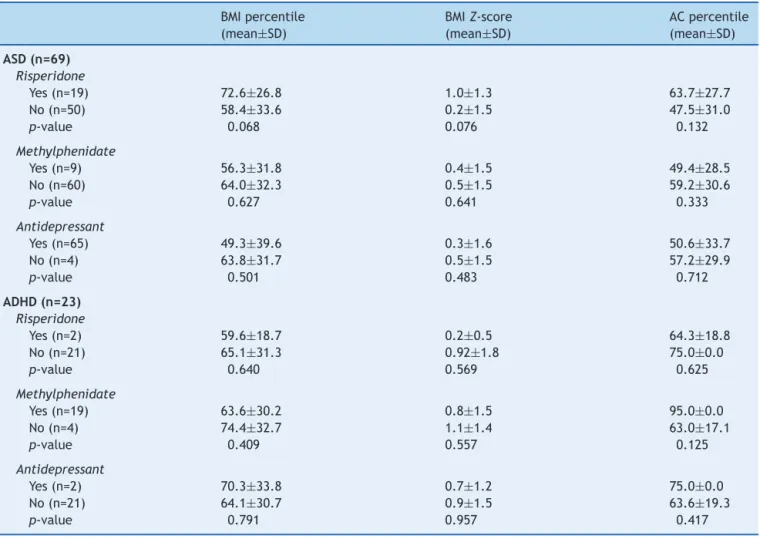
OfADHDpatients,20(87%)weretakingpsychiatricdrugs
(Table3).AmongASDpatients,26(37.7%)weretaking
psy-chiatric drugs. In ASD group, therewas a tendency for a
higher percentage of BMI (p=0.06) in participants taking
risperidone. Of the 21 participants taking risperidone, 5
(23.8%)ofguardiansspontaneouslyreportedseen a
signifi-cantincreaseinappetiteafterdruginitiation.Ofthetotal
28participantsinuseofmethylphenidate,whenfacedwith
anopenquestiononsideeffects,13(44.8%)guardians
spon-taneouslyreportedthattherewasasignificantdecreasein
appetitewiththedrug.
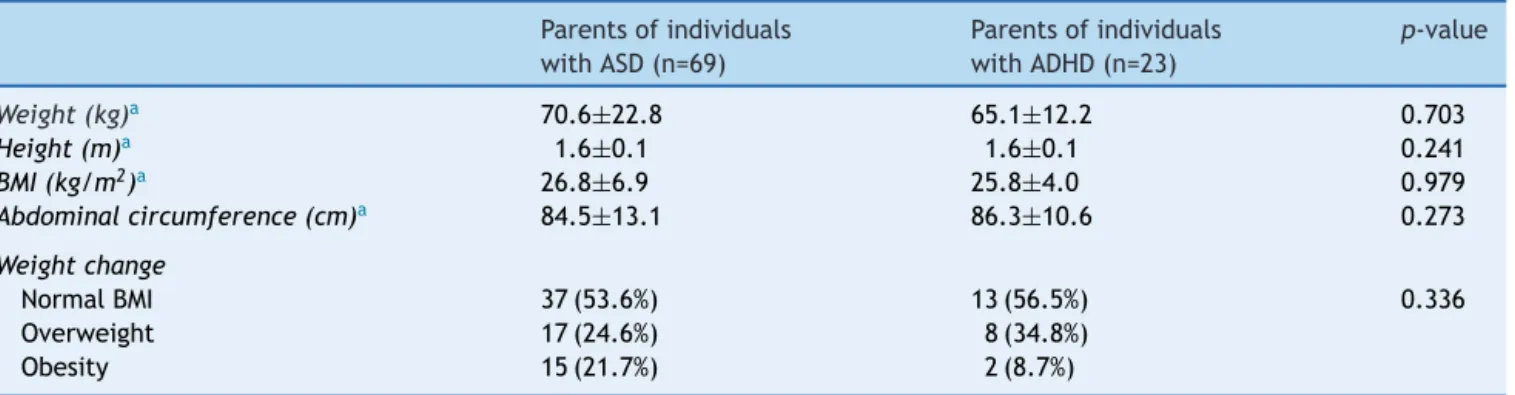
Parentsofparticipants withASDandADHD didnot
dif-ferwithrespecttoanthropometricmeasurements(Table4).
Therewas also nosignificant difference between parents
of individuals with ASDand ADHD regarding frequency of
overweightandobesity(p=0.34).
Table1 Comparisonofbody massindex(BMI) andweightchangebetween individualswithattentiondeficit/hyperactivity disorder(ADHD)andautismspectrumdisorder(ASD)andcontrols.
Controls(n=19) ADHD(n=23) ASD(n=69) p-value
BMIpercentilea 35.8±28.5 64.6±30.2 62.9±32.0 0.006
BMIZ-scorea −0.55±1.13 0.87±1.42 0.49±1.51 0.002
Weightchanges 0.044
Underweight 21.0% 0.00% 6.7%
Normal 73.7% 65.2% 53.3%
Overweight 0.00% 17.5% 18.3%
Obesity 5.3% 17.4% 21.7%
BMI,bodymassindex.Boldindicatesp-valuesignificantat<0.05.
Table2 Correlationofclinicalfeatureswithbodymassindex(BMI)andwaistcircumferenceinindividualswithautismspectrum disorder(ASD)andattentiondeficit/hyperactivitydisorder(ADHD).
BMIpercentile BMIZ-score ACpercentile
ASD(n=69)
SCDC
Correlationcoefficient 0.059 0.062 −0.009
Sig.(2tailed) 0.727 0.717 0.960
ADHD(n=23)
SNAP-I
Correlationcoefficient −0.200 −0.251 −0.667
Sig.(2tailed) 0.555 0.457 0.219
SNAP-HI
Correlationcoefficient −0.230 −0.331 0.803
Sig.(2tailed) 0.496 0.320 0.102
SNAP-OD
Correlationcoefficient −0.621 −0.370 0.410
Sig.(2tailed) 0.041 0.263 0.493
AC,abdominalcircumference;SCDC,Social andCommunicationDisordersChecklist; SNAP-I,SNAP-IVinattentionsubscale; SNAP-HI, SNAP-IVhyperactivitysubscale;SNAP-OD,SNAP-IVoppositionanddefiancesubscale.Boldindicatesp-valuesignificantat<0.05.
Table3 Analysis ofassociationsbetween druguse andbody massindex(BMI)andwaistcircumferenceinindividualswith autismspectrumdisorder(ASD)andattentiondeficit/hyperactivitydisorder(ADHD).
BMIpercentile (mean±SD)
BMIZ-score (mean±SD)
ACpercentile (mean±SD)
ASD(n=69)
Risperidone
Yes(n=19) 72.6±26.8 1.0±1.3 63.7±27.7
No(n=50) 58.4±33.6 0.2±1.5 47.5±31.0
p-value 0.068 0.076 0.132
Methylphenidate
Yes(n=9) 56.3±31.8 0.4±1.5 49.4±28.5
No(n=60) 64.0±32.3 0.5±1.5 59.2±30.6
p-value 0.627 0.641 0.333
Antidepressant
Yes(n=65) 49.3±39.6 0.3±1.6 50.6±33.7
No(n=4) 63.8±31.7 0.5±1.5 57.2±29.9
p-value 0.501 0.483 0.712
ADHD(n=23)
Risperidone
Yes(n=2) 59.6±18.7 0.2±0.5 64.3±18.8
No(n=21) 65.1±31.3 0.92±1.8 75.0±0.0
p-value 0.640 0.569 0.625
Methylphenidate
Yes(n=19) 63.6±30.2 0.8±1.5 95.0±0.0
No(n=4) 74.4±32.7 1.1±1.4 63.0±17.1
p-value 0.409 0.557 0.125
Antidepressant
Yes(n=2) 70.3±33.8 0.7±1.2 75.0±0.0
No(n=21) 64.1±30.7 0.9±1.5 63.6±19.3
p-value 0.791 0.957 0.417
Table4 Anthropometricdata andfrequencyofweightchangeofparentsofindividualswithattentiondeficit/hyperactivity disorder(ADHD)andautismspectrumdisorder(ASD).
Parentsofindividuals withASD(n=69)
Parentsofindividuals withADHD(n=23)
p-value
Weight(kg)a 70.6±22.8 65.1±12.2 0.703
Height(m)a 1.6±0.1 1.6±0.1 0.241
BMI(kg/m2)a 26.8±6.9 25.8±4.0 0.979
Abdominalcircumference(cm)a 84.5±13.1 86.3±10.6 0.273
Weightchange
NormalBMI 37(53.6%) 13(56.5%) 0.336
Overweight 17(24.6%) 8(34.8%)
Obesity 15(21.7%) 2(8.7%)
BMI,bodymassindex.
a Valuesareexpressedasmean±standarddeviation.
Discussion
Overweightandobesity arepublichealth problems in the generalpopulation.Theincidenceofmanychronicdiseases inadulthoodisdirectlyrelatedtochildhoodobesity.1
Obe-sity increases the risk of children having short and long
termhealthproblems,suchasdiabetes,cardiovascularand
psychosocial diseases. International studies indicate that
childrenandadolescentswithASDandADHDmaybe
particu-larlyvulnerabletosuchweightchanges.4---13Thisworkshows
thatBrazilianchildrenandadolescentswithASDandADHD
also appear tobe more proneto overweight and obesity
comparedtothegeneralpopulation.
Few Brazilian studies have investigated this issue.
Domingues evaluated 30 children in a special school of
CampoGrandeandfoundthatfour(13.3%)wereobeseand
seven(23.3%)wereunderweight.21Emidioetal.evaluated
23 autisticchildren andadolescentsand foundthat three
(13%)wereunderweight,five(21.7%)wereoverweight,and
six(26.1%)wereobse.22Althoughbothstudiesindicatehigh
ratesofoverweightandobesityinchildrenandadolescents
withASD,theabsenceofacontrolgroupsignificantlylimited
theinterpretationofthefindings.
Nascimento et al.found nodifferencein frequency of
overweight amongchildren andadolescents with
‘‘ADHD-indicative’’ and controls, or when comparing the BMI of
boththegroups.23Alimitationofthisstudyistheinclusion
of children with only ‘‘ADHD-indicative’’, without a
con-firmeddiagnosisofthedisorder.Moreover,thestudydidnot
properlysetthevariable‘‘overweight’’,aswellasdirectly
compared theBMI of the two groups, instead of
compar-ingthe adjusted percentilefor age.In contrast,Paranhos
et al. reported that all 70 children and adolescents with
ADHDevaluatedattheUniversityHospitalofBrasiliawere
eutrophic.24 However, this study also did not adequately
definedtheweightchange and didnotusethe percentile
variableand/ortheageandsex-specificBMIz-scores.
TherearefewpublishedstudiesthatcomparedBMIand
frequency of overweight/obesity between developmental
disorders. Curtin et al. performed a review of medical
records of children and adolescents in care in a tertiary
centerforneuropsychiatricdisordersandfoundafrequency
ofoverweight andobesity of,respectively, 29%and17.3%
in ADHD patients and 35.7% and 19% in ASD patients.25
The Curtin study limitation is that anthropometric
mea-surementswereobtainedfrommedicalrecords,therewas
no standardization in the form of data collection.
More-over,therewasnocontrol groupor comparisons between
groups. Chenet al.evaluated only thefrequency of
obe-sity (BMI ≥95th percentile) in children and adolescents
withchronicdesases(physical,developmental,and
behav-ioral) and found frequency of 23.4% in ASD patients and
18.9% in ADHD patients.26 The study by Chen et al. also
hasa number of limitations, such asusing data fromthe
NationalSurveyofChildren’sHealth(NSCH2003),inwhich
allinformationwascollectedbytelephone;thepossibility
ofhavingthesameparticipantwithcomorbiditiesincluding
ASDandADHDatthesametime;andnostatistical
calcula-tionforcomparisonbetweengroups.Morerecently,Philips
etal. useddata fromthe National Health Interview
Sur-vey(2008---2010)tocomparethefrequencyofunderweight,
overweight,andobesityinadolescentswithvarious
devel-opmentaldisorders.13 Obesityandunderweight weremore
commonin allneurodevelopmentaldisorders,but the
fre-quency of obesity was particularly high in the subgroup
withASD(31.8%),whereaspatientswithADHDhadalower
prevalence(17.6%).Thefrequencyofoverweightwas
simi-larbetweenthegroupswithdevelopmentaldisorders(ASD:
20.9%;ADHD:18.0%)andchildrenwithtypicaldevelopment
(18.2%).Thestudyshouldalsobeinterpretedwithcaution
becauseofitslimitations,includingthemedicaland
anthro-pometricdatacollectiononlybyinterviewingtheguardians;
non-pairingbysexbetweenthecontrolandASDandADHD
groups,therewasprevalenceoffemaleadolescentsinthe
control group13; and the high frequency of comorbidities
between ASD and ADHD (60% of ASD patients also had
ADHD).
Acommonlimitationofmanystudiesofweightchanges
inpeoplewithASDandADHDis thattheauthors useonly
theBMIasbase.Suchanapproachdoesnotallowthedirect
measurement of body composition and/or distribution of
bodyfat,theremaybeincreasedBMIbecauseofincreased
musclemass.Waistcircumferencemeasurementiseasy to
obtainandcanindicatethe presenceofvisceral adiposity
inchildren.27Inthiscontext,thepresentstudyshowedthat
groupswithASDandADHDdidnotdifferfromeachotheror
inrelationtoBMI(highcomparedtocontrol)norinrelation
TheseverityofASDandADHDsymptomsdidnot
corre-latewithweightchange.However,oppositionanddefiance
symptomsnegativelycorrelatedwithBMIpercentileinADHD
participants. Korczak et al. noted that ADHD could
pre-dictobesitylaterinlife,butaccordingtotheauthorsthis
associationwouldbecompletelyexplainedbythepresence
of behavior disorder in childhood.28 Although
opposition-defianceandbehaviorsymptomsareoftencorrelated,this
seeminglydiscrepantfindingraisesthequestionofwhether
these conditions may have differential effect on feeding
behavior(e.g.,refusaltoeatandfrequenttantrumsrelated
tofoodintheopponent-defiantdisorder).
Consistent with the medical literature, there was a
trend towards the association of risperidone intake and
higherBMI percentile in ASD patients. Increasedappetite
and metabolic alterations are common side effects of
risperidone.20Interestingly,althoughtheparentsofchildren
takingmethylphenidatehave reporteddecreasedappetite
withthissubstance,thiswasnotreflectedinlowerBMIin
ADHDchildren. Itwasnotpossible tocomparethe BMIof
ADHDchildrentakingornottakingmethylphenidatebecause
almostallofthemweretakingthisdrug.However,although
methylphenidatecommonsideeffectisdecreasedappetite,
otherstudieshavefoundnodifferenceinBMIbetweenADHD
childrenreceivingornotmethylphenidate.6,7
Finally,itwasseenforthefirsttimeintheliteraturethat
parentsofchildrenwithASDandADHDdidnotdifferinBMI,
waistcircumference,andfrequencyofoverweight/obesity.
Although nearly half of parents are overweight/obese,
unfortunatelyitwasnotpossibletocomparethemwiththe
controlgroupbecausethechildrenandadolescentsofthe
controlgroup were examined at school without the
pres-ence of their parents. Some studies suggest that obesity
in parents is a risk factor for ASD and ADHD. However,
more investigations are needed to assess factors
under-lyingthis possible association, suchasgenetic/epigenetic
influence, family habits, inflammatory changes resulting
fromobesity duringgametogenesis and pregnancy, among
others.14,29
Theseresultsshouldbeinterpretedwithcaution.Dueto
itscross-cuttingnature,onecannotinfercausalitybetween
ASD,ADHD,andhigherfrequencyofoverweightandobesity.
Furthermore,thisstudyincluded arelativelysmall
conve-niencesampleof ADHDpatientsandcontrols. Allpatients
were recruited froma singletertiary center where more
complexcaseswithmorepronouncedsymptomsofADHDand
ASDareusuallytreated,whichcouldcompromisethe
exter-nalvalidityofthestudy.Moreover,therewereasignificant
proportion of underweight children in the control group,
which highlighted a peculiarity of the sample involved in
this work. The lack of waist circumference measurement
in the controls and anthropometricmeasurement in their
parentsis alsoa limitation thatshould bementioned. On
the other hand, consecutive sampling, direct and careful
measurementofanthropometricparametersofpatientsand
communitycontrolswithoutdevelopmentaldisorders,
diag-nosisandevaluationofpatientsbyexperiencedclinicians,
sample matched bygender and age, andthe exclusionof
comorbidcasesofADHDandASDarestrengthsofthestudy
thatshouldbehighlighted.
Insummary,thisstudyshowedthatchildrenand
adoles-centswithASDandADHDfollowed-upinoutpatientclinics
areat increasedriskof overweightandobesitythan their
typicallydeveloping peers. Drugssuch asrisperidonemay
havesomecausalroleandpatientstakingthesesubstances
requireclose monitoringfor metabolic changes.However,
geneticandenvironmentalfactors(e.g.,pooreatinghabits
and sedentary lifestyle) should also be considered. We
emphasizethatobesityandoverweightaregeneralrisk
fac-torsfordisordersandresponsibleforworseningthequality
oflife.Thus,itisveryimportantthatphysiciansroutinely
assesstheweightoftheirpatientswithASDandADHDand
givethemadvisesonhealthylivinghabits.
Funding
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brasil - 304272/2012-4), Fundac¸ão de Amparo à Pesquisa do Estado de Minas Gerais (Fapemig, Brasil - APQ-04625-10), and Coordenac¸ão de Aperfeic¸oamento de Pessoal de Nível Superior (Capes, Brasil).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
Dr.IGBarbosareceivedpostdoctoralscholarshipfromCapes (Capes/DBP/CEX/PNPDNo.2039-58/2013).
References
1.OgdenCL,CarrollMD,KitBK,FlegalKM.Prevalenceof child-hoodandadultobesityintheUnitedStates,2011---2012.JAMA. 2014;311:806---14.
2.FloresLS,GayaAR,PetersenRD,GayaA.Trendsofunderweight, overweight,andobesityinBrazilianchildrenandadolescents. JPediatr(RioJ).2013;89:456---61.
3.PimentaTA,RochaR.AobesidadeinfantilnoBrasil:umestudo comparativoentreaPNSN/1989eaPOF/2008-09entrecrianc¸as de5 a9anos deidade.FIEPBull Online.2012;82.Available from: http://www.fiepbulletin.net/index.php/fiepbulletin/ article/view/2224[accessed02.04.15].
4.Khalife N, Kantomaa M, Glover V, Tammelin T, Laitinen J, EbelingH,etal.Childhoodattention-deficit/hyperactivity dis-order symptoms are risk factors for obesity and physical inactivityinadolescence.JAmAcadChildAdolescPsychiatry. 2014;53:425---36.
5.Cortese S, Vincenzi B. Obesity and ADHD: clinicaland neu-robiological implications. Curr Top Behav Neurosci. 2012;9: 199---218.
6.Holtkamp K, Konrad K, Müller B, Heussen N, Herpertz S, Herpertz-DahlmannB,et al.Overweight and obesity in chil-drenwithattention-deficit/hyperactivitydisorder.IntJObes RelatMetabDisord.2004;28:685---9.
7.FliersEA,BuitelaarJK,MarasA,BulK,HöhleE,FaraoneSV, etal.ADHDisariskfactorforoverweightandobesityin chil-dren.JDevBehavPediatr.2013;34:566---74.
9.Cortese S, Castellanos FX. The relationship between ADHD and obesity:implications for therapy. ExpertRev Neurother. 2014;14:473---9.
10.ZuckermanKE,HillAP,GuionK,VoltolinaL,FombonneE. Over-weightandobesity:prevalenceandcorrelatesinalargeclinical sampleofchildrenwithautismspectrumdisorder.JAutismDev Disord.2014;44:1708---19.
11.Broder-Fingert S, Brazauskas K, Lindgren K, Iannuzzi D, Van Cleave J. Prevalence of overweight and obesity in a large clinicalsample of children withautism. Acad Pediatr. 2014;14:408---14.
12.BandiniL,CurtinC,AndersonS,Philips S,MustA. Foodasa rewardand weight statusin children with autism. FASEBJ. 2013;27:1063---111.
13.PhillipsKL, SchieveLA, VisserS,BouletS,Sharma AJ,Kogan MD, et al. Prevalence and impact of unhealthy weight in a national sampleof US adolescents withautism and other learning and behavioral disabilities. Matern Child Health J. 2014;18:1964---75.
14.SurénP,GunnesN,Roth C,BresnahanM,HornigM,Hirtz D, etal.Parentalobesity and riskofautismspectrumdisorder. Pediatrics.2014;133:e1128---38.
15.AmericanPsychiatricAssociation.ManualDiagnósticoe Estatís-tico de Transtornos Mentais. 5th ed. (DSM-5) Porto Alegre: ArtmedEditora;2014.
16.SkuseDH,MandyWP,ScourfieldJ.Measuringautistictraits: heri-tability,reliability,andvalidityoftheSocialandCommunication DisordersChecklist.BrJPsychiatry.2005;187:568---72. 17.MattosP,Serra-PinheiroMA,RohdeLA,PintoD.Apresentac¸ão
deumaversãoemportuguêsparausonoBrasildoinstrumento MTA-SNAP-IVdeavaliac¸ãodesintomasdetranstornododéficit deatenc¸ão/hiperatividadeesintomasdetranstornodesafiador edeoposic¸ão.RevPsiquiatrRS.2006;28:290---7.
18.KuczmarskiRJ,OgdenCL,GuoSS,Grummar-StrawnLM,Flegal KM,MeiZ,etal.2000CDCgrowthchartsfortheUnitedStates: methodsanddevelopmentNationalCenterforHealthStatistics. VitalHealthStat.2002;11:1---19.
19.FryarCD,GuQ,OgdenCL.Anthropometricreferencedatafor childrenandadults:UnitedStates,2007---2010NationalCenter forHealthStatistics.VitalHealthStat.2012;22:11.
20.NationalHealth.NutritionExaminationSurvey.Anthropometry proceduresmanual.Atlanta:CDC;2007.
21.Domingues G. Relac¸ão entre medicamentos e ganho de peso em indivíduos portadores de autismo e outras sín-dromes relacionadas. Mato Grosso do Sul: Nutric¸ão Ativa; 2007.
22.Emidio PP, FagundesGE, Barchinski MC, Silva MA. Avaliac¸ão nutricional em portadores da síndrome autística. Nutrire. 2009;34:382.
23.Nascimento EM, Contreira AR, Silva EV, Souza LP, Beltrame TS.Desempenhomotoreestadonutricionalemescolarescom transtorno do déficit de atenc¸ão e hiperatividade. J Hum GrowthDev.2013;23:1---7.
24.ParanhosCN,AucelioCN,SilvaLC,PigossiM,VieiraNC,Silva TL, et al. Transtornode déficitde atenc¸ãoe hiperatividade (TDAH)---A avaliac¸ãodopadrãonoEEGeestadonutricional de crianc¸as eadolescentes de Brasília/DF. Pediatr Moderna. 2013;49:227---31.
25.CurtinC,BandiniLG,PerrinEC,TyborDJ,MustA.Prevalence ofoverweightinchildrenandadolescentswithattentiondeficit hyperactivitydisorderandautismspectrumdisorders:achart review.BMCPediatr.2005;5:48.
26.ChenAY,KimSE,Houtrow AJ,NewacheckPW. Prevalenceof obesityamongchildrenwithchronicconditions.Obesity(Silver Spring).2010;18:210---3.
27.Mantovani RM, Rios DR, Moura LC, Oliveira JM, Carvalho FF, Cunha SB, et al. Childhood obesity: evidence of an association between plasminogen activator inhibitor-1 levels and visceral adiposity. JPediatr Endocrinol Metab. 2011;24: 361---7.
28.Korczak DJ,LipmanE,Morrison K,Duku E,SzatmariP.Child andadolescentpsychopathologypredictsincreasedadultbody massindex: resultsfrom aprospective communitysample.J DevBehavPediatr.2014;35:108---17.