www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
The
institutionalized
elderly:
sociodemographic
and
clinical-functional
profiles
related
to
dizziness
夽
,
夽夽
Tábada
Samantha
Marques
Rosa
a,∗,
Anaelena
Braganc
¸a
de
Moraes
b,c,
Valdete
Alves
Valentins
dos
Santos
Filha
a,d,eaPostgraduatePrograminHumanCommunicationDisorders(PPGDCH),UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,
RS,Brazil
bDepartmentofStatistics,UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil cEpidemiology,UniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,RS,Brazil dSpeechTherapyCourse,UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil
ePostgraduatePrograminCommunicationSciences---HumanCommunication,UniversidadeFederaldeSantaMaria(UFSM),
SantaMaria,RS,Brazil
Received10September2014;accepted2February2015 Availableonline11December2015
KEYWORDS
Elderly;
Long-stayinstitution fortheelderly; Healthprofile; Dizziness
Abstract
Introduction:Dizzinessisamongthemostcommoncomplaintsintheelderlypopulation.
Objective: Todeterminethesociodemographicandclinical-functionalprofilesof institutional-izedelderlypeoplerelatedtodizziness.
Methods:Cross-sectional prospective study with institutionalizedelderlypeopleaged 60 or more years.A questionnaireonsociodemographicandclinical-functional characteristicswas applied,andananamnesisofoccurrenceofdizzinesswasheld,aswellastheDizzinessHandicap Inventoryquestionnaire.
Results:48.9%oftheelderlysubjectshaddizziness.Themeannumbersofdiseasesand medica-tionsassociatedwithdizzinesswere,respectively,4.5diseasesand7.8medications.Wefound asignificantassociationbetweentheoccurrenceofdizzinessanddiseasesofthe musculoskele-talsystem,sub-connectivetissueandgenitourinarysystem,aswellastheuseofmedications forthemusculoskeletalsystem.ThescoresforhandicapdegreeinfunctionalDHIwere signif-icantlyhigheramong elderlysubjectswhoneededwalkingaids,whohadsufferedfalls,and thosemanifestinganxiety.
夽 Pleasecitethisarticleas:RosaTSM,deMoraesAB,dosSantosFilhaVAV.Theinstitutionalizedelderly:sociodemographicand clinical-functionalprofilesrelatedtodizziness.BrazJOtorhinolaryngol.2016;82:159---69.
夽夽Institution:UniversidadeFederaldeSantaMaria(UFSM),SantaMaria,RS,Brazil. ∗Correspondingauthor.
E-mail:samarqs@hotmail.com(T.S.M.Rosa). http://dx.doi.org/10.1016/j.bjorl.2014.12.014
Conclusion:Oursampleincludedsubjectsofadvancedage,primarilywomen,whowere institu-tionalizedlessthanfiveyears,withmultiplediseasesandpolypharmacyusers.Theypresented long-standing short-duration mixed dizziness, that occurred more than once a month and affectedmainlythefunctionalaspect.
© 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE
Idoso;
Instituic¸ãodelonga permanênciapara idosos;
Perfildesaúde; Tontura
Oidosoinstitucionalizado:perfissociodemográficoeclínico-funcionalrelacionadosà tontura
Resumo
Introduc¸ão:Atonturaestáentreasqueixasmaiscomunsdapopulac¸ãoidosa.
Objetivo:Determinarosperfissociodemográficoeclínico-funcionaldeidosos institucionaliza-doscomrelac¸ãoàtontura.
Método: Estudo prospectivo transversal, com idosos institucionalizados com ≥ 60 anos de idade.Foiaplicadoumquestionárioreferenteàscaracterísticassociodemográficase clínico-funcionais, assim como foi feita anamnese sobre a ocorrência de tontura, e aplicado o questionárioDizzinessHandicapInventory.
Resultados: 48,9%dosidososapresentaramtontura.Asmédiasdonúmerodedoenc¸ase medica-mentosassociadosàtonturaforam,respectivamente,4,5doenc¸ase7,8medicamentos.Houve associac¸ãosignificativaentreocorrência detontura edoenc¸asdosistemaosteomuscular,do tecido subconjuntivo e do aparelho geniturinário, bemcomo usode medicamentos para o sistemamusculoesquelético.OsescoresdograudehandicapnoDHIfuncionalforam significa-tivamentemaioresparaosidososquenecessitavamdeauxílioàmarcha,paraosquetiveram quedaeparaosqueapresentaramansiedade.
Conclusão:Amostracaracterizadapormulheresdeidadeelevada,commenosdecincoanos deinstitucionalizac¸ão,commúltiplasdoenc¸asemedicamentos.Apresentamtonturamista,de curtadurac¸ão,comsurgimentoháanos,manifestando-semaisdeumavezaomês,prejudicando principalmenteoaspectofuncional.
© 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Publi-cado por Elsevier Editora Ltda. Este é um artigo Open Access sob a licença CC BY (https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Humanagingcompromisescertainskillsofthecentral
ner-voussystem(CNS),andaffectsareasresponsibleforsignal
processing from the vestibular, visual and proprioceptive
systems.Thesesensorysystemsareessentialfor
maintain-ing body balance and when affected, negatively impact
the ability to change adaptive reflexes,1 responsible for
postural control and orientation of the body relative to
space.2
Dizzinessis amongthemost commoncomplaintsinthe
elderly and may be characterized as a sense of
giddi-ness,afeelingof‘‘light-headedness’’,asenseofimminent
fall,instability,afloatingsensation,vertigo,atendencyto
deviate when walking, body imbalance, falls, and spatial
disorientation, among others.3 These changes may result
infractures,lossofmobility anddependenceonothersto
performdailyactivities.4
Intheworld’spopulation,10---15%ofpeoplehave
dizzi-ness,andthiscomplaintranksseventhplaceamongthose
most frequently found in women, and is the fourth most
common complaint among men. After 65 years, balance
changesareconsidered tobethemostcommonsymptoms
inthegeriatricpopulation,reachingaprevalenceof85%.5
ThreeoutoffourAmericansaged70orolderhavepostural
balanceproblems.6The causesofdizzinessmaybe
associ-ated withorganicand/or psychicdysfunction,whichhave
extra-vestibular (visual, neurological,emotional) or
vesti-bularorigin.7,8
Inordertoquantifyinterferencesfromphysicaland
func-tional/emotional dizzinesson daily activities ofa subject
suffering vertigo, aspecific questionnaire called Dizziness
HandicapInventory (DHI)wasdeveloped andvalidated by
Jacobson and Newman,9 with the aim of evaluating the
self-perception of the incapacitating effects caused by
dizziness.10InastudyinwhichDHIwasapplied,allelderly
subjectstestedshowedchangesinqualityoflife;physical
aspectswerethemostaffected,andfunctionalaspectswere
themostaffectedinolderindividuals.11
People with dizziness usually report difficulty with
mental concentration, memory loss and fatigue. Besides
generatingphysicalinsecurity,thesesymptomscanleadto
psychicinsecurity,irritability,lossofself-confidence,
Alsoinvolvedindizzinessinadditiontothefactors
men-tionedabove,alargenumberoftheelderlypopulationtake
multiple medicines (polypharmacy)because theyalso are
afflicted with a high number of comorbidities that bring
about physiologicalchangesin theirpharmacokineticsand
pharmacodynamics;thisadds totheongoing degenerative
process.13
The number of drugsused bythe elderlypopulation is
amajorriskfactorforiatrogenicevents,withan
exponen-tial relationship betweenmagnitude ofpolypharmacy and
the likelihoodof adverse reactions, druginteractions and
theuseofinappropriatedrugs.14Thus,elderlypeople
resid-ing in long-stay institutionsfor the elderly (LSIEs)are at
increased risk for iatrogenic events, due to disabling
dis-eases,frailtyandlow functionality,15 sometimesrequiring
drugprescription.
The use of tools to investigate the clinical-functional
status of elderly people with and without body balance
disorders,and therelationship tosociodemographic
char-acteristics, canadd informationtoassistthesearch for a
timelydiagnosisandamoreeffectivetherapeutic
orienta-tion.
Thus, the aim of this study is to determine the
socio-demographicand clinical-functionalprofiles of
insti-tutionalizedelderlysubjectsrelatedtodizziness.
Methods
Thisis across-sectionalhistoricalcohortstudy,conducted
inthreephilanthropiclong-stayinstitutionsfortheelderly
fromAugust2013toJanuary2014.Thestudywasapproved
by the Research Ethics Committee under opinion number
322,139 onits 20June 2013session. In orderto obtain a
FreeandInformedConsentTerm(FICT),wecompliedwith
therecommendationsfromResolutionnumber466/2012of
the National Council of Health, which regulates research
involvinghumanbeings.
The subjects signedtheFICT formafter readingit and
withtheirconcerns andquestionsalreadyclarified by the
researcher.Forthosepresentingsomemotorand/orvisual
disabilitythatpreventedthemfromwriting,theformwas
signedbytheheadoftheinstitution.
For sample selection, the following inclusion criteria
were considered: individuals aged ≥60 years, according
to Decree number 1,395/GM of the National Health
Pol-icy for the Elderly,16 residing in a charitable long-stay
home. Individualspresenting neurological disorders;
judg-ment, language and/or cognition loss, or dementia, who
werenotbeingabletounderstandthenecessaryprocedures
for theassessment ofstudy variables,would notagreeto
takepartinthestudyorsigntheFICTform,wereexcluded
fromthisstudy.
Thiswasaconsecutive,conveniencesampletotaling142
elderlysubjects.Ofthese,44wereexcludedbecausethey
fell below the minimum cutoff level of 10 points in the
evaluation of the Mini-Mental State Examination (MMSE)
measuringtheabilityofunderstandingandverbal
communi-cation,accordingtoFolstein,FolsteinandMcHugh.17 Thus,
thefinalsampleconsistedof98elderlyindividuals;32were
maleand66female.
Becauseofthelimitedinformationoneducationinthe
medical records of the elderly subjects, and considering
that the classification of Folstein, Folstein and McHugh17
presentslargescorerangesforthecategorizationof
demen-tia,wedecidedinfavorofthatclassificationinthisstudy.
Theevaluationsof theelderlysubjectswereheld
individ-uallyinaroommadeavailablefortheseactivitiesineach
LSIE. A meeting withthe head of each institution to
dis-cusstheoperationalorganizationofthisresearch,hadbeen
completedpreviously.
At first, the elderly were evaluated through a
ques-tionnairecomposedof openandclosedquestionsduringa
face-to-faceinterview.Thisinstrumenthadbeenpreviously
testedwith30seniors,andthenecessarycorrectionswere
made.Forelderlysubjectspresentingdifficultyof
expres-sionofspokenlanguage,theassistanceoftheircaregivers
wasrequested,andforthosewhoshowedfatigueduringthe
interviewanadditionalinterviewwasscheduled.
Thestudyvariableswereclassifiedassocio-demographic
(gender,age,skincolor,maritalstatus,educationandtime
sincebeinginstitutionalized),whichwereobtaineddirectly
frommedicalrecords,andclinical-functional.The
clinico-functionalgroupincludedthenumberandtypeofdiseases
anddrugs,classifiedaccordingtotheInternational
Classifi-cationofDiseases(ICD-10)andtheAnatomicalTherapeutic
Chemical(ATC)ClassificationIndex,theuseofwalkingaids,
theoccurrenceoffalls,fracturesinupperandlowerlimbs
relatedtofalls,asubjectiveperceptionofvisionand
hear-ing(verypoor,poor,fair,good,orexcellent),thefrequency
ofphysicalactivityandemotionalissuessuchaspresenceor
absenceofanxietyanddepression,andwhetherthesubject
wasundergoingpsychologicaland/orpsychiatrictreatment.
It should be noted that the diagnosis of diseases and
prescribeddrugs was obtained directly from the medical
recordsofeachelderlysubject,forwhichtheLSIE’sdoctors
wereresponsible.
Subsequently, a history was obtained concerning the
occurrenceof dizziness, and information about its onset,
type,triggeringfactors,intensity andduration,frequency,
interference withdaily activities, and any
neurodegener-ative manifestations, habitsand subjective perception of
dizziness, as, classified according to the Visual Analogue
Scale(VAS),wasregistered.
Finally, the DHI questionnaire, developed by Jacobson
and Newman9 and containing 25 questions assessing
self-perceptionoftheincapacitatingeffectscausedbydizziness
(emotional,physicalandfunctionalaspects),wasapplied.
Thisquestionnairewasadaptedtotherealityof
institution-alizedelderlypersons.Toanalyzetheresults,threepossible
answerswereconsideredinthequestionnaire,withthe
fol-lowingscores:yes=4points;sometimes=2points,andno=0
points.Themaximumpossiblescoresinemotional,physical,
andfunctionaldomainswere32,36,and32points,
respec-tively,totalingapossiblemaximumscoreof100points.For
thetotal DHI score, the higherthe value, the higher the
degreeofdisabilityoftheelderlysubjectinthecontextof
dizziness.
To analyze statistical data, we initially conducted
a descriptive analysis and, later, an inferential
analy-sis using non-parametric tests: chi-square, Fisher exact,
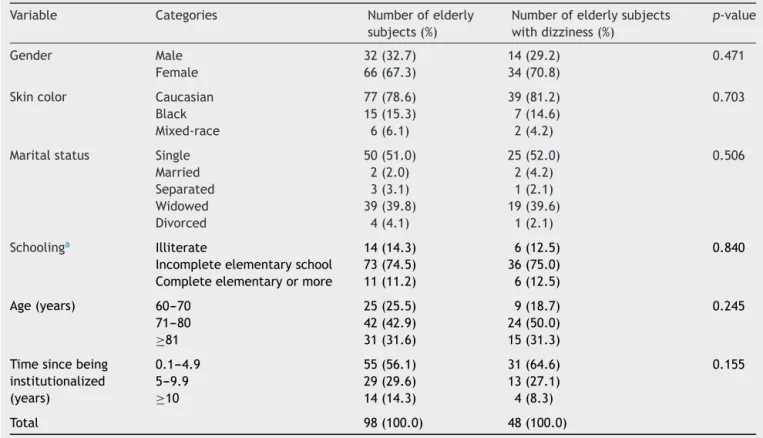
Table1 Distributionoffrequenciesofinstitutionalizedelderlypeoplewithrespecttosociodemographicaspectsanddizziness (n=98).
Variable Categories Numberofelderly subjects(%)
Numberofelderlysubjects withdizziness(%)
p-value
Gender Male 32(32.7) 14(29.2) 0.471 Female 66(67.3) 34(70.8)
Skincolor Caucasian 77(78.6) 39(81.2) 0.703 Black 15(15.3) 7(14.6)
Mixed-race 6(6.1) 2(4.2)
Maritalstatus Single 50(51.0) 25(52.0) 0.506 Married 2(2.0) 2(4.2)
Separated 3(3.1) 1(2.1) Widowed 39(39.8) 19(39.6) Divorced 4(4.1) 1(2.1)
Schoolinga Illiterate 14(14.3) 6(12.5) 0.840
Incompleteelementaryschool 73(74.5) 36(75.0) Completeelementaryormore 11(11.2) 6(12.5)
Age(years) 60---70 25(25.5) 9(18.7) 0.245
71---80 42(42.9) 24(50.0)
≥81 31(31.6) 15(31.3)
Timesincebeing institutionalized (years)
0.1---4.9 55(56.1) 31(64.6) 0.155
5---9.9 29(29.6) 13(27.1)
≥10 14(14.3) 4(8.3)
Total 98(100.0) 48(100.0)
Chi-squaretest,orFisher’sexacttest.
aIncompleteelementaryeducation,1---4yearsofschooling;completeelementaryeducationormore,≥5yearsofschooling.
significancewassetat 5%.Analyseswereperformed using
theSTATISTICA9.1software.
Results
Our sample consisted of 98 institutionalized elderly
sub-jects,withameanageof 76.3years(±8.5),ranging from
60to94 years.The meantimeof institutionalization was
5.6years(±6.9),rangingfrom2.4monthsto42years.With
respecttodizzinesscomplaints(n=48),48.9%reportedthat
theyexperienced dizziness.Therewasnosignificant
asso-ciation of dizziness with the socio-demographic variables
considered.
Table1liststhedistributionofelderlysubjectsaccording
tosocio-demographicvariables,andtheirassociation with
theoccurrenceofdizziness.
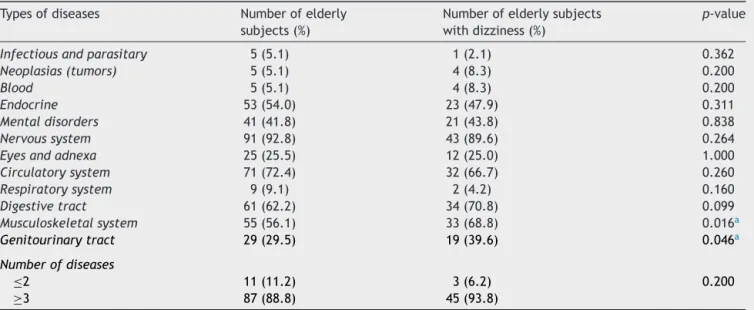
Table2showsdataontheprevalenceofdiseasesamong
theelderly,andassociationswiththeoccurrenceof
dizzi-ness.
Table 3 lists data onthe frequency distribution of the
typesofdrugsused,aswellasassociationswiththe
occur-renceofdizziness.
Themeannumberofassociateddiseasesper
institution-alizedelderlysubjectwas4.5(±1.6),withamaximum of
8;10elderlypatients(10.2%)presented1or2diseases,39
(39.7%)had3or4diseases,and48(48.9%)had≥5diseases.
Astothenumberofmedicationsused,wefound7.8(±3.7)
drugsperelderlysubject,withamaximumof17drugs.All
theelderlysubjectsinthisstudyweretakingsomekindof
medication.
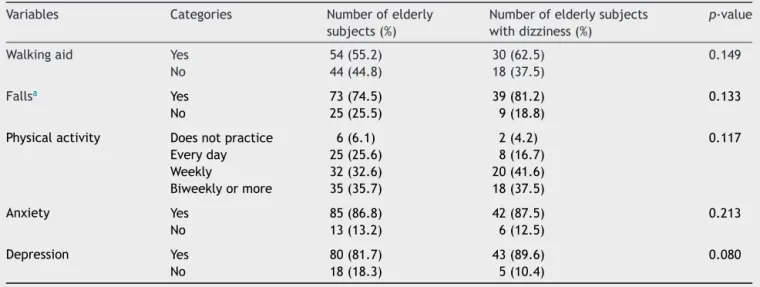
Table4showstheprevalenceofotherclinical-functional
characteristics: use of walking aids, occurrence of falls,
physical activity,anxiety, depression, and the association
ofthesevariableswiththeoccurrenceofdizziness.
Althoughithasbeenshownthattheoccurrenceoffalls
andpresenceofanxietyanddepressionhavenosignificant
associationwithdizziness,ourfindingsdemonstrate
impor-tant numerical differences with regard to complaints of
dizzinessamongelderlypeoplewithor withoutsuch
mor-bidities.
Historical data revealed that 29.2% of elderly patients
with dizziness had suffered fractures due to falls, but a
significant association (p=0.562) was not found. As for
self-perceptionofsightandhearing,ahighnumberof
sub-jects chose the ‘‘normal’’ option for both sight (40.8%)
and hearing (36.7%). Considering only those who
experi-enced dizziness, the ‘‘poor’’ option was chosen for both
sight(35.4%)andhearing(37.5%).Wemustemphasizethat,
considering the group of elderly patients with dizziness,
60.4% are or were in psychological treatment, and 16.6%
areorwerereceivingpsychiatrictreatment.
Table 5 shows the characteristics of dizziness (onset,
type,triggeringfactors,durationandfrequency).
Regarding self-perception of the intensity of dizziness
by the elderlyas measured by EVA,a meanof 6.2 points
(±1.1)(range:3---8points)wasobtained.Therewasno
Table2 Clinical-functionalcharacteristicsofinstitutionalizedelderlypeopleandassociationbetweenthetypesandnumber ofdiseasesandoccurrenceofdizziness(n=98).
Typesofdiseases Numberofelderly subjects(%)
Numberofelderlysubjects withdizziness(%)
p-value
Infectiousandparasitary 5(5.1) 1(2.1) 0.362
Neoplasias(tumors) 5(5.1) 4(8.3) 0.200
Blood 5(5.1) 4(8.3) 0.200
Endocrine 53(54.0) 23(47.9) 0.311
Mentaldisorders 41(41.8) 21(43.8) 0.838
Nervoussystem 91(92.8) 43(89.6) 0.264
Eyesandadnexa 25(25.5) 12(25.0) 1.000
Circulatorysystem 71(72.4) 32(66.7) 0.260
Respiratorysystem 9(9.1) 2(4.2) 0.160
Digestivetract 61(62.2) 34(70.8) 0.099
Musculoskeletalsystem 55(56.1) 33(68.8) 0.016a
Genitourinarytract 29(29.5) 19(39.6) 0.046a
Numberofdiseases
≤2 11(11.2) 3(6.2) 0.200
≥3 87(88.8) 45(93.8)
Blood,bloodandhematopoieticorgans,andimmunedisorders;Endocrine,nutritionalendocrineandmetabolicdiseases;mental disor-ders,mentalandbehavioraldisorders.Chi-squareorFisher’sexacttest.
a Significantassociation(p≤0.05).
theintensityofdizzinessintheagegroups.However,in
rela-tiontogender, menshowedsignificantlyhighervaluesfor
intensityofdizzinesscomparedtowomen(p=0.012).
Considering only those elderly individuals who
com-plained of dizziness, we identified that the most
com-promised daily activity was physical activity (87.5%).
Neuro-vegetativesymptomswereidentifiedin52.1%ofthe
elderly;thesymptomsmostcommonlyreportedwere
nau-sea (29.2%), tachycardia (18.8%), sweating and diarrhea
(4.2%). Among the habits of the elderly with dizziness,
coffee consumption was the most frequently mentioned
(87.5%),followed by the consumption of ‘‘chimarrão’’(a
typeoftea)(58.3%),sugar(56.3%),andtobacco(6.3%).
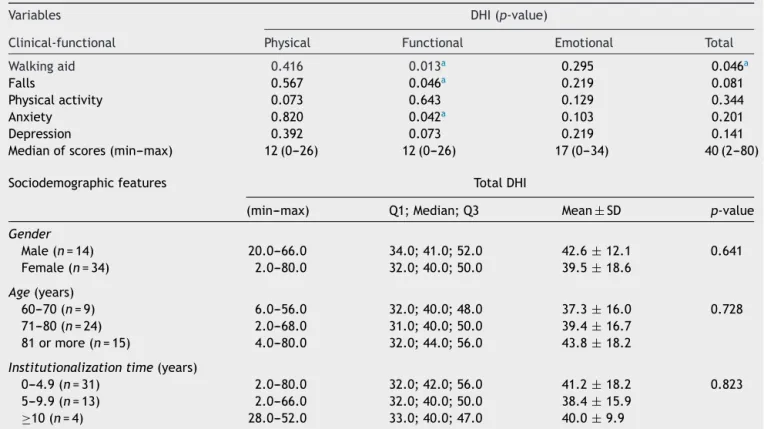
Table 6 lists a comparison of the scores for DHI
sub-scaleswithrespecttotheuseof walkingaids,occurrence
offalls, physical activity,anxiety and depression, aswell
asdescriptivemeasuresoftotalDHIscoresbygender,age,
time since being institutionalized and the significance in
thecomparisonofthesescores.Althoughtheoccurrenceof
depression,eitherpreviousorcurrent,wasnotsignificantly
associatedwithdizziness,ahigherpercentageofdizziness
intheelderlycurrentlydepressedwasfound.
Table3 Clinical-functionalcharacteristicsofinstitutionalizedelderlypeopleandtheassociationbetweentypesandnumber ofdrugsandtheoccurrenceofdizziness(n=98).
Typeofdrug Numberofelderly subjects(%)
Numberofelderlysubjects withdizziness(%)
p-value
Otoneurological 20(20.4) 12(25.0) 0.321
Cardiovascularsystem 67(68.3) 30(62.5) 0.279
Digestivetract 82(83.6) 43(89.6) 0.172
Nervoussystem 88(89.7) 42(87.5) 0.520
Hematologicalsystem 1(1.0) 1(2.1) 0.490
Muscularsystem 55(56.1) 33(68.8) 0.016a
Respiratorysystem 8(8.1) 1(2.1) 0.060
Hormonalpreparations 55(56.1) 24(50.0) 0.309
Ophthalmological 24(24.4) 12(25.0) 1.000
Numberofdrugsa
1or2 7(7.1) 3(6.3) 0.506
3or4 14(14.3) 5(10.4)
≥5 77(78.3) 40(83.3)
Muscularsystem,musculoskeletalsystemandsub-connectivetissue;digestivetract,digestiveandmetabolictract;hormonal prepara-tions,systemichormonalpreparations.Chi-squareorFisher’sexacttest.
Table4 Clinical-functionalcharacteristicsofinstitutionalizedelderlypeopleand associationwith occurrenceofdizziness (n=98).
Variables Categories Numberofelderly subjects(%)
Numberofelderlysubjects withdizziness(%)
p-value
Walkingaid Yes 54(55.2) 30(62.5) 0.149 No 44(44.8) 18(37.5)
Fallsa Yes 73(74.5) 39(81.2) 0.133
No 25(25.5) 9(18.8)
Physicalactivity Doesnotpractice 6(6.1) 2(4.2) 0.117
Everyday 25(25.6) 8(16.7)
Weekly 32(32.6) 20(41.6)
Biweeklyormore 35(35.7) 18(37.5)
Anxiety Yes 85(86.8) 42(87.5) 0.213
No 13(13.2) 6(12.5)
Depression Yes 80(81.7) 43(89.6) 0.080
No 18(18.3) 5(10.4)
Chi-squaretestorFisherexacttestforassociation.
aDuringtheinstitutionalizationperiod.
With respectto functional DHI,statistical valueswere
significantlyhigherforthoseparticipantswhoneededsome
helptowalk,forthosewhosufferedfalls,andforthose
pre-sentinginananxietystate.InthecomparisonoftotalDHI
scores, according tosocio-demographic variables (gender,
age,andtimesincebeinginstitutionalized),nosignificant
differenceswerefound,butwedididentifyadirect
propor-tionalrelationshipbetweentheageoftheelderlyandtotal
DHIscore.
Discussion
Over the years, the sensory and motor systems
respon-sible for maintenance of equilibrium suffer degenerative,
infectiousandtraumaticprocessesthathindertheiroptimal
functioning.18
Although there was no significant association with
thosesocio-demographiccharacteristicsweconsideredwith
respecttotheimportanceoftheprevalenceofdizzinessin
Table5 Featuresofdizzinessininstitutionalizedelderlysubjects(n=48).
Variable Categories Numberofelderlysubjects withdizziness(%)
Onset Days 4(8.3)
Weeks 3(6.2) Months 13(27.0) Years 28(58.5) Type Rotational 20(41.6) Instability 5(10.4) Imbalance 26(54.1)
Fall 1(2.0)
Triggeringfactors Turntheheadfromsidetoside 19(39.7) Quicklyliftthetrunk 17(35.4) Standupfastfromasittingposition 10(20.8) Extendtheheadbackwards 2(4.1) Duration Longduration 21(42.6)
Shortduration 27(57.4) Frequency Everyday 17(35.4) Morethanonceamonth 26(54.2) Lessthanonceamonth 5(10.4)
Table6 Comparison between scoresofDHIsubscales andtotal DHIscore versusclinical-functional andsociodemographic aspectsofinstitutionalizedelderlypeople(n=48).
Variables DHI(p-value)
Clinical-functional Physical Functional Emotional Total Walkingaid 0.416 0.013a 0.295 0.046a
Falls 0.567 0.046a 0.219 0.081
Physicalactivity 0.073 0.643 0.129 0.344
Anxiety 0.820 0.042a 0.103 0.201
Depression 0.392 0.073 0.219 0.141
Medianofscores(min---max) 12(0---26) 12(0---26) 17(0---34) 40(2---80)
Sociodemographicfeatures TotalDHI
(min---max) Q1;Median;Q3 Mean± SD p-value
Gender
Male(n=14) 20.0---66.0 34.0;41.0;52.0 42.6± 12.1 0.641
Female(n=34) 2.0---80.0 32.0;40.0;50.0 39.5±18.6
Age(years)
60---70(n=9) 6.0---56.0 32.0;40.0;48.0 37.3± 16.0 0.728
71---80(n=24) 2.0---68.0 31.0;40.0;50.0 39.4±16.7
81ormore(n=15) 4.0---80.0 32.0;44.0;56.0 43.8±18.2
Institutionalizationtime(years)
0---4.9(n=31) 2.0---80.0 32.0;42.0;56.0 41.2± 18.2 0.823
5---9.9(n=13) 2.0---66.0 32.0;40.0;50.0 38.4±15.9
≥10(n=4) 28.0---52.0 33.0;40.0;47.0 40.0± 9.9
DHI,DizzinessHandicapInventory;Q1,1stquartile;Q3,3rdquartile;SD,standarddeviation.
Mann---WhitneyUorKruskal---Wallistests.
a Statisticalsignificanceforp≤0.05.
theelderly,wefoundthatagreatnumberof
institutional-izedelderlypersons(48.9%)complainedofdizziness;thisis
similartothe study by Borges,Garcia andRibeiro,19 who
identified a prevalence of 58.0% for dizziness complaints
intheirgroupofinstitutionalizedelderlypersons.Inother
studieswithcommunity-basedolderadults,theprevalence
ofdizzinesswasreportedtobe42%and45%.20,21
In the present study, 70.8% of the elderlypeople with
dizziness,werefemale,whichisinlinewithstudiesinthe
literature that found 53%20 and 80%22 of female patients
amongelderlypeoplewithvestibulardisorders.Thiscould
beexplained by agreater concern onthe part of women
to seek medical advice, compared to men,20,22 and also
bythefactthat,withmenopause,womenaremoreprone
toheart disease, suggesting a strictrelationship between
bloodpressureandfemalehormones.23 Withregardtoskin
color,mostelderlypatientswithdizziness(81.2%)were
Cau-casian,thoughthislackedstatisticalsignificance.Nostudies
werefoundestablishinganassociationofskincoloror
eth-nicdatawiththeoccurrenceofdizzinessintheelderly.In
studiespublished,whiteskincolorwaspresentin67.0%,24
80.5%,25 and 90.0%26 of institutionalized elderly persons,
similartoourstudy(78.6%ofolderpeoplewithwhiteskin
color).
As tomaritalstatus, most elderlysubjects weresingle
(51.0%). Other studies have found 38.9%27 and 63.0%24 of
single elderly subjects. No studies were found analyzing
dizzinessassociatedwithmaritalstatusinthispopulation.
Inthisstudy,thelevelofeducation‘‘completed
elemen-tary or more’’ occurred in 12.5% of elderly patients with
dizziness; most subjects withsuch symptom (75%) stated
an ‘‘incomplete elementary education’’; this association
lacked statistical significance. In the reviewed literature,
17.5%28and30.8%21 ofelderlypatientswithbalance
disor-dershad‘‘completedelementaryeducationormore.’’
Agreaterlevelof educationis thoughttoexerta
posi-tiveinfluenceinmaintainingbrainstructuresandincreasing
synapticdensity,whichhelpstoreducethedamagesuffered
bytheCNSwithaging.29
In this study, the majority of institutionalized elderly
subjectswerein the71---80 yearsrange,witha meanage
of 76.3 years,similar tothe study by Borges,Garcia and
Ribeiro19 thatfoundameanof74.6yearsfor
institutional-izedelderlypeople.Inanotherlongitudinalstudy,27.0%of
non-institutionalizedelderlysubjectsaged>65years
com-plainedofdizzinessduring thepreceding six months,and
54.0%ofthoseaged>70yearsreportedit,30whichisinline
withourfindings:57.1%prevalenceforelderlysubjectsaged
71---80years.
Oursubjectshadameanof5yearsand6monthssince
being institutionalized, affirming data from a study that
reported 5 years and 8 months.31 It is believed that the
institutionalization processoccurs because the elderlydo
nothaveadequatephysical,andpsycho-social,conditionsto
livealone,andsometimestheydonothavefamilysupport
Intheanalysisofclinical-functional characteristics,we
identifiedastatisticallysignificantdifferencebetweenthe
occurrenceof dizzinessand diseasesof the
musculoskele-talsystem,sub-connectivetissueandgenitourinarysystem,
withaprevalenceof56.1%and39.6%,respectively.Despite
the lack of a significant association, diseases of the
ner-vous system have been identified as the most prevalent
characteristics (89.6%). In the literature, lower
percent-ages were identified for diseases of the musculoskeletal
system and sub-connective tissue (41.2%),32 genitourinary
tract(12.5%)28andnervoussystem(10%).28
Itisimportanttonotethatchangesintheosteo-articular
systemsuchasphysiologicalosteopenia,cartilaginousaging,
sarcopeniaandreductionin nerveconduction velocityare
stronglyassociatedwiththeagingprocess.Painand
disor-dersof themusculoskeletal systemarethemost frequent
complaintsoftheelderly,andrheumaticdiseasesalsohad
ahigherincidencewithadvancingage,suchas
osteoporo-sis, osteoarthritis, and polymyalgia rheumatica.33 In the
samecontext,researchersstatethatdiseasesofthe
circu-latoryandmusculoskeletalsystems,asaresultofperipheral
and/orcentralinvolvement,canmanifestthemselvesinthe
formofbalancedisordersandcausesofinstability.2
Accordingtotheliterature,despitethelackof
neurologi-calsymptomsorsignsintheelderlypopulationdizzinessmay
arisein association with central nervoussystem diseases,
suchasvertebrobasilarinsufficiencyandmultiplesclerosis.
Thesediseasescanaffecttheperipheralvestibularsystem,
resultinginconcomitantlabyrinthinesymptomsandsigns.34
Regardingthenumberofdiseasesaffectingtheelderly,
wefoundameanof4.5diseases,with48.9%reportingfive
or more associated diseases. Although it lacked a
signifi-cantstatisticalcorrelation,wefoundthat93.8%ofelderly
patientswithdizzinesshavethreeor moreassociated
dis-eases.AsurveyofelderlyresidentsinthecityofCuiabá(MT)
revealedthepresenceofthreeormorediseasesin42.0%of
thesubjectswithdizziness.21Inanotherstudyconsistingof
institutionalizedelderlysubjects,thisoccurrenceindicated
a7.3timesgreaterchanceofhavinganepisodeofdizziness,
comparedtothosewhohadnodiseasesatall.35
Althoughmoreelderlysubjectstookmedicationsforthe
nervoussystem(89.6%),thedigestivesystem(83.6%)andthe
cardiovascularsystem (68.3%), thosetaking medicines for
themuscularsystem(57.3%)werestatisticallysignificantly
morelikelytoexperiencedizziness.
Astudy conductedin Finlandrevealed that
institution-alizedelderlysubjectswithoutdizzinesstookanaverageof
7.9drugsperperson,indicatingthatpolypharmacyinLSIEsis
stillacurrentproblem.36Inthepresentstudy,wefoundthat
ourpopulationusedameanof7.8medicationsperelderly
person,withamaximum numberof 17drugs,aswell asa
high incidence(83.3%) of subjectstaking 5 or more
med-ications.This findingreflects the international literature,
in which 74% of the elderly were in a state of
polyphar-macy, defined as taking more than five medications per
patient.37
Theprevalenceofpolypharmacyishighinvarioushealth
sectors,withaveragenumbersof9.9---13.6medicinestaken
by hospitalized patients; up to seven for patients in the
intensivecareunit,and7.2---8.1medicationsper
institution-alizedpatient.15Accordingtotheliterature,thehigherthe
consumptionofdrugsbytheelderlysuchasantipsychotics,
sedatives, antidepressants, antihypertensives, analgesics
andanxiolytics,thegreaterthepossibilityofpotential
inter-actionsandsideeffectsofdrugs,Almostallareassociated
withvertigo,imbalanceandepisodesoffalls.30
Inthisstudy,despite thelack of significantassociation
betweenclinical-functionalcharacteristicsof
institutional-izedelderlypersonsandoccurrenceofdizziness,therewasa
decreasingprevalenceof89.6%,87.5%and81.2%for
depres-sion, anxiety and falls, respectively, showing a clinically
importantrelationship.
Asforthe depressionassociatedwithdizzinessin
insti-tutionalized elderlypeople, in this study a prevalence of
89.6%wasobserved;thisdatacontrastswithasurveywhich
found a prevalence of 37.3% among elderly subjects in
thecommunity.21 Elderlypatientswithahighernumberof
depressivesymptomsaremorelikelytohavedizziness
com-paredtothosewithfewersymptoms;inaddition,theyalso
tendtoexperiencethefollowingconsequences:decreased
functionalperformanceindailyactivities,anxietyand
inse-curity,andinthecourseoftimetheseindividualsmayhave
moodchanges,thusworseningdepression.4
Withregardtofalls,thepresentstudyfoundhigh
preva-lence,differingfromotherstudiespublishedthatreported
aprevalenceof50.0%,1962.3%26 and14.9%.38
When asked about their self-perceived sightand
hear-ing, 35.4% and 37.5% of the elderly with dizziness,
respectively, chose a ‘‘poor’’ option. In another study
involvingcommunity-basedelderswithdizziness,an
occur-renceof visual(100%) andhearing(41%) impairmentswas
identified.21
Elderlypersonstend toshowinvolvementof other
sys-tems relatedtovestibularfunction,includinghearingand
visual impairment.28 Hearing impairment and presence of
vertigoareconditionsresultingfromthehighsensitivityof
auditory and vestibularsystems to commonclinical
prob-lems inthe process ofaging. These individualscommonly
indicatethattheirvisualsystemalsosufferstheeffectsof
advancing age,andocular changes, suchascataractsand
glaucoma,thatareresponsibleforadecreaseinvisual
acu-ity,andwhichcontributestostaticanddynamicinstability
ofthebody.2
Themainconsequenceofthenaturalagingprocessofthe
vestibularsystemisadegenerationofthevestibulo-ocular
reflex(VOR),39 theresultof whichis instabilitywithbody
rotation and, consequently, a deviation when walking.40
Withitsorigininthesemicircularcanals,VORoperates by
generatingeyemovementsatthesamespeedashead
move-ment,butintheoppositedirection,41 inordertomaintain
astablevisualfieldduringheadmovement,42thusallowing
acrisp,cleanimageevenduringmovement.41
Regardingdizzinesscomplaints,thepopulationofelderly
patients in our study reported that their episodes began
morethanoneyearago(58.5%).Ourdatadiffersfromthat
obtained inthe study bySouza,22 that showedthat 54.0%
reported an onset occurring five or more yearsago, thus
demonstratingthechronicnatureofdizzinessinthat
popu-lation.
Inourstudy,therewasapredominanceofnon-rotational
dizziness,definedasanimbalance,in54.1%oftheelderly
subjects, similar to the result obtained by Ferreira and
Yoshitome,38whofoundaprevalenceof46.2%.However,our
dizzinessin38.0%oftheelderlypopulationinthecityofSão Paulo.
Thetriggeringfactorsfordizzinessmoreoftenreported
by the elderly in this study were turning the head from
side toside (39.7%) and lifting thetrunk quickly (35.4%).
Some authors state that postural hypotension is
associ-ated with an increased risk of dizziness and falls.28,38 It
is common for older people to report various types of
movements being associatedwith dizziness. Studies show
that up to 74% of older people reported more than one
triggering activity resultingin dizziness,4,30 withthemost
frequently cited being rising from a decubitus position
(range of 45.9---58.0%)28 and turning the head (range of
25.8---67.5%).24Keepingtheheadstillinanypositionwasthe
mostcommonlyreportedtriggeringfactorfordizziness;this
wasidentifiedin60%oftheelderly.22Suchheadmovements
orpositionspromoteexcitationofthevestibularsystemand
oftencausevertigoandothertypes ofdizziness,asin the
casesofbenignparoxysmalpositionalvertigo(BPPV)
preva-lentinolderpatients.28
Short-term dizzinesswaspresent in 57.4%of the
insti-tutionalized elderly participants, in line with the studies
of Gassmann and Rupprecht30 and of Souza,22 in which
theprevalencewas48.9%and44%,respectively. Forthose
elderly who reported long-term dizziness this can be
explained by the difficulty in obtaining a full vestibular
compensationbytheagingpopulation.28
When askedabout thefrequencyof dizziness,54.2%of
theelderlyinourstudyreportedanoccurrenceofepisodes
ofmorethanonceamonth,whichagreeswiththefindingsof
Souza,22whofoundasporadicfrequencyofdizzinessin66%
ofelderlysubjects.Thatauthoralsoreportedthataregular
andconstantoccurrenceofdizzinessisusuallyseeninolder
peoplewithamorepronouncedanddisablingclinicaltype
ofdizziness.
Regardingself-perceptionofdizzinessintensityas
mea-suredbyEVA,inthecurrentstudyanaverageof6.2points
(±1.1)wasreported(minimumandmaximumscores:3and8
points,respectively),similartothefindingsofastudywith
elderly people with vestibular dysfunctionthat showed a
meanof6.62 points(±2.45)withminimumandmaximum
scoresofzeroand10,respectively.28Ourmalesubjectsalso
showedasignificantlystrongerintensityof dizziness(EVA)
whencomparedtowomen.However,wecouldnotfindany
studies investigatingthis association to compare withour
findings.
EVA is the most used tool for assessing the
subjec-tive perception of patientswith respecttothe degree or
intensity ofdizziness,43 postural instability,44 and/or body
imbalance.40,45
Inourstudy,thedailyactivitymostimpairedwas
physi-calactivity(87.5%).Astudyincludingactiveandsedentary
elderlysubjectsfromthecommunitynotedthatthegroup
ofsedentaryseniors(33%)hasmorecomplaintsofdizziness
thantheactiveones(20%).46
A prevalenceof neuro-vegetativesymptomsin
associa-tion with dizziness was reported by 52.1% of the elderly
subjects,whichagreeswithstudiesshowinganassociation
betweendizzinessandneuro-vegetativesymptomsand
psy-chological changes.3,28 In this study, the most commonly
reportedeatinghabitwascoffeeconsumption(87.5%).One
studysuggests thatcertaineatinghabitssuch asthe
con-sumptionofcoffee,matetea(‘‘chimarrão’’) andsugar,as
wellassmoking,amongothers,shouldbeavoidedbyelderly
patients with balance disturbances, as these habits may
exacerbatecochleovestibularsymptoms,makingthe
vesti-bularcompensationevenslower.47
Inthecurrent study,DHIfunctionaldomainindices are
significantlyhigherforolderpeoplewhoneedwalkingaids,
suffer falls, and for those who show anxiety, a finding
whichagrees witha studythat evaluatedelderlypatients
withchronic vestibulardisease andobserved a significant
association betweenfalls and functional DHI(p=0.010).48
AccordingtoPeresandSilveira,49thefunctionaldomainof
DHIis important tothe qualityof life of seniors, sinceit
interferes with the individual’s dependence on the social
context.
Scherer,Lisboaand Pasqualotti5 identifieda significant
difference(p=0.02)inthefunctionalaspectforcomplaints
ofbodyimbalance. Theirfindingsdifferfromstudies that
investigatedthemostimpairedfunctionaldomaininelderly
patientswithdizziness,withmeansof16.80and8.60points,
respectively.48,50
In the current study, we could identify a directly
pro-portional,butnotsignificant,relationshipbetweenelderly’s
ageandtotalDHIscore;thatis,forolderseniors,ahigher
totalDHIscorewasfound.Thisfindingisinlinewithastudy
that observed greater commitment of functional aspects
withincreasingage,butdidnotfindthesamerelationship
betweentotalDHIscoreandthepatient’sage.10
Changes in balance resulting from dizziness trigger a
series of psychosocial consequences that are manifested
throughnegativefeelings,interferingwithactivitiesofdaily
lifeoftheaffectedindividuals.11,34
Inviewof theseconsiderations,thisstudy makesclear
the need for interventions for the elderly in long-stay
institutions,aiming atprevention,promotion andpossible
rehabilitationofthehealthofinstitutionalizedelderly
per-sons,withtheobjectiveof reducingtheincidenceoffalls
andtheresultingconsequencesofsuchaccidents.
Conclusions
The typical elderly subject in our study of subjects with
dizzinessliving in long-stayinstitutions wasan unmarried
Caucasian women aged over 70 years, who did not
com-pleteanelementarylevelof educationandwhohadbeen
institutionalizedlessthanfiveyears.Shehadmultipleother
comorbidities, took multiple mediations, experienced a
mooddisorder,andwasundergoingpsychologicaltreatment.
Asagroup,oursubjectsindicatedthattheyhadpoorvisual
and auditory acuity, and experienced imbalance episodes
followedbyshort-duration vertigo,that hadbeen present
foryears,occurredmorethanonceamonth,weretriggered
byheadandbodymovementsandmainlyaffectedfunctional
aspects.
Conflicts
of
interest
References
1.TeixeiraCS,DornelesP,LemosLFC,PrankeGI,RossiAG,Mota CM.Avaliac¸ãodainfluênciadosestímulossensoriaisenvolvidos namanutenc¸ãodoequilíbriocorporalemmulheresidosas.Rev BrasGeriatrGerontol.2011;14:453---60.
2.Meireles AE,Pereira LMS,OliveiraTG, Christofoletti G, Fon-secaAL.Alterac¸õesneurológicasfisiológicasaoenvelhecimento afetamo sistemamantenedordoequilíbrio.RevNeurocienc. 2010;18:103---8.
3.Gananc¸aMM,CaovillaHH,Gananc¸aFF,DonáF,Branco-Barreiro F,PaulinoCA,etal.Comodiagnosticaretratarvertigem.Rev BrasMed.2008;65:6---14.
4.TinettiME,WilliamsCS,GillTM.Dizzinessamongolderadults:a possiblegeriatricsyndrome.AnnInternMed.2000;132:337---44. 5.SchererS,LisboaHRK,PasqualottiA.Tonturaemidosos: diag-nóstico otoneurológicoeinterferêncianaqualidadede vida. RevSocBrasFonoaudiol.2012;17:142---50.
6.DillonCF,GuQ,HoffmanHJ,KoCW.Vision,hearing,balance, andsensoryimpairmentinAmericansaged70yearsandover: UnitedStates,1999---2006.NCHSDataBrief.2010;31:1---8. 7.Santos JB, Garcia AP. Estudo do impacto da qualidade de
vidadeindivíduosportadoresdetontura.ActaORL.2007;25: 152---6.
8.ZeigelboimBS,KlagenbergKF,DaRosaMR,JurkiewiczAL, Mar-ques JM.Inter-relac¸ão do dizziness handicap inventory com oexame vestibularequeixasotoneurológicas.RevBrasMed. 2009;66:10---7.
9.Jacobson GP, Newman CW. The development of the dizzi-ness handicap inventory. Otolaryngol Head Neck Surg. 1990;116:424---7.
10.NishinoLK,GranatoL,CamposCAH.Aplicac¸ãodoquestionário dequalidadedevidadiáriaempacientespréepós-reabilitac¸ão vestibular.ArqIntOtorrinolaringol.2008;12:517---22.
11.CastroASO,GazollaJM,NatourJ,Gananc¸aFF.Versãobrasileira do Dizziness Handicap Inventory. Pró-Fono R Atual Cient. 2007;19:97---104.
12.Gananc¸aMM,CaovillaHH.Desequilíbrioereequilíbrio:vertigem temcura?SãoPaulo.Lemos.1998:13---9.
13.Rozenfeld S. Prevalência, fatores associados e mau uso de medicamentosentreosidosos:umarevisão.CadSaúdePública. 2003;19:717---24.
14.Passarelli MCG, Gorzoni ML. Iatrogenia: reac¸ões adversas a medicamentos.In:JacobFilhoW,GorzoniML,editors. Geria-triaegerontologia:oquetodosdeviamsaber.SãoPaulo:Roca; 2008.p.19---30.
15.Lucchetti G,GraneroAL, PiresSL, GorzoniML.Fatores asso-ciadosàpolifarmáciaem idososinstitucionalizados.RevBras GeriatrGerontol.2010;13:51---8.
16.Brasil. Ministério da Saúde Portaria n. 1.395/GM de 10 de dezembrode1999.PolíticaNacionaldeSaúdedoIdoso.Brasília. 17.FolsteinMF,Folstein SE,McHughPR.‘‘Mini-mental state’’.A practicalmethodforgradingthecognitivestateofpatientsfor theclinician.JPsychiatrRes.1975;12:189---98.
18.TinettiME,KumarC.Thepatientwhofalls:‘‘It’salwaysa trade-off’’.JAMA.2010;303:258---66.
19.Borges LL, Garcia PA, Ribeiro SOV. Características clínico-demográficas, quedas e equilíbrio funcional de idosos Institucionalizados e comunitários. Fisioter Mov. 2009;22: 53---60.
20.Bittar RSM, Oiticica J, Bottino MA, Gananc¸a FF, Dimitrov R. Estudo epidemiológico populacional da prevalência de tontura na cidade de São Paulo. Braz J Otorhinolaryngol. 2013;79:688---98.
21.MoraesSA,SoaresWJS,RodriguesRAS,FettWCR,FerriolliE, PerraciniMR.Tonturaemidososdacomunidade:estudodebase populacional.BrazJOtorhinolaryngol.2011;77:691---9.
22.SouzaRF [dissertac¸ão]Correlac¸ãoentreequilíbriocorporale capacidadefuncionaldeidososcomdisfunc¸õesvestibulares per-iféricas.SãoPaulo,SP:UniversidadeBandeirantedeSãoPaulo; 2011.
23.BarelM,LouzadaJCA,MonteiroHL,AmaralSL.Associac¸ãodos fatoresderiscoparadoenc¸ascardiovascularesequalidadede vida entre servidores da saúde. Rev Bras Educ Fís Esporte. 2010;24:293---303.
24.LisboaCR, Chianca TCM. Perfilepidemiológico, clínico e de independênciafuncionaldeumapopulac¸ãoidosa institucional-izada.RevBrasEnferm.2012;65:482---7.
25.Pelegrin AKAP, Araújo JA, Costa LC, Cyrillo RMZ, Rosset I. Idososde umaInstituic¸ãode LongaPermanênciadeRibeirão Preto: níveis de capacidade funcional. Arq Ciênc Saúde. 2008;15:182---8.
26.Gonc¸alvesLG,VieiraST,SiqueiraFV,HallalPC.Prevalênciade quedasemidososasiladosdomunicípiodeRioGrande,RS.Rev SaúdePública.2008;42:938---45.
27.DanilowMZ,MoreiraACS,VillelaCG,BarraBB,NovaesMRCG, OliveiraMPF.Perfilepidemiológico,sociodemográficoe psicos-socialdeidososinstitucionalizadosdoDistritoFederal.Comum CiêncSaúde.2007;18:9---16.
28.GazzolaJM,Gananc¸a FF,ArataniMC, Perracini MR,Gananc¸a MM. Caracterizac¸ão clínica de idosos com disfunc¸ão vestibular crônica. Braz J Otorhinolaryngol. 2006;72: 515---22.
29.ColcombeSJ,EricksonKL,ScalfPE,KimJS,PrakashR,McAuley E, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Sci Med Sci. 2006;61: 1166---70.
30.GassmannKG,RupprechtR. Dizzinessinanoldercommunity dwellingpopulation:amultifactorialsyndrome.JNutrHealth Aging.2009;13:278---82.
31.JensenJ,NybergL,GustafsonY,OlssonLL.Fallandinjury pre-ventioninresidentialcare ---effects inresidentswithhigher and lower levels of cognition. J Am Geriatr Soc. 2003;51: 627---35.
32.GushikemP[dissertac¸ão] Avaliac¸ãootoneurológicaemidosos comtontura.SãoPaulo,SP:UniversidadeFederaldeSãoPaulo; 2001.
33.SaderCS,RossiE.O.envelhecimentodosistemaosteoarticular. In:FreitasEV,PyL,NeriAL,Canc¸adoFAX,GorzoniML,Rocha SM,editors.TratadodeGeriatriaeGerontologia.RiodeJaneiro: GuanabaraKoogan;2002.p.508---14.
34.Gananc¸aMM,CaovillaHH,MunhozMSL,SilvaMLG,Gananc¸aFF, Gananc¸aCF.Avertigemexplicada:implicac¸õesterapêuticas. RevBrasMed.1999;6:1---20.
35.TamberAL,BruusgaardD.Self-reportedfaintnessordizziness comorbidityand useofmedicines.Anepidemiologicalstudy. ScandJPublicHealth.2009;37:613---20.
36.Hosia-RandellHM,MuurinenSM,PitkäläKH.Exposureto poten-tiallyinappropriatedrugsanddrug---druginteractionsinelderly nursinghome residentsinHelsinki, Finland:a cross-sectional study.DrugsAging.2008;25:683---92.
37.HanlonJT,WangX,GoodCB,RossiMI,StoneRA,SelmaTP,etal. Racialdifferencesinmedicationuseamongolder,long-stay vet-eransaffairsnursinghomecareunitpatients.ConsultPharm. 2009;24:439---46.
38.Ferreira DCO, Yoshitome AY. Prevalência e caraterísticas das quedas de idosos institucionalizados. Rev Bras Enferm. 2010;63:991---7.
39.ZeeDS. Vestibularadaptation. In:Herdman SJ,editor. Vesti-bularrehabilitation.1sted.Philadelphia:F.A.DavisCompany; 2000.p.77---86.
41.MaranhãoET,Maranhão-FilhoP.Vestibulo-ocularreflexandthe headimpulsetest.ArqNeuropsiquiatr.2012;70:942---4. 42.Zanardini FH, Zeigelboim BS, Jurkiewicz AL, Marques JM,
BassettoJM.Reabilitac¸ão vestibularem idosos comtontura. Pró-FonoRAtualCient.2007;19:177---84.
43.HånssonEE,ManssonNO,HåkanssonA.Effectsofspecific reha-bilitationfordizzinessamongpatientsinprimaryhealthcare. Arandomizedcontrolledtrial.ClinRehabil.2004;18:558---65. 44.Kammerlind AS, Håkansson JK, Skogsberg M. Effects of
bal-ancetraininginelderlypeoplewithnonperipheralvertigoand unsteadiness.ClinRehabil.2001;15:463---70.
45.HerdmanSJ,BlattP,SchubertMC,TusaRJ.Fallsinpatientswith vestibulardeficits.AmJOtol.2007;21:847---51.
46.Silva TO,Freitas RS, Monteiro MR, Borges SM. Avaliac¸ão da capacidadefísicaequedasem idososativosesedentáriosda comunidade.RevBrasClinMed.2010;8:392---8.
47.Mantello EB, Moriguti JC, Rodrigues-Júnior AL, Ferrioli E. Efeito da reabilitac¸ão vestibular sobre a qualidade de vida de idosos labirintopatas. Braz J Otorhinolaryngol. 2008;74: 1---14.
48.Santos EM, Gazzola JM, Gananc¸a CF, Caovilla HH, Gananc¸a FF. Impacto da tontura na qualidade de vida de idosos comvestibulopatiacrônica.Pró-FonoRAtualCient.2010;22: 427---32.
49.PeresM,SilveiraE.Efeitodareabilitac¸ãovestibularemidosos: quanto ao equilíbrio,qualidade de vida e percepc¸ão. Ciênc saúdecolet.2010;15:2805---14.