w w w . r b o . o r g . b r
Case
Reports
Complications
after
total
knee
arthroplasty:
periprosthetic
fracture
after
extensor
mechanism
transplantation
夽
,
夽夽
Camilo
Partezani
Helito
a,∗,
Leonardo
Pozzobon
b,
Riccardo
Gomes
Gobbi
c,
Jose
Ricardo
Pecora
d,
Gilberto
Luis
Camanho
eaOrthopedist,PreceptoroftheKneeGroup,InstituteofOrthopedicsandTraumatology,HospitaldasClínicas,FaculdadedeMedicina,
UniversidadedeSãoPaulo(HC-FMUSP),SãoPaulo,SP,Brazil
bResidentPhysicianintheKneeGroup,InstituteofOrthopedicsandTraumatology,HC/FMUSP,SãoPaulo,SP,Brazil
cAttendingPhysicianintheKneeGroup,InstituteofOrthopedicsandTraumatology,HC/FMUSP,SãoPaulo,SP,Brazil
dAttendingPhysician,HeadoftheKneeGroup,InstituteofOrthopedicsandTraumatology,HC/FMUSP,SãoPaulo,SP,Brazil
eTitularProfessoroftheDepartmentofOrthopedicsandTraumatology,FMUSP,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received19July2012 Accepted3October2012
Keywords:
Arthroplasty,replacement,knee Postoperativecomplications Infection
a
b
s
t
r
a
c
t
WiththeincreaseintotalkneereplacementsinBrazilthereisalsoanincreaseinthenumber ofcomplications.Theauthorsreportacaseinwhich3seriouscomplicationshappenedafter atotalkneereplacementandthetreatmentwasbasedontheliterature,butindividualized tothepatientinsomeimportantpoints.Theoutcomewasconsideredverygood.
©2013SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Complicac¸ões
após
artroplastia
total
de
joelho:
fratura
periprotética
após
transplante
do
mecanismo
extensor
Palavras-chave: Artroplastiadojoelho Complicac¸õespós-operatórias Infecc¸ão
r
e
s
u
m
o
Comoaumentodonúmero de artroplastias noBrasilexisteum aumentosignificativo tambémnonúmero desuascomplicac¸ões. Osautores relatamum casode trêsgraves complicac¸õesapósumaartroplastiatotaldojoelhoemqueotratamentofoifeitobaseado naliteratura,porémindividualizadoemalgunspontosparaasnecessidadesdapacienteem questão.Odesfechofoiconsideradodesucesso.
©2013SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora Ltda.Todososdireitosreservados.
夽Pleasecitethisarticleas:HelitoCP,PozzobonL,GobbiRG,PecoraJR,CamanhoGL.Complicac¸õesapósartroplastiatotaldejoelho:
fraturaperiprotéticaapóstransplantedomecanismoextensor.RevBrasOrtop.2013;48:460–464.
夽夽
StudyconductedattheMedicalInvestigationLaboratoryfortheMusculoskeletalSystem,DepartmentofOrthopedicsand Traumatol-ogy,SchoolofMedicine,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil.
∗ Correspondingauthorat:RuaDr.OvídioPiresdeCampos,333,CerqueiraCesar,CEP05403-010,SãoPaulo,SP,Brazil.
E-mail:camilohelito@yahoo.com.br(C.P.Helito).
Introduction
Withnotablyincreasingnumbersoftotalkneearthroplasty proceduresinBrazilandworldwide,1thenumberof compli-cationsarealsoincreasingsignificantly.2–4 Thus,wepresent acaseinwhichasequence ofthreecomplicationsofhigh morbidityoccurred(dehiscenceoftheoperativewoundwith infection,failureofthe extensor mechanismand peripros-thetic fracture) but the patient nonetheless presented a positiveoutcomewithsatisfactorylimbfunction.
Case
report
Thepatient was an 81-year-old retired white woman. She underwenttotalleft-kneearthroplastyin2002andthentotal right-kneearthroplastyin2007.Onthefourthdayafterthe second operation, asshe left the hospitalupon being dis-charged,she fellfrom astanding positionand injured the anteriorregionofherknee. Thishaverisetodehiscenceof the operativewound and exposureof the prosthesis, with loss of the patellar component. The patient was readmit-tedtohospitalandunderwentasurgicalcleaningprocedure withcollectionofculturingsamplesand antibiotictherapy for six weeks in order to control a local infectious pro-cesscaused by multisensitiveStaphylococcus aureus. During the operation,around 60% ofthe remainder ofthe patella wasresectedbecauseoffragmentation.Thepatientevolved well with regard to her clinical condition and local infec-tion. However, during outpatient follow-up, she gradually developeda painful condition with inability toextend her kneeandlateraldislocationoftheremainderofthepatella uponactivecontractionofthequadriceps.Thisconsequently
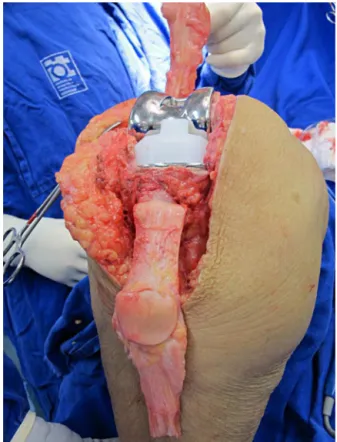
Fig.1–Transplantedextensormechanismfromatissue bankafterfixationinthetibia.
progressedtomedialinstabilityandamajoropeningof val-gus from 2007 to 2011. She did not present evidence of looseningofthefemoralandtibialcomponentsofthe arthro-plasty.
Fig.3–Patientwithactivekneeextensioninthe immediatepostoperativeperiod.
InOctober2011,thepatientunderwentasurgical proce-dureforreconstructionoftheextensormechanismandthe medialcollateralligamentusinganautologousgraft froma tissuebank.Acompleteextensormechanism(quadriceps ten-don,patella, patellar tendon and anterior tibialtuberosity) (Fig.1)andtwoflexortendonswereusedforthemedial liga-mentcomplex.
Asocketwascutintheregionoftheanteriortibial tuberos-ityinordertoinsertthepress-fittedboneplugofthegraft, togetherwitha4.5mmcorticalscrewwithawasher(Fig.2).
Duringtheoperation,itwasobservedthatthetibialand femoralcomponentswerefixedandwellpositioned,andno exchangesweremade.
Thepatientalreadypresentedactivekneeextensionduring theimmediatepostoperativeperiod(Fig.3)andhad satisfac-toryevolutionuntilfourmonthsafterthesurgery,whenshe
startedtopresentaconditionofpainanddifficultyin extend-ingtheknee.
Fromradiographsproducedduringtheoutpatient follow-up, atibialperiprosthetic fracture wasobservedjustbelow thecomponentinthedistalregionoftheosteotomyofthe anteriortibialtuberosity.Onceagain,itwasseenthatthe tib-ial componentdidnotshowany signsofloosening.Atthe outpatientconsultation,thepatientalreadypresentedsigns ofinitialconsolidationofthe fracture,suchthatitwasnot possibletoestablishexactlywhenithadoccurred(Fig.4).
Althoughsurgicaltreatmentforthefractureinquestionis recommendedintheliterature,itwasdecidedtouse conser-vativetreatmentwithakneeimmobilizerextendingfromthe inguinaltothemalleolarareaandloadrestriction,sincethe radiographsalreadyshowedsomesignsofinitial consolida-tion.
Aftertwomonthsofconservativetreatment,thepatient wasfreefrompain, withactivekneeextension,quadriceps strengthofgradeIVandkneerangeofmotionof0–100◦,and alsonolongerpresentedvalgusinstability.Theradiographic examinationsshowedthatcompleteconsolidationhadtaken place,bothofthefractureandofthetibialcomponentofthe graft(Figs.5and6).
Discussion
Manycomplicationsmayoccuraftertotalkneearthroplasty. Infection or dehiscence of the operative woundshould be treatedaggressively, withserialdebridement andantibiotic therapyasearlyaspossible.Althoughthecaseinquestion presentedacutely,withexposureoftheprosthesisafter ante-riortraumatotheknee,manycasesmaypresentinalessfully manifestedformanditwillbeuptothesurgeontotakea deci-sionregardingwhethertomanagethecasemoreaggressively becauseofsuspecteddeepinfection.5,6Inthismanner,there
Fig.5–Frontalandlateralradiographsshowingperiprostheticfracturingnowfullyconsolidated.
isahighchanceofcuringtheinfectiousprocessandsalvaging thecomponentsofthearthroplastyincasesofacuteinfection. Afterbecomingcuredfromtheinfection,ourpatientthen evolvedwithfailureoftheextensormechanism,another com-plicationthathasbeendescribedasdifficult-to-treatinthe literature,7 and valgusfailure oftheknee. For along time, arthrodesiswastheonlyviableoptionforthistypeof con-dition. With the advent of tissue banks, new possibilities started toappear, and wedecided toperform transplanta-tionofanautologousextensormechanism fromthe tissue bankoftheInstituteofOrthopedicsandTraumatology(IOT) of Hospital das Clínicas, Faculdade de Medicina, Universi-dadedeSãoPaulo(HC-FMUSP).Verysatisfactoryresultsfrom thisprocedure havealreadybeen reportedinthe literature
Fig.6–Patientwithactivekneeextensionafter consolidationofthefracturethroughconservative treatment.
internationally,8 although there are no Brazilian published dataonthistopic.
Evenwiththehighcomplicationratefromthisprocedure, including infection and the addedmorbidity dueto recon-structionofthemedialcollateralligament,anexcellentresult wasobtainedforourpatient.Sheachievedactiveextension immediatelyaftertheinitialprocedureandthemedialrepair wassuccessful,withacuteimprovementofthevalgus insta-bilitythatwasmaintainedduringtheoutpatientfollow-up.
Afterthegoodevolutionbothoftheextensormechanism and ofthevalgusinstability,the patientevolvedwith frac-turing in the distal region ofthe prosthesis. There are no reportsintheworldwideliteratureofperiprostheticfractures followingtransplantationofanextensormechanism,but it canbesaidthattheosteotomycausedboneweaknessinthe areawhereitwasperformed.Moreover,theproximityofthe tibialtunnelofthemedialgraftalsocontributedtoward weak-eningthemetaphysealregionofthetibia.Contrarytowhat the treatmentalgorithmsrecommend forsuchfracturesof thetibiafollowingkneearthroplasty,9,10wedecidedto insti-tuteconservativetreatmentbecauseofthepatient’sadvanced ageandthehighmorbidityofanewsurgicalprocedure.This treatmentconsistedofusinganimmobilizer extendingthe inguinaltothemalleolarregionandlimitingtheloadborne bythelimb.Aftertwomonthsofthistreatment,weobtained asatisfactoryresultwithactivekneeextensionand radiolog-icalimagingthatshowedconsolidationofboththefracturing andtheosteotomy.
Conflicts
of
interest
r
e
f
e
r
e
n
c
e
s
1. LosinaE,ThornhillTS,RomeBN,WrightJ,KatzJN.The dramaticincreaseintotalkneereplacementutilizationrates intheUnitedStatescannotbefullyexplainedbygrowthin populationsizeandtheobesityepidemic.JBoneJointSurg Am.2012;94:201–7.
2. GarvinKL,KonigsbergBS.Infectionfollowingtotalknee arthroplasty:preventionandmanagement.InstrCourseLect. 2012;61:411–9.
3. SchoderbekJrRJ,BrownTE,MulhallKJ,MounasamyV,IorioR, KrackowKA,MacaulayW,SalehKJ.Extensormechanism disruptionaftertotalkneearthroplasty.ClinOrthopRelat Res.2006;446:176–85.
4. PlatzerP,SchusterR,AldrianS,ProsquillS,KrumboeckA, ZehetgruberI,etal.Managementandoutcomeof periprostheticfracturesaftertotalkneearthroplasty.J Trauma.2010;68:1464–70.
5.D’EliaCO,SantosALG,LeonhardtMC,LimaALLM,PécoraJR, CamanhoGL.Tratamentodasinfecc¸õespós-artroplastiatotal dejoelho:resultadoscom2anosdeseguimento.ActaOrtop Bras.2007;15:158–62.
6.ParviziJ,ZmistowskiB,AdeliB.Periprostheticjointinfection: treatmentoptions.Orthopedics.2010;33:659.
7.SpringerBD,DellaValleCJ.Extensormechanismallograft reconstructionaftertotalkneearthroplasty.JArthroplasty. 2008;23Suppl.7:35–8.
8.BurnettRS,ButlerRA,BarrackRL.Extensormechanism allograftreconstructioninTKAatameanof56months.Clin OrthopRelatRes.2006:159–65.
9.FelixNA,StuartMJ,HanssenAD.Periprostheticfracturesof thetibiaassociatedwithtotalkneearthroplasty.ClinOrthop RelatRes.1997:113–24.