Brazilian
Journal
of
OTORHINOLARYNGOLOGY
www.bjorl.org
ORIGINAL
ARTICLE
Dysphagia
progression
and
swallowing
management
in
Parkinson’s
disease:
an
observational
study
夽
,
夽夽
Karen
Fontes
Luchesi
∗,
Satoshi
Kitamura,
Lucia
Figueiredo
Mourão
UniversidadeEstadualdeCampinas(UNICAMP),Campinas,SP,Brazil
Received1June2013;accepted3March2014 Availableonline8October2014
KEYWORDS Parkinsondisease; Deglutition;
Diseaseprogression; Deglutitiondisorders; Speechtherapy
Abstract
Introduction:Dysphagiaisrelativelycommoninindividualswithneurologicaldisorders.
Objective:To describethe swallowingmanagementand investigate associated factorswith swallowinginacaseseriesofpatientswithParkinson’sdisease.
Methods:Itisalong-termstudywith24patients.Thepatients wereobservedinafive-year period (2006---2011).Theyunderwent FiberopticEndoscopicEvaluation ofSwallowing, Func-tionalOralIntakeScaleandtherapeuticinterventioneverythreemonths.Inthetherapeutic interventiontheyreceivedorientationaboutexercisestoimproveswallowing.TheChi-square, Kruskal---WallisandFisher’stestswereused.Theperiodoftimeforimprovementorworsening ofswallowingwasdescribedbyKaplan---Meieranalysis.
Results:Duringthefollow-up,tenpatientsimproved,fivestayedthesameandnineworsened theirswallowingfunctionality.Themediantimeforimprovementwastenmonths.Priortothe worseningtherewasamediantimeof33monthsoffollow-up.Therewasnoassociatedfactor withimprovementorworseningofswallowing.The maneuversfrequently indicatedin ther-apeuticinterventionwere:chin-tuck,bolusconsistency,boluseffect, strengthening-tongue, multipleswallowsandvocalexercises.
Conclusion:Theswallowingmanagementwascharacterized byswallowingassessmentevery threemonthswithindicationofcompensatoryandrehabilitationmaneuvers,aimingtomaintain theoralfeedingwithoutrisks.Therewasnoassociatedfactorwithswallowingfunctionalityin thiscaseseries.
© 2014Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:LuchesiKF,KitamuraS,MourãoLF.DysphagiaprogressionandswallowingmanagementinParkinson’sdisease: anobservationalstudy.BrazJOtorhinolaryngol.2015;81:24---30.
夽夽
Institution:UniversidadeEstadualdeCampinas,Campinas,SP,Brazil.
∗Correspondingauthor.
E-mail:karenluchesi@yahoo.com.br(K.F.Luchesi). http://dx.doi.org/10.1016/j.bjorl.2014.09.006
1808-8694/©2014Associac¸ãoBrasileiradeOtorrinolaringologia eCirurgiaCérvico-Facial. PublishedbyElsevierEditoraLtda.All rights
DysphagiaprogressionandswallowingmanagementinParkinson’sdisease 25
PALAVRAS-CHAVE Doenc¸adeParkinson; Deglutic¸ão;
Progressãoda doenc¸a; Transtornosde deglutic¸ão; Fonoterapia
Progressãoetratamentodadisfagianadoenc¸adeParkinson:estudoobservacional
Resumo
Introduc¸ão: Adisfagiaéfrequenteemindivíduoscomdistúrbiosneurológicos.
Objetivo: Descreverotratamentodadisfagiaeinvestigarfatoresassociadosàdeglutic¸ãoem umasériedecasoscomdoenc¸adeParkinson.
Método: Trata-sedeumestudolongitudinalcom24pacientesacompanhadosporumperíodode cincoanos(2006---2011).Todosforamsubmetidosàvideoendoscopiadadeglutic¸ão,classificac¸ão deacordocomaFunctionalOralIntakeScale(FOIS)ereceberamorientac¸õessobreotratamento dadeglutic¸ãoacadatrêsmeses.Asorientac¸õesdotratamentodadeglutic¸ãocompreenderam exercíciosparaamelhoradadeglutic¸ão.OstestesQui-quadrado,Kruskal---WalliseFisherforam utilizadosparainvestigarassociac¸ãoentreoestadodadeglutic¸ãoevariáveisclínicas.
Resultados: Duranteoacompanhamento,dezpacientesmelhoraram,cincomantiveramenove pioraramafuncionalidadedadeglutic¸ão.Umamedianadedezmesesfoiobservadaatéa mel-horanadeglutic¸ãoserobtida.Foiobservadaumamedianade33mesesdeacompanhamentoaté apioranadeglutic¸ão.Asmanobrasmaisfrequentementeindicadasnaterapiaforam:queixo parabaixo,mudanc¸anaconsistênciaenoefeitodobolo,exercíciosparaforc¸aemobilidadede língua,deglutic¸õesmúltiplaseexercíciosvocais.
Conclusão:Otratamentodadisfagiafoicaracterizadoporavaliac¸õestrimestraisdadeglutic¸ão comindicac¸ãodemanobrascompensatóriasereabilitadoras.Nestacasuísticanãoforam iden-tificadosfatoresassociadosàsmudanc¸asnafuncionalidadedadeglutic¸ão.
©2014Associac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicado por ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Dysphagia is common in individuals with neurological disorders. It affects food intake, which may lead to complicationssuchaschoking,malnutrition,andpulmonary aspiration.1
Parkinson’s disease (PD) is one of the most com-monneurodegenerative disease inthe elderlypopulation, with a worldwide incidence between 1 and 20 per 1000people/year.2,3 It is characterized by impairment of
basal ganglia in voluntary movements, causing resting tremor, rigidity, akinesia (or bradykinesia), and postural instability.2,4
Dysphagiais verycommonin PD,affectingover 80%of individuals, reflecting the underlying motor impairments andtheextentofthedisease’sprogression.5Theswallowing
difficultiesmostfrequentlyassociatedwithPDarerelated to the oral and pharyngeal phase, resulting in abnormal bolus formation,delayed swallowingreflex,and prolonga-tionofthepharyngealtransittime,withrepetitiveswallows toclearthethroat.6
Thesedysphagia-relatedimpairmentshaveadirect influ-enceonthenutritionalandhealthstatusofthepatients,and are associated with increased morbidity and mortality.7,8
However,fewstudieshavedescribedtheprogressionof dys-phagiaanditsseverityinPD.9Thereisverylittleinformation
regardingthetemporalaspect ofdysphagia progressionin PD.
KnowledgeondysphagiaprogressioninPDcoulddecrease theriskof aspirationpneumonia,consequentlydecreasing theriskofdeath,sinceitisoneofthemostfrequentcauses of deathin thispatients.10,11 It canalso orient physicians
andtherapistsonwhattoexpectoftheirpatientsandwhich treatmentmaybenecessaryovertime.
Swallowing management, through the utilization of methodsthat compensate for the alterationsin the swal-lowingprocess,aimstopreserveasafeoralfeedingaslong aspossible. Swallowing management is based on maneu-vers that, according to Crary,12 can be categorized as
compensatoryandrehabilitationmaneuvers.Compensatory maneuvers refer to behavioral intervention in dysphagia, characterizedbydietarymodifications,changesinthe man-ner of administrationof the diet, changes in the patient position,andalterationsin themechanism of swallowing. These maneuvers,such aschin-tuck, head rotation,head tilt, head back, among others, are commonly known as postural maneuvers. Their purpose is to direct the bolus andmodifytheflow velocityofthebolus. Themaneuvers characterizedbydietmodificationspromotechangesin sen-sorystimuli, as modifying volume and consistency of the foodmayaltersensoryinput.Themodificationofthe swal-lowingmechanismrequireschangesinswallowingpattern, regardingmusclestrength,rangeofmotion,and coordina-tionofeventsinswallowing,forexampleeffortswallowing, supraglotticmaneuver,multipleswallows,betweenothers. Among rehabilitation maneuvers are the sensor-motor oralexercises,whichenablemodificationsofforce,length, andrangeof motionofthestructuresinvolvedin theoral cavity,pharynx,andlarynx.Amongthemostusedmaneuvers arethe shakermaneuver, lingual control,vocal exercises, andpharyngealexercises.
Methods
Selectionofpatients
This was a prospective long-term study of 24 dysphagic patients with idiopathic PD, followed-up for a five-year period(2006---2011)inalargeBrazilianuniversityhospital. Thiswasanopen caseseriesand,duringthefiveyearsof study,somepatientsdroppedout.Thepatientswereinuse ofmedicineswithLevodopa.
Only the patients who had at least three evaluations, complaintsofswallowing,exclusiveoralfeeding,and regu-larcheck-upswithanoutpatientneurologistwereincluded inthe study.Patientswithnon-oral feeding and concomi-tantdiseasesordisordersthatcouldcausedysphagiawere excluded.
Procedures
Patients underwent swallowing evaluation, assessment throughtheFunctionalOralIntakeScale(FOIS),13and
ther-apeuticinterventioneverythreemonths.
The swallowing evaluation was obtained through a fiberopticendoscopic evaluationof swallowing(FEES)and clinically. In both evaluations, three types of food were offered:(1)lemonjuicecoloredwithgreenfoodcoloring; (2) Nectar, honey, and pudding consistencies, all colored withgreenfoodcoloring (thesefluids wereobtained with theadditionof two,three, andfourteaspoonsofa thick-ener[Thicken-easy®]to100mLofwater,respectively,and
wereofferedintwodifferentquantities,3mLand7mL);(3) solidconsistency,representedbyacornstarchbiscuit.
Thefoodwasgiventopatientsinthefollowingsequence: liquidandnectar(3mLand3mL,respectively,followedby 7mLand7mL,respectively);honey(3mLand3mL, respec-tively, followed by 7mL and 7mL, respectively); pudding (twotablespoons); solid(½ cornstarchbiscuit).Theliquid
foodwas administered in 20mL syringes, and the sample wasintroducedintothepatient’soralcavity.Asdifficulties inswallowingwereobserved,airwayprotectivemaneuvers and/orchangesinheadposturewereperformedinorderto assistoralfeedinginasafeway.
FEES was conducted by an otolaryngologist, while the foodwasofferedbyaspeech-languagetherapist.
Intheclinicalevaluation,asthepatientsswallowed, cer-vicalauscultationwasperformedtoidentifyabnormalsigns atthepharyngealswallowingphase.Oralbolustransittime, anteriororposteriorescape,positivecervicalauscultation (with signs that indicate a presence of stasis or penetra-tionwithaspirationrisk),coughing(before,during,orafter swallowing),andwetvoicewerealsoobservedbya speech-languagetherapist.
Based on the clinical evaluation and FEES, the FOIS13
wasapplied.The FOIS rankspatients intolevels,adapted tothe present study asfollows: level 1,No oral feeding; Level2,tube-dependentwithminimalattemptsoffoodor liquid;Level3,Tube-dependentwithconsistentoralintake offoodorliquid;Level4,Completeoraldietofoneortwo consistencies(nectarandhoney,honeyandpudding);Level 5a,Completeoraldietwithmultipleconsistenciesbutwith restrictions in two consistencies (for example, solid and
liquid),withorwithoutcompensation;Level5b,Complete oral diet with multiple consistencies but with restriction of one consistency (for example, solid or liquid), withor without compensation; Level 5c,Complete oral diet with multiple consistencies, but requiring compensation; Level 6, Completeoral diet withmultiple consistencieswithout special preparation but with specific food limitations (for example: fibers, grains, and some vegetables) and speed andvolume modificationif necessary; andLevel 7, Completeoraldietwithnorestriction.
Atthe initial evaluation,every patientreceiveda cor-responding FOIS classification. Every time the patients returnedtothehospitaltheywerereevaluatedand reclas-sified underFOIS. To analyzethe swallowingfunctionality byKaplan---Meiersurvivalanalyses,patientswereobserved until occurrence of the event improvement or the event worsening, i.e.,theywereobserveduntilthepoint ofthe timeatwhichafallorriseinFOISwasnoted.Patientswhose swallowing functionality stayed the same were observed duringthefollow-upperiodandnoeventwasregistered.
Following these swallowing evaluations, patients received therapeutic intervention every three months regarding adequate food consistency and volume, in additiontomaneuversor exercisestoimproveswallowing functionality.Theywereorientedtoperformthemaneuvers dailyandreceivedwritteninstructionsforeachone.
Thecompensatorymaneuversusedwere(1)chin-tuck,to improveairwayprotectionduringswallowing;(2)bolus con-sistency,tofacilitatethefeedingofpatientswithdecreased coordinationoftongue,reducedcontractionofpharynges, delayintriggeringswallowingreflex,reducedairway protec-tionandchewingdifficulty;(3)effortfulswallow,toincrease strengthtoejectthebolusandtoapproximatethelarynx structures, improving airway protection; (4) frequency of swallowing(multipleswallows),toclearstasis;and(5)bolus effects,i.e.changesinvolume,viscosity,temperature,or taste,wereintroducedinordertoimproveoraland pharyn-gealsensibilityandcontrolbolusmanagement.
The following rehabilitation maneuvers were used (1) tongue strengthening, to increase strength to eject the bolus; (2)tongue control,toimprovetonguemobility and facilitate the bolus management in the oral cavity; (3) Shakermaneuver,toincreasestrengthinsuprahyoid mus-cles reducing the penetration and aspiration risk due to stasis in pyriform sinus; (4) vocal exercises, to improve airway protection though the improvement in the glot-tis adduction; (5) tongue holding (Masako maneuver), to increasemovementsofpharyngealmusclesagainstthebasis ofthetongueduringtheactofswallowing.
Dataanalysis
The patients were classified according to changes in swallowing functionality measured by FOIS, grouped as: improved,nochange,andworsened.
DysphagiaprogressionandswallowingmanagementinParkinson’sdisease 27
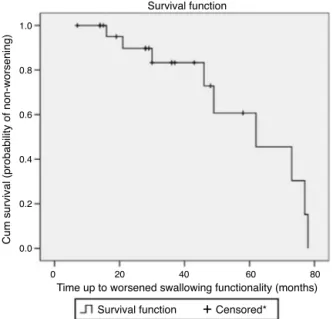
Theswallowingfunctionalityovertimewasdescribedby Kaplan---MeierSurvivalAnalysis.It isimportanttomention thattheresultsofasurvivalanalysisexpresstheprobability ofthepatientnotsufferingfromagiveneventovertime.
The statistical analysiswas performed usingStatistical Package for the Social Sciences (SPSS), version 13.0 for Windows, and p-values lower than 0.05 were considered significant.
This studywasapprovedbytheEthicBoardCommittee oftheUniversityofCampinas(Protocolnumber796/2005).
Results
Thegroupof24patientscomprised16menand8women. TheaverageageofonsetofPDsymptomswas53.8(±6.5) years. The average age for the first evaluation was 65.4 (±8.6)years.Theaveragediseasedurationwas139.2(±65) months,i.e.,anaverageof11yearsbetweenthefirst symp-tomsandthefirstevaluationforswallowingmanagement.
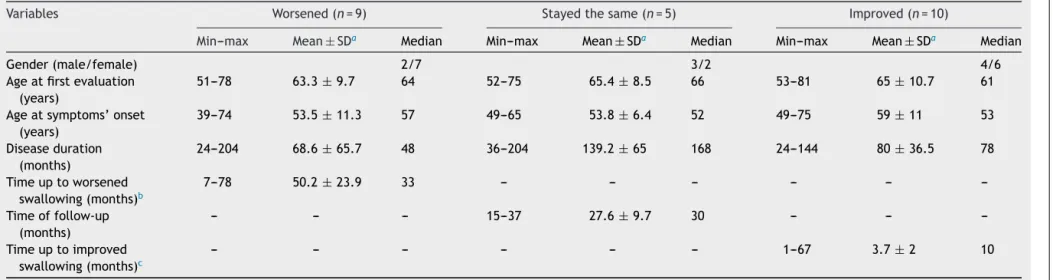
Ten patients improved, five presented no change, and nineworsenedtheirswallowingfunctionalityduring follow-up. The characteristics of these groups are described in
Table 1. There was no statistically significant difference betweenthegroups.
Noneoftheinvestigatedvariableswasstatistically asso-ciatedwithswallowingfunctionalityinthiscaseseries.
Fig.1showsthesurvivalcurveoftheworsened swallow-inggroup.Thiscurveillustratesthechanceofnotsuffering fromworseningofswallowinginthiscaseseries.
The patients gradually lost swallowing functionality. AccordingtoKaplan---Meieranalysis,theyhad17% probabil-ityofworsenedswallowingfunctionalityatthetenthmonth offollow-up.
+
1.0
0.8
0.6
0.4
0.2
0.0
Survival function
C
um survival (probability of non-worsening)
Survival function Censored*
0 20 40 60 80
Time up to worsened swallowing functionality (months)
Figure 1 Survival plot considering worsened swallowing according to Functional Oral Intake Scale (FOIS) levels in Parkinson’sdiseasepatientsfollowedatadysphagiaoutpatient between2006and2011(n=24).*Censoredobservationshows patients lostinfollow-uporpatients withoutworsened swal-lowingfunctionalityduringtheobservationperiod.
0.6
0.5
0.4
0.3
0.2
0.1
0.0
Hazard function
C
um hazard (probability of improvement)
0 10 20 30 40 50 60 70
Time up to improved swallowing functionality (months)
Censored* Survival function
+
Figure 2 Hazard plot considering the improved swallow-ingaccordingto FunctionalOralIntake Scale(FOIS) levelsin Parkinson’sdiseasepatientsfollowedatadysphagiaoutpatient between2006and2011(n=24).*Censoredobservationshows patientslosttofollow-uporpatientswithoutimproved swal-lowingfunctionalityduringtheobservationperiod.
Fig.2showsthehazardfunctionoftheimprovementof swallowinggroup.Thiscurveillustratesthechanceof swal-lowingimprovement in thiscase series.The majority had improvedswallowingfunctionalityuptothetenthmonth. Accordingto theKaplan---Meier analysis, in tenmonths of follow-up, the probability of improvement in swallowing functionalitywas44%.
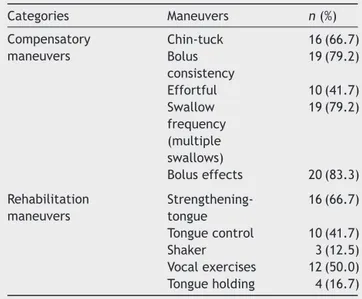
The frequencies of maneuvers indicated in the thera-peuticintervention are shown in Table 2. The maneuvers chin-tuck, bolus consistency, tongue strengthening, vocal exercises, swallow frequency,and bolus effect were sug-gestedto50%ormoreofthepatients.
Discussion
Inthiscaseseries,anaverageof11yearsbetweenPDonset andthepatient’sfirstevaluationatthedysphagiaoutpatient clinicwasobserved.Thiscouldbeexplainedbyseveral fac-tors,includinglack ofinformationor latencybetweenthe PDonsetandthebeginningofswallowingcomplaints. The literatureindicates that the delay in seeking professional assistance may be damaging, especially since dysphagia is prevalent in long-standing PD, but may be subclinical specially in the early course of the disease.5,14
Objec-tiveswallowingevaluationshaverepeatedlyfoundimpaired swallowingin over 50% of patients with PDwho reported noswallowingabnormalities.14 During thedisease course,
75---97% of the patients will suffer from dysphagia.15---17
Becauseoftheseevidences,itisimportanttopayattention toswallowing, always monitoring for weight loss, malnu-trition,andpulmonaryaspectsinordertoavoiddysphagia complications.
Mülleretal.,18 in apostmortemstudy,found amedian
Luchesi
KF
et
al.
Table1 DescriptiveanalysisofclinicalaspectsofacaseseriesofpatientswithParkinson’sdiseasefollowedinadysphagiaoutpatientbetween2006and2011,stratifiedby swallowingfunctionality(n=24).
Variables Worsened(n=9) Stayedthesame(n=5) Improved(n=10)
Min---max Mean±SDa Median Min---max Mean±SDa Median Min---max Mean±SDa Median
Gender(male/female) 2/7 3/2 4/6
Ageatfirstevaluation (years)
51---78 63.3±9.7 64 52---75 65.4±8.5 66 53---81 65±10.7 61
Ageatsymptoms’onset (years)
39---74 53.5±11.3 57 49---65 53.8±6.4 52 49---75 59±11 53
Diseaseduration (months)
24---204 68.6±65.7 48 36---204 139.2±65 168 24---144 80±36.5 78
Timeuptoworsened swallowing(months)b
7---78 50.2±23.9 33 --- --- --- --- ---
---Timeoffollow-up (months)
--- --- --- 15---37 27.6±9.7 30 --- ---
---Timeuptoimproved swallowing(months)c
--- --- --- --- --- --- 1---67 3.7±2 10
a Standard-deviation(SD).
b TimeestimatedfromtheonsetofParkinson’sdiseasesymptoms.
DysphagiaprogressionandswallowingmanagementinParkinson’sdisease 29
Table 2 Frequency of maneuvers recommended in the swallowing management in a case series of patient with Parkinson’s disease followed in a dysphagia outpatient between2006and2011(n=24).
Categories Maneuvers n(%)
Compensatory maneuvers
Chin-tuck 16(66.7) Bolus
consistency
19(79.2)
Effortful 10(41.7) Swallow
frequency (multiple swallows)
19(79.2)
Boluseffects 20(83.3)
Rehabilitation maneuvers
Strengthening-tongue
16(66.7)
Tonguecontrol 10(41.7)
Shaker 3(12.5)
Vocalexercises 12(50.0) Tongueholding 4(16.7)
approximately 14 years, and a dysphagia latency of 10 years. The authors demonstrated that disease durationis important,becausethelatencyofdysphagiacomplaintswas positivelycorrelatedwiththetotalsurvivaltime.
Thepresentstudyfoundnoassociationbetweengender andswallowingfunctionalityinPD.Intheliterature,a rela-tionshipbetweenbronchoaspirationandgenderwasalsonot observed.19,20Thesefactsrevealthataspectsrelatedto
gen-der,suchashormones,anatomicdifferences,amongother gender differences,appeartonotinfluence swallowingof PDpatients.
Althoughtheprogressiveimpairmentofswallowingisan expectedfact,inthisstudy,maintenanceor improvement ofswallowingfunctionalitywasobservedinthemajorityof thepatientsduringthefollow-upperiod.
There was no statistic difference found between the groups that presented no change, improved, or worsened swallowing functionality. Although this study did not find aspectsstatisticallyassociatedwithswallowingchangesin PDpatients,Lorefaltetal.21reportedasignificantreduction
of solid food intake in older patients with PD. The non-ingestion of solidfoods per seindicates a loss in FOIS. In PD,highermortalityisassociatedwithsomeaspects,such asolderage,dysphagia,andlatediagnosis.22 Accordingto
Auyeungetal.23theolderonsetisassociatedwithanegative
impactonsurvivalofPDpatient.
An earlierfirstevaluationandstartof swallowing man-agement in PD patient is very important. Manor et al.8
observed that, in PD, swallowing management in earlier stages of dysphagia wasable to preventaspiration pneu-monia and help in the maintenance of the quality of life. Therefore, early swallowing management may pos-itively affect swallowing functionality. According to the literature, compensatory maneuvers used in swallowing managementcanimproveairwayprotectionandreduce dys-phagiacomplications.24
DespitealackofblindcontrolledstudiesandalthoughPD is aprogressive andneurodegenerative disease,thereare
otherstudies indicatingthat improvementcanbebrought byrelativelysimpleinterventions.25,26Althoughthepresent
study did not aim to verify the efficacy of the methods of therapeutic intervention, the patients in this swallow-ing management group showed improvement in the first tenmonths.AccordingtoRobbins,12whensomemaneuvers
areperformedrepeatedly,theypromoteneuroplasticityand improvetheswallowingfunctionality.
SwallowingmanagementinPD
Theswallowingmanagementofpatientswith neurodegen-erativediseasesisrelativelyrecent;formanyyears,itwas believedthatdegenerativediseasewouldhaveaconsequent progressive dysphagia; swallowing could not be rehabili-tated, and thus any attempt to therapeutic intervention wouldbedoomedtofailure.
Theswallowingmanagementaimstoimprovethe swal-lowingactasmuchaspossibleandtocompensateforwhat cannotbesolved,inordertosavedeglutition.
As a result of this study, it was observed that one of themostrecommended interventionswere compensatory. Thegreater useof compensatorymaneuversin PDcanbe explainedbytheinstantaneousresultoftheseinswallowing, whatcanbeverifiedempiricallyinclinicalandinstrumental evaluation.
Compensatorymaneuvers are designed to redirect the bolusawayfromtheairway,withoutchangingairway phys-iology.The literatureelucidatesthat thickeningliquids to a nectar or honey consistency should be used because it exhibitsanimmediateeffect.27 Chin-tuckmaneuveris
fre-quentlyrecommendedforswallowingthinliquids.28 InPD,
there are evidences that the chin-tuck maneuver com-bined with thick liquid can be important in preventing pneumonia.20
In this swallowing management program, bolus consis-tencywasindicatedwhenothermaneuverswereinefficient tomaintainoralfeedinganditwasnecessarytoavoidthe consistenciesthatwerehazardous.
Forthepatientofthisstudy,theboluseffectmaneuver wasindicatedwhenthelackoforalcontrolmadeitdifficult toswallowquicklyandingreatervolumes.Theboluseffect, andchangesintheconsistency,taste,ortemperatureofthe bolus,improveoralintakeandpreventaspiration.
Other frequently indicated maneuversin this swallow-ing management were frequency or multiple swallowing. Theywereindicatedtobeperformedduringthedaily feed-ing,aimingtoclearstasisandreducethechanceoflarynx penetrationoraspiration.
In rehabilitation maneuvers, the exercises of tongue strengtheningandtonguecontrolwerefrequentlyindicated becausetonguemovementsofPDpatients,especiallythose responsible for propulsion and chewing, are considered hypokineticin theoral phase.In thesepatients the swal-lowingoralphaseisusuallylongerandevenslowerthanthe pharyngealphase.29
Forhalfofthepatients,vocalexerciseswereindicated, asthereareevidencesthatthistypeofexercisesworksto improve the cough function and tongue’s mobility during swallowing,27 whichleadstoabetterswallowing
Futurestudiesabouttheefficacyofinterventionmethods in swallowingof PD patients arenecessary. The improve-mentandmaintenance,notexpectedinneurodegenerative diseases,foundinthepresentstudy,suggestthatswallowing managementmightpositivelyaffectswallowing functional-ityofPDpatients,butitcannotbeaffirmedduetothedesign ofthisstudy.
Inconclusion,the swallowingfunctionality was charac-terizedbymaintenanceorimprovement,especiallyinthe firsttenmonthsoffollow-up,comprisingcompensatoryand rehabilitation maneuvers, reoriented each three months. Therewasnoassociatedfactorwithchangesinswallowing functionalityinthesecases.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.CraryMA.Adultneurologicdisorders.In:GroherME,editor. Dys-phagia---clinicalmanagementinadultsandchildrenSt.Louis: Elsevier/Mosby;2009.p.72---98.
2.SchragA,Ben-ShlomoY,QuinnNP.Cross-sectionalprevalence survey of idiopathic Parkinson’s disease and parkinsonismin London.BMJ.2000;321:21---2.
3.RijkMC,BretelerMM,GravelandGA,OttA,GrobbeeDE,Van DerMeche’FG,etal.PrevalenceofParkinson’sdiseaseinthe elderly:theRotterdamstudy.JNeurol.1995;45:2143---6. 4.Jankovic J. Pathophysiology and assessment of parkinsonian
symptomsandsigns.In:PahwaR,LyonsK,KollerWC,editors. HandbookofParkinson’sdisease.NewYork:TaylorandFrancis GroupLLC;2007.p.79---104.
5.Potulska A, Friedman A, Krolicki L, Spychala A. Swallowing disorders in Parkinson’s disease. Parkinsonism Relat Disord. 2003;9:349---53.
6.FelixVN,CorrêaSMA,SoaresRJ.Atherapeuticmaneuverfor oropharyngeal dysphagiain patients with Parkinson disease. Clinics.2008;63:661---6.
7.MarikPE,KaplanD.Aspirationpneumoniaanddysphagiainthe elderly.Chest.2003;124:328---36.
8.Manor Y, Giladi N, Cohen A, Fliss DM, Cohen JT. Validation ofa swallowing disturbancequestionnairefor detecting dys-phagia in patients with Parkinson’s disease. Mov Disord. 2007;22:1917---21.
9.Müller J, Wenning GK, Verny M, McKee A, Chaudhuri KR, Jellinger K, et al. Progression of dysarthria and dysphagia inpostmortem-confirmedParkinsoniandisorders.ArchNeurol. 2001;58:259---64.
10.D’AmelioM,RagoneseP,MorganteL,ReggioA,CallariG,Salemi G,etal.Long-termsurvivalofParkinson’sdisease:a population-basedstudy.JNeurol.2006;253:33---7.
11.SchüpbachMW,WelterML,BonnetAM,ElbazA,GrossardtBR, MesnageV,etal.MortalityinpatientswithParkinson’sdisease treatedbystimulationofthesubthalamicnucleus.MovDisord. 2007;22:257---61.
12.CraryMA.Treatmentforadults.In:CraryMA,GroherME, edit-ors.Dysphagia:clinicalmanagementinadultsandchildren.St. Louis:Elsevier/Mosby;2009.p.275---307.
13.Crary MA, Mann GDC, Groher ME. Initial psychometric assessment of a functional oral intake scale for dyspha-gia in stroke patients. Arch Phys Med Rehabil. 2005;86: 1516---20.
14.MillerN,NobleE,JonesD,BurnD.Hardtoswallow:dysphagia inParkinson’sdisease.AgeAgeing.2006;35:614---8.
15.Logemann JA, Blonsky ER, Boshes B. Editorial: dysphagia in parkinsonism.JAMA.1975;231:69---70.
16.StroudleyJ,WalshM.Radiologicalassessmentofdysphagiain Parkinson’sdisease.BrJRadiol.1991;64:890---3.
17.Bird MR, Woodward MC, Gibson EM, Phyland DJ, Fonda D. Asymptomatic swallowing disorders in elderly patients with Parkinson’sdisease:adescriptionoffindingsonclinical exam-inationandvideofluoroscopyinsixteenpatients.AgeAgeing. 1994;23:251---4.
18.MillerN, Allcock L,Hildreth AJ,Jones D,NobleE,Burn DJ. Swallowing problems in Parkinson’s disease: frequency and clinical correlates. J Neurol Neurosurg Psychiatry. 2009;80: 1047---9.
19.Baldeschi M,DiCarlo A, RoccaWA,for ILSA WorkingGroup. Italian longitudinal study on aging Parkinson’s disease and parkinsonisminalongitudinalstudy:two-foldhigherincidence inmen.JNeurol.2000;55:1358---63.
20.LogmannJA,GenslerG,RobbinsJ,LindbladAS,HindJA,Kosek S,etal.Arandomizedstudyofthreeinterventionsforaspiration ofthinliquidsinpatientswithdementiaorParkinson’sdisease. JSpeechLangHearRes.2008;51:173---83.
21.LorefältB,GránerusAK, UnossonM.Avoidance ofsolidfood inweightlosingolderpatientswithParkinson’sdisease.JClin Nurs.2006;15:1404---12.
22.Lo RY,Tanner CM,Albers KB,LeimpeterAD, FrossRD, Bern-steinAL,etal.ClinicalfeaturesinearlyParkinson’sdiseaseand survival.ArchNeurol.2009;66:1353---8.
23.AuyeungM,TsoiTH,MokV,CheungCM,LeeCN,Li R,et al. Tenyearssurvivalandoutcomesinaprospectivecohortofnew onsetChineseParkinson’sdiseasepatients.JNeurolNeurosurg Psychiatry.2012;83:607---11.
24.RobbinsJ,GenslerG,HindJ,LogemannJA,LindbladAS,Brand D,etal.Comparisonoftwointerventionsforliquidaspiration onpneumoniaincidence arandomizedtrial.Ann InternMed. 2008;148:509---18.
25.ElSharkawiA,RamigL,LogemannJA,PauloskiBR,Rademaker AW, Smith CH, et al. Swallowing and voice effects of Lee SilvermanVoiceTreatment(LSVT(R)):a pilotstudy.JNeurol NeurosurgPsychiatry.2002;72:31---6.
26.Hockstein NG, Samadi DS, Gendron K, Handler SD. Sialor-rhea: amanagement challenge.Am Fam Physician.2004;69: 2628---34.
27.RussellJA,CiucciMR,ConnorNP,SchallertNT.Targeted exer-cisestherapyforvoiceandswallowinpersonswithParkinson’s disease.BrainRes.2010;1341:3---11.
28.LogemannJA.Evaluation andtreatmentofswallowing disor-ders.2nded.Austin,TX:Pro-Ed;1998.