www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Partial
laryngectomy
in
glottic
cancer:
complications
and
oncological
results
夽
Agnaldo
José
Graciano
a,∗,
Marina
Sonagli
b,
Ana
Gabriela
Clemente
da
Silva
b,
Carlos
Augusto
Fischer
a,
Carlos
Takahiro
Chone
caDepartmentofSurgery,DivisionofOtolaryngologyandHeadandNeckSurgery,HospitalSãoJosé,Joinville,SC,Brazil bDepartmentofSurgery,HospitalSãoJosé,Joinville,SC,Brazil
cDepartmentofOtolaryngologyandHeadandNeckSurgery,UniversidadeEstadualdeCampinas(UNICAMP),Campinas,SP,Brazil
Received7November2014;accepted5May2015 Availableonline19October2015
KEYWORDS
Carcinoma; Larynx; Laryngectomy; Radiotherapy
Abstract
Introduction:Mostpatientswithlaryngealcarcinomapresenttumorsintheglottisthatcanbe treatedbydifferenttreatmentmodalities.Someauthorsconsideropenpartiallaryngectomy asobsolete,whileothersstilldeemthisasaviableandcost-efficientoption.
Objectives: Tocomparetheoncologicalandfunctionalresultsofaseriesofpatientsundergoing partiallaryngectomyvs.externalradiotherapyforthetreatmentofglotticcancer.
Methods:Historicalcohortstudywithaseriesofglotticcarcinomapatientsundergoingpartial laryngectomyorexternalradiotherapyduringaperiodoftenyears.
Results:Sixty-two patients withglottic carcinomawereincluded. Group A comprised those submitted topartiallaryngectomy(n=30),andGroup B,thosewhounderwentradiotherapy (n=32).Theywerehomogeneousinthecomparisonofmeanage,56.4vs.60.4years(p=0.12) anddistributioninpathologicalstage(p=0.91).Withregardtooncologicaloutcome,therewere nodifferencesindistantmetastasisrates,orsecondprimarytumorbetweengroups(p=1.0),as wellasindisease-freetime,laryngealrescue-freetime,andoverallfive-yearsurvival.Severe complicationrateswerealsosimilarbetweengroups.
Conclusion: Openpartiallaryngectomyhadcomplicationratesandoncologicalresultssimilar tothoseofradiotherapyfor patients withglotticcarcinomasandshouldstillbe considered amongthemainavailabletherapeuticoptions.
© 2015Associac¸˜aoBrasileira de Otorrinolaringologiae CirurgiaC´ervico-Facial.Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:GracianoAJ,SonagliM,daSilvaAGC,FischerCA,ChoneCT.Partiallaryngectomyinglotticcancer:complications
andoncologicalresults.BrazJOtorhinolaryngol.2016;82:275---80.
∗Correspondingauthor.
E-mail:entbrazil@gmail.com(A.J.Graciano). http://dx.doi.org/10.1016/j.bjorl.2015.05.011
PALAVRAS-CHAVE
Carcinoma; Laringe; Laringectomia; Radioterapia
Laringectomiaparcialnocâncerglótico:complicac¸õeseresultadosoncológicos
Resumo
Introduc¸ão:Amaioriadospacientescomcarcinomadelaringeapresentamtumoresnaregião glótica suscetíveis a diferentes modalidades de tratamento. Alguns autores consideram a laringectomia parcial aberta em desusoenquanto outros ainda aindicamcomo uma opc¸ão viávelecustoeficiente.
Objetivos: Compararosresultadosoncológicosefuncionaisdeumasériedepacientes submeti-dosàlaringectomiaparcialversusradioterapiaexternaparaotratamentodocâncerglótico.
Método: Estudotipocoortehistóricacomumasériedepacientescomcarcinomaglótico sub-metidosàlaringectomiaparcialouradioterapiaexternaemperíodode10anos.
Resultados: Foramincluídos62pacientescomcarcinomaglóticodistribuídosemGrupoA: sub-metido à laringectomia parcial (n =30) e Grupo B submetido a radioterapia (n= 32) que semostraram homogêneosnacomparac¸ãodemédia deidadede 56,4vs.60,4(p=0,12)e distribuic¸ãoemestadiospatológicos(p=0,91).Comrelac¸ãoaodesfechooncológico,nãoforam observadasdiferenc¸asnastaxasdemetástaseàdistancia,ousegundoprimárioentreosgrupos (p=1,0)assimcomonotempolivrededoenc¸a,tempolivrederesgatelaríngeoesobrevida geralem5anos.Astaxasdecomplicac¸õesseverastambémforamsemelhantesentreosgrupos.
Conclusão:A laringectomia parcial aberta apresentou taxas de complicac¸ões e resultados oncológicossemelhanteàquelesdotratamentoradioterápicoparapacientescomcarcinomas glóticoseaindadeveserconsideraentreasprincipaisopc¸õesterapêuticasdisponíveis. ©2015Associac¸˜aoBrasileira deOtorrinolaringologiaeCirurgiaC´ervico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Laryngealcarcinomavariesinincidencethroughout differ-entgeographicalregions,beingmorecommoninSouthern Europe(10.9/100,000), EasternEurope(9.2/100,000),and SouthAmerica(7.2/100,000).Thiscancerismorefrequent in males and corresponds to 2.5% of all tumors in men, representing the sixth most common malignancy in men inBrazil.1 Mostpatientswithlaryngealcarcinoma present
their tumor in the glottic region, and 55---75% are
diag-nosed with early cancers, with a favorable prognosis.2---5
Therefore,inthesecaseswheneverpossiblethetherapyfor
laryngeal cancer should aim for a high rate of local
con-trolassociatedwithpreservationof function.Suchresults
canbeachievedbydifferentapproaches, including
exter-nalbeamradiotherapy,transorallasermicrosurgery,partial
open laryngectomy and, more recently, robotic transoral
surgery.Eachoftheseoptionshasspecificadvantagesand
limitations, such as tumor extension, need for functional
reconstruction,technicalskill,andadequateresources.6,7
Currently,apredominanceofradiotherapyandtransoral
lasermicrosurgery appeartobethe treatment modalities
mostcommonlyused,particularlyforearlyglottic
carcino-mas,with open partial laryngectomy considered by some
authorsto befalling into disfavor.8 However,others have
notedthatopensurgerycanguaranteeanadequate
oncolo-gicalcontrol,associatedwithamoreaccuratepathological
stagingfor thecorrectindicationofadjuvant therapyand
riskstratificationofthesepatients.9,10Althoughsurgeryand
radiation therapy have coexisted asa treatment for
can-cer of the larynx sincethe early 20th century, there are
stillconflictingresultswhenthesetwotherapeutic
modal-itiesarecompared.Theaimof thisstudywastoevaluate
theoncologicalandfunctionalresultsofaseriesofpatients
undergoingopenpartiallaryngectomyvs.external
radiothe-rapyforthetreatmentofglotticcanceroflarynx.
Methods
This was a longitudinal historical cohort study approved
by the local Research Ethics Committee under No.
20538013.2.0000.5362andbasedondatacollectionof
medi-calrecordsfrompatientswithsquamouscellcarcinomaina
glottal laryngeal site, confirmed by the pathologyservice
and submitted to partial laryngectomy or external beam
radiation therapy at a tertiary centerfrom 2002to 2012.
PatientswithselectedT1/T2andT3earlyglotticcarcinoma
limitedtotheglottiswithoutmassiveextensiontothe
supra-glottis, infraglottis or to the paraglottic space, and who
weresuitablefortreatmentwithorganpreservation,were
consideredforinclusioncriteriainthestudy.Patientswith
bulkyT3glotticcarcinomanotsuitableforconservative
sur-gicaltreatmentandpatientswithadvancedT4carcinoma,
aswellaspatientswithminimalclinicalfollow-up(lessthan
24months)wereexcludedfromthestudy.
Allpatientswereinformedabouttreatmentoptionsbya
multidisciplinaryteaminvolvingsurgeons,radiation
oncolo-gists,andmedicaloncologists,andaftercounseling
under-wentpartiallaryngectomyorradiationtherapywithatotal
doseof70Gy(fractionatedat2Gy/day,fivedaysperweek)
asinitialtreatment,dependingonthepatient’spreference.
Chemotherapywithcisplatin20mg/m2/dayincombination
with5-fluorouacil1000mg/m2/dayby intravenousinfusion
ondays1---4and22---25wasperformed concomitantlywith
radiationforpatientswithT2orT3tumors(thusexcluding
patients with T1 glottic carcinoma) according to
Table1 Distributionaccordingclinicalstaging.
Staging Radiotherapy Opensurgery p
EC1 17(53.10%) 13(43.33%) EC2 9(28.10%) 7(23.33%) EC3 6(18.8%) 10(33.33%)
Total 32 30 0.91
indicatedforpatientswhopresentednarrow-compromised surgical margins, vascular/perineural invasion, and/or regional metastasis. After the selection of patients, an evaluation of homogeneity between the groups was con-ducted,andthecomparabilityofsampleswasdetermined. Theepidemiologicalcharacteristics,initialtreatmenttype, need for a temporary (during the treatment period) or permanent (patients who were unableto maintain venti-lation without tracheostomy after the end of treatment) tracheostomy,useofenteralnutritionvianasogastrictube orgastrostomy,complicationsduringtreatment(aspiration pneumonia, blood transfusion, salivary fistula), and need for adjuvant treatment (radiotherapy and/or chemother-apy)wereevaluated.Anevaluationofoncologicalresultsfor three-yeardisease-freetime,local-regionalrecurrence-free time,andoverallfive-yearsurvivalwasconducted.
Statistics
The results of quantitative variables were described as mean,median,minimumandmaximumvalues,andstandard deviations.Qualitativevariableswereexpressedas frequen-ciesandpercentages.Tocomparethegroupsdefinedbythe initialtreatment(radiationtherapyorsurgery)comparedto meanage,Student’st-testwasusedfor independent sam-ples.Regarding qualitativevariables,either Fisher’sexact test or the chi-squared test was employed for this com-parison. The comparison between groups with respect to disease-freetime,laryngealrescue-freetime,andsurvival timewascarriedoutusingtheLog-ranktest.Kaplan---Meier curveswerepresentedinordertodescribetheevolutionof thecasesinbothgroupscomparedtothetimesofinterest.
p-Values<0.05wereconsideredasstatisticallysignificant.
Results
During ten years, 199 patients with laryngeal carcinoma agedbetween30and84years,92.5%male,wereevaluated. The mostcommonsiteoflaryngeal cancerwastheglottis
Relapse Censored
156 144 132 120 108 96 84 72 60 48 36 24 12 0
Relapse-free time (months) 0.0
0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
Cumulative proportion
Surgery
Radiotherapy
p=.737
Figure1 Relapse-freetime/months.
in99patients(49.25%),followedbythesupraglotticareain 52cases(26.13%),while another49patients(24.62%)had largelesionsclassifiedastransglottictumors.
Among the 199 patients with laryngeal carcinoma, 62 patientswithglotticcarcinomawereincludedanddivided intotwogroupsaccordingtotheinitialproposedtreatment: GroupAunderwentpartiallaryngectomy(n=30)andGroup Bunderwentradiotherapy, withor without chemotherapy (n=32). Supracricoid laryngectomy was performed on 18 patients(twoT1b,sixT2,tenT3),whilefrontolateral laryn-gectomywasusedin12patients(11T1aandoneT2).Both groupswerehomogeneouswhencomparingmeanage(57.5
vs.59.5yearsforpatientsundergoingsurgeryor radiothe-rapy,respectively).Thesamewasobservedfordistribution in different clinical staging for the two groups (Table 1).
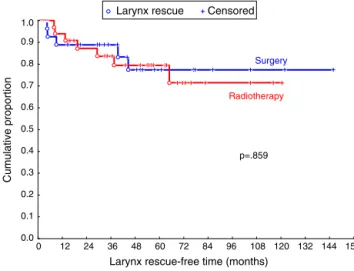
Evaluations of complications during treatment and
func-tional results are presented in Table 2. With regard to
oncologicaloutcome,nodifferenceswereobservedin
dis-tantmetastasisoccurrencerateorinsecondprimarytumor
betweengroups,aswellasindisease-freetime,laryngeal
rescue-freetime,andoverallfive-yearsurvival,asshownin
Figs.1---3.
Discussion
Itis currently accepted that radiotherapy,transoral laser
microsurgery, and open partial laryngectomy can provide
highlocalcontrolratesforpatientswithearlyglottic
carci-nomaoflarynxcoupledwithfunctionalconservationofthe
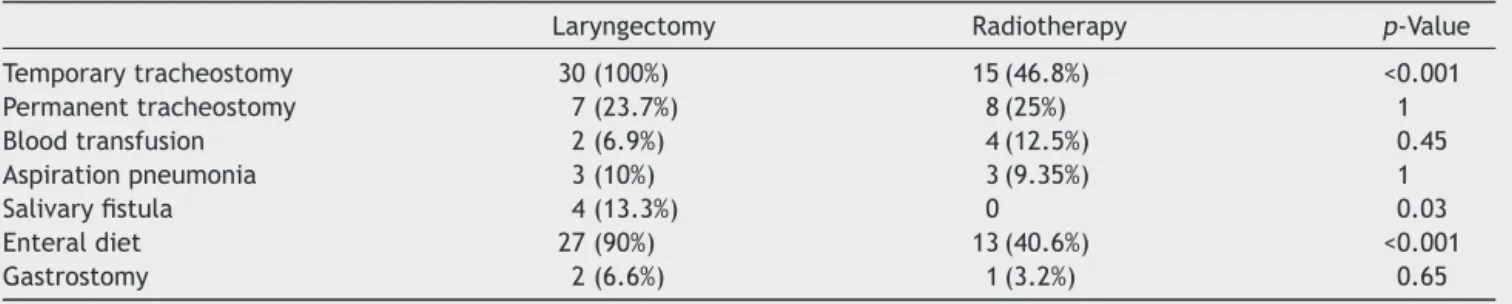
Table2 Complicationsandfunctionalresults.
Laryngectomy Radiotherapy p-Value
Temporarytracheostomy 30(100%) 15(46.8%) <0.001
Permanenttracheostomy 7(23.7%) 8(25%) 1
Bloodtransfusion 2(6.9%) 4(12.5%) 0.45
Aspirationpneumonia 3(10%) 3(9.35%) 1
Salivaryfistula 4(13.3%) 0 0.03
Enteraldiet 27(90%) 13(40.6%) <0.001
Larynx rescue Censored 156 144 132 120 108 96 84 72 60 48 36 24 12 0
Larynx rescue-free time (months) 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 Cumulative proportion Surgery Radiotherapy p=.859
Figure2 Larynxrescue-freetime.
organ.However,thereappearstobenohigh-levelevidence regarding the best treatment option for these patients, because of the lack of randomized studies comparing thesedifferent treatment options.11 Conservative surgery
has been one of the mainstays of treatment of laryngeal
cancersincethefirstsuccessfulresectionvialaryngofissure
credited to Sands in 1863,12 and later followed by the
descriptionofahemilaryngectomyperformedbyBillrothin
1875.13 In parallel tothe developmentof newtechniques
forpartiallaryngectomy,theevolutionofradiationtherapy
resultedin aneffective optionfor conservativetreatment
forlaryngeal carcinomas.14 Sincethen, somestudies have
triedtoassesstheoncologicaloutcomesofradiotherapyand
conservativesurgeryforglotticcarcinomas,butconflicting
results are often described, as those observed by Bron
etal.15 andZoharetal.,16 whofoundhigherlocalcontrol
ratescomparedtothoseofopensurgery,whileRuccietal.17
suggestedthatthelocal-regionalcontrolwithradiotherapy
wouldbemoreefficient,particularlyforpatientswithT1a
andT1bglotticcarcinomas.
However,Pontesetal.18 followed 43patients withT1a
andT1b laryngealcarcinomasubmittedtoaninitial
treat-ment with radiotherapy and observed a high recurrence
rate in 30.2% of patients after a mean follow-up time of
29.5 months. In the present series,it was observed that
Death Survival 156 144 132 120 108 96 84 72 60 48 36 24 12 0
Survival-free time (months)
0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 Cumulative proportion Surgery Radiotherapy p=0.903
Figure3 Overallsurvival.
theoverallthree-yeardisease-freeratesweresimilarboth
forpatientsundergoingpartiallaryngectomy(80.8%)andfor
thoseundergoingradiotherapy(76.9%).Althoughthereare
fewstudiesthatdirectlycomparedtheoncologicalresultsof
partiallaryngectomyvs.radiotherapyforselectedearlyand
T3glotticcarcinomasinthesameinstitution,in1984Kaplan
etal.19indicatedthatpatientswithearlyglotticcarcinomas
hadsimilaroncologicaloutcomeswhentreatedwith
radio-therapy or surgery.However,itwasobserved thatsurgery
was superior to radiotherapy in patients withreduced or
fixed vocal fold mobility (patients selected: T2 and T3);
thus,itwassuggestedthatopenlaryngectomyshouldbethe
firstlineoftreatmentforthesepatients.Theseresultswere
corroborated in a recent evidence-based review by Hartl
etal.20;theseauthorsconcludedthatpatientswithT2
glot-ticcarcinomacanachieveinitiallocalcontrolratesbetween
84% and 95%, which are comparableto rates after
radio-therapy,open partialsurgery,or transorallaserresection.
However,theyemphasizedthatpatientswithT2glottic
car-cinoma presenting reducedmobility or deepextension to
paraglotticspaceorventriclerepresentedasubgroupwith
lower local controlrates, whensubjected toradiation or
laser transoral surgery. Succo et al.21 also suggested that
openpartialsurgeryresultsinhigherlocalcontroland
long-term laryngeal preservation rates in patients with glottic
carcinoma, showing decreased or fixed vocal cord
mobil-itycomparedtothosetreatedwithtransorallasersurgery,
andconsideredthatthiswasduetothefactthat16.8%of
patientsclinicallystagedascT2wereclassifiedaspT3with
pathologicalstaging,andthatthisgroupwouldbe
particu-larlyfavoredbypartiallaryngectomy.
In general, there is evidence suggesting that patients
withglotticcancershowsimilarfive-yearsurvivalratesafter
radiotherapyoropenpartiallaryngectomy,rangingfrom70%
to88%forpatientswithT1carcinomaandbetween64%and
78%forT2tumors.4Thesamecanbeobservedinthepresent
study,withoverallfive-yearsurvivalratesof77.4%and72.9%
afterradiotherapyandsurgery,respectively.
Consideringthepossibilityofsimilaroncologicalresults,
some authorssuggest that partiallaryngectomy shouldbe
consideredasthefirsttherapeuticchoiceforglottictumors,
allowingaprecisepathologicalstagingofthedisease;
radio-therapy would be reserved for adjuvant therapy,or for a
second primarycarcinoma.22 However,radiotherapyis the
primaryform ofinitial treatment for glottic carcinoma in
mostcentersandreachesratesof84.4%ofcasesinCanada
and63.2%ofpatientsintheUnitedStates.23Oneadvantage
of radiotherapy is the possibilityof avoiding a temporary
or permanent tracheostomy usually associated with
con-servative laryngectomy.However,the authorsnoted that,
despitethefactthattemporarytracheostomieshavebeen
morefrequentinpatientsundergoingpartiallaryngectomy,
definitive tracheostomy rates (patients who could not be
decannulatedafterinitialtreatment)were28.1%and23.3%
afterradiotherapy andopenpartial laryngectomy,
respec-tively. Therefore,considering permanent tracheostomyas
themainnegativefunctionalconsequenceinthetreatment
ofpatientswithlaryngealcarcinoma,24,25thepresentstudy
didnotobserveasignificantdifferencebetweenthese
ther-apeuticmodalitiesregardingthisissue.
Anotherimportantaspectofthefunctionalpreservation
allowingcontinuationofanon-restrictedoraldiet.Whilethe
needfortemporaryenteralnutritionwassignificantlyhigher
inpatientsundergoingsurgery,itshouldbenotedthat40.6%
of patients undergoingradiotherapy also required enteral
nutritionduringtreatment,andsimilarratesofdietaryneed
fortemporarygastrostomywereobserved,bothinpatients
undergoingradiationtherapy(3.2%)andopenpartial
laryn-gectomy(6.7%).Dysphagiaafterpartiallaryngectomyisdue
tolocalchanges,causedbyresectionofstructuresandalso
bychangesinthemechanismoflaryngealelevation,while
radiationcausesdamagetothemucosaand
pharyngolaryn-gealmuscletissuesthatisdirectlyrelatedtothetherapeutic
doseused.
Debelleixetal.26 reviewedtheliteratureandconcluded
that,toreducethelaryngealedema,itwouldbe
appropri-atetolimittheradiationdoseincidenttonon-tumorareas
of the larynxtoabout 40---45Gy;but today mostpatients
receive 70Gyin conventional radiotherapy.Francis et al.
evaluatedtherelationshipbetweenthetherapeutic
modal-ityandthepotentialoflong-termdysphagiainpatientswith
headandneckcancer,concludingthatpatientsundergoing
radiotherapyandchemotherapy are2.5 timesmoreprone
toundergodysphagiacomparedtopatientsundergoing
sur-gicaltreatmentalone.27 Otherdrawbacksinthequalityof
life for patients with laryngeal cancer are also reported,
for instance, worsening invoice qualityand a
predisposi-tiontorespiratoryinfections(aspirationpneumonia)dueto
weaknessin swallowing. Traditionally,it hasbeen
consid-eredthatsurgery,eitheropenorendoscopic,isresponsible
forthehigherincidenceoftheseundesirableeffectswhen
compared to radiation therapy. This study demonstrated
thattheincidenceofaspirationpneumoniawascomparable
after radiotherapy (9.35%) andopen partiallaryngectomy
(10%).Somestudieshavealsoshownthatpartial
laryngec-tomypromotesbetterresultsconcerningdentalproblems,
drymouth,andswallowingingeneral.4,8
Although the literature suggests that oncological and
functionalresultscanbesimilarwhencomparingopen
par-tiallaryngectomyvs.radiotherapyforpatientswithglottic
cancer,theauthorshavenotedadeclineintheuseofopen
surgeryinrecentdecadesinfavoroflessinvasivetreatment
modalities,such as radiation or transoral laser resection.
However, it is important to emphasize that partial
laryn-gectomyremainsanoncologicallyandfunctionallyeffective
option,especiallyforpatientswithglotticcarcinomaswith
adecreaseorfixationofvocalfoldmobility,orinsituations
suchasunavailabilityoflasertechnologyor evenin
radio-therapyserviceswithalongwaitingtimefortreatment.
Conclusion
Open partial laryngectomy presented disease-free time
and overall survival outcomes similar to those obtained
with radiotherapy for selected patients with early
glot-ticandT3carcinomas,alsodemonstratingsimilarratesof
severe laryngealdysfunctionwithneed of permanent
tra-cheostomy.Therefore,thisproceduremust bemaintained
amongthemain therapeutic modalitiesavailable for such
cases,andthetreatmentselectionshouldconsiderthe
avail-abilityoflocalresources,waitingtimeforeachtreatment
modality,andpersonalpreferences.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Estimativa 2014: Incidência de Câncer no Brasil/Instituto NacionaldeCâncerJoséAlencarGomesdaSilva,Coordenac¸ão dePrevenc¸ãoeVigilância.RiodeJaneiro:INCA;2014http:// www.inca.gov.br/estimativa/2014/estimativa-24042014.pdf 2.GroomePA,O’SullivanB,IrishJC,RothwellDM,MathKS,
Bis-settRJ,etal.GlotticcancerinOntario,CanadaandtheSEER areasoftheUnitedStates:dodifferentmanagement philoso-phies produce different outcome profiles? J Clin Epidemiol. 2001;54:301---15.
3.JemalA,MurrayT,WardE,SamuelsA,TiwariRC,GhafoorA, etal.Cancerstatistics,2005.CACancerJClin.2005;55:10---30. 4.BackG, Sood S.The managementofearlylaryngeal cancer: optionsforpatientsandtherapists.CurrOpinOtolaryngolHead NeckSurg.2005;13:85---91.
5.StewartBW,WildCP,editors.WorldCancerReport2014.Lyon: WorldHealthOrganization;2014.p.1488---524.
6.ThomasL,DrinnanM,NateshB,MehannaH,JonesT,PaleriV. Openconservationpartiallaryngectomyforlaryngealcancer:a systematicreviewofEnglishlanguageliterature.CancerTreat Rev.2012;38:203---11.
7.Caicedo-GranadosE,BeswickDM,ChristopoulosA,Cunningham DE,RazfarA,OhrJP,etal.Oncologicandfunctionaloutcomes of partiallaryngeal surgery for intermediate-stage laryngeal cancer.OtolaryngolHeadNeckSurg.2013;148:235---42. 8.Silver CE, Beitler JJ, Shaha AR, Rinaldo A, Ferlito A.
Cur-rent trends in initial management of laryngeal cancer: the declining use of open surgery. Eur Arch Otorhinolaryngol. 2009;266:1333---52.
9.Brumund KT, Gutierrez-Fonseca R, Garcia D, Babin E, Hans S,Laccourreye O.Frontolateralverticalpartiallaryngectomy withouttracheotomyfor invasivesquamouscellcarcinomaof the true vocal cord: a 25year experience.Ann Otol Rhinol Laryngol.2005;114:314---22.
10.Mendenhall WM, Parsons JT, Stringer SP, Cassisi NJ, Million RR. T1---T2 vocalcord carcinoma:a basisfor comparingthe resultsofradiotherapyandsurgery.HeadNeckSurg.1988;10: 373---7.
11.Dey P, Arnold D, Wight R, MacKenzie K, Kelly C, Wilson J. Radiotherapyversusopensurgeryversusendolaryngealsurgery (withorwithoutlaser)forearlylaryngealsquamouscellcancer. CochraneDatabaseSystRev.2014,http://dx.doi.org/10.1002/ 14651858.CD002027[Publishedonline22.04.02].
12.KirchnerJA.Ahistoricalandhistologicalviewofpartial laryn-gectomy.BullNYAcadMed.1986;62:808---17.
13.Bailey BJ. Partial laryngectomy and laryngoplasty. Laryngo-scope.1971;81:1742---71.
14.DeSchryverA.Radiotherapyoflaryngealcancer.General princi-plesandresultsinT1andT2cases.ActaOtorhinolaryngolBelg. 1992;46:187---95.
15.BronLP,SoldatiD,ZouhairA,OzsahinM,BrossardE,MonnierP, etal.Treatmentofearlystagesquamous-cellcarcinomaofthe glotticlarynx:endoscopicsurgeryorcricohyoidoepiglottopexy versusradiotherapy.HeadNeck.2001;23:823---9.
16.ZoharY,RahimaM,ShviliY,TalmiYP,LurieH.The controver-sialtreatmentofanteriorcommissurecarcinomaofthelarynx. Laryngoscope.1992;102:69---72.
17.Rucci L, Gallo O, Fini-Storchi O. Glottic cancer involving anterior commissure: surgery vs. radiotherapy. Head Neck. 1991;13:403---10.
andsalvagesurgeryafterrecurrence.BrazJOtorhinolaryngol. 2011;77:299---302.
19.KaplanMJ,JohnsME,ClarkDA,CantrellRW.Glotticcarcinoma. Therolesofsurgeryandirradiation.Cancer.1984;53:2641---8. 20.HartlDM,FerlitoA,BrasnuDF,Langendijk JA,RinaldoA,
Sil-verCE,etal.Evidence-basedreviewoftreatmentoptionsfor patientswithglotticcancer.HeadNeck.2011;33:1638---48. 21.Succo G, Crossetti E, Bertolin A, Lucioni M, Caracciolo A,
Panetta V, et al. Benefits and drawbacks of open par-tial horizontal laryngectomies, part A: early-intermediate stageglotticcarcinoma.HeadNeck.2015,http://dx.doi.org/ 10.1002/hed.23997[Publishedonline10.01.15].
22.LefebvreJL.Whatistheroleofprimarysurgeryinthetreatment oflaryngealandhypopharyngealcancer?HayesMartinlecture. ArchOtolaryngolHeadNeckSurg.2000;126:285---8.
23.GroomePA,MackillopWJ,RothwellDM,O’SullivanB,IrishJC, Hall SF, et al. Management and outcome of glottic cancer:
apopulation-basedcomparisonbetweenOntario, Canadaand theSEERareasoftheUnitedStates.JOtolaryngol.2000;29: 67---77.
24.Campbell BH, Marbella A, Layde PM. Quality of life and recurrenceconcerninsurvivorsofheadandneckcancer. Laryn-goscope.2000;110:895---906.
25.ArmstrongE,IsmanK,DooleyP,BrineD,Riley N,DenticeR, etal.Ainvestigationintothequalityoflifeofindividualsafter laryngectomy.HeadNeck.2001;23:16---24.
26.Debelleix C, Pointreau Y, Lafond C, Denis F, Calais G, BourhisJH.Normal tissuetolerance toexternalbeam radia-tiontherapy:larynxandpharynx.CancerRadiother.2010;14: 301---6.