REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brSCIENTIFIC
ARTICLE
A
comparison
of
various
supraglottic
airway
devices
for
fiberoptical
guided
tracheal
intubation
Thomas
Metterlein
∗,
Anna
Dintenfelder,
Christoph
Plank,
Bernhard
Graf,
Gabriel
Roth
UniversitätsklinikumRegensburg,KlinikfürAnästhesiologie,Regensburg,Germany
Received17July2015;accepted22September2015 Availableonline26May2016
KEYWORDS
Difficultairway; Fibreopticintubation; Supraglotticairway device
Abstract
Background: Fiberopticalassistedintubationviaplacedsupraglotticairwaydeviceshasbeen describedassafeandeasyproceduretomanagedifficultairways.Howevervisualizationofthe glottisapertureisessentialforfiberopticalassistedintubation.Variousdifferentsupraglottic airwaydevicesarecommerciallyavailableandmightofferdifferentconditionsforfiberoptical assistedintubation.Theaimofthisstudywastocomparethebestobtainableviewoftheglottic apertureusingdifferentsupraglotticairwaydevices.
Methods:Withapprovalofthelocalethicscommittee52adultpatients undergoingelective anesthesiawererandomlyassignedtoasupraglotticairwaydevice(LaryngealTube,Laryngeal MaskAirwayI-Gel,LaryngealMaskAirwayUnique,LaryngealMaskAirwaySupreme,Laryngeal Mask AirwayAura-once). Afterstandardized induction ofanesthesiathesupraglotticairway devicewasplacedaccordingtothemanufacturersrecommendations.Aftersuccessful ventila-tionthepositionofthesupraglotticairwaydeviceinregardtotheglotticopeningwasexamined withaflexiblefiberscope.Afullyorpartiallyvisibleglotticaperturewasconsideredassuitable forfiberopticalassistedintubation.Suitabilityforfiberopticalassistedintubationwascompared betweenthegroups(H-test,U-test;p<0.05).
Results:Demographicdatawasnotdifferentbetweenthegroups.Placementofthesupraglottic airwaydeviceandadequateventilationwassuccessfulinallattempts.Glotticviewsuitablefor fiberopticalassistedintubationdifferedbetweenthedevicesrangingfrom40%forthelaringeal tube(LT),66%forthelaryngealmaskairwaySupreme,70%fortheLaryngealMaskAirwayI-Gel and90%forboththeLaryngealMaskAirwayUniqueandtheLaryngealMaskAirwayAura-once.
Conclusion:Noneoftheusedsupraglotticairwaydevicesofferedafullorpartialglotticviewin allcases.HowevertheLaryngealMaskAirwayUniqueandtheLaryngealMaskAirwayAura-once seemtobemoresuitableforfiberopticalassistedintubationcomparedtootherdevices. ©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:tom.metterlein@gmx.net(T.Metterlein). http://dx.doi.org/10.1016/j.bjane.2015.09.007
PALAVRAS-CHAVE
Viaaéreadifícil; Intubac¸ãoguiadapor fibraóptica;
Dispositivo supraglótico
Umacomparac¸ãodeváriosdispositivossupraglóticosparaintubac¸ãotraquealguiada
porfibraóptica
Resumo
Justificativa: A intubac¸ãoguiada porfibra óptica(IGFO)atravésdedispositivo supraglótico (DSG) tem sidodescritacomo um procedimentoseguro efácil parao manejodeviaaérea difícil. Noentanto,avisualizac¸ãodaaberturadagloteéessencial paraaIGFO.VáriosDSG diferentes estãocomercialmente disponíveise podem oferecer diferentescondic¸ões para a IGFO.Oobjetivodesteestudofoicompararamelhorvisãoobtidadaaberturadaglotecomo usodediferentesDSG.
Métodos: Comaaprovac¸ãodoComitêdeÉticalocal,52pacientesadultossubmetidosà aneste-siaeletivaforamrandomicamentedesignadosparaumDSG(tubolaríngeo(TL),máscaralaríngea (ML)I-Gel,MLUnique,MLSupreme,MLAura-once).Apósainduc¸ãopadronizadadaanestesia, o DSG foi colocadode acordocom asrecomendac¸ões do fabricante.Apósventilac¸ão bem-sucedida,aposic¸ãodoDSGemrelac¸ãoàaberturadaglotefoiexaminadacomumendoscópio flexível.Umaaberturadaglotetotalouparcialmentevisívelfoiconsideradacomoadequada paraaIGFO.Aadequac¸ãoparaaIGFOfoicomparadaentreosgrupos(teste-H,teste-U;p<0,05).
Resultados: Osdadosdemográficosnãoforamdiferentesentreosgrupos.AColocac¸ãodoDSGe aventilac¸ãoadequadaforambem-sucedidasemtodasastentativas.Avisãodagloteadequada paraaIGFOdiferiuentreosdispositivos,variandode40%paraoTL,66%paraaMLSupreme, 70%paraaMLI-Gele90%paraambasasmáscaraslaríngeasUniqueeAura-once.
Conclusão:NenhumdosDSGusadosofereceuumavisãototalouparcialdagloteemtodosos casos.Porém,asmáscaraslaríngeasUniqueeAura-onceparecerammaisadequadasparaaIGFO emcomparac¸ãocomosoutrosdispositivos.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Successfulairwaymanagementisaprimarygoalduring gen-eral anesthesiaas well as in many emergencysituations. Whiletrachealintubationisconsideredasgoldstandard,it requiresadequateskills.Thereisareportedincidenceof dif-ficultintubationrangingfrom0.05%to18%.1TheAmerican
SocietyofAnesthesiologists(ASA)TaskForceonManagement of the Difficult Airway therefore emphasizes the impor-tance of alternative, less invasive devices for adequate oxygenationincasetrachealintubationfails.2Thelaryngeal
maskairway(LMA)isexplicitlymentioned inthe2003ASA recommendations. Various alternative LMAs (Fig. 1) were marketedsincethen. Differentshapesandmaterials were usedtoachieveabetterairwayseal,lesspharyngealtrauma and facilitate proper placement. In 1999 another supra-glottic airway device (SAD), the laryngeal tube (LT) was introduced.3Itisasingle-lumentubewithoesophagealand
pharyngeal cuffs connected toa single inflation line with a ventral opening for ventilation between the two cuffs (Fig.1).3Afterblindinsertion,allSADsprovideapatent
air-wayinthemajorityofpatientsatfirstattempt.Thismakes SAD an interesting alternative in emergency medicine.4,5
The feasibility evenwithout extensive trainingprovides a simpletoolfor airwaymanagement.3 Accordingtovarious
airwaymanagementalgorithms emergencyoxygenationof thepatientcan beachievedby insertinga SADin caseof a failed intubation. Nevertheless in emergency situations trachealintubation isstillrequired toprotectthepatient fromaspiration.3,6Whenthereplacementofthesupraglottic
device by a tracheal tube is necessary, maximum patient safetymust beconsidered. The primarily inserted device isdedicatedtomaintainairwaypatencywhileother inter-ventions are prepared or take place.7 Ideally oxygen can
beprovidedthroughoutthetubeexchangeprocesstoavoid desaturation.
Various methods describe a safe replacement of the inserted SAD by a tracheal tube. Atherton described the blind insertion of a tube exchanger into the trachea via theplacedLMAwithaconsiderablesuccess rate.8Amore
sophisticated procedure was described by Hawkins et al. Toensureproperplacementofthetrachealtube,thetube exchangerisplacedunderfibre-opticguidance.9Avery
sim-ilarprocedurewaspublishedbyGenzwuerkeretal.usinga laryngealtubeasprimaryairway.Againthetubeexchanger wasplacedunderfibreopticguidanceandallowedthefast and easy placement of the tracheal tube.10 Success rate
ofthe fiberoptical assisted intubation (FAI)is significantly highercompared tothe blind insertion of a tube or tube exchanger.Thiscaneasilybeexplainedbythefrequent sub-optimalpharyngealpositionof theSAD.The distalorifices oftheSADandtheglotticaperturehavetobeinlineifthe SADisusedfortrachealintubation.
Figure1 Usedcommerciallyavailablesupraglotticairwaydeviceslefttoright(LT-D,i-Gel,Unique,Supreme,Aura-Once).
thepharyngealpositionof thecommerciallyavailable SAD variesconsiderably.
Aimof thisstudy wastoevaluatethe pharyngeal posi-tionofdifferentsupraglotticdevicesinrespecttotheglottis apertureandtheirpotentialfeasibilityasadedicatedairway forFAI.Ithasnotyetbeen systematicallyexaminedwhich devicesallowapropervisualizationoftheglotticaperture.
Methods
With approval of the local ethics committee 52 patients undergoing elective laser treatment for genital condylo-mas were examined by the three anesthesiologists (one 4thyear resident andtwo attendings).All three anesthe-siologistswerefamiliarwithandhadadequate experience with the used SADs. Glottic view between the different deviceswasthereforecomparedbetweenthelaryngealtube --- LT-D (VBM Medizintechnik GmbH, Sulz a.N., Germany), theI-GelLMA(Intersurgical,SanktAugustin,Germany),the LMAUnique(TeleflexMedicalGmbH,Kernen,Germany),the LMA Supreme (Teleflex Medical GmbH, Kernen, Germany) andtheLMA Aura-Once(AmbuGmbH, Bad Nauheim, Ger-many) (Fig. 1). After prior written consent the patients were randomized to a specific SAD using independently preparedenvelopesthatweredrawnrightbefore anesthe-sia. They received 7.5mg of midazolam orally one hour prior to surgery. Anesthesia was induced with Remifen-tanil (0.4g/kg/min) and Propofol (2.5mg/kg bolus and
0.1mg/kg/mincontinuousinfusion).Anesthesia depthwas monitoredand face-mask ventilation wasstarted at aBIS valuebelow40.ThesizeoftheSADwaschosenandinserted accordingtothemanufacturer’s recommendations.Before insertion, the cuffs were deflated and a water-soluble lubricant(InstruGel,Dr.DeppeLaboratorium,Kempen, Ger-many) was applied. After pharyngeal placement the cuff wasinflatedtoreachacuffpressureof20mmHg.Successful ventilationwasestablishedanda3.4mmflexiblefiberscope (10BS, Pentax,Hamburg, Germany) wasinserted intothe SADusingabronchoscopyadapterbyanexaminerblinded
tothedevice.Thebronchoscopewasadvancedtothe dis-tal orifice of the SAD and a picture of the best possible glotticviewwastaken.Duringtheexaminationanesthesia wasmaintainedwithcontinuousinfusionofremifentaniland propofol.Afterremovalofthefiberscopefurthercarewas providedaccordingtoourhospitalstandards.
The pictures of the glottic apertures were afterwards graded by anobserver blindedtothe device accordingto the following grading system, introduced by Brimacombe andBerry.11 (fullglottisview---I,glotticaperturepartially
visible --- II, glotticaperture notvisible ---III) (Fig. 2)Full andpartialviewoftheglotticaperturewereconsideredas suitableforfibreopticguidedtrachealintubation.
Alldataisgivenasmeanandinterquartilerange. Glot-ticvisualizationscoreswerecomparedbetweenthegroups using the Kruskal---Wallis-H-test and the Mann---Whitney-U -test with Win-STAT (R. Fitch Software, Bad Krozingen, Germany);p<0.05wasconsideredstatisticallysignificant.
100 90 80
70 60
50 40
30 20 10
0 LT (n=10)
i-Gel (n=10)
Supreme (n=12)
Unique (n=10)
Aura-I (n=10)
Suitable Not suitable
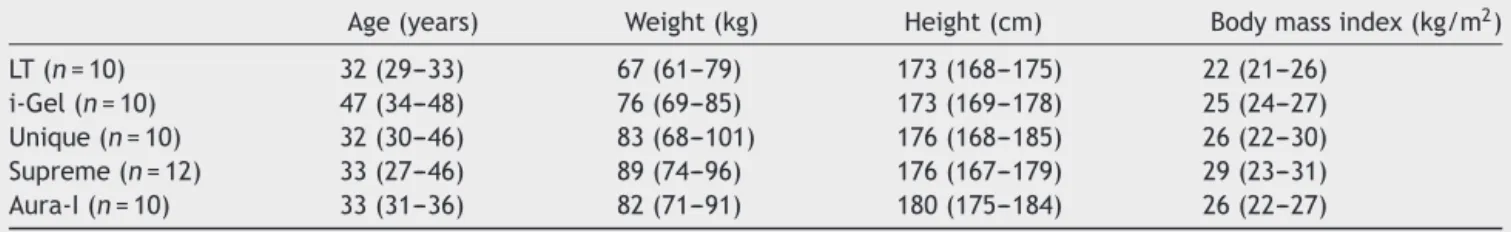
Table1 Demographicdataoftheexaminedpatients.Nodifferencebetweenthegroupswasobserved.Dataasmedianand interquartilerange.
Age(years) Weight(kg) Height(cm) Bodymassindex(kg/m2)
LT(n=10) 32(29---33) 67(61---79) 173(168---175) 22(21---26)
i-Gel(n=10) 47(34---48) 76(69---85) 173(169---178) 25(24---27) Unique(n=10) 32(30---46) 83(68---101) 176(168---185) 26(22---30) Supreme(n=12) 33(27---46) 89(74---96) 176(167---179) 29(23---31) Aura-I(n=10) 33(31---36) 82(71---91) 180(175---184) 26(22---27)
Table2 Glotticviewatthedistalapertureofthesupraglotticairwaydevice.
FullyvisibleI PartiallyvisibleII NotvisibleIII SuitableforFAI NotsuitableforFAI
LT(n=10) 3 1 6 4a 6
i-Gel(n=10) 7 3 7a 3
Unique(n=10) 9 1 9a 1
Supreme(n=12) 8 4 8a 4
Aura-I(n=10) 9 1 9a 1
a p<0.05significantdifferencebetweenLTandtheotherdevices.Nodifferencesbetweentheotherdevices.
Figure3 Glotticviewobtainedwiththefibrescopeantthedistalorificeofthesupraglotticairwaydevice.(A)Fullviewofthe aperture;(B)partialviewoftheaperture;(C)noobtainableviewoftheaperture.
Results
Demographic data(age,weight,height) wasnot different betweentheexaminedgroups(Table1).Placementofthe SADwassuccessfulinallattemptsandadequateventilation waspossibleinallpatients.Glottic viewdifferedbetween thestudieddevices(Table2).
Suitable conditions for FAI (full or partial glottis view) weregivenin50%withtheLT,in83%withtheLMASupreme, in70%withtheLMAI-Geland90%withtheLMAUniqueand theLMAAura-Once(Fig.3).
Adverseeventswerenotdocumentedinanyofthecases.
Discussion
Airwayrelatedcomplicationsarerarebutpotentially disas-trousduringgeneralanesthesiaandinemergencymedicine. Approximately 600 people die worldwidefrom difficulties withintubationeveryyear.1Manymoredevelopsevere
neu-rologicaldamage.2Theincidenceofdifficultintubationfor
electivesurgeryrangesfrom0.05%to18%,dependingonthe typeofsurgeryandthepre-existingmedicalconditions.1In
emergencymedicine theincidence ofa difficult airwayis evenhigher.
TheseandotherresultsledtoASArecommendationsfor theuseofalternativeairwayadjunctsthatallowadequate ventilationand oxygenation firstpublished in 1993.12 The
LMAwasprimarilymentionedinthepublishedguidelinesin 2003.2SincethenvariousdifferentSADshavebeenbrought
onthemarket.Variationsinprocessedmaterialandshape supposedlyfacilitateinsertionandimprovedventilation.It couldbedemonstratedallofthesedevicesallowemergency oxygenationandventilationincaseofafailedtracheal intu-bation.
fibreopticcontrolwascorrectinonly59%ofallcases.13This
supportstheideaofusingafiberscoperatherthaninserting adeviceblindlythroughanyairwaydevice.Becauseofthe variablepositionoftheblindlyinsertedSADwithrespectto theglotticaperture, theuseof afibreoptic bronchoscope increasesthesuccess rate of trachealintubation.13,14 The
orificeoftheSADandtheglotticaperturehavetobeinline toallowinsertionoftubeortubeexchanger.Aproper laryn-gealalignmentcanonlybeverifiedbyfiberopticaly.FAIvia LMAhasbeendescribedincasereportsandwasevaluatedin variousstudies.Itisconsideredareliableandsavemethod tomanage a difficult airway. Similar results exist for the laryngealtubethatisgainingpopularityintheprehospital setting.3
HoweverithastobeconsideredthatSADsdonotalways allowaFAIin allpatients.Aproperpharyngealpositionis essential.Withthevariationsinshapeandmaterialithas tobeassumedthatthepharyngealpositionofcommercially available SADvaries considerably. Aimof this preliminary study wasto examine if some of the very different SADs haveabetterpharyngeal positiontoallowFAI. Uptonow thishasnotbeenevaluatedsystematically.
The resultsof thisstudydemonstrate thatallthe used SADs are suitable to adequately oxygenate and ventilate the patient. This confirms the role of SAD in emergency airwaymanagement.IdeallythepositionoftheSADinthe pharynxinvolvesacloserelationofthedistalorificeofthe deviceandtheglotticaperturetoallowidealair-flow.This however could not always be demonstrated in our study. The pharyngeal position of the SADis variable,as shown before.Visualization of the glottisfrom the distal orifice ofthe insertedsupraglotticairway isnot alwayspossible. This limits the possibility to perform a FAI and explains whyablindinsertionpotentiallyfails.Relevantdifferences wereseen between the examined commercially available systems.The LMA Unique andthe LMA Aura-i offeredthe bestglotticviews. Intubationwouldhavebeen possiblein 90%oftheattempts.TheresultsfortheLTwereless con-vincing. Tracheal intubation would have been possible in only 40% of the cases. The results for the LMA I-Gel and theLMASupremewereacceptablewitharound70%success rate.Apparentlytheshapeandpossiblythematerialofthe LMAUniqueandtheLMA Aura-Ileadtohigherpercentage ofproperpharyngealposition.Ourresultsalsodemonstrate thatanaccuratepositionisnotnecessarilyneededtoallow adequateoxygenationandventilation.Onlyiftheinserted airwayisusedasabridgetoguidetrachealintubationthe pharyngealpositionbecomesrelevant.Incasesof afailed trachealintubationwithneedfor asaveendotracheal air-wayitshouldbeconsideredtoprimarilyinsertadevicethat allowsFAI.ExchangeoftheSADinterruptsoxygenationand putsthepatientatriskforaspiration.
The results providing a 90% success rate suggest that theconceptof asupraglotticairwayasguidefortracheal intubationisnotonlysuitableforemergencysituations.In conditionswhenheadmovementfordirectlaryngoscopyhas tobeavoided(e.g.instablefracturesofthecervicalspine) a tracheal intubation via SAD is a save and easy option. The described procedure might be a relevant alternative toawakefibreopticintubation;anevenmoresophisticated procedurewithpotentialdiscomfortforthepatient.A rel-evantadvantageof theuseofaSADasbridge totracheal
intubationisthepossibilityofcontinuousoxygenationand ventilationduringendoscopyusingabronchoscopyadapter. The described concept ofa dedicatedairway istherefore notonlyanoptionforanunexpecteddifficultintubationbut canalsobeusedinacontrolledsetting.Thisallows train-ing infibreoptic intubation andensures patientsafetyfor anticipateddifficultintubations.7
Limitations
Because of the preliminary character of the study only a small number of patients were examined per device. A larger number of patients need to beexamined toverify theresults.Difficultintubationoftenoccursinpatientswith anabnormalpharyngealorlaryngealanatomy.Iftheresults fromthisstudy can betransferredintothis patientgroup alsohastobesubjecttofurthertrials.
Conclusion
AllexaminedSDAscanserveasemergencyairwaystoallow oxygenation in case of difficult intubation. Not all of the examineddeviceshoweverhaveapharyngealpositionthat allowsafibreopticguidedtrachealintubation.Further stud-ies have to examine if these preliminary results can be verified.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterests.
Acknowledgements
Thestudyincludingdataacquisitionandanalysisaswellas manuscriptpreparationwasfundedbydepartmental fund-ing.
References
1.BenumofJL.Managementofthedifficultairway.AnnAcadMed Singapore.1994;23:589---91.
2.American Society of Anesthesiologists Task Force on Man-agement of the Difficult Airway. Practice guidelines for managementofthedifficultairway:anupdatedreportbythe AmericanSocietyofAnesthesiologistsTaskForceon Manage-mentoftheDifficultAirway.Anesthesiology.2003;98:1269---77. 3.GenzwuerkerHV,HilkerT,HohnerE,etal.Thelaryngealtube: anewadjunctforairwaymanagement.PrehospEmerg Care. 2000;4:168---72.
4.Asai T, Murao K, Shingu K. Efficacy of the laryngeal tube duringintermittentpositive-pressureventilation.Anaesthesia. 2000;55:1099---102.
5.DorgesV,OckerH,WenzelV,etal.Thelaryngealtube:anew simpleairwaydevice.AnesthAnalg.2000;90:1220---2.
6.CookTM,HardyR,McKinstryC,etal.Useofthelaryngealtube asadedicatedairwayduringtrachealintubation.BrJAnaesth. 2003;90:397---9.
8.AthertonDP,O’SullivanE,LoweD,etal.Aventilation-exchange bougieforfibreopticintubationswiththelaryngealmask air-way.Anaesthesia.1996;51:1123---6.
9.Hawkins M, O’Sullivan E, Charters P. Fibreoptic intubation usingthecuffedoropharyngealairwayandAintreeintubation catheter.Anaesthesia.1998;53:891---4.
10.GenzwuerkerHV,VollmerT,EllingerK.Fibreoptictracheal intu-bationafterplacementofthe laryngealtube. Br JAnaesth. 2002;89:733---8.
11.BrimacombeJ,BerryA.Aproposedfiber-opticscoringsystemto standardizetheassessmentoflaryngealmaskairwayposition. AnesthAnalg.1993;76:457.
12.Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task ForceonManagementoftheDifficultAirway.Anesthesiology. 1993;78:597---602.
13.Campbell RL, Biddle C,Assudmi N, et al. Fiberoptic assess-ment of laryngeal mask airway placement: blind insertion versus direct visual epiglottoscopy. J Oral Maxillofac Surg. 2004;62:1108---13.