w w w . r b o . o r g . b r
Update
Article
Current
concepts
on
the
sagittal
balance
and
classification
of
spondylolysis
and
spondylolisthesis
夽
,
夽夽
Marcos
Antonio
Tebet
DisciplineofOrthopaedicsandTraumatology,FaculdadedeMedicinadeJundiaí,Jundiaí,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received4April2013 Accepted9April2013
Keywords:
Spondylolisthesis
Spondylolysis/classification Posturalbalance
Radiographypanoramic
a
b
s
t
r
a
c
t
Treatment ofspondylolysis andspondylolisthesis remains a challenge fororthopaedic surgeons,neurosurgeonsandpaediatrics.Inspondylolisthesis,ithasbeenclearly demon-stratedoverthepastdecadethatspino-pelvicmorphologyisabnormalandthatitcanbe associatedtoanabnormalsacro-pelvicorientationaswellastoadisturbedglobalsagittal balanceofspine.ThisarticlepresentstheSDSG(SpinalDeformityStudyGroup)classification oflumbosacralspondylolisthesis.Thepropertreatmentofspondylolisthesisisdependent onrecognizingthetypeofslip,sacro-pelvicbalanceandoverallsagittalbalanceandits nat-uralhistory.Althoughanumberofclinicalradiographicfeatureshavebeenidentifiedas riskfactors,theirroleasprimarycausativefactorsorsecondaryadaptativechangesisnot clear.Theconservativetreatmentofadultisthmicspondylolisthesisresultsingood out-comeinthemajorityofcases.Ofthosepatientswhofailconservativetreatment,success withsurgeryisquitegood,withsignificantimprovementinneurologicfunctioninthose patientswithdeficits,aswellasimprovementinpatientswithbackpain.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Conceitos
atuais
sobre
equilíbrio
sagital
e
classificac¸ão
da
espondilólise
e
espondilolistese
Palavras-chave:
Espondilolistese
Espondilólise/classificac¸ão Equilíbriopostural Radiografiapanorâmica
r
e
s
u
m
o
Otratamentodaespondilóliseedaespondilolistesepermaneceumdesafiopara ortopedis-tas,neurocirurgiõesepediatras.Nasespondilolisteses,temsidoclaramentedemonstrado na última décadaque a morfologia sacro-pélvica estáanormal e queisso pode estar associadoaumaanormalorientac¸ãosacro-pélvicaetambémalteraroequilíbriosagital globaldacoluna.Esteartigoapresentaaclassificac¸ãoSDSG(SpinalDeformityStudyGroup) daespondilolisteselombossacral.Aspropostasdetratamentoparaaespondiolistesesão dependentesdoreconhecimentodotipodedeslizamento,equilíbriosacro-pélvicoebalanc¸o sagital edesuahistória natural.Apesarde haverdiversosachados clínicose radiográ-ficosquesãoidentificadoscomofatoresderiscodeprogressão,osfatoresprimáriosou secundáriosquecausamaprogressãopermanecemobscuros.Otratamentoconservador paraespondilolisteseístmicadoadultoapresentabonsresultadosnamaioriadoscasos.
夽
Pleasecitethisarticleas:TebetMA.Conceitosatuaissobreequilíbriosagitaleclassificac¸ãodaespondilóliseeespondilolistese.Rev BrasOrtop.2014;49:3–12.
夽夽
StudyconductedattheDisciplineofOrthopedicsandTraumatology,FaculdadedeMedicinadeJundiaí,Jundiaí,SP,Brazil. E-mail:matebet@uol.com.br
tambémébom,commelhoriasignificativadafunc¸ãoneurológicatantoquantomelhoria dadorlombar.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Thetermspondylolisthesisisdefinedasatranslationofone vertebraoveranotherintheanteriororposteriordirection.In theadult,thisoccursinthelumbarcolumnasaresultofa defectinbonearchitecture,traumaordegenerativeprocess.1
The term spondylolisthesis is derived from the Greek
spondylos, meaning “vertebra”, and olisthesis, meaning “to
slide”.Thefirstobservationofspondylolisthesisoccurredin 1772bytheBelgianobstetricianHerbiniaux2 duringa
deliv-erycomplicatedbyanarrowinginthechannelbecauseofa slippageofL5vertebraoverthesacrum.
Thistermwasfirstusedin1854byKilianinLonsteinetal.3
Spondylolisthesisisdefinedasatranslationofonevertebral bodyovertheadjacentcaudalvertebrainananterioror,in moreseriouscases,anteriorandcaudaldirection. Spondyloly-sisisadefectintheparsinterarticularis,butwithoutoccurrence ofslippage.
Spondylolisthesishasbeenaconditiondifficultto under-standfor orthopaedists, neurosurgeons and paediatricians, becauseofthegreatvarietyofexistinganatomicalandclinical forms.Therearefewpathologicalconditionsofthecolumnin whichthereissomuchtherapeuticcontroversy.
Consideringthatthespondylolisthesisis“aslippageofa portion ofthe column over other adjacent part”, wemust rememberthatthe columnthatslidalsomovedthe entire trunk,andthismaybringclinicalconsequence.
Theaetiology ofthis diseaseismultifactorial andisnot yetperfectlyclear.Thenaturalhistoryisnotwellestablished fromthe pointofview ofthe knowledgeofitsreal causes, pathogenesisanddevelopment.4
Spondylolisthesisandspondylolysisareusuallywell tol-erated by patients, but in some cases the severity of the symptoms and a condition unresponsive to conventional medical treatment have caused the indication for surgical treatment.5
Epidemiology
and
aetiology
Theincidenceofspondylolysisinthegeneralpopulationis about6%,withamale:femaleratioof2:1.6
The incidence of spondylolisthesis in children under 6 yearsis2.6%,whileinadultsitis5.4%.6
Thedegenerativespondylolisthesisrarelyaffects individ-ualsbelowtheageof40years,andisfourtofivetimesmore commoninwomenthaninmen.InastudybyLoveetal.,7
sub-jectswhohadfacetorientation>45◦inthesagittalplanewere 25timesmorelikelytodevelopdegenerative spondylolisthe-sis.
Thereseemstoexistageneticandfamilialassociationwith spondylolysisandspondylolisthesis,because26%ofpatients
withisthmicspondylolisthesishadfirst-degreerelativeswith thesamedisease.8
Theincidencevariesaccordingtoethnicity:itismore com-moninCaucasianthaninblackpeople.InatribeofEskimos inAlaskatheincidencereachesabout50%.9
Theexactaetiologyofmostcasesremainsobscure. Thedysplasticlesionsoftheparsinterarticularis,fractureor oftheelongamentandofspinabifidaconcealabroaddistal spinalcanal.Dysplasiainbothfacets(lowerlumbarandupper sacral)isacommonfindinginspondylolisthesis,especiallyin thosewithhighgrade.
Thesuperiorsacralfacettogetherwiththelowerlumbar facetformsabonehookwhichpreventstranslation.Dysplasia canoccurineitherorbothfacets.Thus,thehookeffectislost.6
Thepresenceofspondylolysis/spondylolisthesisisrarein non-ambulatorypatients,whichattachesimportancetothe orthostatismroleandofrepeatedmicrotraumasinthe devel-opmentofspondylolysis.
Biomechanicalstudieshavedemonstratedanincreasein stress inthe parsinterarticularis with the columnin exten-sionandincreaseofshearforcesthroughthesamearea,with persistenceoflordosis.7
Activitiesthatincreaselordosisandmaintainthecolumn inextension,suchasolympicgymnastics,diving, weightlift-ing, volleyball, football and pathologies such as kyphosis, increasetheincidenceoffractureoftheparsandof spondy-lolysisandspondylolisthesis.10
Sagittalbalanceinspondylolisthesis
Thespondylolisthesesaredivided intohigh(slippage>50%) andlow(slippage<50%)grade.
Theclassificationsusedforspondylolisthesisarenot use-ful for surgicaltreatment indicationsand, asnoted in the lastdecade,thesagittalbalanceisthekeyfactorforsurgical treatment.11
One explanation for the aetiology of developmental spondylolisthesis,whichtakesintoaccountthesagittal bal-ance, is that, in the presence of spondylolysis and bone dysplasia,themechanicalstressappliedtothelumbosacral junctionisincreasedbecauseofthealteredsacro-pelvic mor-phology,whichleadstoanabnormalsecondaryspino-pelvic equilibrium. Becauseofboneremodellingbygrowth plates (Heuter-Volkmanlaw),asecondarydeformityofthebodyof L5,sacrumandpelvisalsoaltersthebiomechanicalforcesin the lumbosacralcolumn, whichcontributestothe progres-sionofspondylolisthesis,inaprocesssimilartowhatoccurs inBlountdisease.
A
PI b
b
p
q o
o a
a
c
c
PI
B
Fig.1–(A)PelvicIncidence(PI)isdefinedastheangle formedbytheintersectionofalinedrawnfromthecentre ofthefemoralheadtowardsthemidpointofthesacral endplate(o–a)andalineperpendiculartothecentreofthe sacralendplate(a).Thesacralendplateisdefinedbya segment(b–c)formedbetweentheposteriorhornofthe sacrumandtheanteriortopoftheS1sacralpromontory.(B) Whenthefemoralheadsarenotperfectlyoverlapped,the centreofeachoneofthemismarkedandalinedrawn betweentwopoints(q–p)willconnectthecentreofthetwo heads.Theline(o–a)willbedrawnfromthecentreofthe line(q–p),i.e.,point(o),tothecentreofthesacralendplate.
perpendiculartotheupperplateauofS1.PIincreasesslightly andconsistentlyinadulthood.12ThevalueofPIishigherin
spondylolisthesis,increasinglinearly,accordingtothe sever-ityofslippage12(Fig.1).
Thepelvictilt(PT)andthesacralslope(SS)measurethe sacro-pelvicorientationinthesagittalplane,beingevidenced inthe lumbosacral lateral view.SS isdefined as theangle betweentheupperhorizontalplateauandS1,whilePTisthe anglebetweenthelineconnectingthemidpointoftheupper plateauofS1andthecentreoffemoralrotationwithavertical line(Figs.2A–Band3B).
PThasavalue(+)whentheline(o–a)islocatedposterior toVRLvalueand(–)whentheline(o–a)isanteriortoVRL.
We must understand that PI is a measure of a static structure.PTandSS,ontheotherhand,aredependent pos-itions,becausetheydependonthe angularpositionofthe sacrum/pelvisinrelationtothefemoralhead,whichchanges
Vertical reference line
(VRL) b
b
a
a
c
c
PT
PT
PI
o
o
A
B
Fig.2–(A)Pelvictilt(PT)isdefinedbytheintersectionofa verticalreferenceline,whichoriginatesfromthefemoral headcentre(o)andthemidpointofthesacralendplate(a). (B)PTcanbeinfluencedbyPI,sincetheysharetheline (o–a)andtheterminalsacralplateisacommonreference lineforboth.
in the orthostatic and sitting positions. PT/SS ratio isalso affectedbythebendingandlumbosacral-pelvicextension.
PIisthesumofSSand PT(Fig. 3B);then,IPisastrong determinant ofthe spatial orientationof the pelvisin the osthostatism,i.e.thehigherthePI,thegreaterwillbethePT orSS,orboth.ThenormalvaluesofPI,SSandPTinchildren are49.1◦,41.4◦ and7.7◦,respectively.13Inadultsthenormal valuesare51.8◦,39.7◦and12.1◦.12
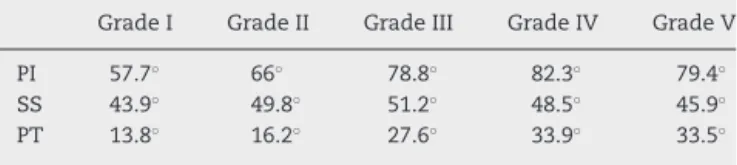
Thevaluesinspondylolisthesis12areshowninTable1.
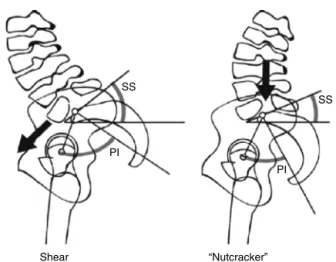
InthestudybyRoussoulyetal.,14patientswithhighPIand
SSresultinincreasedshearforceincidentonthelumbosacral junction,whichcreatesmorestressontheparsinterarticularis
ofL5.ButinthosepatientswithlowPIandaminorSS,there maybeanimpactamongtheposteriorelementsbetweenL5 andthoseofL4andS1duringextension,therebycausingan effectof“nutcracker”inparsinterarticularisofthe5thlumbar vertebra.
Table1–Valuesofspondylolisthesisinaccordancewith thedegreeofslippage.
GradeI GradeII GradeIII GradeIV GradeV
PI 57.7◦ 66◦ 78.8◦ 82.3◦ 79.4◦
SS 43.9◦ 49.8◦ 51.2◦ 48.5◦ 45.9◦
SS
SS
b
b a
c
o
c
Horizontal reference line (HRL)
VRL
HRL PT
PI
PI = SS + PT
A
B
Fig.3–(A)Sacraltilt(SS)isdefinedastheintersectionof thehorizontalreferenceline(HRL)andthesacralendplate (b–c).(B)Thesacralslope(SS)isrelatedtoPIandPT becauseitsharesareferenceline(b–c)incommonalong thesacralendplate.
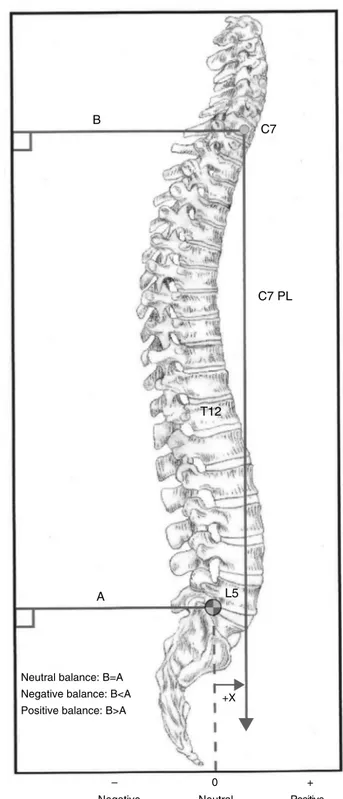
Thesacralprojection(distancefromthesacrumtoaplumb linefromC7)isanotherbiomechanicaldeterminant.Typically, theplumbline(PL)passesthroughS1(Fig.4).
Becauseofthesemorphologicalchanges,thesagittal bal-ancecanonlybeachievedbyhyperlordosis.Greatervertical tiltofthesacrumwillberequiredtomaintainsagittalbalance, whenthisisnotpossibleonlywithhyperlordosis.This verti-calizationofthesacrumisaccompaniedbycontractureofthe hamstrings,whichcircumventcaudallytheischialmuscles, andtheanteriorpelviscephalad.14
With these data, there are three possible biomechani-caloutcomes: first,the forces generated byan increase in lumbarlordosishave,asconsequence,thedevelopmentand progressionofspondylolisthesis;andsecond,the biomechan-icalchangesgeneratechanges inpostureandgait thatare compensatorymechanismstomaintainsagittalbalance;and finallythebiomechanicalchangesmouldtheadjacent verte-brae.
Evidenceofthepresenceofabnormalsagittalspino-pelvic
alignmentinspondylolisthesis
Althoughthe correlationbetween pelvicincidence(PI) and spondylolisthesisisevident,thereare nopublisheddatain theliteraturethatmayconfirmthecause/effectrelationship betweenthesetwo.However,asthepelvicincidence(PI) is
C7
C7 PL
T12
L5 A
Neutral balance: B=A
+X
–
0 +
Negative Neutral Positive Negative balance: B<A
Positive balance: B>A B
Fig.4–SagittalBalance:PL=plumbline.TheAlineis drawnfromthesuperior-posteriorborderofS1 perpendiculartotheverticaledgeoftheradiograph.Its lengthismeasuredinmillimetres.TheBlineisdrawnfrom thecentreofC7perpendiculartotheverticaledgeofthe radiograph.Itslengthismeasuredinmillimetres.
SS
SS
PI
PI
Shear “Nutcracker”
Fig.5–Thepostureinshearandin“nutcracker”,published byRoussoulyetal.14forlow-gradespondylolistheses.
However,notallpatientswithspondylolisthesisatL5-S1 presentwithPIabovethenormal.Roussoulyetal.14observed,
inastudywith82subjectswithlow-gradespondylolisthesis, thepresenceoftwodistinctsubgroupswithrespecttoform andsacro-pelvicbalance,whichcanbeaffectedbydifferent pathogenicmechanisms.Accordingtotheseauthors,patients withhighPIandsacralslope(SS)showanincreaseintheshear forcesincidentatthelumbosacraljunction,whichcauses fur-thertensionontheparsarticularisofL5:thesheartype(Fig.5). Ontheother hand,thosepatientswithlowPIand SSmay presentclampingoftheposteriorelementsofL5betweenL4 andS1duringextension,whicheventuallycausesaneffectin “nutcracker”ontheparsarticularisofL5.
Forcasesofhigh-gradespondylolisthesis,Hreskoetal.16
identifiedtwosubgroupsofsacro-pelvicalignment:with bal-ancedorunbalancedpelvicposture(Fig.6).The“balanced” groupincludespatientswhointheorthostaticpositionshow highSSandlowpelvictilt(PT).Patientsinthegroup “unbal-anced”includethose who inthe orthostatic position have retrovertedpelvisandverticalizedsacrum,whichcorresponds toa low SS and high PT. Ithas been shown that patients withhighdegreeofvertebralslippagehaveameanPI>60◦.
Balanced pelvis Retroversed pelvis
Fig.6–Balancedandretroversedpelvicposturepublished byHreskoetal.16forhigh-gradespondylolistheses.
Table2–ClassificationofWiltse,NewmanandMacnab. TypeI–dysplasticcongenitalabnormalitiesoftheposteriorelements
TypeII–isthmic:defectintheparsinterarticularis.Threetypes: Lithic–fatiguefractureofthepars
Elongationofthepars Acutefractureofthepars
TypeIII–Degenerative:degenerationofthediscandfacets,whichcreates instabilityandmobilityonsegment
TypeIV–Traumatic:acutefractureofthepedicles,facetsorblades (exceptpars)
TypeV–Pathologic:becauseofneoplasticormetabolicprocesses
Thiscontrastswiththosewithlow-grade spondylolisthesis, inwhomPIvaluesarelow,normalorhigh.
Furthermore,itwasobservedthatthesagittalbalance,i.e. themeasurementoftheplumblinefromC7,wassignificantly increased(>3cm)inthose withretroverted posture (unbal-anced);thissuggeststhatthepositivesagittalimbalancemay beassociatedwiththistypeofspino-pelvicalignment. Mac-Thiongetal.17showedinacomparativestudybetweenagroup
of131patientswithspondylolisthesisandacontrolgroupof 120 patients, thatthe normalsagittal balance ofthetrunk was maintainedinpatientswithlow-grade spondylolisthe-sis,whilethesagittalbalancewaschangedinpatientswith high-gradespondylolisthesis.Again,thespino-pelvicbalance wasalteredinthegroupofhigh-gradespondylolisthesis asso-ciatedwithsacral-pelvicimbalance.
Classification
Thespondylolisthesishasbeen described byWiltse etal.18
classification(Table2),basedonetiologicalandtopographical criteria, withfivetypes.Itisdifficulttopredictits progres-sionandresponsetotreatment.Therecognitionthatsurgical decompression mayleadtoinstabilityofthecolumnmade necessaryasixthtype:iatrogenicspondylolisthesis.
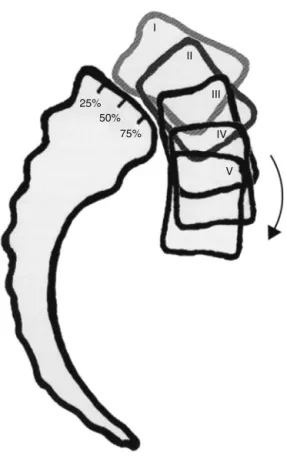
Another systemusedisthe oneproposed byMeyerding etal.19in1932(Fig.7),inwhichthedegreeofslippageis
cal-culatedbytheratiobetweentheanterosuperiordiameterof thesacrumandthedistanceofpreviousslippageofvertebra L5.Thus,itcanbeconsidered:gradeI–25%orless,gradeII– between25%and50%,gradeIII–between50%and75%,and gradeIV–greaterthan75%.ThedegreeV,asspondyloptosis, doesnotbelongtotheoriginaldescription.
ThescaleofMeyerdingonlydescribesthedegreeof tan-gential slippage, though in high-grade dysplasias there is kyphosis,inadditiontothetangentialtranslation.Themore usedgradingsystemforhigh-gradeslippagesisthatproposed byNewmanand modifiedbyDeWaldetal.,20inwhich the
domeandtheanteriorsurfaceofthesacrumaredividedinto tenparts(Fig.8).Themeasureistakenbasedontheposition oftheposterior-inferiorcornerofthebodyofthefifth verte-brainrelationtothedomeofthesacrum(firstmeasure)and thesecondmeasureisgivenbythepositionofthe anterior-inferiorcornerofthebodyofthevertebraL5inrelationtothe anteriorsurfaceofS1.
Marchettietal.andBartolozzietal.21developeda
25% 50%
75% I
II
III
IV
V
Fig.7–Meyerdingclassification.
versusdevelopmentaltypeandalsodividesthe developmen-talspondylolisthesisindysplasticoflowandhighgrade.
Noneoftheseclassificationsystemsweredesignedwith thegoalofassistinginsurgicalplanningof spondylolisthe-ses.Thus, theguidelines and outcome studiesand clinical follow-uparemostlybasedonthedegreeofslippage.21,22
Fur-thermore,theseclassifications20,21 donottakeintoaccount
thesacro-pelvicsagittalbalance,althoughmorerecent stud-iessuggesttheimportanceofthisbalanceintheassessment, progressionandtreatmentofspondylolisthesis.23,24Thismay
betheexplanationforthelargeamountofpublishedstudies onsurgicaltechniques.
A
B
C
Fig.8– Newmangraduationsystem,modifiedbyDeWald.20
Table3–SDSGclassificationbasedinspino-pelvic posture.
Spondylolisthesis Lowgrade<50%
Type1:PI<45◦(“nutcracker”) Type2:PI=45–60◦
Type3:PI>60◦
Highgrade>50% Type4:Balancedpelvis Retroversedpelvis Type5:Balancedcolumn Type6:Unbalancedcolumn
Recently,Mac-Thiongetal.andLabelleetal.25proposeda
newclassificationsystemforspondylolisthesis,withthegoal ofassistingintheevaluationandtreatmentoflumbosacral spondylolisthesis.Thisclassificationclarifiestheconceptsof dysplasiaoflowandhighgradepresentedbyMarchettietal. andBartolozzietal.21andincorporatesthelatestknowledge
ofthemorphologyandthesacral-pelvicsagittalbalance.Eight typesofspondylolisthesisaredescribedasfollows:(1)degree ofslippage(lowandhighgrade),(2)degreeofdysplasia(low andhighgrade)and(3)sagittalsacro-pelvicbalance.The clas-sificationisorganizedintogroupsandsubgroupsinascending degreesofseriousness,inordertodevelopaprogressive algo-rithmofsurgicalcomplexityproportionaltotheincreasein theseverityofspondylolisthesis.
Classificationproposedbythestudygroupofspinal
deformities(SpinalDeformityStudyGroup[SDSG])
The SDSG submitted a classification for spondylolisthesis betweenL5andS1thathasbeensimplifiedandrefined.This classificationisbasedonthreecharacteristicsthatcanbe eval-uatedinlateralview(sagittal)radiographofthecolumnand pelvis:(1)degreeofslippage(loworhigh),(2)pelvicincidence (low,normalorhigh)and(3)spino-pelvicbalance(balancedor unbalanced).Thus,sixsubtypescanbeidentified(Table3).23–25
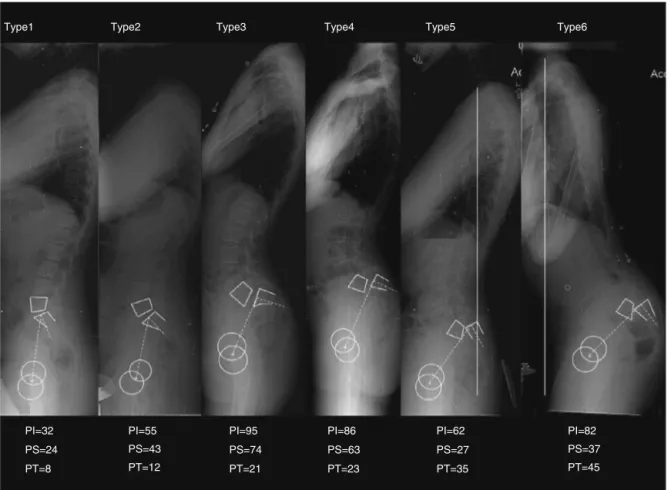
Toapplytheclassification,inthefirstplacethedegreeof slip-pageismeasuredonalateralradiographofthecolumn.Soit canbedeterminedwhethertheslippageislow-grade(0,1and 2:<50%slippage)orhighgrade(3,4orspondyloptosis:>50% slippage).Then,thesagittalbalanceismeasuredtodetermine thesacro-pelvicandspino-pelvicalignment.Themeasuresof PI,SS,PTandoftheplumblineofC7areused.Forlow-grade spondylolistheses,threetypesofsacro-pelvicbalancecanbe found:type1,“nutcracker”,asubgroupwithlowPI(<45◦);Type 2,asubgroupwithnormalPI(between45◦and60◦);andtype 3,asheartype,asubgroupwithhighPI(>60◦).Forthosecases withhigh-gradespondylolisthesis,threetypesarealsofound. Eachcasemustfirstbeclassifiedasifpresentingabalanced orunbalancedsacro-pelvic,usingvaluesofPIandSS.16The
spino-pelvicbalanceisdeterminedwiththeuseoftheplumb lineofC7.Ifthislinefallsonorbehindthefemoralhead,the columnwillbebalanced;ifitfallsinfrontofthefemoralhead, thecolumnwillbeunbalanced.
Type1
PI=32
PI=55
PI=95
PI=86 PI=62 PI=82 PS=24 PS=43 PS=74
PS=63
PS=27 PS=37 PT=8 PT=12 PT=21
PT=23 PT=35 PT=45
Type2 Type3 Type4 Type5 Type6
Fig.9–ClassificationoftheSpinalDeformityStudyGroup.PI=pelvicincidence,SS=sacralslope,PT=pelvictilt.
column)andtype6(retrovertedpelviswithunbalanced col-umn).Fig.9showssixclinicalexamplesofthesepositions.
Progression
factors
AccordingtoBoxaletal.,26thebestparametertopredict
pro-gressionisagreatslippageangle(>55◦);thisangleisformed bytheintersectionofalinedrawnparalleltotheinferiorface ofL5andaperpendiculartotheposteriorfaceofthebodyof S1.Theauthorsalsoreportthataprogressionmayoccur,even afterasolidposteriorarthrodesis.
PatientswithlowPIandlowSS(“nutcracker”mechanism) havealowriskofprogression.Dysplasiaandslippageofhigh grade(>50%)werealsoreportedasafactorforprogressionof spondylolisthesis.27
Otherfactorsinfavourofprogressiontoisthmic spondy-lolistheses are female gender, slippage >50% and children beforethegrowthspurt.24
Itwasobservedthatpatientswithspondylolisthesiscaused bydysplasiahaveahigherchanceofprogressionversusthose withspondyloliticspondylolisthesis.28
Clinical
manifestations
Thesymptomscanbedividedintosymptomsinchildrenand adults.
Inchildren,thespondylolisthesisisusuallyasymptomatic. Exaggeratedlumbarlordosismaybethefirstwarningsignand ashorteningofhamstringsoccurs.Withthe verticalization ofthesacrum,thebuttocksbecomeheart-shaped,becauseof thebonyprominence.Withtheprogression,thepatient devel-opsatypicalposture,becauseofthehamstringshortening, verticalizationofthesacrumandincreasedlordosis,known asPhalen-Dicksonsignal(bendingofthekneesandhips).In symptomaticcases,themechanicallowbackpainisthemost commoncomplaint.3Theseverityofpainmayormaynotbe
relatedtothedegreeofslippage.Radiculopathyisless com-mon,butisobservedwiththeprogressivetranslation,when instabilityispresent.RadiculopathyofL5occursmoreoften thanradiculopathyofS1.S1rootcompressionoccursinhigh degreesofslippagebecauseoftherootstretchingstressabove theedgeofthesacrum.Thepainincreaseswiththeextension ofthecolumnandimproveswithrest.29
Inadultsthelumbarpainwithor withoutirradiationto the lower limbsiscommon; this istypically a mechanical painthatworsenswithextension.Thepainmustbe differ-entiatedfrom discogenic pain, whichworsenswith flexion andinthesittingposition.Neurogenicclaudicationisalsoa commonsymptom, definedasapaininthelower extremi-ties, numbnessorweakness associatedwithambulationor withtheseatedposition.30Painisthepredominantsymptom,
presentin94%ofpatients,followedbyparesthesia(63%)and weakness(43%).31Neurogenicclaudicationmustbe
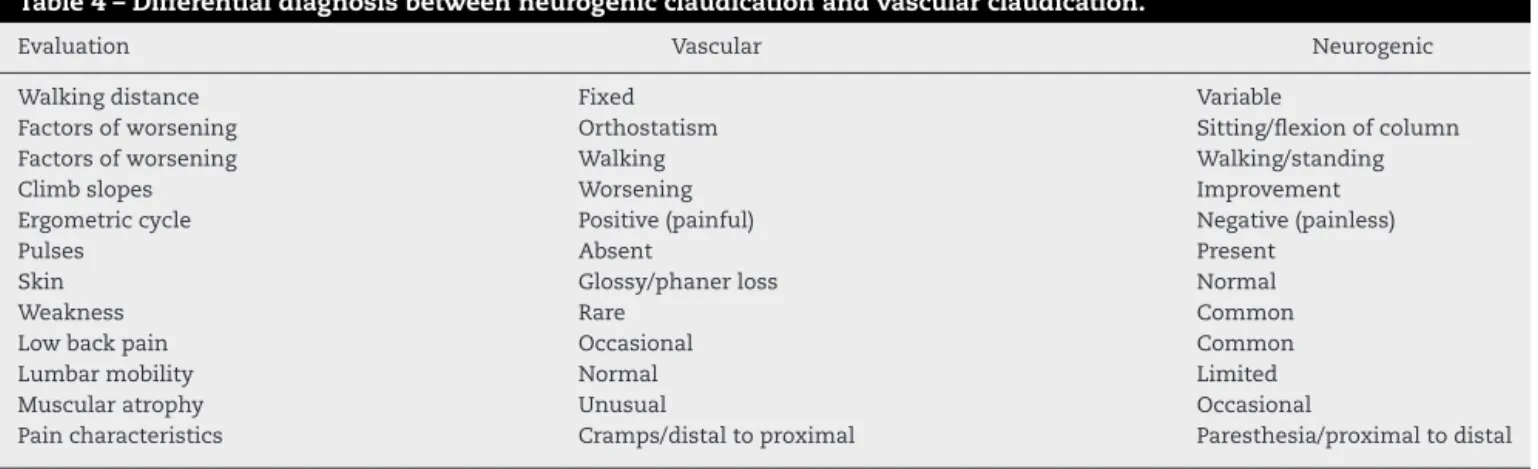
Table4–Differentialdiagnosisbetweenneurogenicclaudicationandvascularclaudication.
Evaluation Vascular Neurogenic
Walkingdistance Fixed Variable
Factorsofworsening Orthostatism Sitting/flexionofcolumn
Factorsofworsening Walking Walking/standing
Climbslopes Worsening Improvement
Ergometriccycle Positive(painful) Negative(painless)
Pulses Absent Present
Skin Glossy/phanerloss Normal
Weakness Rare Common
Lowbackpain Occasional Common
Lumbarmobility Normal Limited
Muscularatrophy Unusual Occasional
Paincharacteristics Cramps/distaltoproximal Paresthesia/proximaltodistal
Diagnosis
Thediagnosisisestablishedonradiographsofthelumbar col-umninfrontalandprofileincidenceswiththepatientinthe orthostaticposition.Otherviewsusedarelocatedprofileand rightandleftobliqueincidences.
Inradiographsinobliqueincidence,the“Scottishdog”can beseen,wherethe“collar”representslysisinthepars.26
Computed tomographyhas littlevalue inthe diagnosis; thistechniquecan demonstratesclerosisand thedefect in thepars.
MRIis theexam ofchoicetoview the disc atthe level ofthe deformity. This imagingtechnique is used in cases ofradiculopathy andtovisualizeboneoedemaanddefects
inthe pars articularis. Moreadvanced image examinations,
such as computed tomography by single photon emission (SPECT),32aremoresensitiveandprovidemoredetails.
Ander-sonetal.33reportedthat20%ofpatientswithnegativeresults
onastandardbonescanwithsuspectedacutespondylolysis showedalesionoftheparswhenassessedwithSPECT.
Treatment
of
spondylolisthesis
Thespondylolisthesis can be oflow grade (slippage <50%) or of high grade (slippage >50%) and both types can be treatedconservatively.However,thehigh-degree spondylolis-thesesrespondmorepoorlytoconservativetreatmentwhen comparedwiththoseconditionsoflowdegree.31The
conser-vativetreatmentisbestsuitedfordisplacementssmallerthan 30–50%inthegrowingchildandforsomedisplacementslarger than50%inyoungadults.Forsymptomaticpatients, excel-lentclinicalresponsehasbeen obtainedwithrestrictionof physicalactivity andtheuse ofortheses(TLSO) inorderto avoidrepetitivemovementsofhyperextensionofthelumbar column.13
Forpatients withchroniclowback pain,Panjabiet al.34
demonstrated that the strengthening of specific muscle groups improves the patient’s response to pain; so, these authorsstartedtorecommendthestrengtheningofthe trans-verse abdominal, internal oblique and multifidus muscles. Besidesthestrengtheningofthesespecificmusclegroups,the strengtheningofthehipflexorsandthestretchingof ham-stringsalsoimprovethepatientresponsetolowbackpain.13
AccordingtoDeWald,20thegoalinthesurgicaltreatmentof
spondylolisthesisisthefusionofthesmallestpossible num-ber ofmobile segments ofthe column,which restores the sagittalverticalaxis,withthesacrumandlumbarcolumnin asnormalaspossibleaposition,andthefusionofthe non-competent disc spaces.Thistypeoftreatmentisindicated in asymptomatic children withgreater than 50% slippage, forasymptomaticpatientswithskeletalmaturityandgreater than 75% slippage, for symptomatic patients who do not respondtoconservativetreatment,progressionofdeformity andneurologicaldeficit.30
Insymptomaticadultpatientswithlow-grade degenera-tivespondylolisthesis,posterolateralarthrodesis(PLA)insitu hasbetterclinical outcomeswhencomparedtosupervised exerciseprogrammes.35,36 However,PLAhasbeenunableto
maintainintraoperativecorrectionoftheslippageangle,due totheprogressivedegenerationoftheanteriordiscspace.35
Suketal.37andLaRosaetal.38conductedacomparativestudy
betweenPLAand360◦arthrodesis(PLA+PLIF)andfoundthat many postoperativeradiologicalparameters, suchasfusion rate,reductionoftheslippageangleandmaintenanceofthe correction ofthedeformity, were superiorin patientswith arthrodesis360◦.However,clinicallyinnoneofthesestudies PLAorPLIFwasstatisticallysuperior.39
A decompression isindicated incasesofradiculopathy. UsuallytheL5rootisinvolvedattheforaminalleveland com-pressedbytheproximalportionoftheparsastheslippageis enhancedbyfibrocartilaginoustissueinthedefectivepars.In casesofradiculopathyorotherneurologicaldeficits,suchas caudaequina,decompressionisindicated.TheGillprocedure isthebasisfordecompressionbyremovingthelooseblade.39
Thedecompressionofthenerverootcanbedoneonlyinadult patientswithradiculopathyandlowgradespondylolisthesis throughtheprocedureofGilletal.40However,thisprocedure
iscontraindicatedinpaediatricpatients,inwhomitshould alwaysbeaccompaniedbyanarthrodesis.
The reductionofhigh gradespondylolisthesis has been indicated,sincethisprocedureisabletoimprovetheaesthetic appearance, correct the lumbar angles, improve the pelvic indexandthesagittalbalanceandevenrecoverthe kypho-sisthatoccursinthelowerlumbarregion.40Inmostcases,
relativelymoreelongated.Becauseoftheseanatomical find-ings,thereductionmanoeuvrecanapplytensiontotheroots, withtheriskofneurologicalinjury.41
Final
considerations
The isthmic spondylolisthesis is an acquired disease that becomessymptomaticinyoungadults,because ofthe pre-maturedegenerative process ofthe intervertebral disc and facetjoints,aswellasthemechanicalimbalancesthatleadto changesinthesagittalbalanceofthecolumn.Theprogression ofslippageismorerareinadultsthaninchildren.
The radiographic examination of these patients should includethepanoramicradiographofthecolumnandthe visu-alizationofthefemoralheads,toallowanangularevaluation ofthelumbosacraljunctionandofthesagittalbalance.
Conservativetreatment with physicalrehabilitationand analgesicshasgenerallyshowngoodresults.
Thesurgicaltreatmentwithnerverootdecompressionand arthrodesisisindicatedincaseswheretheconservative treat-menthasfailedorthereisaprogressiveneurologicaldeficit. Theresultofsurgicaltreatmenthasbeengood interms of relievingthechroniclowbackandradicularpain.
Theclassificationsystem proposed bySDSGis practical andeasytoapplyandshouldbeusedandmorestudiedin ourcountry. Thepurpose ofthis classification emphasizes thatpatientswithspondylolisthesisL5/S1 forma heteroge-neousgroupwithseveralposturaladjustmentsandthatthis shouldbeconsideredbyphysicianswhenindicatinganytype of treatment. While we cannot employ an algorithm that establishesaspecifictreatmentforeach subtype,itis sug-gestedthatinpatientswithtype4ofspino-pelvicalignment, forcedattemptsatreductionmaynotbenecessary.Obtaining thesagittalalignmentwitharthrodesisand surgical instru-mentationisenough.Forthosepatientswithtype5,weshould preferablytrytoreduceandrealign,butinverydifficultcases, instrumentationandarthrodesisafterposturalreductionmay besufficientforobtainingthepropersagittalalignment,since thatthealignmentofthecolumnismaintained.The reduc-tionandalignmentaremandatoryintype6patients,inwhom thesagittalalignmentisseriouslyimpaired.
Thecircumferentialfusion(360◦)withsurgical instrumen-tationhasshownalowerrateofnon-union,butthiscannotbe correlatedwithresultssuperiortothoseoftheposterolateral arthrodesis.
Conflicts
of
interest
Theauthordeclaresnoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. AhnUM,AhnNU,BuchowskiJM,KebaishKM,LeeJ,SongES, etal.Functionaloutcomeandradiographiccorrectionafter spinalosteotomy.Spine(Philadelphia,PA,1976).
2002;27(12):1303–11.
2. HerbiniauxG.Traitesurdiversaccouchemenslabprieuxet surpolypesdelamatrice.Brussels:JLDeBoubers;1782.
3.LonsteinJE.Spondylolisthesisinchildren.Cause,natural history,andmanagement.Spine(Philadelphia,PA,1976). 1999;24(24):2640–8.
4.NazarianS.Spondylolysisandspondylolytic spondylolisthesis.Areviewofcurrentconceptson pathogenesis,naturalhistory,clinicalsymptoms,imaging, andtherapeuticmanagement.EurSpineJ.1992;1(2):62–83. 5.HarrisIE,WeinsteinSL.Long-termfollow-upofpatientswith
grade-IIIandIVspondylolisthesistreatmentwithandwithout posteriorfusion.JBoneJointSurgAm.1987;69(7):960–9. 6.FredricksonBE,BakerD,McHolickWJ,YuanHA,LubickyJP.
Thenaturalhistoryofspondylolysisandspondylolisthesis.J BoneJointSurgAm.1984;66(5):699–707.
7.LoveTW,FaganAB,FraserRD.Degenerativespondylolisthesis developmentaloracquired?JBoneJointSurgBr.
1999;81(4):670–4.
8.WiltseLL.Theetiologyofspondylolisthesis.JBoneJointSurg Am.1962;44:539–60.
9.StewartTD.Theageincidenceofneural-archdefectsin Alaskannatives,consideredfromthestandpointofetiology.J BoneJointSurgAm.1953;35(4):937–50.
10.MohriakR,SilvaPDV,TrandafilovJuniorM,MartinsDE, WajchenbergM,CohenM,etal.Espondilólisee espondilolisteseemginastasjovens.RevBrasOrtop. 2010;45(1):79–83.
11.MardjetkoS,AlbertT,AnderssonG,BridwellK,DeWaldC, GainesR,etal.Spine/SRSspondylolisthesissummary statement.Spine(Philadelphia,PA,1976).2005;306Suppl.:S3. 12.BerthonnaudE,DimnetJ,RoussoulyP,LabelleH.Analysisof
thesagittalbalanceofthespineandpelvisusingshapeand orientationparameters.JSpinalDisordTech.2005;18(1):40–7. 13.LegayeJ,Duval-BeaupèreG,HecquetJ,MartyC.Pelvic
incidence:afundamentalpelvicparameterfor
three-dimensionalregulationofspinalsagittalcurves.Eur SpineJ.1998;7(2):99–103.
14.RoussoulyP,GolloglyS,BerthonnaudE,LabelleH,
WeidenbaumM.Sagittalalignmentofthespineandpelvisin thepresenceofL5-s1isthmiclysisandlow-grade
spondylolisthesis.Spine(Philadelphia,PA,1976). 2006;31(21):2484–90.
15.LabelleH,Mac-ThiongJM,RoussoulyP.Spino-pelvicsagittal balanceofspondylolisthesis:areviewandclassification.Eur SpineJ.2011;20(Suppl.5):641–6.
16.HreskoMT,LabelleH,RoussoulyP,BerthonnaudE. Classificationofhigh-gradespondylolisthesesbasedon pelvicversionandspinebalance:possiblerationalefor reduction.Spine(Philadelphia,PA,1976).2007;32(20):2208–13. 17.Mac-ThiongJM,WangZ,deGuiseJA,LabelleH.Postural
modelofsagittalspino-pelvicalignmentanditsrelevancefor lumbosacraldevelopmentalspondylolisthesis.Spine (Philadelphia,PA,1976).2008;33(21):2316–25. 18.WiltseLL,NewmanPH,MacnabI.Classificationof
spondylolysisandspondylolisthesis.ClinOrthopRelatRes. 1976;(117):23–9.
19.MeyerdingHW.Spondylolisthesis.BoneJointSurg. 1931;13(1):39–48.
20.DeWaldRL.Spondylolisthesis.In:BridwellKH,DeWaldRL, editors.Thetextbookofspinalsurgery.2thed.Philadelphia: Lippincott-Raven;1997.p.1202–10.
21.MarchettiPC,BartolozziP.Classificationofspondylolisthesis asaguidelinefortreatment.In:BridwellKH,DeWaldRL, HammerbergKW,editors.Thetextbookofspinalsurgery.2nd ed.Philadelphia:Lippincott-Raven;1997.p.1211–54.
22.HermanMJ,PizzutilloPD,CavalierR.Spondylolysisand spondylolisthesisinthechildandadolescentathlete.Orthop ClinNorthAm.2003;34(3):461–7.
23.SmithJA,HuSS.Managementofspondylolysisand
24.CuryloLJ,EdwardsC,DeWaldRW.Radiographicmarkersin spondyloptosis:implicationsforspondylolisthesis
progression.Spine(Philadelphia,PA,1976).2002;27(18):2021–5. 25.Mac-ThiongJM,LabelleH.Aproposalforasurgical
classificationofpediatriclumbosacralspondylolisthesis basedoncurrentliterature.EurSpineJ.2006;15(10):1425–35. 26.BoxallD,BradfordDS,WinterRB,MoeJH.Managementof
severespondylolisthesisinchildrenandadolescents.JBone JointSurgAm.1979;61(4):479–95.
27.TebetMA,PasqualiniW,AlvesAP,AzuagaTL.
Espondilolistese.In:CristanteAF,BarrosFilhoTEP,editors. Coluna.RiodeJaneiro:Elsevier;2012.p.125–37.
28.McPheeIB,O’BrienJP,McCallIW,ParkWM.Progressionof lumbosacralspondylolisthesis.AustralasRadiol. 1981;25(1):91–5.
29.JankowskiR,NowakS,ZukielR,PucherA,BlokT.Surgical strategiesindegenerativelumbarspondylolisthesis. Columna.2006;5(1):99–103.
30.KatzJN,DalgasM,StuckiG,KatzNP,BayleyJ,FosselAH,etal. Degenerativelumbarspinalstenosisdiagnosticvalueofthe historyandphysicalexamination.ArthritisRheum. 1995;38(9):1236–41.
31.LabelleH,RoussoulyP,BerthonnaudE,TransfeldtE,O’Brien M,ChopinD,etal.Spondylolisthesis,pelvicincidence,and spinopelvicbalance:acorrelationstudy.Spine(Philadelphia, PA,1976).2004;29(18):2049–54.
32.RobilottaCC.Atomografiaporemissãodepositrons:uma novamodalidadenamedicinanuclearbrasileira.RevPanam SaludPublica.2006;20(2–3):134–42.
33.AndersonK,SarwarkJF,ConwayJJ,LogueES,SchaferMF. QuantitativeassessmentwithSPECTimagingofstress injuriesoftheparsinterarticularisandresponsetobracing.J PediatrOrthop.2000;20(1):28–33.
34.PanjabiMM.ThestabilizingsystemofthespinePartI. Function,dysfunction,adaptation,andenhancement.J SpinalDisord.1992;5(4):383–9.
35.MöllerH,HedlundR.Surgeryversusconservative managementinadultisthmicspondylolisthesis–a
prospectiverandomizedstudy:part1.Spine(PhiladelphiaPA, 1976).2000;25(13):1711–5.
36.TebetMA,PasqualiniW,CarvalhoMP,FusãoAF,SeguraEL. Tratamentocirúrgicodaespondilolistesedegenerativae ístmicadacolunalombar:avaliac¸ãoclínicaeradiológica. Coluna.2006;5(1):109–16.
37.SukSI,LeeCK,KimWJ,LeeJH,ChoKJ,KimHG.Adding posteriorlumbarinterbodyfusiontopediclescrewfixation andposterolateralfusionafterdecompressionin
spondylolyticspondylolisthesis.Spine(Philadelphia,PA, 1976).1997;22(2):210–9.
38.LaRosaG,ContiA,CacciolaF,CardaliS,LaTorreD, GambadauroNM,etal.Pediclescrewfixationforisthmic spondylolisthesis:doesposteriorlumbarinterbodyfusion improveoutcomeoverposterolateralfusion?JNeurosurg. 2003;99(Suppl.2):143–50.
39.JacobsWC,VreelingA,DeKleuverM.Fusionforlow-grade adultisthmicspondylolisthesis:asystematicreviewofthe literature.EurSpineJ.2006;15(4):391–402.
40.GillGG,ManningJG,WhiteHL.Surgicaltreatmentof spondylolisthesiswithoutspinefusion;excisionoftheloose laminawithdecompressionofthenerveroots.JBoneJoint SurgAm.1955;37(3):493–520.