www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Pulmonary
hypertension
evaluation
by
Doppler
echocardiogram
in
children
and
adolescents
with
mouth
breathing
syndrome
夽
,
夽夽
Marcela
Silva
Lima
a,∗,
Carolina
Maria
Fontes
Ferreira
Nader
b,c,
Letícia
Paiva
Franco
d,e,
Zilda
Maria
Alves
Meira
f,
Flavio
Diniz
Capanema
g,
Roberto
Eustáquio
Santos
Guimarães
h,
Helena
Maria
Gonc
¸alves
Becker
h,iaUniversidadeFederaldeMinasGerais(UFMG),DepartamentodeCirurgiaeOftalmologia,BeloHorizonte,MG,Brazil bFaculdadedeSaúdeeEcologiaHumana(FASEH),Vespasiano,MG,Brazil
cFaculdadedeSaúdeeEcologiaHumana(FASEH),Fundac¸ãodeAmparoaPesquisadoEstadodeMinasGerais(FAPEMIG),
ProgramaInstitucionaldeBolsasdeIniciac¸ãoCientíficaeTecnológica(PROBIC),Vespasiano,MG,Brazil
dUniversidadeFederaldeMinasGerais(HC-UFMG),HospitaldasClínicas,BeloHorizonte,MG,Brazil eUniversidadeFederaldeMinasGerais(UFMG),FaculdadedeMedicina,BeloHorizonte,MG,Brazil fUniversidadeFederaldeMinasGerais(UFMG),DepartamentodePediatria,BeloHorizonte,MG,Brazil
gNúcleodeInovac¸ãoTecnológica,Fundac¸ãoHospitalardoEstadodeMinasGerais(FHEMIG),SantaEfigênia,MG,Brazil
hUniversidadeFederaldeMinasGerais(UFMG),FaculdadedeMedicina,DepartamentodeOftalmologia,Otorrinolaringologiae
Fonoaudiologia,BeloHorizonte,MG,Brazil
iUniversidadeFederaldeMinasGerais(HC-UFMG),HospitaldasClínicas,CentroMultidisciplinardeAtenc¸ãoaoRespiradorOral,
BeloHorizonte,MG,Brazil
Received7January2016;accepted31March2016 Availableonline8June2016
KEYWORDS Mouthbreathing; Adenoidectomy; Pulmonary hypertension; Doppler
echocardiography; Rhinitis
Abstract
Introduction:Adenotonsillar hyperplasia (ATH) andallergic rhinitis (AR) are themost com-mon causes ofupper airwayobstructionin children.Such diseases, by affectingthe upper airways,cancausechronicalveolarhypoventilation,pulmonaryvasoconstrictionandpulmonary hypertension,whichinsomecases,areirreversible.
Objective:Thiscross-sectionalstudy aimedtoevaluatetheprevalenceofpulmonary hyper-tensionintwogroupsofmouth-breathing(MB)2---12yearsoldchildrenwithATHandisolated allergicrhinitis,throughDopplerechocardiography.
夽 Pleasecitethisarticleas:LimaMS,NaderCM,FrancoLP,MeiraZM,CapanemaFD,GuimarãesRE,etal.Pulmonaryhypertensionevaluation
byDopplerechocardiograminchildrenandadolescentswithmouthbreathingsyndrome.BrazJOtorhinolaryngol.2017;83:292---8.
夽夽
StudycarriedoutatHospitalSãoGeraldo,HospitaldasClinicas,FaculdadedeMedicina,UniversidadeFederaldeMinasGerais(UFMG), BeloHorizonte,MG,Brazil.
∗Correspondingauthor.
E-mail:marcelasl03@yahoo.com.br(M.S.Lima).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.03.020
Methods:54patientswithATHandindicationsforadenoidectomyand/ortonsillectomyand24 patientswithpersistentallergicrhinitiswereselectedandsubmittedtoDoppler echocardiog-raphy.TheSystolicPulmonaryArteryPressure(SPAP)wasdeterminedbytricuspidregurgitation andtheMeanPulmonaryArteryPressure(MPAP)wascalculatedfromtheSPAP.Similar measure-mentswerecarriedoutin25nasalbreathing(NB)individuals.
Results:ThemeanMPAPandSPAPwerehigherintheMBthanintheNBgroup(17.62±2.06 [ATH]and17.45±1.25[AR]vs.15.20±2.36[NB]mmHg,p<0.005,and25.61±3.38[ATH]and 25.33±2.06[AR]vs.21.64±3.87[NB]mmHg,p<0.005,respectively)andthemean accelera-tiontimeofpulmonaryflowtrace(Act)washigherintheNBthanintheMBgroup(127.24±12.81 [RN]vs.114.06±10.63ms[ATH]and117.96±10.28[AR]MS[AR];p<0.0001).
Conclusion: NoneoftheMBchildren(ATHandAR)metthePHcriteria,althoughindividualswith bothATHandisolatedARshowedsignificantevidenceofincreasedpulmonaryarterypressureby DopplerechocardiographyinrelationtoNBindividuals.Nodifferenceswereobservedbetween theATHandARgroups.
© 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE Respirac¸ãobucal; Adenoidectomia; Hipertensão pulmonar;
Ecodopplercardiografia; Rinite
Avaliac¸ãodehipertensãopulmonarpelaecodopplercardiografiaemcrianc¸as
eadolescentescomsíndromedorespiradororal
Resumo
Introduc¸ão: Ahiperplasiaadenotonsilar(HAT)earinitealérgica(RA)consistemnascausasmais comunsdeobstruc¸ãodeviasaéreassuperioresemcrianc¸as.Taisafecc¸ões,aocomprometera viaaéreasuperior,podemocasionarhipoventilac¸ãoalveolarcrônica,vasoconstric¸ãopulmonar ehipertensãopulmonar,emalgunscasosirreversível.
Objetivo: Esteestudotransversalobjetivouavaliaraprevalênciadehipertensãoarterial pul-monaremdoisgruposdecrianc¸asrespiradorasorais(RO):comHATerinitealérgicaisolada,de 2a12anos,pormeiodeexameecodopplercardiográfico.
Método: Foramselecionadosesubmetidosàecodopplercardiografia54pacientescomHATcom indicac¸ãodeadenoidectomiae/outonsilectomiae24pacientescomrinitealérgicapersistente. Apressãosistólicadaartériapulmonar(PSAP)foideterminadapelaregurgitac¸ãotricúspidee apressão médiadaartériapulmonar (PMAP)foi calculadaapartir daPSAP. Determinac¸ões similaresforamrealizadasem25respiradoresnasais(RN).
Resultados: As médias da PMAP e da PSAP foram maiores nos grupos de RO do que nos RN (17,62±2,06 [HAT] e 17,45±1,25 [RA] vs. 15,20±2,36 [RN] mmHg; p<0,005; e 25,61±3,38[HAT]e25,33±2,06[RA]vs.21,64±3,87[RN]mmHg;p<0,005;respectivamente) eamédiadotempodeacelerac¸ãodotrac¸adodofluxopulmonar(TAc)foimaiornosRNquenos gruposdeRO(127,24±12,81[RN]vs.114,06±10,63ms[HAT]e117,96±10,28[RA]MS[RA]; p<0,0001).
Conclusão:Nenhumacrianc¸arespiradoraoral(HATeRA)preencheuoscritériosdeHP,embora tanto os portadores deHATquanto de RAisoladaapresentaram evidências significativasde aumentodapressãoarterialpulmonarpelaecodopplercardiografiaemrelac¸ãoaosrespiradores nasais.Nãoseobservoudiferenc¸aentreosgruposHATeRA.
© 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Mouth breathing syndrome (MBS) refers to the clinical condition in which the individual has a breathing pattern performed predominantly through the oral cavity for a periodlongerthansixmonths.1,2Amongtheetiologies,
aller-gic rhinitis is the most common cause of chronic upper airway obstruction (UAO),3 accounting for up to 85% of
cases. The hypertrophy of adenoids and/or tonsils corre-spondsto79.2%,beingthemaincauseofObstructiveSleep Apnea(OSA)inchildren.1,4---9
hypertension (PH).6---14 PH in children is defined as Mean
Pulmonary Artery Pressure (MPAP) ≥25mmHg or Systolic Pulmonary Artery Pressure (SPAP) ≥35mmHg at rest.6,15
Although there are few reports of severe manifestations suchascorpulmonaleanddeath,16---21PHinitsinitialphase
has been very prevalent in some studies involving up to 84% of mouth breathers (MB).11 Nevertheless,
underdiag-nosis is observed in the initial phase of PH due to the scarcityofcardiovascularsymptoms.11 Anearly approach,
with adenotonsillectomy and treatment of allergic rhini-tis,promptlyreverseselevatedpressuresinthepulmonary artery.6---9,12---14,22
The Doppler echocardiographic evaluation is a non-invasive method that allows the estimation of the MPAP and SPAP values with a sensitivity of 79---100% and a specificityof68---98%.15,23Inspiteofitslow-costand
poten-tial for an early assessment of cardiac complications, it is not routinely performed in patients with UAO, being restrictedtoseverecasesofOSAwithevidentcardiovascular deterioration.6,7,9,12,13
This studyaimedtoevaluatethepresenceofPH inMB withUAOcausedbyATHandARinchildrenandadolescents treatedinareferralcenterthroughtheDoppler echocardi-ographicmethod.
Methods
ThisstudywasapprovedbytheResearchEthicsCommittee (CAAEnumber:20931213.0.0000.5149).The patientswere informedaboutthestudyanditsobjectivesandwereasked tosignthefreeandinformedconsentform,afterassisted readingandguidance.
The sampleconsisted ofchildren andadolescentsaged twototwelveyears,MBwithATHandAR,treatedasfirst consultation at the Mouth Breather Outpatient Clinic, in additiontopatientswithnoMBcomplaints,treatedatthe pediatric and speech therapy outpatient clinic for other complaintsthat wereallocatedinthe nasalbreather(NB) group.
Patientsample sizewascalculatedusingtwo compara-tivestudies12,13 involving twoproportions:the comparison
of pulmonary hypertension (PH) prevalence in the MB versus the prevalence of PH in the NB group. Consid-ering the prevalence of 10%12 in NB and 60%13 or more
in MB, in order to detect differences between the two groups in at least 50% (˛=0.05 and ˇ=0.10), it would
be necessary to have at least 21 patients in each
group.
At the selection procedure, patients underwent anam-nesis,complete otorhinolaryngological examination, aller-gologicevaluation withskin test punctureanda multidis-ciplinary evaluation (physical therapist, orthodontist and speech therapist). Together with the subjective evalua-tionof nasal obstruction, all patients underwent anterior activerhinomanometry (RAA)and Doppler echocardiogra-phic assessment. Patients who met the following criteria wereselected:
Inclusion criteria --- We included MB patients with tonsillarhyperplasia gradeIIIor IVand/or adenoid hyper-plasiawithnasopharynxobstruction ≥75%,24 confirmedby
otorhinolaryngologicalexaminationand fibronasopharyngo-laryngoscopy(ATH group) and clinical diagnosis of rhinitis withpositiveskintest(ARgroup).
• ATH group: mouth breathing children with hyperplasia of the palatine tonsil grade III and grade IV and/or adenoidhyperplasiawithnasopharynxobstruction≥75%, confirmed by otorhinolaryngological examination and fibronasopharyngolaryngoscopy,withor without positive skintest;
• ARgroup:mouth breathingchildren withoutobstructive adenotonsillarhyperplasiaandwithnasalhyperreactivity andpositiveskintest;
• NBgroup:nasalbreathingchildrenwithoutadenotonsillar hyperplasiaandnegativeskintest.
Exclusion criteria --- Patients with heart disease; pre-vious craniofacial and respiratory system surgeries; skin lesionsthatpreventedtheperformanceofskinallergictest (SAT); respiratory infection in the upperand low respira-torytractsinthelast14days;chroniccomorbidities;tobe usingor havingusedthefollowingmedications:intranasal corticosteroids, anticholinergics,systemic or topical vaso-constrictor,nasalcromolyn orother nasaldecongestantin thepastfourweeks;antihistaminesinthelasttwoweeks; oralcorticosteroids andleukotrienereceptorantagonistin thelasteightweeks;specificimmunotherapy inthepast3 months;andthosewhodidnotsignthefreeandinformed consent(FIC)formwereexcluded.4,9,12,25---27
Operationaldefinitions
Thestudyconsistedofthreestages:1---selectionofMBand NBin pediatricclinicsandreferraltothespecialized cen-ter;2---evaluationofreferralsfordiagnosticconfirmationor exclusionoftheOBSandforetiologicaldiagnosisand classifi-cationofATH;3---performingtheDopplerechocardiography todiagnosePH.
All patients, MB and NB, were submitted to com-pleteotorhinolaryngologicalexamination,allergyskintest, fibronasopharyngolaryngoscopyandactiveanterior rhinom-etry. Tonsil size wasclassified according to the Brodsky’s criteria,27consideringthedegreeoforopharyngeal
obstruc-tion. Adenoid hyperplasia was rated by nasal endoscopy accordingtothepercentageofchoanallumenobstruction degree.1,24
Allpatients underwent Doppler echocardiographywith color flow mapping using Phillips® IE 33 device. For the
SPAP analysis, tricuspid regurgitation measurement was performed using the apical window in the apical four-chamber view, measuringsystolic peakvelocityand using Bernoulli’sformula;theMPAPestimatewasperformedusing the formula:MPAP=0.61×SPAP+2mmHg28;in additionto
Table1 Demographicandanthropometricdata.
NB(n=25) ATH(n=54) AR(n=24)
Mean (SD) Mean (SD) Mean (SD)
Malegender(%/n) 32.0% 8 57.4% 31 58.3% 14
Age(years)a 7.30 (2.47) 6.04b (2.24) 7.42 (2.05)
Weight(kg) 27.92 (11.07) 22.83 (8.20) 25.36 (8.79)
Height(m)a 1.27 (0.17) 1.15b (0.15) 1.23 (0.15)
BMI(kg/m2) 16.24 (2.77) 16.57 (2.63) 16.08 (2.18)
a StatisticallysignificantdifferencebetweengroupwithARandgroupwithATH(p<0.05). b StatisticallydifferentfromtheNBgroup(p<0.05).
The echocardiographerswereunawareofwhichgroup the patientbelongedto.
Analyzedvariable
MPAPandSPAP
Accordingtothe recommendationsof the‘‘Guidelinesfor thediagnosisandtreatmentofpulmonaryhypertension’’,15
PH consists in MPAP≥25mmHg. When MPAP is between 20mmHgand24mmHg,analteredMPAPisconsidered,but aswe donot know thesignificance of itsclinical impact, it is not considered asPH. The value for SPAP≥35mmHg is also considered diagnostic in some studies, as well as TAc≤100ms.12,28
Statisticalanalysis
Categorical data are shown asnumbers and percentages, andcontinuousdataasmeanandstandarddeviation. Cat-egoricalvariablesofpatients andcontrolswerecompared usingthe chi-square test. Continuous variables were ana-lyzedby Student’sttest. Comparisonsbetweenthestudy groups werecarriedoutthroughbilateralhypothesis tests consideringasignificancelevelof5%(=0.05).
Results
The study population consisted of 54 chronic mouth breatherswithATH andsurgical indicationfor adenoidec-tomyand/or tonsillectomy(31males, witha meanageof 6.04±2.24 years and mean BMI of 16.57±2.63) and 24 patientswithpersistentAR(14males,withameanageof 7.42±2.05yearsandmeanBMIof16.08±2.18)compared to25healthy patientswithout UAO.There wasa statisti-callysignificantdifferenceinageandheight,withthemean heightandagebeinglowerintheATHgroup.However,there werenosignificant differencesingender,weightandbody massindex(BMI)(Table1).
Regardingthehistoryobtainedatthereferraloutpatient clinicanddirectedtoparents and/orguardiansof theMB aboutthebehavioroftheirchildrenduringsleep,allofthem reportedmouth breathing. Among the complaintsrelated to OSA, all patients with adenotonsillar hypertrophy and 19patients (79.2%) fromtherhinitis group complainedof snoring,while breathing pauses suggestiveof apnea were prevalentin 62.7% and 39.1% in the ATH and AR groups, respectively.Regardingadenoidhyperplasiawithindication foradenoidectomy,42patients(77.7%)hadadenoids occu-pying75%ormoreofthenasopharynx,and17(31.4%)had adenoids occupying 90% or more. Allergic rhinitis with a
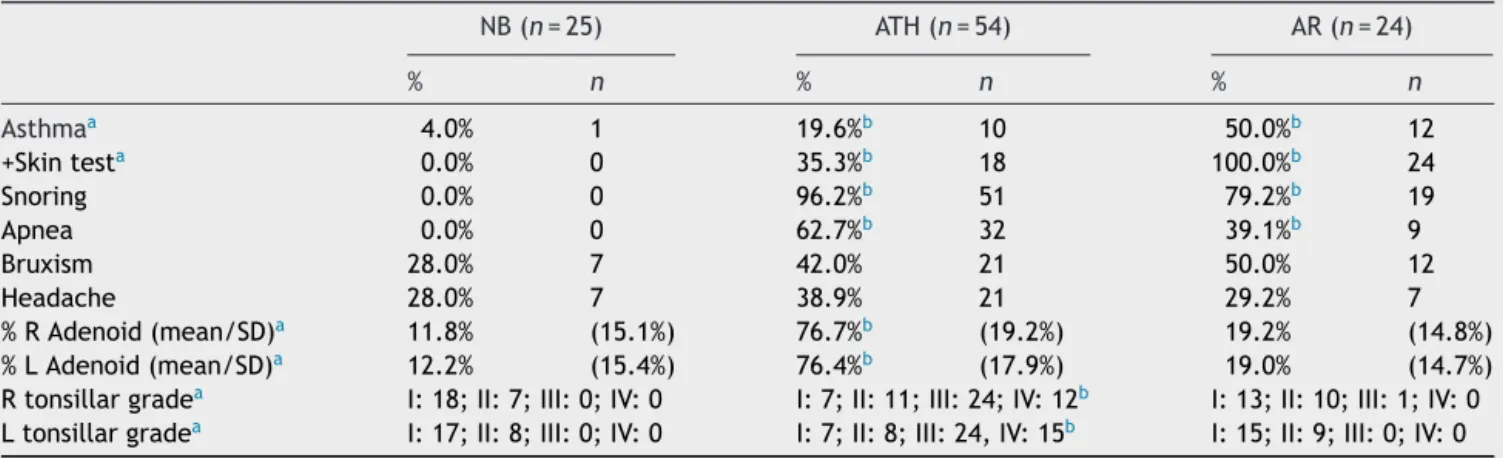
Table2 Dataobtainedfromthehistoryandphysicalexaminationofpatientsatthefirstconsultationatthereferralclinic.
NB(n=25) ATH(n=54) AR(n=24)
% n % n % n
Asthmaa 4.0% 1 19.6%b 10 50.0%b 12
+Skintesta 0.0% 0 35.3%b 18 100.0%b 24
Snoring 0.0% 0 96.2%b 51 79.2%b 19
Apnea 0.0% 0 62.7%b 32 39.1%b 9
Bruxism 28.0% 7 42.0% 21 50.0% 12
Headache 28.0% 7 38.9% 21 29.2% 7
%RAdenoid(mean/SD)a 11.8% (15.1%) 76.7%b (19.2%) 19.2% (14.8%)
%LAdenoid(mean/SD)a 12.2% (15.4%) 76.4%b (17.9%) 19.0% (14.7%)
Rtonsillargradea I:18;II:7;III:0;IV:0 I:7;II:11;III:24;IV:12b I:13;II:10;III:1;IV:0 Ltonsillargradea I:17;II:8;III:0;IV:0 I:7;II:8;III:24,IV:15b I:15;II:9;III:0;IV:0
a StatisticallysignificantdifferencebetweengroupwithARandgroupwithATH(p<0.05). b StatisticallydifferentfromtheNBgroup(p<0.05).
Table3 MeanvaluesofSPAP,MPAPandTAc.
NB(n=25) ATH(n=54) AR(n=24)
Mean(SD) Mean(SD) Mean(SD)
SPAP(mmHg) 21.64(3.87) 25.61a(3.38) 25.33a(2.06)
MPAP(mmHg) 15.20(2.36) 17.62a(2.06) 17.45a(1.25)
TAc(mmHg) 127.24(12.81) 114.06a(10.63) 117.96a(10.28)
aStatisticallydifferentfromtheNBgroup(p<0.05).
StatisticallysignificantdifferencebetweentheARgroupandgroupwithATH(p<0.05).
30
25
20
SP
AP (mmHg)
Nasal breathers ATH AR
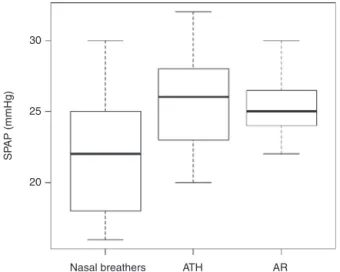
Figure1 Boxplotgraphshowingtheassociationbetweenthe SPAPintheMBandNBgroups.
positiveskin testwasdetectedin18(35.3%)patientswith ATH(Table2).
Amongtheechocardiographicfindings,weobserveda dif-ferenceregardingMPAPandSPAP,beinghigherintheMBthan theNBgroup(17.62±2.06(ATH)and17.45±1.25(AR)vs. 15.20±2.36and25.61±3.38mmHg(ATH)and25.33±2.06 (AR)vs.21.64±3.87mmHg,p<0.005,respectively),while TAcwas higherin NB (127.4±12.81 vs.114.06±10.63ms (ATH)and117.96±10.28,p<0.0001).Therewasno signifi-cantdifferencebetweenSPAP,MPAPandTAcvaluesamong mouthbreatherswhenconsideringthedifferentetiologies, ATHandAR(Table3).
NochildhadPHattheechocardiography.Sevenpatients
with ATH (12%) had MPAP≥20mmHg, but none had
MPAP≥25mmHg. The rhinitis group and NB group had a patientwithMPAP≥20mmHgeach.TAcrangedfrom84to 136ms in the ATH group, from 96 to 142ms in patients withARand100to146msinthegroupofnasalbreathers. TAc≤100mswasfound in sixpatients withadenotonsillar hypertrophy(11%),inonepatientoftheNBgroupandinone patientoftheARgroup.SPAPrangedfrom19to32mmHg in patients fromthe ATH group and from22 to32 in the ARgroup,whereasintheNBgroupSPAPrangedfrom16to 30mmHg(Fig.1).
Discussion
In this study, statistically significant differences were observedbetweentheoralandnasalbreathersinrelation
toPH measures (SPAP, MPAPand TAc), whichindicate the riskofdevelopmentoffutureirreversiblecardiopulmonary complications.However,nopatienthadadiagnosisof PH, contrarytowhatisdescribedintheliterature.
Naibogluetal.assessedthechangeinPulmonaryArtery Pressure (PAP)inchildren withadenotonsillectomy indica-tioncomparedtoacontrolgroup.Ofthe39patientswith upperairwayobstruction,84%wereconsideredhypertensive duetoincreasedMPAP,whereasinthecontrolgrouponlytwo patientswereclassifiedashypertensive.However,theused cutoffvaluewas20mmHgandthecalculationofMPAPwas performed throughTAc, which is an unreliable parameter whenitisnotcorrectedbytheheartrate.12
InastudycarriedoutbyYilmaz13etal.(2005),52children
wererandomlyselected,agedbetween4and11years,with thediagnosisofUAOsecondarytoATHand33childreninthe controlgroup. MPAPlevelswerecomparedbetween cases and controls, and the first group had significantly higher blood pressure levels (MPAP of 23.13±7.68 in cases and 16.11±7.24incontrols).
AsintheNaibogluwork,Yilmazetal.classifiedas hyper-tensivethosepatientswithMPAP>20mmHg.However,the prevalenceofPHwaslowerwiththeinvolvementof51%of patients withadenotonsillectomy indication,comparedto 3%inthecontrolgroup.Bothstudiesevaluatedthereversal ofMPAPvaluesaftertheadenotonsillectomyandfound sim-ilarpressurevaluestothoseinthecontrolgroupafterthe procedure.12,13
Inadditiontotheaforementionedstudies,arecentone byMarthaetal.analyzedSPAPandMPAPvaluesin33 chil-dren withadenotonsillarhypertrophy and comparedthem with10controlpatients.ThediagnosisofPAHwasachieved throughDopplerechocardiographicevaluationandpatients withSPAP≥30mmHg or MPAP≥25mmHgwereconsidered hypertensive.Theprevalenceofhypertensionwas36%inthe ATHgroup,alowervaluethaninotherstudies.The evalua-tionofsystolicpressurewasmadebytricuspidregurgitation, whereasinpatientswithoutthisregurgitation,MPAPwas cal-culatedfromTAc.Inthegroupof19patientsinwhichthe evaluationwasperformed bytheMahan formula,a calcu-lationthatdependsontheTAcvalue,theprevalenceofPH washigher.6
Incontrasttothe aforementionedstudies, thepresent study also assessed the impactof allergic rhinitis on pul-monary pressure and compared the findings to the group withadenotonsillarhypertrophy.Althoughtherehavebeen fewstudiesonARandPH,9,10wecandemonstratethatthe
The association between allergic rhinitis (AR)and pul-monary hypertension was also evaluated in a study with 35patientsthatcorrelatedsymptomseveritywithchanges in echocardiography in patients with seasonal allergic rhinitis. The literature showed an increase in PAP during patients’symptomaticperiods,withareductioninPAP val-ues during the asymptomatic period. The symptom that showed a higher correlation with PAP results was nasal obstructionseverity,indicatingapreviouslydiscussed asso-ciation of nasal resistance increase with cardiopulmonary alterations.10
Some12 studies use TAc to evaluatePH with the
refer-ence value (limit of normality)of 100ms.This methodis often used in adults, but has limitations in children with elevatedheartrate,asitcansignificantlyinfluencethe pat-ternoftheoutflowtractvelocitycurveandtheacceleration time.Therefore,othermethodsarerecommended, particu-larlythoseusingcontinuousDoppler,sinceitallowsindirect measurementoftheSystolicPulmonaryArteryPressureby assessingtricuspidregurgitation.29 Inthepresentstudy,we
usedthemeasurederivedfromtricuspidregurgitation,the most recommendedmethod andthe onewithlower inter andintraobservervariability.
This studyisrelevantfor theliterature,asitcan influ-enceclinicalpracticethroughanewapproachproposalfor MB,inadditiontowarnagainstcardiopulmonaryrisksthat arenotasyetwell established.The careof patientswith UAOshouldnotfocusonlyonpatientswithATH,aschanges inpulmonarypressurewerecomparableinpatientswithATH andAR.Thus,theearlyidentificationofpatientsatriskfor PHisimportant,asitisdirectlyrelatedtoprognosisbecause of thepotentialreversibility of thepicture, when correc-tivesurgicalprocedureand/ordrugtreatmentindicationare carriedoutinatimelymanner.6,9,12,13
Conclusion
AlthoughnoMBintheassessedsamplewasdiagnosedwith PH, bothSPAP andMPAP, measured byDoppler echocardi-ography,showedincreasedmeanswhencomparedtonasal breathers,i.e.,thenormalstandard.Thisfactmaypose a greaterriskforfutureheartcomplicationsinpatientswith MBS.
Patients with allergic rhinitis showed elevated values of MPAP and SPAP that were similar to thoseobtained in patientswithupperairwayobstructionduetoadenotonsillar hypertrophy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.BeckerHMG,GuimaraesRES,PintoJA,VasconcellosMC. Respi-radorbucal.In:LeãoE,editor.Pediatriaambulatorial.5thed. BeloHorizonte:Coopmed;2012.
2.SafferM.Mouthbreather.In:IIIAPO/IFOSpediatricentmanual; 2002.p.166---77.
3.Chedid KAK, Difrancesco RC, Junqueira PAS.A influência da respirac¸ãooralnoprocessodeaprendizagemdaleituraeescrita emcrianc¸aspré-escolares.RevPsicopedag.2004;21:157---63. 4.BarrosJulianaRC,BeckerHMG,PintoJA.Avaliac¸ãodeatopiaem
crianc¸asrespiradorasbucaisatendidasemcentrodereferência. JPediatr.2006;82:458---64.
5.Abreu RR, Rocha RL, Lamounier JA, Guerra AFM. Etiologia, manifestac¸õesclínicasealterac¸õespresentesnascrianc¸as res-piradorasorais.JPediatr.2008;84:529---35.
6.Martha AS, Velho FJ, Eick RG, Goncalves SC. Reversal of pulmonary hypertension in children after adenoidec-tomy or adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2013;77:237---40.
7.KocS,AytekinM,KalayN,OzcetinM,BurucuT,OzbekK,etal. The effectofadenotonsillectomyon right ventriclefunction andpulmonaryarterypressureinchildrenwithadenotonsillar hypertrophy.IntJPediatrOtorhinolaryngol.2012;76:45---8. 8.Miman MC, Kirazli T, Ozyurek R. Doppler echocardiography
inadenotonsillarhypertrophy.IntJPediatrOtorhinolaryngol. 2000;54:21---6.
9.YükselH,Cos¸kunS,Ona˘gA.Dopplerechocardiographic eval-uationofpulmonaryarterialpressureinchildrenwithallergic rhinitis.IntJPediatrOtorhinolaryngol.2001;60:21---7. 10.BayrakP,KirmazC,SekuriC,YukselH. Ispulmonaryarterial
pressure affected by allergicrhinitiswith nasal obstruction? AsianPacJAllergy.2007;25:121---6.
11.DiFrancesco RC, FortesFSG, Komatsu CL.Melhora da quali-dadedevidaemcrianc¸asapósadenoamigdalectomia.RevBras Otorrinolaringol.2004;70:748---51.
12.Naiboglu B, Deveci S, Duman D, Kaya KS, Toros S, Kinis V, et al. Effect of upper airway obstruction on pulmonary arterial pressure in children. IntJ Pediatr Otorhinolaryngol. 2008;72:1425---9.
13.Yilmaz MD, Onrat E, Altuntas A, Kaya D, Kahveci OK, Ozel O,et al.Theeffectsoftonsillectomyandadenoidectomyon pulmonary arterial pressure in children. Am J Otolaryngol. 2005;26:18---21.
14.Abdel-AzizM.Asymptomaticcardiopulmonarychangescaused byadenoidhypertrophy.JCraniofacSurg.2011;22:1401---3. 15.Galie N, Hoeper MM, Torbicki A, Vachiery JL, Barbera JA,
BeghettiM,etal.Guidelinesforthediagnosisand treatment ofpulmonaryhypertension.EurHeartJ.2009;30:2493---537. 16.SpektorS,BautistaAG.Respiratoryobstructioncausedbyacute
tonsillitisandadenoiditis.JMed.1956;56:2118---21.
17.Noonan JA. Reversible cor pulmonale due to hypertrophied tonsils and adenoids: studies in two cases. Circulation. 1965;31/32:164---8.
18.MenascheVD,FarrehiC,MillerM.Hypoventilationandcor pul-monale due to chronic upper airway obstruction. J Pediatr. 1965;67:198---203.
19.LukeMJ,MehriziA,FolgerGM,RoweRD.Chronic nasopharyn-gealobstructionasacauseofcardiomegaly,corpulmonaleand pulmonaryedema.Pediatrics.1966;37:762---8.
20.MacartneyFJ,PandayJ,ScottO.Corpulmonaleasaresultof chronicnasopharyngealobstructionduetohypertrophied ton-silsandadenoids.ArchDisChild.1969;44:585---92.
21.CronjeRE,HumanGP,SimsonL.Hypoxemicpulmonary hyper-tensioninchildren.SAfrMedJ.1966;8:40---2.
22.SchiffmannR,FaberJ,EidelmanAI.Obstructivehypertrophic adenoidsand tonsilsasacauseofinfantile failuretothrive: reversed by tonsillectomy and adenoidectomy. Int J Pediatr Otorhinolaryngol.1985;9:183---7.
23.TrowTK,McardleJR.Diagnosisofpulmonaryarterial hyperten-sion.ClinChestMed.2007;28:59---73.
25.EAACI.Positionpaper:allergenstandardizationandskintests. TheEuropeanAcademyofAllergologyandClinicalImmunology. Allergy.1993;48:48---82.
26.McGoonMD.Theassessmentofpulmonaryhypertension.Clin ChestMed.2001;22:493---508.
27.BrodskyL.Modernassessmentoftonsilsandadenoids.Pediatr ClinNorthAm.1989;36:1551---69.
28.Chemla D, Castelain V, Humbert M, Hébert JL, Simonneau G, Lecarpentier Y, et al. New formula for predicting mean pulmonaryarterypressureusingsystolicpulmonaryartery pres-sure.Chest.2004;126:1313---7.