w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Colonic
complications
following
human
bone
marrow
transplantation
Paulino
Martínez
Hernández-Magro
a,∗,
Juan
Pablo
Pe ˜na
Ruiz
Esparza
b,
Eduardo
Villanueva
Sáenz
b,
José
Luis
Rocha
Ramírez
b,
Enrique
Gómez
Morales
c,
Isaac
Felemovicius
Hermagnus
daHospitalGuadalupanodeCelaya,Celaya,Mexico
bHospitaldeEspecialidades,CentroMédicoNacionalSigloXXIIMSS,MexicoCity,Mexico
cHematologyDepartment,CentroMédicoNacionalSigloXXIIMSS,MéxicoCity,Mexico
dDepartmentofSurgery,UniversityofMinnesota,Minneapolis,UnitedStates
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received28May2014 Accepted11August2014
Availableonline4September2014
Keywords:
Coloniccomplications Humanbonemarrow transplantation Superinfection
a
b
s
t
r
a
c
t
Background:Humanbonemarrowtransplantation(BMT)becomesanacceptedtreatmentof leukemia,aplasticanemia,immunodeficiencysyndromes,andhematologicmalignancies. Colorectalsurgeonsmustknowhowtodetermineandmanagethemaincolonic complica-tions.
Objective:Toreviewtheclinicalfeatures,clinicalandpathologicalstagingofgraftvshost disease(GVHD),andtreatmentofpatientssufferingwithcoloniccomplicationsofhuman bonemarrowtransplantation.
Patientsandmethods:Wehavereviewedtherecordsofallpatientsthatreceivedanallogeneic bonemarrowtransplantandwereevaluatedatourColonandRectalSurgerydepartment duetogastrointestinalsymptoms,betweenJanuary2007andJanuary2012.Thestudywas carriedout inpatientswho developedcolonic complications,allofthem withclinical, histopathologicalorlaboratorydiagnosis.
Results:Thestudygroupwasconstitutedby77patients,43maleand34femalepatients.We identifiedcoloniccomplicationsin30patients(38.9%);fivepatientsdevelopedintestinal toxicityduetopretransplantchemotherapy(6.4%);graftvs.hostdiseasewaspresentin 16patients(20%);13patients(16.8%)developedacutecolonicGVHD,and3(3.8%)chronic GVHD.Infectionwasidentifiedin9patients(11.6%).
Conclusions:Thethreeprincipalcoloniccomplicationsarethechemotherapytoxicity,GVHD, andsuperinfection;theonsetofsymptomscouldhelptosuspectthetypeofcomplication (0–20daychemotherapytoxicity,20andmoreGVHD),andinfectioncouldappearinany timeoftransplantation.
©2014SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
∗ Correspondingauthor.
E-mail:paulinomhm@hotmail.com(P.M.Hernández-Magro).
http://dx.doi.org/10.1016/j.jcol.2014.08.002
Complicac¸ões
do
cólon
após
transplante
de
medula
óssea
humana
Palavras-chave:
Complicac¸õesdocolo Transplantedemedulaóssea humana
Superinfecc¸ão
r
e
s
u
m
o
Experiência: Otransplantedemedulaósseahumana(MOH)passouaserumtratamento adotadoparaleucemia, anemia aplástica, síndromesde imunodeficiência eneoplasias hematológicas.Cirurgiõescolorretaisdevemsabercomodeterminaretratarasprincipais complicac¸õesdocólon.
Objetivo: Revisarascaracterísticasclínicas,estadiamentosclínicoepatológicodadoenc¸a do enxerto versushospedeiro (DEVH)e o tratamentode pacientes padecendo comas complicac¸õescolônicasdotransplantedemedulaósseahumana.
PacienteseMétodos: Revisamososregistrosdetodosospacientesquereceberamum trans-plantedemedulaósseaalogênicaeforamavaliadosemnossoDepartamentodeCirurgia doCóloneRetoemfunc¸ãodesintomasgastrointestinais,entrejaneirode2007ejaneirode 2012.Oestudoteveporbaseospacientesquedesenvolveramcomplicac¸õesdocólon,todos comdiagnósticoclínico,histopatológicooulaboratorial.
Resultados: Ogrupode estudofoiconstituído por77 pacientes,sendo43homense34 mulheres.Identificamoscomplicac¸õesdocólonem30pacientes(38,9%);cincopacientes exibiamtoxicidadeintestinalporquimioterapiaantesdotransplante(6,4%);DEVHestava presenteem16pacientes(20%),13pacientes(16,8%)foramacometidosporDEVHcolônica agudatrêspacientes(3,8%)DEVHcrônica.Infecc¸ãofoidetectadaem9pacientes(11,6%).
Conclusões: Astrêsprincipaiscomplicac¸õesdocólonsão:toxicidadeporquimioterapia, DEVHesuperinfecc¸ão.Osurgimentodossintomaspoderiaajudaralevantarsuspeitassobre otipodecomplicac¸ão(0–20dias,toxicidadeporquimioterapia;20oumaisdias,DEVH). Infecc¸õespodemocorreremqualquermomentodotransplante.
©2014SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
During the 1980s the human bone marrow transplanta-tion(BMT)becamefromexperimentaltherapyforend-stage patients to its current place as an accepted treatment of leukemia, aplastic anemia, immunodeficiency syndromes, andhematologicmalignancies.1–5Thelong-termdisease-free
survivalforuntransfused patientswithsevereaplastic ane-miaisupto80%andforpatientswithacutenonlymphoblastic leukemiatransplantedinfirstremissionitapproaches60%,1,2
thereforethenumberofallogeneicbonemarrow transplanta-tionsperformedworldwideincreasesexponentially.6,7
BMTmaycauseintestinaldamagebythreemechanisms: toxicityfrompretransplantchemoradiation,graft-versus-host disease (GVHD), and infection in the immunosuppressed host.Themainlatecomplicationofallogeneicbonemarrow transplantisthe GVHD.3–5 Intestine, skin, lungs,8 liverand
lymphoidorgansarethemaintargetorgansinGVHD.4About
30–50%ofallogeneicmarrowrecipientswilldevelopintestinal GVHD,2,9–12 with afataloutcome in upto 15%.11
Gastroin-testinaltractinvolvementisfrequentlythemostsevereand difficulttotreat.4
Allogeneic bone marrow transplantation is now widely practiced, and therefore, specialist evaluations for a mul-tidisciplinaryteamare nowdemanding;gastroenterologists and colorectalsurgeons mustknow how todetermineand manage these main colonic complications. The aim of this study is review the clinical, laboratorial, endoscopic
and pathological features, and treatment of patients suf-fering with colonic complications of human bone marrow transplantation.
Patients
and
methods
Wehave reviewedthe records ofall patientsthat received anallogeneicbonemarrowtransplantandwereevaluatedat ourColonandRectalSurgerydepartmentdueto gastrointesti-nalsymptoms,betweenJanuary2007andJanuary2012.The studywasconductedonlyinpatientswhodevelopedcolonic complications,allofthemwithclinical,histopathologicalor laboratorydiagnosis.
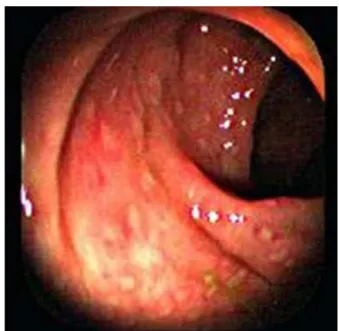
Fig.1–Normalappearanceofthecolonicmucosain colonoscopy.
whichallsubsequenteventsweredated,aswellastheonset ofdigestivesymptoms.
Results
ThefirstBMTdoneinourhospitalwasin1995,andits appli-cationhasbeenincreasingwithtime.Wereviewedtherecords of77patientswithallogeneictransplantsperformedbetween 2007and2012,whopresenteddigestivesymptoms,andwere submitted to evaluation at the Colon and Rectal Surgery department.Thestudygroupwasconstitutedby43maleand 34femalepatients,withagesfrom16to50years,mean31.3. Theindicationfortransplantwas:in38patientsChronic Mye-locyticLeukemia,in20patientsAcuteMyelogenousLeukemia, in8 patientsAcute Lymphoblastic Leukemia, in7patients MyelodisplasicSyndrome,andin4patientsAplasticAnemia.
Fig.2–Arectalbiopsyshowingdiffusedestructionof cryptsaseffectofconditioningchemotherapy.
HLAwas100%identicalin65patients.Weidentifiedcolonic complicationsin30patients(38.9%)thatarepresentedas fol-lows.
Chemotherapytoxicity
Five patients developedintestinal toxicity dueto pretrans-plantchemotherapy(6.4%);allofthempresentedhighwatery diarrhea,anorexia,nausea,andcrampyabdominalpain.The symptoms onset was from day 5 to day 12. At physical examination with generalized colic abdominal pain, there was increase in frequency of intestinal peristalsis but no signsofperitonitis,colonicmucosaappearednormalinthe endoscopic studies (colonoscopy or rectoscopy) and biop-siesreportedonlychemotherapytoxicity(Figs.1and2)with regenerationatday16–20,nopathogenswereisolatedfrom stools. All patients were treated conservatively with fluid and electrolyte replacementand prophylactic therapywith metronidazole 500mg IVt.i.d plus ciprofloxacin 500mgIV
Fig.4–Colonicbiopsyshowingapoptosis(cellnecrosisin crypts),flatteningepithelium,andtotalepithelial
denudation.
b.i.d.Resolutionofthesymptomswasachievedin2–3weeks approximately.
Graftvs.hostdisease
Graft vs. hostdisease was present in16 patients(20%), 13 patients(16.8%)developedacutecolonicGVHD,and3(3.8%) chronic GVHD; symptoms were developed from day 20 to day182,characterizedbynausea,anorexia,vomiting,crampy abdominalpain, profuse diarrhea with mucous, and occa-sionallylowergastrointestinal(GI)bleeding,withabdominal distensionwithoutperitonealsigns.
4patients developed skin (maculopapularskin rash on the trunk, palms, soles and ears) and hepatic manifesta-tions(jaundiceandserumtransaminaseincrease).Allpatients underwent colonoscopy with findings of patchy erythema andinflammationofthemucosathroughthecolon(Fig.3), mostfrequentlyinascendantcolon,andileocecalvalvearea; histopathologystudyofthemucosalbiopsiesconfirmedGVHD (Fig. 4). All patients were treatedwith fluid, an electrolyte replacement,and steroidtherapy wasinitiatedwith metil-prednisolone0.5–2mg/kg/dayinallpatients;2patientswith lowerGIbleedingreceivedsubcutaneousinjectionof somato-statinanalogs(octreotide,50gt.i.d),and8ofthepatients
withacuteGVHDreceived totalparental nutrition(TPN) to maintainintestinalrest.Bleedingstoppedspontaneouslyin allpatients.Eightpatientsreceivedasacomplementoftheir systemicimmunosuppresionanempirictreatmentwith9mg oralbudesonideinadailysingledosefor3weeks.Onepatient developedacute respiratory failure and pulmonary hemor-rhagesecondarytopulmonaryGVHDand diedonthe59th posttransplantday.
The3patientswithchronicGVHDweretreatedonan out-patientbasiswithoralprednisone.
Infection
Infection was identified in 9 patients (11.6%). 5 patients with cytomegaloviral enterocolitis (CMV) corroborated
Fig.5–ColonoscopicappearanceofCMVinfection.Ulcers varyfrompunctuatelesionstocoalescingdeepulcers.
by endoscopic appearance and histopathological studies (Figs. 5 and 6), identifying the characteristic intranuclear inclusionbodiesofCMV;3patientsdeveloped pseudomem-branous colitis (Clostridium difficile) showing the typical presence of the adherent so-called pseudomembranes at thecolonoscopy(Fig.7),and1patientwaswith superinfec-tion byShigella, obtainedinfecalculturesand withedema and multiplesmall ulcerationsinthe colonmucosain the colonoscopy(Fig. 8). Theonset ofsymptomsbegan onday 8onwards.Allpatientswereinitiallytreatedwiththesame general indications,fluid and electrolytereplacement, etc., and then the specific treatmentfor each condition, ganci-clovir 5mg/kg/b.i.dforCMV,vancomicine500mgIVq.i.d or metronidazole500mgIVt.i.dforpseudomembranouscolitis andciprofloxacin500mgIVb.i.dforthepatientwithShigella superinfection.
Fig.7–Mucosaledemaandpresenceofpseudomembranes incolonoscopy.
Discussion
The human bone marrow transplantation has become an acceptedtreatmentforpatients withseveralhematological disorders.1,13Themarrowisgivenbyintravenousinfusionand
within2–4weeksthemarrowcellularityandperipheralcounts increaseasthedonorgraftbecomesfunctional.
Diagnosisandtreatmentofthegastrointestinal complica-tionscanbeextremelycomplex,asonemustdecidewhether asymptomisduetotheconditioningregimentoxicity,GVHD, infectionoracombinationofcauses.12Diarrheaisacommon
andserioussymptomofthiscomplications.7,10,14
Chemotherapy toxicity must be suspected when the patientdevelopsintestinalsymptomsfrom dayzerotoday 20. Previous studies have shown that diarrhea caused by cytoreductive therapyhas resolvedby day20 inalmost all
Fig.8–Mucosaledemaandulcerationinsuperinfectionby Shigella.
patients. When chemotherapyiscombinedwithtotal body irradiationweobservediffusemucosalabnormalitieswithin 10daysoftransplantation,andnecrosisofintestinalcrypts, withatypiaofcryptcellnuclei;biopsyspecimenstaken16–20 daysaftertransplantationshowedevidenceofregeneration. Venocclusivediseasesoftheliverandpericentralhepatocyte necrosishavebeenrelatedtochemoradiationtherapyandcan evenproducefulminanthepaticfailure.Theadditiveor pos-siblesynergisticeffectofradiationininducingorgandamage duringallogeneicGVHDiswellrecognized.5 Thusradiation
hasbeenreportedtoreducesurvivaltime,induceGVHDat earliertime,enhancetheintensityofGVHD,orincreasethe incidenceofGVHD.10
AcuteGVHDusuallystarts4–5weeksaftermarrow trans-plantation, and consists of dermatitis, enteritis, and liver disease. Patients with intestinal involvement have profuse diarrheausuallywaterywithamucoidappearance,crampy abdominalpain,nausea,anorexia,andbloodintheirstools; thepatientsmayhaveabdominalpainwithsometimes perit-onealsignsprobablyfortransmuraledemaandinflammation ofthesmallintestine4;GVHDcaninvolveupper
gastrointesti-naltract,characterizedbythenonspecificsymptomatologyof nausea, vomiting,bloating,andfoodintolerance15;incolon
themostfrequentlocalizationofdiseaseisintheascending colon, butallregionsofthecolonhavebeenreportedtobe involved.ThebasichistopathologicalfeatureofacuteGVHD, which occursinthefirst 100daysposttransplant,is necro-sisofindividualcellsintheregeneratingcompartmentofthe mucosa.16ThebasicpathologyofchronicGVHDisfibrosisof
thesubmucosaandsubserosawhichoccursgenerallyafter3 monthsposttransplant,thereforemucosalbiopsyisoflimited usefulnessinthediagnosisofchronicGVHD.16
Antimicrobialchemotherapytargetedtointestinal anaer-obic bacteria in marrow transplant recipients reduces the severity of acute GVHD and supports the theory that the intestinal anaerobic bacterial microflora playsa significant roleinthepathogenesisofacuteGVHDafterhumanmarrow transplantation.17,18
Endoscopicexaminationisusuallysafeforpatientswith GVHD. It can give critical information on clinical deci-sionmaking whenthe histologyisdiscordant withclinical presentation.19,20TheendoscopicappearanceofGVHDranges
from normal mucosa to erythema, mucosal sloughing, or patchyerosions.7,10,21,22Biopsyhasbeenshowntobeaccurate
intheidentificationofGVHD.7,11
HistopathologicfindingsofGVHDare:colonicwall inflam-matory infiltrate of mature and activated lymphocytes, macrophages,andneutrophils.10,23Cryptdropoutand
necro-sis (apoptosis) are the characteristic histological lesions (“exploding crypt cells”) and are present only in relatively intact mucosa; when the disease is advanced with total mucosadenudationthe biopsy isless specific.1,12 GVHDin
biopsysamplescanbehistologicallygradedasfollows:GradeI: singlecellnecrosisandapoptosis;GradeII:evidenceof epithe-lialdamagebycrypt/glandularabscess,epithelialflattening orcrypt/glandulardilation;GradeIII:dropoutofoneormore crypts/glands,andGradeIV:totalepithelialdenudation.24
Radiographicevaluationcanshowoccasional pneumato-sis in small intestine,25 mucosal and submucosal edema,
barium enema, be aware that these findings can be also causedbycytomegalovirusenteritisorradiationinjury, mak-ingimpossiblethedifferentiationonthebasisofradiographic findingsalone.26 Jonesetal.11 usedCTscantoevaluatethe
extentofgastrointestinalinvolvement;theirfindingsinclude wall thickening, bowel fold enlargement, bowel dilatation, luminalnarrowing,mesentericnodes,andincreaseddensity inmesentericfatcompatiblewithinflammation,withscans obtained16–25daysafterinitialscans.
ThestandardtreatmentofacuteGVHD,irrespectiveofsite, iscorticosteroidsand/orimmunosuppressiveagents.4,27
Oper-ative interventionis rarelytherapeutic, but surgerycan be performedfor complicationsof intestinalgraft-versus-host diseasenotrespondingtomedicaltherapy.4,28Maturesurgical
judgmentisnecessarytoavoidunnecessaryandvery danger-ousoperations.
PerianalinfectionsareararecomplicationofBMT,these infections are polymicrobial, and organisms isolated are similartothoseseenintheperianalinfectionsof nonimmuno-suppressedpatients.29
Thefinding inthe stoolsof fungal elements, parasites, pathogenicbacteriaorvirusessuggestssuperinfections com-plicatingBMT.
Cytomegalovirusinfectionhasbeendocumentedin40–50% of patients undergoing BMT.30 Not only
immunoglobu-lin and antivirals such as acyclovir are proposed medical treatments,30butalsosurgicaltreatmenthasbeenreported
incomplications.31Diagnosisismadehistologicallywiththe
presenceof typical or atypical cytomegalovirus inclusions, becausethemorphologicfeaturesaresimilar withGVHD.32
Massivehematocheziasecondarytograft-versus-hostdisease andcytomegalovirusinfectionhasbeenreported.33Otherviral
infectionsreportedinBMTpatientsareherpessimplexvirus infection.Onlysixpatients withintestinalinfection dueto herpesvirus(colitisinallofthecases)havebeenreportedin theliterature.34
Cryptosporidiaareprotozoalparasitesthatcaninfectthe gastrointestinaltractofman.Inimmunologicallynormal sub-jectsthediseaseisself-limited,resolvinginfivetotendays. CryptosporidiuminfectionhasbeenreportedfollowingBMT asacauseofdiarrhea.35Theproposedtreatmentforthis
con-ditionincludesmetronidazoleandnitazoxanidewhichhave beenshowntoimprovesymptoms.36
Eosinophiliccolitisisarareinflammatorydisease charac-terizedbyeosinophilicinfiltrationofthecolonandperipheral bloodeosinophilia.Eosinophiliccolitishasbeenreportedin associationwithallogeneicbonemarrowtransplantation.37
Conclusions
Asthepracticeofbonemarrowtransplantisincreasing,itis almostcertainthatagastroenterologistorcolorectalsurgeon shouldbefacedtothistypeofcoloniccomplications devel-opedinconsequence.Wemustknowhowtoidentifyandtreat themopportunelywiththeassistanceofamultidisciplinary teamtoofferagoodoutcometothepatient.
The three principal colonic complications are the chemotherapy toxicity, GVHD, and superinfection; the onsetofsymptomsisimportant,andcouldhelptosuspect
the type of complication (0–20 day chemotherapy toxicity, 20 and more GVHD, infection could appearin any timeof transplantation)andplanthetypeoftreatment.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.McDonaldGB,ShulmanHM,SullivanKM,SpencerGD. Intestinalandhepaticcomplicationsofhumanbonemarrow transplantation.PartI.Gastroenterology.1986;90:460–77.
2.SullivanKM,SchulmanHM,StorbR,EeidenPL,Whiterspoon RP,McDonaldGB,etal.Chronicgraft-versus-hostdiseasein 52patients:adversenaturalcourseandsuccessfultreatment withcombinationimmunosuppresion.Blood.1981;57:267–75.
3.VolgelsangGB,FarmerER,HessAD,AltamonteV,Beschorner WE,JabsDA,etal.Thalidomideforthetreatmentofchronic graft-versus-hostdisease.NewEnglJMed.1992;326:1055–8.
4.IraniJL,CutlerCS,WhangEE,ClancyTE,RussellS,Swanson RS,etal.Severeacutegastrointestinalgraft-vs-hostdisease. Anemergingsurgicaldilemmaincontemporarycancercare. ArchSurg.2008;143:1041–5.
5.HillGR,CrawfordJM,CookeKR,BrinsonYS,PanL,FerraraJL. Totalbodyirradiationandacutegraft-versus-hostdisease: theroleofgastrointestinaldamageandinflammatory cytokines.Blood.1997;90:3204–13.
6.FerraraJL,JoachimDeegH.Graft-versus-hostdisease.NEngJ Med.1991;324:667–73.
7.XuCF,ZhuLX,XuXM,ChenWC,WuDP.Endoscopic
diagnosisofgastrointestinalgraf-versus-hostdisease.WorldJ Gastroenterol.2008;14:2262–7.
8.Ramírez-AcevesR,Gómez-MoralesE,Sánchez-ValleE, Blanco-LemusE,Pimentel-CruzE,Pizzuto-ChávezJ, Cabrera-Mu ˜nozML.Trasplantedemedulaósea.GacMed Mex.2001;137:59–63.
9.SaleGE,ShulmanHM.hepathologyofbonemarrow transplantation.USA:MassonPublishing;1984.p.77–103 [chapter6].
10.EigenbrodtML,EigenbrodtEH,ThieleDL.Histologicsimilarity ofmurinecolonicgraftversushostdisease(GVHD)tohuman colonicGVHDandinflammatoryboweldisease.AmJPathol. 1990;137:1065–76.
11.JonesB,FishmanEK,KramerSS,SiegelmanSS,SaralR, BeschornerWE,etal.Computedtomographyof gastrointestinalinflammationafterbonemarrow transplantation.AJR.1986;146:691–5.
12.ShidhamVB,ChangCC,ShidhamG,GhazalaF,LindholmPF, KampalathB,etal.Colonbiopsiesforevaluationofacute graft-versus-hostdisease(A-GVHD)inallogeneicbone marrowtransplantpatients.BMCGastroenterol.2003;3:5.
13.VogelsangGB.HowItreatchronicgraft-versus-hostdisease. Blood.2001;97:1196–201.
14.CoxGJ,MatsuiSM,LoRS,HindsM,BowdenRA,HackmanRC, etal.Etiologyandoutcomeofdiarrheaaftermarrow transplantation:aprospectivestudy.Gastroenterology. 1994;107:1398–407.
15.WeisdorfDJ,SnoverDC,HaakeR,MillerWJ,McGlavePB, BlazarB,etal.Acuteuppergastrointestinalgraft-versus-host disease:clinicalsignificanceandresponseto
immunosuppressivetherapy.Blood.1990;76:624–9.
17.BeelenDW,ElmaagacliA,MüllerKD,HircheH,SchaeferUW. Influenceofintestinalbacterialdecontaminationusing metronidazoleandciprofloxacinorciprofloxacinaloneonthe developmentofacutegraftversushostdiseaseaftermarrow transplantationinpatientswithhematologicmalignancies: finalresultsandlong-termfollowupofanopen-label prospectiverandomizedtrial.Blood.1999;93:3267–75.
18.BeelenDW,HaralambieE,BrandtH,LinzenmeierG,Müller KD,QuabeckK,etal.Evidencethatsustainedgrowth suppressionofintestinalanaerobicbacteriareducestherisk ofacutegraft-versus-hostdiseaseaftersiblingmarrow transplantation.Blood.1992;80:2668–76.
19.CheungDY,KimJI,KimSS,SungHY,ChoSH,ParkSH,etal. Endoscopicevaluationingastrointestinalgraft-versus-host disease:comparisonswithhistologicalfindings.DigDisSci. 2008;53:2947–54.
20.Cruz-CorreaM,PoonawalaA,AbrahamSC,WuTT,Zahurak M,VogelsangG,etal.Endoscopicfindingspredictthe histologicdiagnosisingastrointestinalgraft-versus-host disease.Endoscopy.2002;34:808–13.
21.SaitoH,OshimiK,NagasakoK,YashiroK,TanakaT,ToyodaC, etal.Endoscopicappearanceofthecolonandsmallintestine ofapatientwithhemorrhagicentericgraft-vs-hostdisease. DisColonRectum.1990;33:695–7.
22.SaitoH,OshimiK,NagasakoK,YashiroK,TanakaT,ToyodaC, etal.Endoscopicappearanceofthecolonandsmallintestine ofapatientswithhemorrhagicentericgraft-vs.-hostdisease. DisColonRectum.1990;33:695–7.
23.BombíJA,NadalA,CarrerasE,RamírezJ,Mu ˜nozJ,RozmanC, etal.Assessmentofhistopathologicchangesinthecolonic biopsyinacuteGraft-versus-hostdisease.AmJClinPathol. 1995;103:690–5.
24.YamasakiS,Miyagy-MaeshimaA,KakugawaY,MatsunoY, Ohara-WakiF,FujiS,etal.Diagnosisandevaluationof intestinalgraft-versus-hostdiseaseafterallogeneic hematopoieticstemcelltransplantationfollowing
reduced-intensityandmyeloablativeconditioningregimens. IntJHematol.2013;97:421–6.
25.DayDL,RamsayNKC,LetourneauJG.Pneumatosisintestinalis afterbonemarrowtransplantation.AJR.1988;151:85–7.
26.JonesB,KramerSS,SaralR,BeschornerWE,YolkenRH, TownsendTR,etal.Gastrointestinalinflammationafterbone
marrowtransplantation:graft-versus-hostdiseaseor opportunisticinfection?AJR.1988;150:277–81.
27.SullivanKM,WitherspoonRP,StorbR,DeegHJ,DahlbergS, SandersJE,etal.Alternating-daycyclosporineand prednisonefortreatmentofhigh-riskchronic graft-versus-hostdisease.Blood.1988;72:555–61.
28.EvansJ,PercyJ,EcksteinR,MaD,SchnitzlerM.Surgeryfor intestinalgraft-versus-hostdisease.Reportoftwocases.Dis ColonRectum.1998;41:1573–6.
29.CohenJS,BenjaminPazI,O’DonellMR,EllenhornJDI. Treatmentofperianalinfectionfollowingbonemarrow transplantation.DisColonRectum.1996;39:981–5.
30.MillerW,FlynnP,McCulloughJ,BalfourJrHH,GoldmanA, HaakeR,etal.Citomegalovirusinfectionafterbonemarrow transplantation:anassociationwithacutegraft-v-host disease.Blood.1986;67:1162–7.
31.HaniMA,BenAchourJ,ZoghlamiA,NajahN.Acute cytomegaloviruscolitisafterbonemarrowtransplantation. TunisMed.2003;81:145–8.
32.KrausMD,Feran-DozaM,Garcia-MolinerML,AntinJ,Odze RD.Cytomegalovirusinfectioninthecolonofbonemarrow transplantationpatients.ModPathol.1998;11:29–36.
33.ShabahangM,PasqualeMD,BittermanP,CirenzaE,SpitzerT, EvansSR.Massivehematocheziasecondaryto
graft-versus-hostdiseaseandcytomegalovirus.AmJ Gastroenterol.1994;89:632–3.
34.KingreenD,NitscheA,BeyerJ,SiegertW.Herpessimplex infectionofthejejunumoccurringintheearly
posttransplantationperiod.BoneMarrowTransplant. 1997;20:989–91.
35.ManivelC,FilipovichA,SnoverDC.Cryptosporidiosisasa causeofdiarrheafollowingbonemarrowtransplantation.Dis ColonRectum.1985;28:741–2.
36.FaraciM,CappelliB,MorrealeG,LaninoE,MoroniC, BandettiniR,etal.NitazoxanideorCD3+/CD4+lymphocytes forrecoveryfromsevereCryptosporidiuminfectionafter allogeneicbonemarrowtransplant?PediatrTransplant. 2007;11:113–6.